Abstract
Background: Previous studies have identified significant variability in attention-deficit / hyperactivity disorder (ADHD) prevalence estimates worldwide, largely explained by methodological procedures. However, increasing rates of ADHD diagnosis and treatment throughout the past few decades have fuelled concerns about whether the true prevalence of the disorder has increased over time.
Methods: We updated the two most comprehensive systematic reviews on ADHD prevalence available in the literature. Meta-regression analyses were conducted to test the effect of year of study in the context of both methodological variables that determined variability in ADHD prevalence (diagnostic criteria, impairment criterion and source of information), and the geographical location of studies.
Results: We identified 154 original studies and included 135 in the multivariate analysis. Methodological procedures investigated were significantly associated with heterogeneity of studies. Geographical location and year of study were not associated with variability in ADHD prevalence estimates.
Conclusions: Confirming previous findings, variability in ADHD prevalence estimates is mostly explained by methodological characteristics of the studies. In the past three decades, there has been no evidence to suggest an increase in the number of children in the community who meet criteria for ADHD when standardized diagnostic procedures are followed.
Keywords: ADHD, epidemiology, prevalence, time, cross-cultural, methodology
Key Messages.
Estimates of ADHD prevalence are significantly variable.
Variability of prevalence rates is accounted for by methodological characteristics of studies, specifically diagnostic criteria used, source of information, and requirement of impairment for the diagnosis.
Geographical location and year of study are not associated with variability of prevalence estimates.
By aggregating prevalence studies of ADHD conducted in the past three decades, there is no evidence to suggest an increase in the number of children in the population who meet criteria for ADHD when standardized diagnostic procedures are followed.
Background
Attention-deficit / hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by a persistent pattern of inattention, hyperactivity and impulsivity that is pervasive across settings and leads to various degrees of functional impairment.1 The recognition and treatment of ADHD date from the second half of the 20th century.2 Since then, significant advances have been made towards understanding the disorder, resulting in the dissemination of knowledge across societies and in increasing recognition and treatment of affected individuals.3,4 Nevertheless, concerns about the true prevalence of ADHD and its validity have been raised.3
Concerns about the prevalence and validity of the disorder emerged for several reasons, among them: (i) an evident variability in estimates across different studies; (ii) an apparent higher prevalence in Western societies, especially in the USA; and (iii) an apparent increase in rates of the disorder over time.3,4 In 2007, Polanczyk et al.5 published the first comprehensive review of the literature on the prevalence of ADHD, which included 102 studies conducted across the world. The studies ascertained non-referred samples of children and adolescents, who were assessed according to a variety of procedures to identify the disorder. Studies adhering to diagnostic criteria from one of the three versions of DSM (III, III-R or IV) or the recent versions of the ICD (9 or 10) were included. Meta-analysis resulted in a pooled prevalence rate of 5.29% [95% confidence interval (CI) 5.01 – 5.56], associated with significant heterogeneity. A meta-regression analysis identified that diagnostic criteria, source of information for reporting the symptoms, and requirement of functional impairment for the diagnosis were methodological procedures significantly associated with variability of estimates. The analysis identified that study location was associated with heterogeneity only when estimates from Africa and the Middle East were compared with estimates from North America. Estimates from Europe, Oceania, South America and Asia did not differ from estimates from North America.5
The meta-regression analysis addressed the first two concerns frequently raised regarding the prevalence of the disorder. Firstly, results indicated that in fact there was a high degree of variability between estimates, largely explained by study methods. This did not necessarily imply a lack of validity, but more likely reflected a lack of consensus between investigators on how best to ascertain the disorder.6 Secondly, results indicated that study location was not a significant factor in variability of estimates, excluding Africa and the Middle East. Because only four estimates of ADHD prevalence from each one of these two geographical regions were included in the analysis, no definite conclusions could be drawn. Finally, the analysis did not address the question of the effect of time over the variability of estimates.
In 2012, Willcutt7 published a second comprehensive review of the literature on the prevalence of ADHD, focused only on studies using DSM-IV diagnostic criteria; 86 studies were included, over half of them published after the 2007 review. Meta-analytical results generated estimates in children and adolescents ranging from 5.9% to 7.1%, depending on the source of information for the diagnosis. Further results detected significant heterogeneity between estimates, but once again country or region where the study was conducted did not explain the variability, supporting previous findings.7 In addition, this study also did not address the effect of time on estimates.
