Sir,
Lichen planus pigmentosus (LPP) is an uncommon entity in children. Besides, the linear variant of LPP is an uncommon variant of the condition. We report a case of a 5-year-old boy with linear LPP over the nose with additional co-localization of milia. The scarcity of documentation of such presentation in pediatric age group prompted this report.
A 5-year-old boy presented with a single streak of bluish-black lesions over the nose, of 2 years duration, which was occasionally pruritic. Besides, the parents reported the development of two pinhead-sized whitish elevated lesions over these lesions; since the last 1-year. There was no history of any elevated lesion, erythema, or scaling preceding the presenting lesion. Past medical, surgical, and family histories were noncontributory. There was no history of any trauma, drug intake, contact with aromatic oils, perfumes, or herbs prior to the development of the lesions. Cutaneous examination showed multiple brown to bluish-black macules coalescing to form a single, linear macule over the dorsum of the right side of the nose, extending from the root until the nasal opening [Figure 1]. The lower half of the lesion revealed mild erythema. There were no similar lesions elsewhere. Besides, two pinhead-sized pearly white papules suggestive of milia were observed over the upper half of the linear macule. Mucosae, scalp, hair, and nails were normal. Considering the clinical differentials of linear LPP, ashy dermatosis, and postinflammatory hyperpigmentation, a skin biopsy was conducted. Histopathology revealed epidermal basal layer degeneration, scarce perivascular lymphohistiocytic infiltrate, prominent pigment incontinence, and dermal melanophages, consistent with a diagnosis of LPP [Figures 2 and 3]. Hematological investigations were normal and serology for hepatitis C negative. He was prescribed 2% hydroquinone and sunscreens for a month, which resulted in almost 60-70% improvement. The milia were manually extirpated with a needle.
Figure 1.

Solitary linear macule over the dorsum of right side of the nose
Figure 2.
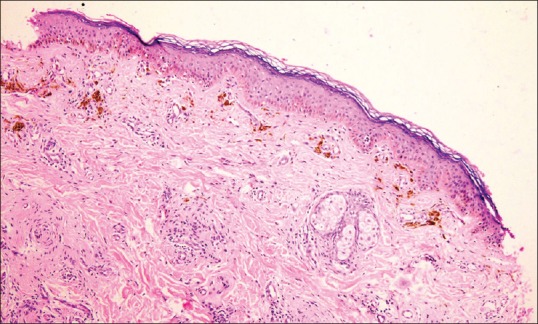
Photomicrograph showing basal layer degeneration, perivascular lymphohistiocytic infiltrate, pigment incontinence, and dermal melanophages (H and E, ×100)
Figure 3.
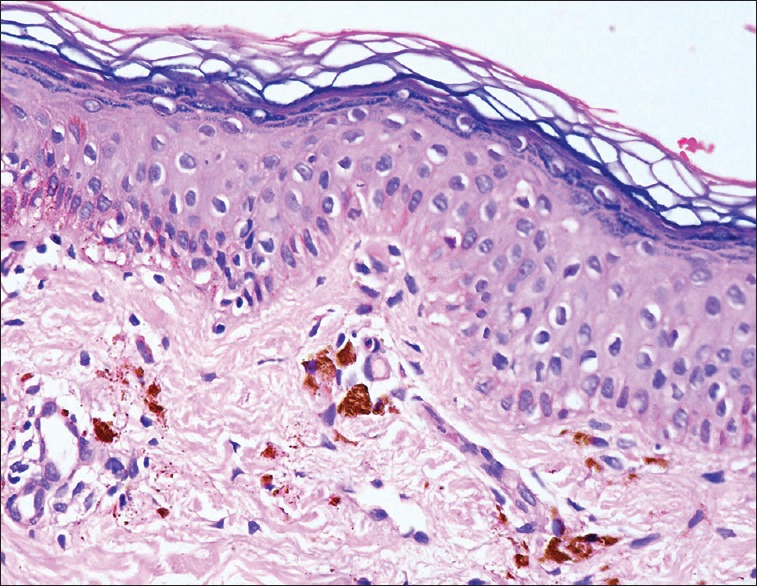
Photomicrograph showing basal layer degeneration, prominent pigment incontinence, and dermal melanophages (H and E, ×400)
LPP usually manifests in middle-aged population. Clinically, dark brown to bluish macules insidiously appear and expand, coalescing to form larger lesions, usually in sun-exposed areas, especially face and neck. The pigmentation may be diffuse, reticular, blotchy, linear, or perifollicular; with the diffuse type being the most common. Atypical presentations include involvement of nonsun-exposed areas (LPP inversus), flexural, linear, and segmental or zosteriform lesions.[1,2] Various factors, for example, viral infections and topical agents including mustard oil, amla oil, henna, and hair colors have been suggested as potential triggers. Apoptosis of keratinocytes may be caused by granzyme B and bone morphogenetic protein-4.[3] Histological features include epidermal atrophy, basal layer degeneration, dermal perivascular or lichenoid infiltrate, and pigment incontinence.[2]
