Abstract
Objective
To assess the coping strategies used by family decision makers of adult critical care patients during and after the critical care experience and the relationship of coping strategies to posttraumatic stress symptoms experienced 60 days after hospitalization.
Design
A single-group descriptive longitudinal correlational study.
Setting
Medical, surgical, and neurological ICUs in a large tertiary care university hospital.
Patients
Consecutive family decision makers of adult critical care patients from August 2012 to November 2013. Study inclusion occurred after the patient's fifth day in the ICU.
Interventions
None.
Measurements and Main Results
Family decision makers of incapacitated adult ICU patients completed the Brief COPE instrument assessing coping strategy use 5 days after ICU admission and 30 days after hospital discharge or death of the patient and completed the Impact of Event Scale-Revised assessing post-traumatic stress symptoms 60 days after hospital discharge. Seventy-seven family decision makers of the eligible 176 completed all data collection time points of this study. The use of problem-focused (p = 0.01) and emotion-focused (p < 0.01) coping decreased over time while avoidant coping (p = 0.20) use remained stable. Coping strategies 30 days after hospitalization (R2 = 0.50, p < 0.001) were better predictors of later posttraumatic stress symptoms than coping strategies 5 days after ICU admission (R2 = 0.30, p = 0.001) controlling for patient and decision-maker characteristics. The role of decision maker for a parent and patient death were the only noncoping predictors of post-traumatic stress symptoms. Avoidant coping use 30 days after hospitalization mediated the relationship between patient death and later posttraumatic stress symptom severity.
Conclusions
Coping strategy use is a significant predictor of posttraumatic stress symptom severity 60 days after hospitalization in family decision makers of ICU patients.
Keywords: acute posttraumatic stress disorder, coping behavior, decision making, family members, intensive care unit, intensive care unit burden
Some family members of critically ill patients experience tremendous psychological distress during the ICU experience (1–5). Lemiale et al (6) reported in a French cohort that 36% of ICU family members are taking anxiolytic or antidepressant drugs on discharge or death of their family member. In the months following the ICU experience, family members are at risk for ongoing psychological distress, including symptoms of generalized anxiety disorder, depression, panic disorder, posttraumatic stress disorder (PTSD), and complicated grief (7–12). Specifically, the prevalence and severity of PTSD symptoms in post-ICU family members have been increasingly recognized in the literature (7–10, 13–18).
Critically ill patients are often incapable of participating in their own medical decision making due to sedation, delirium, coma, or neurological compromise (19, 20). A majority of ICU patients rely on a substitute decision maker, usually a family decision maker (FDM), to participate in decision making with the healthcare providers at some point during their ICU illness (21). The risk of loss of a family member and the difficulty of making potentially life or death decisions may add to the anxiety and stress of FDMs. The high prevalence of PTSD symptoms following the ICU experience in FDMs of ICU patients compared with other family members may reflect these extreme threats (7, 8, 15).
The relationship of coping to psychological and physical health outcomes has been studied extensively in the behavioral literature (22). Incorporating the concepts of Lazarus and Folkman (23), researchers describe three categories of coping behavior: problem focused, emotion focused, and avoidant (24, 25). Avoidant coping has been shown to be a predictor of decreased psychological adjustment in individuals suffering from acute and chronic health problems and associated with PTSD symptoms following a traumatic event (26–30). The use of avoidant coping strategies also has been associated with increased emotional distress among neuroscience ICU family members and with higher risk of PTSD symptoms in mothers of premature neonatal ICU infants (31, 32).
The purposes of this study were to determine: 1) the coping strategies used by FDMs of ICU patients early in the ICU admission and 30 days following hospital discharge or death of the patient for whom the FDM made decisions and 2) the relationship between coping strategies used by FDMs during and after the decision-making experience and PTSD symptoms experienced by FDMs 60 days after hospital discharge or death of the patient for whom the FDM made decisions.
MATERIALS AND METHODS
Sample and Setting
The institutional review board of the study site approved this study. The current study was part of a larger National Institutes of Health-funded study (1RO1NR013322-01) examining decision making of ICU FDMs. The research setting included three adult ICUs at a large tertiary care center. The study inclusion criteria for ICU patients were 1) mechanical ventilation or predicted ICU stay of greater than 5 days, 2) lack of cognitive decisional capacity, 3) age more than 18 years, and 4) has an identified FDM. Exclusion criteria for ICU patients included: 1) able to make their own care decisions and 2) family meeting planned to discuss withdrawal of life-sustaining interventions for the patient or withdrawal in process. Study inclusion criteria for FDMs of ICU patients were 1) over 18 years, 2) identified as the primary person responsible for ICU patient decision making, and 3) able to speak English.