The question of increasing prevalence of ADHD over time is a natural reflection of the finding that rates of diagnosis have been rising in recent years. For example, in the USA, two national telephone surveys demonstrated that the percentage of children aged 4 to 17 years with a lifetime diagnosis of ADHD, according to parents, increased by 21.8% from 2003 to 2007.8 The increase in the rates of diagnosis is not a phenomenon limited to ADHD in the child mental health field. Several studies have documented an increase in prevalence rates of autistic spectrum disorders (ASD) in diverse cultures over past years.9 There is very good evidence indicating that changes in diagnostic criteria and in policies for special education, and increasing awareness and access to medical services may explain the increasing rates over time.10 However, the possibility that a true increase in the incidence of ASD and also in ADHD exists cannot currently be excluded due to lack of definite evidence. One additional reason for concern is whether pressure from pharmaceutical industries contributes to increasing rates of diagnoses and consequently of prescriptions for treatment of the disorders.3 A true and significant increase in prevalence rates of ADHD across the past few decades, reflecting an increase in incidence, should be an issue of public health concern. The reasons behind this phenomenon would need to be explored, and the identification of associated factors would potentially allow for a better understanding of the aetiology of the disorder and a more efficient way of delineating preventive strategies and treatment interventions.
Therefore, to test the effect of time on prevalence estimates of ADHD generated by standardized diagnostic procedures, we took advantage of the two most comprehensive systematic reviews of the literature on prevalence studies of ADHD conducted until now, and updated them through a joint effort by the two research teams involved in these previous studies. We then investigated the effect of the year of the studies as a further independent variable in a multivariate meta-regression analysis. Additionally, because more studies had accumulated since the first meta-regression was reported, we conducted updated analyses to explore the variability of estimates as a function of study methods and geographical location.
Methods
Literature search
We built our literature review on the two most comprehensive reviews on ADHD prevalence studies available in the literature. Polanczyk et al.5 searched for original surveys published between 1978 and 2006, which assessed probabilistic samples of individuals 18 years of age or younger, ascertained from the general population (households, birth registers) or from schools, generating point prevalence, with diagnoses based on any DSM (III, III-R, or IV) or ICD (9 or 10) versions. Authors reviewed 9105 abstracts, and 102 studies were included. Willcutt 7 searched for original surveys published between 1994 and 2010 that assessed probabilistic samples of children, adolescents and adults, ascertained from the general population (households, birth registers), primary care or from schools, generating point prevalence, with diagnoses based on DSM-IV. The author reviewed 15 736 abstracts, and 97 studies (86 samples of children and adolescents and 11 samples of adults) were included.
We updated both systematic reviews using the specific search strategy implemented in each study. For Polanczyk et al., we updated the search from 2007 to 2012, and restricted it to only those studies that used ICD, as DSM-IV studies would be identified by Willcutt’s review. Electronic search yielded 163 results (121 in MEDLINE and 42 in PsycINFO). For the Willcutt review, we updated the search from 2011 to 2012, restricting the search to individuals 18 years of age or younger, since the scope of this study was to assess the increase in prevalence rates in youths. Electronic search yielded 1128 results (407 in MEDLINE, 422 in PsycINFO, 39 in ERIC, 260 in Web of Science). All abstracts (1291) and the full reports of original studies were independently reviewed by two authors (G.A.S. and C.K.), who decided on the inclusion of each study according to the original criteria of the Polanczyk et al. review. Disagreements were reviewed by the senior author (L.A.R.). Reference lists were also reviewed.
Among the studies included in the previous reviews and fulfilling the inclusion criteria for this study, 81 were included only in the Polanczyk et al. review, 43 were included only in the Willcutt review and 21 were included in both the Polanczyk et al. and the Willcutt reviews. The main reasons for differences in the inclusion of studies between the two reviews were diagnostic criteria (inclusion of studies using ICD criteria in the Polanczyk et al. review, but not in the Willcutt review) and time-frame (for Polanczyk et al. 1895 to 2006, for Willcutt 1994 to 2010). The updated review identified nine additional studies (two of them were also included in the Willcutt review). Therefore, 154 studies were included in the current study.
Data extraction
Information extracted by the two previous reviews overlapped. Data from the newly identified studies were extracted independently by two authors (G.A.S. and C.K.) according to the protocol used by Polanczyk et al., and disagreements were discussed with the first author (G.V.P.). When multiple prevalence estimates were generated for the same sample according to different methods (e.g. source of information, diagnostic criteria), one estimate was extracted following a predefined protocol ensuring that each individual from each sample contributed only with a single estimate.
Definition of variables included in analyses
We initially looked for year of sample assessment as reported by each study as our main independent variable of interest. Because approximately 30% of studies did not report this information, we used year of publication as proxy information for year of assessment.