Milia are common keratin-filled cystic lesions. While primary milia involve the face of infants, children, and adults, secondary milia in children result from damage to the pilosebaceous unit following trauma, dermabrasion, blistering disorders such as epidermolysis bullosa and porphyria cutanea tarda. Topical steroids and drugs such as vemurafenib and sorafenib have anecdotally been reported to cause milia. Recently, it has been reported in a child with linear cutaneous lupus erythematosus (LE); wherein, dystrophic calcinosis and secondary milia developed, and this was attributed to elevated alkaline phosphatase levels in the skin, lichenoid progression to basal membrane induced by chronic inflammatory course of LE, and trauma due to scratching.[4] In our case, development of milia could be explained by the ongoing inflammatory process of LPP. Co-localization of dermatoses has been reported on numerous occasions. LP has been reported to occur with porokeratosis, vitiligo, and lichen sclerosus.[5] However, to the best of our knowledge, co-localization of linear LPP and milia has not been reported yet.
LPP is rare in children. In a case series of 316 pediatric patients with LP, only nine (2.8%) were detected with LPP.[6] Furthermore, linear LPP is also uncommon (even in adults, the characteristic age group of LPP), with <10 cases reported until date. There is only one pediatric case of localized linear LPP reported.[2] Thus, this communique not only describes a child with a condition which is rare in this age group but also highlights the presence of its rare variant. This sui generis report gains further exclusivity owing to its co-localization with milia; a hitherto unreported association.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kumar YH, Babu AR. Segmental lichen planus pigmentosus: An unusual presentation. Indian Dermatol Online J. 2014;5:157–9. doi: 10.4103/2229-5178.131087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Das A, Mishra V, Podder I, Kumar P, Das D, Das NK. Linear lichen planus pigmentosus: A rare entity with an illusory presentation. Pigment Int. 2014;1:100–2. [Google Scholar]
- 3.Ammar M, Mokni M, Boubaker S, El Gaied A, Ben Osman A, Louzir H. Involvement of granzyme B and granulysin in the cytotoxic response in lichen planus. J Cutan Pathol. 2008;35:630–4. doi: 10.1111/j.1600-0560.2007.00892.x. [DOI] [PubMed] [Google Scholar]
- 4.Ma H, Liao M, Qiu S, Lu R, Lu C. Linear cutaneous lupus erythematosus with calcinosis cutis and milia. Pediatr Dermatol. 2015;32:e33–5. doi: 10.1111/pde.12496. [DOI] [PubMed] [Google Scholar]
- 5.Golchai J, Ramezanpour A. Report of a new case with four skin diseases. Dermatol Online J. 2003;9:15. [PubMed] [Google Scholar]
- 6.Pandhi D, Singal A, Bhattacharya SN. Lichen planus in childhood: A series of 316 patients. Pediatr Dermatol. 2014;31:59–67. doi: 10.1111/pde.12155. [DOI] [PubMed] [Google Scholar]