Design
The study design was a descriptive, longitudinal, correlational study to identify coping strategies and symptoms of PTSD in ICU FDMs and the extent of the relationship between FDM coping strategies and post-ICU PTSD symptoms. An FDM may be 1) a family member previously designated by the patient as the legal durable power of attorney, 2) a family member who was verbally chosen by the patient, but legal documentation does not exist, 3) a relative, or friend, who is available and assumes the role of decision maker, or 4) a legal guardian. A research assistant (RA) rounded in the ICUs on a daily basis to identify patients and FDMs eligible for the study. Enrollment and initial interviews were obtained at the bedside (all ICU rooms were single-patient rooms) or a nearby private room according to the preference of the FDM. When a patient met the eligibility criteria for the study but the FDM was not present at the patient's bedside, the RA explained the study to the potential participant by phone and either arranged a time to meet the participant face-to-face for enrollment or conducted the interview by phone.
The study design had three data collection points: Time 1 (T1) = day 3–5 after ICU admission, Time 2 (T2) = 30 days after discharge from the hospital or death of the patient, and Time 3 (T3) = 60 days after discharge or death of the patient. The demographic form was administered at T1. The Brief COPE instrument was administered at T1 and T2. The Impact of Event Scale-Revised (IES-R) was administered at T3. At 30 days after discharge from the hospital (T2), the FDM was contacted by phone call, e-mail, or standard mail. The same process was followed at 60 days after discharge from the hospital or death of the patient (T3). Bereaved family members contacted at T2 and T3 were encouraged to pursue local bereavement support groups. A $10.00 gift card was offered prior to enrollment in the study and again at T3 upon completion of all study time points to compensate FDMs for the inconvenience of participating in the study during a difficult and stressful time and to stimulate study participation.
Measurement
Demographic Form
Patient and FDM characteristics were obtained from the FDM and the patient's medical records. Patient characteristics included age, gender, ethnicity, length of ICU stay, length of hospital stay, and final disposition of the patient at 30 days (death or discharge from ICU). FDM characteristics included age, gender, ethnicity, relationship to the patient, previous decision-making experience, documentation of patient's living will, and designation of durable power of attorney.
Brief COPE Instrument
Coping strategy was measured at T1 and T2 by the Brief COPE instrument, which is a 28-item measure of coping strategies (33). The Brief COPE consists of 14 subscales of two items each. The items are scored using a 4-point Likert scale with responses ranging from 1 (I haven't been doing this at all) to 4 (I have been doing this a lot). Each of the 14 subscales can be reported as a total score (2–8) or a mean score (1–4) with higher scores indicating more use of the particular type of coping effort. Based on conceptual and theoretical literature, several authors group the 14 subscales into three coping categories or strategies: 1) problem-focused coping, 2) emotion-focused coping, and 3) avoidant coping (34–36). Each category score is reported as a mean score ranging from 1 to 4 (Table A1, Supplemental Digital Content 1, http://links.lww.com/CCM/B207). Several authors have reported on the psychometric properties of the Brief COPE subscales and coping categories (33–36) (Table A2, Supplemental Digital Content 1, http://links.lww.com/CCM/B207).
IES-R Symptoms of posttraumatic stress were measured by the IES-R
The IES-R is a self-report scale that provides information on both the presence and severity of stress-related symptoms. Horowitz et al (37) proposed the original IES, which was revised by Weiss and Marmar (38) to include three subscales corresponding to the three symptom clusters of PTSD described in the Diagnostic and Statistical Manual of Mental Disorders-IV: intrusion, avoidance, and hyperarousal (39). The IES-R is a 22-item instrument scored using a 5-point scale ranging from 0 (not at all) to 4 (extremely) for each item. Total scores may range from 0 to 88 with higher scores indicating higher levels of posttraumatic stress symptoms. Several authors have reported on the validity and reliability of the IES-R instrument (38, 40, 41).
Data Analysis
Descriptive statistics were used to assess frequencies and variability of the data. Nominal or ordinal variables were described using absolute n and proportions. Interval/ratio variables were described using means and sds. Bivariate associations were examined using Pearson correlations and chi-square analysis. Differences between groups were examined using dependent samples t tests, two sample t tests, and one-way analysis of variance (ANOVA). Individual-level change over time was examined using raw data change scores. Change scores for the coping strategies were derived by subtracting T1 scores from T2 scores with positive values indicating an increase in use over time and negative values indicating a decrease in use over time. Reliable Change Indices (RCI) were used to assess the statistical significance of individual-level change in variables over time. RCI was calculated as the difference between T2 and T1 scores divided by the se of the difference in scores between time points (42). RCI scores greater than 1.96 or less than –1.96 indicate a statistically significant change in scores over time (p < 0.05). Associations between demographic variables, coping strategies, and PTSD symptoms were evaluated using multiple regression models, after confirming that the data met test assumptions. Two-sided p values of less than 0.05 were considered statistically significant. Data were analyzed using the Statistics Package for the Social Sciences (SPSS; IBM, Armonk, NY) version 21 software. The sample size was determined on G-Power (3.13) a priori. Based on an α of 0.05 and power of 0.80, 76 FDMs were planned for the study assuming a medium effect size (0.15) for regression of the dependent variable (PTSD symptoms) on the three independent variables (coping strategies). A medium effect size was chosen based on previous studies examining the relationship between coping strategies and PTSD symptoms. Assuming an attrition rate of 20%, a total of 96 FDMs were required to obtain the calculated sample size of 76.