Since our previous analysis documented the relevance of a specific group of methodological variables in the determination of the heterogeneity of ADHD prevalence rates worldwide, we decided also to investigate the role of year of study in the context of these variables. It is important to note that a significant overlap (66%) was detected between studies included here and those already analysed in the Polanczyk et al. meta-regression. The effects of year of study publication and geographical location of the study [North America (reference), Europe, Oceania, South America, Asia, Africa and Middle East] were investigated. Additionally, the effects of the following three methodological variables were tested: source of information, diagnostic criteria and impairment criteria. Source of information was defined in five categories: best-estimate procedure (reference), ‘and rule’ (a symptom was considered to be positive if was endorsed by two informants), parents, ‘or rule’ (a symptom was considered to be positive if was endorsed by one out of two informants), teachers and subjects. Diagnostic criteria was defined in four categories: DSM-III, DSM-III-R, DSM-IV (reference) and ICD-10. The impairment criterion was defined in two categories: yes (reference) and no.
Data analysis
Meta-regression analyses were carried out using linear mixed-effects models.11 Covariates were first tested individually in a univariate analysis and then simultaneously in a multiple meta-regression model via likelihood ratio test (LRT) using the maximum likelihood estimator. The ‘variance accounted for’ (VAF), a pseudo-R2 statistic, is given for each univariate model, indicating the percentage of the total heterogeneity in the true effects (heterogeneity) that is accounted for by each study-level variable (moderator) individually.12 We also calculated the VAF for the model with all covariates included.
Outlier and influential case diagnostics were performed using the externally standardized residuals, DFFITS values, Cook’s distances, covariance ratios, leave-one-out estimates of the amount of heterogeneity, leave-one-out heterogeneity test statistics, hat values and weights.13 The analysis and graphical presentation were conducted with R using the ‘metafor’ package.12
Results
We were able to identify 154 eligible studies published from 1985 to 2012 for inclusion in the current review. This figure represents an increase of approximately 50% in the number of studies published in the past 6 years, considering that the revision by Polanczyk et al. included 102 studies published up to 2006. The 25th, 50th and 75th percentiles of year distribution corresponded, respectively, to years 1997, 2001 and 2005. For 19 studies, the lack of information reported in the articles made it impossible to define the source of information and/or impairment criterion. Because these studies are not considered for multivariate analysis, they were excluded. Table 1 presents the characteristics of 135 studies included in the multivariate analysis.
Table 1.
Description of study methods, geographical location and year of publication of studies included in the multivariate analysis (k = 135)
| Characteristic | k |
|---|---|
| Source of information | |
| Best-estimate | 27 |
| ‘And rule’ | 15 |
| ‘Or rule’ | 11 |
| Parents | 57 |
| Teachers | 19 |
| Subjects | 6 |
| Impairment criterion | |
| Yes | 67 |
| No | 68 |
| Diagnostic criteria | |
| DSM-IV | 81 |
| DSM-III-R | 31 |
| DSM-III | 10 |
| ICD-10 | 13 |
| Geographical location | |
| North America | 48 |
| Europe | 42 |
| Oceania | 7 |
| South America | 10 |
| Asia | 12 |
| Africa | 5 |
| Middle East | 11 |
| Year of publication | |
| 1985–89 | 7 |
| 1990–94 | 13 |
| 1995–99 | 35 |
| 2000–04 | 36 |
| 2005–09 | 30 |
| 2010–12 | 14 |
k, number of studies.
As depicted in Table 2, univariate analysis revealed that all covariates were significantly associated with heterogeneity of prevalence estimates, except for year of study publication (P = 0.68). In the multivariate meta-regression model, source of information, impairment criterion and diagnostic criteria remained significantly associated with heterogeneity of results. Geographical location was no longer significant (P-values range 0.172 – 0.651), and year of publication remained not associated with heterogeneity (P = 0.836). Table 2 presents estimated prevalence difference between all levels of each covariate in relation to the index level. Prevalence rates based on teacher reports were an estimated 5.47% higher than those based on best-estimate procedure (P = 0.003). Prevalence rates with no requirement of impairment were an estimated 2.32% higher than when impairment was required (P = 0.018). Prevalence rates based on DSM-III-R and ICD-10 were an estimated 2.42% and 4.09% lower, respectively, than rates based on DSM-IV (P = 0.044 and P = 0.009, respectively). The final model accounted for 44.1% of the variance.
Table 2.
