Sir,
Mastocytosis is a group of disorders characterized by proliferation of mast cells. It can be an indolent disease limited to the skin (cutaneous mastocytosis and urticaria pigmentosa) or an aggressive one associated with myeloproliferative disorders and leukemias.[1] Telangiectasia macularis eruptiva perstans (TMEP) is a rare type accounting for <1% of cases of cutaneous mastocytosis and usually occurs in adult males although reported in children. Systemic association is rare. Till date, there is no strong evidence of association of mastocytosis and HIV, but there was a report of an apparent temporal association between mastocytosis and HIV.[2] We hereby report a case of TMEP in an HIV patient on highly active anti-retroviral therapy (HAART) proposing the probable relation of mastocytosis and HIV.
A 49-year-old man, who was on HAART for the preceding 7 years, presented to us with occasionally itchy reddish skin lesions over the chest and upper back. The lesions started 1 year back and gradually progressed to present state. Cutaneous examination showed numerous reddish-tan macules and telangiectasia (3–6 mm in diameter) over the anterior aspect of the upper chest and upper back. Few of the macules had coalesced to form patches [Figure 1]. Darier's sign was negative. There was no history of any abdominal pain, diarrhea, flushing, dyspnea, hypotension, black-outs, and bone pain. Family history was unremarkable. Routine laboratory investigations including complete hemogram, hepatic profile, renal profile, blood sugar, and urine examination were within normal limits. HIV serology was reactive. Punch biopsy was taken from a representative lesion, and histological examination showed dilated superficial dermal blood vessels with perivascular infiltrate of spindle-shaped mononuclear cell with eosinophilic cytoplasm and pale nuclei representing mast cells [Figures 2 and 3]. Special stains and immunohistochemical analysis could not be performed due to lack of resources and financial constraints. Based on the clinicopathological correlation, a diagnosis of TMEP was done. The patient was counseled regarding prognosis and the benign nature of the disease and asked for a periodic follow-up. After 2 weeks, the itching had decreased but the patient was subsequently lost to follow-up.
Figure 1.
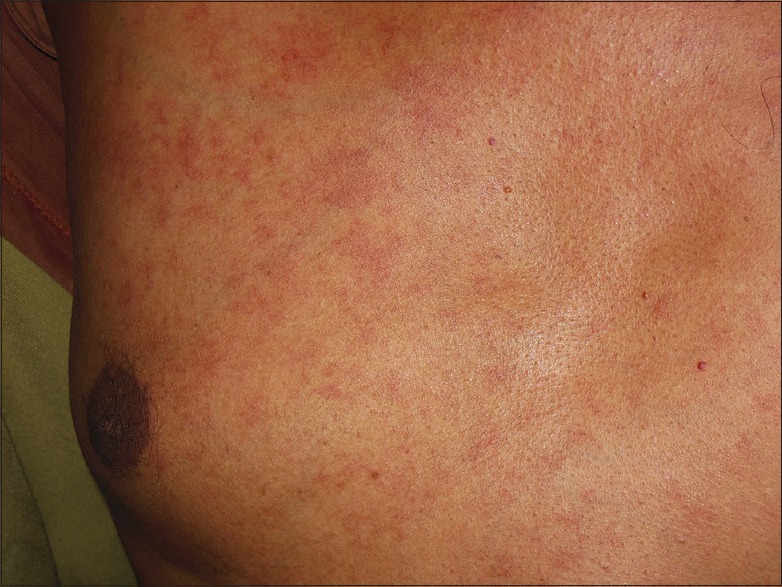
Diffuse erythematous macules and telangiectasia
Figure 2.
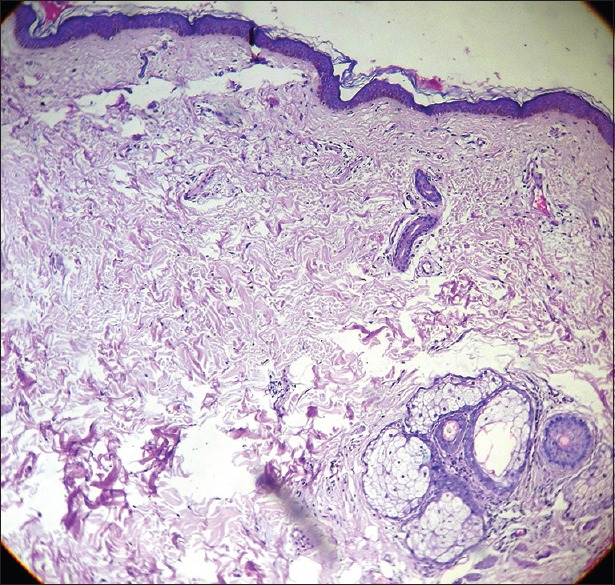
Dilated superficial dermal blood vessels and increased pigmentation of the epidermal basal layer (H and E, ×100)
Figure 3.