Univariate and multiple meta-regression models
| Study characteristics |
Univariate meta-regression models |
Multiple meta-regression models |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated prev diff | SE | 95% CI | P |
Moderator analysisa |
LRT (df = 1) = 73.4495; P <0.0001; VAF = 44.09% |
||||||||
| LRT (df) | P | VAF | Estimated prev diff | SE | 95% CI | P | |||||||
| Source of information | 44.2 (1) | <0.0001 | 29.41% | ||||||||||
| Best-estimate [reference] | − | − | − | − | − | − | − | − | − | − | |||
| ‘And rule’ | −0.82 | 1.54 | −3.87 | 2.23 | 0.596 | −2.35 | 1.63 | −5.60 | 0.89 | 0.153 | |||
| ‘Or rule’ | 4.14 | 1.75 | 0.67 | 7.61 | 0.020 | 2.55 | 1.82 | −1.06 | 6.16 | 0.164 | |||
| Parents | 1.67 | 1.13 | −0.55 | 3.90 | 0.139 | 0.54 | 1.29 | −2.01 | 3.09 | 0.675 | |||
| Teachers | 8.24 | 1.46 | 5.35 | 11.13 | <.0001 | 5.47 | 1.77 | 1.97 | 8.97 | 0.003 | |||
| Subjects | −2.46 | 2.15 | −6.72 | 1.79 | 0.254 | −3.40 | 2.16 | −7.69 | 0.89 | 0.119 | |||
| Impairment criterion | 13.03 (1) | 0.0003 | 9.84% | ||||||||||
| Yes [reference] | − | – | – | – | – | − | − | − | − | − | |||
| No | 3.32 | 0.91 | 1.50 | 45.13 | 0.0004 | 2.32 | 0.96 | 0.40 | 4.22 | 0.018 | |||
| Diagnostic criteria | 20.62 (1) | 0.0001 | 15.22% | ||||||||||
| DSM-IV [reference] | − | − | − | − | − | − | − | − | − | − | |||
| DSM-III-R | –2.93 | 1.11 | –5.14 | –0.74 | 0.01 | –2.42 | 1.19 | –4.78 | –0.06 | 0.044 | |||
| DSM-III | −2.65 | 1.70 | −6.013 | 0.71 | 0.12 | −1.79 | 1.85 | −5.46 | 1.88 | 0.336 | |||
| ICD-10 | –6.37 | 1.55 | –9.44 | –3.31 | <.0001 | –4.09 | 1.53 | –7.13 | –1.05 | 0.009 | |||
| Geographical location | 13.01 (1) | 0.0429 | 9.21% | ||||||||||
| North America [reference] | − | − | − | − | − | − | − | − | − | − | |||
| Europe | –2.36 | 1.15 | –4.64 | –0.085 | 0.04 | −0.77 | 1.08 | −2.92 | 1.38 | 0.478 | |||
| Oceania | −2.23 | 2.19 | −6.54 | 2.08 | 0.31 | −0.88 | 1.94 | −4.72 | 2.96 | 0.651 | |||
| South America | 2.12 | 1.92 | −1.68 | 5.93 | 0.27 | 1.38 | 1.72 | −2.03 | 4.79 | 0.424 | |||
| Asia | –4.04 | 1.75 | –7.50 | –0.567 | 0.02 | −2.19 | 1.59 | −5.33 | 0.96 | 0.172 | |||
| Africa | 0.49 | 2.54 | −4.54 | 5.521 | 0.85 | −2.81 | 2.24 | −7.25 | 1.62 | 0.211 | |||
| Middle East | −2.56 | 1.75 | −6.03 | 0.913 | 0.15 | −1.39 | 1.68 | −4.72 | 1.94 | 0.411 | |||
| Year | 0.03 | 0.08 | −0.12 | 0.19 | 0.68 | 0.177 (1) | 0.6741 | 0.22% | 0.02 | 0.09 | −0.16 | 0.20 | 0.836 |
Prev, prevalence; diff, difference; VAF, variance accounted for; LRT, likelihood ratio test. Bold indicates covariates associated at a P value < 0.05.
aCompares model with no variable vs model with each variable individually via likelihood ratio tests to test the effect of each variable on heterogeneity of estimates and indicates how much of the residual heterogeneity in the reduced model is accounted for in the full model.14
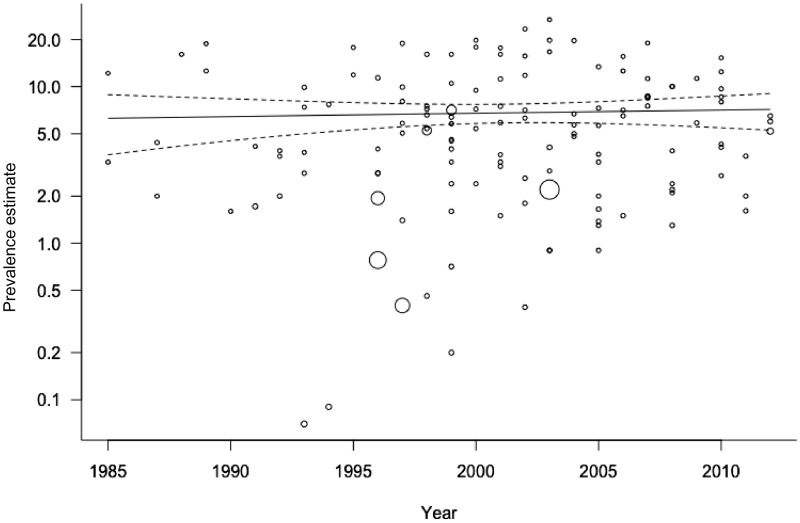
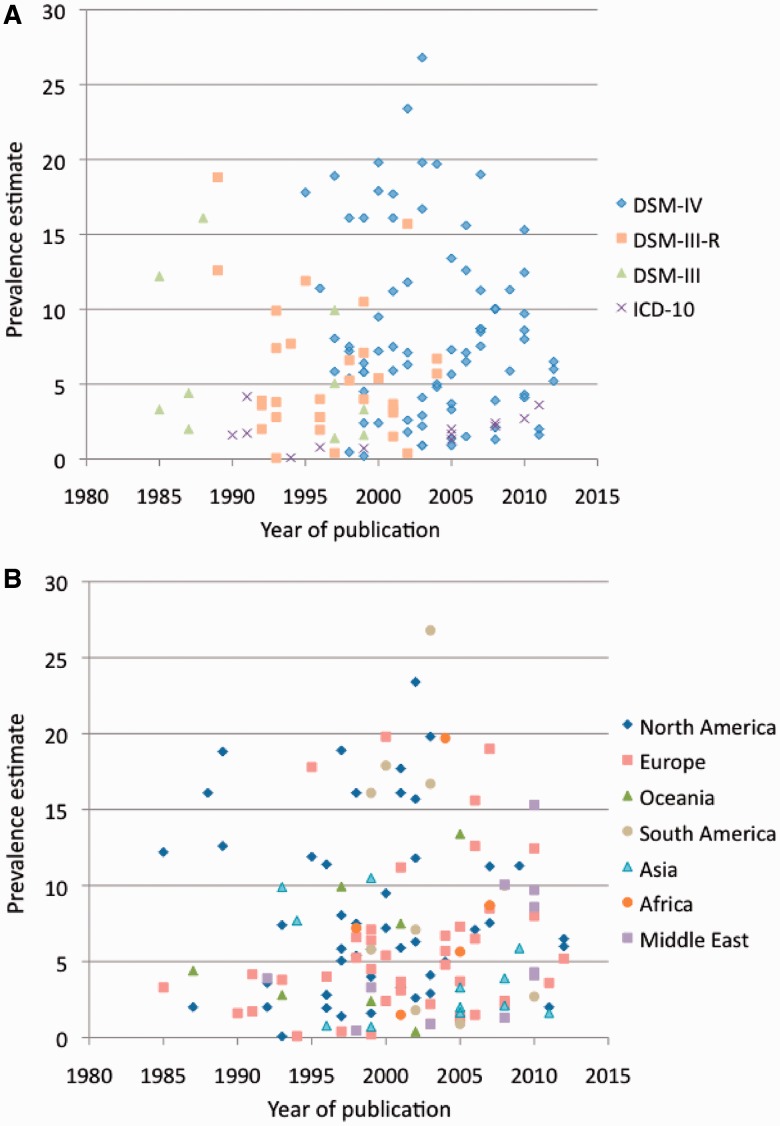
Figure 1 shows prevalence estimates over time. To further explore the effect of year of study on heterogeneity of estimates, we tested its interactive effect with each one of the methodological characteristics and with geographical location. No significant interaction was detected, ruling out a possible increase in the prevalence estimates over time in specific geographical locations or for specific study methods. We specifically tested the effect of methodological variables, geographical location and year of publication only for studies using DSM-IV criteria, published from 1995 to 2012 (k = 81). Results were unchanged from the model including all studies, with significant effect of source of information and impairment criterion, and no effect of geographical location and year of publication (data available upon request). Figure 2 depicts prevalence estimates as a function of time and both diagnostic criteria and geographical location.