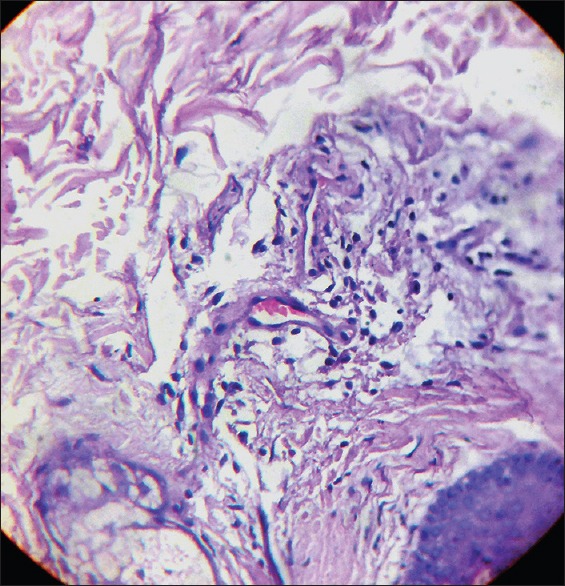
Perivascular infiltration of spindle-shaped cells representing mast cells (H and E, ×400)
Cutaneous mastocytosis is a self-limiting condition, and it does not involve any internal organs. TMEP, accounting for <1% of cases of cutaneous mastocytosis, usually affects adults. Clinically, it is manifested as reddish-brown macules, telangiectasia, and hyperpigmentation, mostly distributed over the upper chest and extremities. Darier's sign is usually negative.[3] Systemic involvement may be present, and this is usually characterized by abdominal pain, diarrhea, flushing, dyspnea, hypotension, syncope, hepatosplenomegaly, lymphadenopathy, and bone changes.[4] Besides, elevated levels of serum tryptase and 24-h urinary n-methylhistamine and prostaglandin D2 metabolites may correlate with systemic manifestations.[5] A mutation in the c-kit oncogene results in the hyperplasia of mast cells, but there is a lack of evidence in the role of c-kit mutations in the etiopathogenesis of TMEP.[6]
Till date, there is no evidence of any interaction between HIV and mast cells, but there are ample evidences of basophil and HIV interaction. Both basophils and mast cells express high-affinity receptor for IgE (FcERI).[7] HIV transactivation protein (Tat) interacts with a chemokine receptor CCR3 and acts as a chemoattractant for FcERI positive cells such as basophils. Besides, another chemotactic factor for basophils is the HIV gp41 envelope glycoprotein. There are quite a few numbers of HIV receptors such as CD4, CCR3, CCR5, and CXR4, which are expressed on basophils and play a role in the infection of basophils with HIV. Similarly, this interplay may infect mast cells as well since both basophils and mast cells are closely related.
Histologically, TMEP shows perivascular and interstitial mast cells surrounding telangiectatic blood vessels. Giemsa or toluidine blue staining delineates the mast cells by virtue of the demonstration of metachromatic granules. The treatment essentially consists of avoidance of the factors which trigger the degranulation of mast cells such as sunlight, variations in temperature, drugs such as polymyxin B, nonsteroidal anti-inflammatory drugs, and morphine. Therapeutic options include H1 antagonists, ketotifen, cromolyn sodium, topical and systemic corticosteroids, leukotriene antagonists, alpha interferon, Psoralen plus ultraviolet light A) therapy, electron beam radiation therapy, and flashlamp pumped dye laser (585 nm wavelength).
To conclude, we report a case of TMEP in an HIV-positive patient and try to explore the probable temporal relation between the two conditions. There is one such report of an association of mastocytosis and HIV in the past.[2] We look forward for further research about the pathogenetic mechanism which can explain this probable association.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Altiner A, Tzu J, Patel R, Meehan S, Sanchez M. Telangiectasia macularis eruptiva perstans. Dermatol Online J. 2011;17:7. [PubMed] [Google Scholar]
- 2.Soilleux EJ, Grills C, Cooper SM. Cutaneous mastocytosis in human immunodeficiency virus: An unfortunate coincidence? Clin Exp Dermatol. 2008;33:619–21. doi: 10.1111/j.1365-2230.2008.02779.x. [DOI] [PubMed] [Google Scholar]
- 3.Oliveira CR, Albuquerque GC, Simon EF, Quinete SS, Carvalho CR. Case for diagnosis. Telangiectasia macularis eruptiva perstans. An Bras Dermatol. 2009;84:87–9. doi: 10.1590/s0365-05962009000100015. [DOI] [PubMed] [Google Scholar]
- 4.Izikson L, English JC, 3rd, Zirwas MJ. The flushing patient: Differential diagnosis, workup, and treatment. J Am Acad Dermatol. 2006;55:193–208. doi: 10.1016/j.jaad.2005.07.057. [DOI] [PubMed] [Google Scholar]
- 5.Costa DL, Moura HH, Rodrigues R, Pineiro-Maceira J, Ramos-E-Silva M. Telangiectasia macularis eruptiva perstans: A rare form of adult mastocytosis. J Clin Aesthet Dermatol. 2011;4:52–4. [PMC free article] [PubMed] [Google Scholar]
- 6.Lee HW, Jeong YI, Choi JC, Lee MW, Choi JH, Moon KC, et al. Two cases of telangiectasia macularis eruptiva perstans demonstrated by immunohistochemistry for c-kit (CD 117) J Dermatol. 2005;32:817–20. doi: 10.1111/j.1346-8138.2005.tb00851.x. [DOI] [PubMed] [Google Scholar]
- 7.Marone G, Florio G, Petraroli A, Triggiani M, de Paulis A. Human mast cells and basophils in HIV-1 infection. Trends Immunol. 2001;22:229–32. doi: 10.1016/s1471-4906(01)01903-2. [DOI] [PubMed] [Google Scholar]