Figure 1.
ADHD prevalence estimates as a function of year of study publication. The point sizes are drawn proportional to the inverse of the standard errors. The predicted average prevalence estimate rate based on a mixed-effects model is added to the plot (with corresponding 95% confidence interval bounds).
Figure 2.
ADHD prevalence estimates over time, as a function of diagnostic criteria (A) and geographical location of studies (B).
Two studies were found to be outliers and influential in the final model according to several diagnostic indexes (Supplementary Figure, available as Supplementary data at IJE online). The exclusion of these studies had very low impact on estimation of coefficients and limited influence on significance tests, except for differences between DSM-III-R and DSM-IV that were no longer significant (P = 0.0557). No association between publication year and variability on prevalence rates was found following the exclusion of outliers [β = 0.0564, 95% confidence interval (CI) −0.0959 to 0.2086, SE = 0.0770, P = 0.4653].
Discussion
We have updated the two most comprehensive systematic reviews of studies addressing the prevalence of ADHD around the world and were able to include 135 studies published from 1985 to 2012 in our final model. Subsequently, we conducted a meta-regression analysis to test the effect of time on variability of estimates and updated previous analyses5 to explore the effect of methods and geographical location of studies. Our findings indicate that when controlling for study methods, prevalence estimates did not vary as a function of year of study during the past three decades. Diagnostic criteria, impairment criterion and source of information remained significantly associated with heterogeneity of estimates. Adjusting for methodological characteristics of studies, geographical location was not associated with heterogeneity of prevalence estimates.
As far as we are aware, this is the first study to directly address the question of a potential increase in prevalence rates of ADHD over time. Concerns were generated from a number of studies which showed that rates of diagnosis and treatment are in fact increasing. Two USA national landline telephone surveys conducted in 2003 and 2007 asked parents whether or not a doctor or other healthcare provider had ever told them that their child aged 4 to 17 years (randomly selected for the survey) had ‘attention deficit disorder or attention deficit hyperactive disorder’. Interviews were conducted with about 102 353 and 73 123 children in each respective year. The percentage of children with a lifetime diagnosis of ADHD increased from 7.8% to 9.5% from 2003 to 2007, a 21.8% increase. In 2007, among those with a current ADHD diagnosis, 66.3% were taking medication for the disorder, representing 4.8% of all children aged 4 to 17 years. Another study using the medical records of a health plan in California reported a relative increase of 24% in the incidence of physician-diagnosed ADHD in children aged 5 to 11 years from 2001 to 2010.14 These figures are in accordance with other studies conducted in the USA,15–17 UK18 and Canada19 using administrative data from the 1990s and 2000s and reporting increasing rates of ADHD diagnosis and prescription of medications for the treatment over time. However, these data do not represent the rates of true prevalence of the disorder as they rely on administrative data, physicians or parents who report the diagnosis. True prevalence rates are estimated by standardized procedures in representative samples of the community.
This study aggregated original studies that estimated the prevalence of ADHD by using standard diagnostic criteria, and identified no effect of year of study on the variability of estimates. This indicates that, controlling for study methods, the true prevalence of the disorder did not increase from 1985 to 2012. Considering that ADHD is a chronic disorder, the absence of modification in prevalence estimates by year of study indirectly suggests that no increase in the incidence of ADHD occurred over the past three decades. Given our findings, the increasing rates of diagnosis of ADHD in clinical and administrative samples are probably related to increasing awareness and access to services. However, it is not possible to rule out potential changes in clinical practices over time. Thus, the validity of ADHD diagnoses in several clinical settings in certain countries like the USA should be carefully assessed in studies designed for this purpose. The estimate of the rates of diagnosis and treatment does not, in general, exceed the estimates of the prevalence of the disorder in the majority of countries where these data are available. In fact, in some countries, rates of diagnosis and treatment are below the estimated prevalence rate, indicating lack of recognition of the disorder and of access to resources.20,21 However, surveillance studies of medical and non-medical use of medications for the treatment of ADHD in different cultures are necessary in order to expand on this issue.
Further results of the meta-regression analysis indicated that study methods are associated with significant heterogeneity of estimates, corroborating previously reported results that were already extensively discussed.5–7,22 Additionally, with the extension of the number of studies included, the current analysis had more power to investigate the effect of geographical location on the variability of estimates, especially for continents less represented in the previous analysis. The estimate for North America remained no different from those of Europe, Oceania, South America and Asia. Estimates from Africa and the Middle East, which increased by 1 and 7 studies, respectively, became no significantly different from that of North America. This is consonant with numerous studies that have addressed cross-cultural differences in regard to symptom expression and structure, identification and treatment of ADHD, and that generally demonstrate invariance across cultures.23–25 Nevertheless, because the vast majority of studies did not ascertain representative samples of each country, it is not possible to exclude the possibility that broader social characteristics impact on the occurrence of the disorder.26 This issue needs to be further explored.
Our study must be understood in the context of its limitations. First, we analysed cross-sectional studies conducted at different time points and locations using different methods. To address the question of modification of the incidence of the disorder over time, higher-quality data would need to come from repeated cross-sectional studies (conducted in the same location with the same age range and using the same methods), successive birth cohorts, and incidence studies. Unfortunately, we were not able to identify such data at the present moment. Therefore, by conducting a meta-regression analysis with a large number of studies, we were able to hold constant the effect of methods and study location to estimate the effect of time. Second, because a substantial proportion of studies did not report years when the sample was assessed, we used year of publication as a proxy. However, because the implicit error in this proxy measure is in the same direction for all studies with a possible small variation among them, we understand that this may not have significantly affected the results. Third, although more studies were included in the present analysis, there are still substantially fewer studies in particular geographical locations, especially Africa and Oceania. More studies in these continents are needed. Fourth, we cannot exclude the possibility that other methodological characteristics not included in the model or not even reported by the studies would be associated with heterogeneity of results.
In spite of these limitations, our results have important implications. First, it is necessary to monitor rates of diagnosis and treatment of the disorder. Second, the stability of the prevalence rates estimated by standardized diagnostic procedures over time indicates that a potential increase of cultural pressure or social expectations over children has not driven an increase of real cases of ADHD across the past three decades. Third, study methods are consistently associated with heterogeneity of prevalence estimates, and further standardization across studies is necessary. Fourth, geographical location is not associated with variability of ADHD prevalence, which is consistent with the notion that cultural or social aspects are not implicated in the aetiology of the disorder.
This is the most comprehensive review on ADHD prevalence studies conducted to date. During the past three decades, prevalence estimates did not vary as a function of time. Increasing rates of diagnosis and treatment of ADHD are likely a reflection of increasing awareness, access to treatment or changing clinical practices. There is no evidence to suggest an increase in the number of children in the population who meet criteria for ADHD when standardized diagnostic procedures are followed.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This work was supported by the National Council for Scientific and Technological Development (CNPq) [Bolsa de Produtividade em Pesquisa to GVP, LAR], Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS) [Post-doctoral scholarships to G.A.S. and C.K.].
Conflicts of interest
G.V.P. has served as a speaker and/or consultant to Eli-Lilly, Novartis, Janssen-Cilag, and Shire Pharmaceuticals, developed educational material for Janssen-Cilag, received travel awards from Shire to take part in two scientific meetings, receives authorship royalties from Manole Editors and receives unrestricted research support from Novartis. E.W. and G.A.S. report no conflict of interest. C.K. took part in two meetings on ADHD sponsored by Novartis and Shire in 2010 and 2011 and in a meeting sponsored for journal editors by Deva in 2010. In the last 36 months, he has received royalties from publishers Artmed and Manole. L.A.R. was on the speakers’ bureau and/or acted as consultant for Eli-Lilly, Janssen-Cilag, Novartis and Shire in the past three years. He receives authorship royalties from Oxford Press and ArtMed. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by him receive unrestricted educational and research support from the following pharmaceutical companies in the past three years: Eli-Lilly, Janssen-Cilag, Novartis and Shire.
Supplementary Material
References
- 1.Biederman J, Faraone SV. Attention-deficit hyperactivity disorder. Lancet 2005;366:237–48. [DOI] [PubMed] [Google Scholar]
- 2.Swanson JM, Sergeant JA, Taylor E, Sonuga-Barke EJ, Jensen PS, Cantwell DP. Attention-deficit hyperactivity disorder and hyperkinetic disorder. Lancet 1998;351:429–33. [PubMed] [Google Scholar]
- 3.Singh I. Beyond polemics: science and ethics of ADHD. Nat Rev Neurosci 2008;9:957–64. [DOI] [PubMed] [Google Scholar]
- 4.Timimi S, Taylor E. ADHD is best understood as a cultural construct. Br J Psychiatry 2004;184:8–9. [DOI] [PubMed] [Google Scholar]
- 5.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007;164:942–48. [DOI] [PubMed] [Google Scholar]
- 6.Polanczyk G, Jensen P. Epidemiologic considerations in attention deficit hyperactivity disorder: a review and update. Child Adolesc Psychiatr Clin N Am 2008;17:245–60. [DOI] [PubMed] [Google Scholar]
- 7.Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 2012;9:490–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children – United States, 2003 and 2007. MMWR 2010;59: 1439–43. [PubMed] [Google Scholar]
- 9.Elsabbagh M, Divan G, Koh YJ, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res 2012;5:160–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fombonne E. Epidemiology of pervasive developmental disorders. Pediatr Res 2009;65:591–98. [DOI] [PubMed] [Google Scholar]
- 11.Raudenbush SW. Analyzing effect sizes: random-effects models. In: Cooper HM, Hedges LV, eds. The Handbook of Research Synthesis. New York: Russell Sage lFoundation, 2009. [Google Scholar]
- 12.Viechtbauer W. Conducting meta-analysis in R with the metafor package. Journal of Statistical Software 2010;36:1–48. [Google Scholar]
- 13.Viechtbauer W, Cheung MW-L. Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods 2010;1:112–25. [DOI] [PubMed] [Google Scholar]
- 14.Getahun D, Jacobsen SJ, Fassett MJ, Chen W, Demissie K, Rhoads GG. Recent trends in childhood attention-deficit/hyperactivity disorder. JAMA Pediatr 2013;167:167–68. [DOI] [PubMed] [Google Scholar]
- 15.Winterstein AG, Gerhard T, Shuster J, et al. Utilization of pharmacological treatment in youths with attention deficit/hyperactivity disorder in Medicaid database. Ann Pharmacother 2008;42:24–31. [DOI] [PubMed] [Google Scholar]
- 16.Robison LM, Skaer TL, Sclar DA, Galin RS. Is attention deficit hyperactivity disorder increasing among girls in the US? Trends in diagnosis and the prescribing of stimulants. CNS Drugs 2002;16:129–37. [DOI] [PubMed] [Google Scholar]
- 17.Robison LM, Sclar DA, Skaer TL, Galin RS. National trends in the prevalence of attention-deficit/hyperactivity disorder and the prescribing of methylphenidate among school-age children: 1990-1995. Clin Pediatr (Phila) 1999;38:209–17. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy S, Wilton L, Murray ML, Hodgkins P, Asherson P, Wong IC. The epidemiology of pharmacologically treated attention deficit hyperactivity disorder (ADHD) in children, adolescents and adults in UK primary care. BMC Pediatr 2012;12:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brault MC, Lacourse E. Prevalence of prescribed attention-deficit hyperactivity disorder medications and diagnosis among Canadian preschoolers and school-age children: 1994-2007. Can J Psychiatry 2012;57:93–101. [DOI] [PubMed] [Google Scholar]
- 20.Polanczyk G, Rohde LA, Szobot C, Schmitz M, Montiel-Nava C, Bauermeister JJ. ADHD treatment in Latin America and the Caribbean. J Am Acad Child Adolesc Psychiatry 2008;47:721–22. [DOI] [PubMed] [Google Scholar]
- 21.Mattos P, Rohde LA, Polanczyk GV. ADHD is undertreated in Brazil. Rev Bras Psiquiatr 2012;34:513–14. [DOI] [PubMed] [Google Scholar]
- 22.Polanczyk G, Rohde LA. Epidemiology of attention-deficit/hyperactivity disorder across the lifespan. Curr Opin Psychiatry 2007;20:386–92. [DOI] [PubMed] [Google Scholar]
- 23.Rohde LA, Szobot C, Polanczyk G, Schmitz M, Martins S, Tramontina S. Attention-deficit/hyperactivity disorder in a diverse culture: do research and clinical findings support the notion of a cultural construct for the disorder? Biol Psychiatry 2005;57:1436–41. [DOI] [PubMed] [Google Scholar]
- 24.Burns GL, de Moura MA, Walsh JA, Desmul C, Silpakit C, Sommers-Flanagan J. Invariance and convergent and discriminant validity between mothers' and fathers' ratings of oppositional defiant disorder toward adults, ADHD-HI, ADHD-IN, and academic competence factors within Brazilian, Thai, and American children. Psychol Assess 2008;20:121–30. [DOI] [PubMed] [Google Scholar]
- 25.Bauermeister JJ, Canino G, Polanczyk G, Rohde LA. ADHD across cultures: is there evidence for a bidimensional organization of symptoms? J Clin Child Adolesc Psychol 2010;39:362–72. [DOI] [PubMed] [Google Scholar]
- 26.Bronfenbrenner U, Ceci SJ. Nature-nurture reconceptualized in developmental perspective: a bioecological model. Psychol Rev 1994;101:568–86. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.