RESULTS
Characteristics of Patients and FDMs
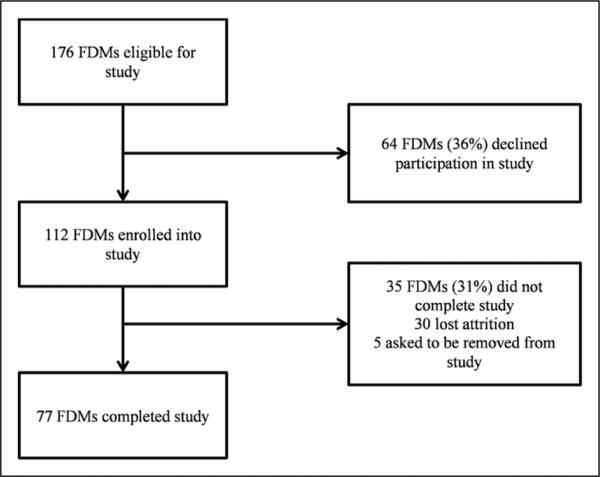
Over the study period from August 2012 to September 2013, a total of 176 FDMs and patients met the eligibility criteria and were approached to participate in the study. Seventy-seven FDMs provided data for all study time points and completed the study. Figure 1 is the flow chart of the study. Individuals completing the study tended to be older than individuals lost to attrition (M = 57.01, sd = 13.82; M = 49.53, sd = 13.16; t (105) = –2.55, p = 0.01). The presence of a living will [X2 (1) = 4.08, p = 0.04] and durable power of attorney [X2 (1) = 4.08, p = 0.04] was higher in the sample completing the study. The proportion of African-American FDMs in the attrition group was higher than the sample group approaching statistical significance (p = 0.09) (Table A3, Supplemental Digital Content 1, http://links.lww.com/CCM/B207). The demographic characteristics of the hospitalized ICU patients and their FDMs are summarized in Table 1. The ICU mortality rate was 30%, which increased to 43% by 30 days after hospital discharge.
Figure 1.
Flow chart of the study. FDM = family decision maker.
Table 1.
Patient and Family Decision-Maker Characteristics
| Patient characteristics | |
| Age, yr, mean (range) | 61.7 (23-86) |
| Gender, n (%) | |
| Female | 37 (48.1) |
| Male | 40 (51.9) |
| Ethnicity, n (%) | |
| African-American | 20 (26) |
| White | 57 (74) |
| Length of ICU stay, d, mean (range) | 13.4 (3-63) |
| Length of hospital stay, d, mean (range) | 19.4 (3-78) |
| Disposition at 30 d post hospital discharge, n (%) | |
| Deceased | 33 (43.9) |
| Facility | 32 (41.6) |
| Home | 12 (15.6) |
| Family decision maker characteristics | |
| Age, yr, mean (range) | 57.0 (21-86) |
| Gender, n (%) | |
| Female | 61 (79.2) |
| Male | 16 (20.8) |
| Ethnicity, n (%) | |
| African-American | 21 (27.4) |
| Latino | 1 (1.3) |
| White | 55 (71.4) |
| Relationship to patient, n (%) | |
| Spouse | 36 (46.8) |
| Child | 22 (28.6) |
| Parent | 9 (11.7) |
| Other | 10 (13) |
| Previous decision-making experience, yes, n (%) | 49 (63.6) |
| Living will, yes, n (%) | 27 (35.1) |
| Durable power of attorney, yes, n (%) | 28 (36.4) |
Posttraumatic Stress Symptoms
The mean IES-R score for the sample was 23.14 sd = 15.90). Eighteen FDMs (23%) had IES-R scores above 33, and 32 FDMs (42%) had scores above 24. The IES-R score differed among FDMs based on the disposition of the patient at 30 days (deceased: M = 29.70, sd = 15.83; alive: M = 18.23, sd = 14.23; t (75) = –3.34, p = 0.001). The IES-R score also varied according to the relationship of the FDM to the patient [F (3, 73) = 2.96, p = 0.04] with children of ICU patients having the highest IES-R scores (M = 29.18, sd = 16.04) and other FDMs (siblings, power of attorney, etc.) having the lowest IES-R scores (M = 11.44, sd = 7.38). The difference in the mean scores between these two groups was statistically significant using one-way ANOVA with post hoc testing (p < 0.05). The IES-R scores of spouses (M = 22.11, sd = 15.06) and parents (M = 24.10, sd = 19.31) were not statistically different from each other or the other relationship categories. No other differences were noted in IES-R score among the patient and FDM characteristics.
FDM Coping Strategies and Posttraumatic Stress Symptoms
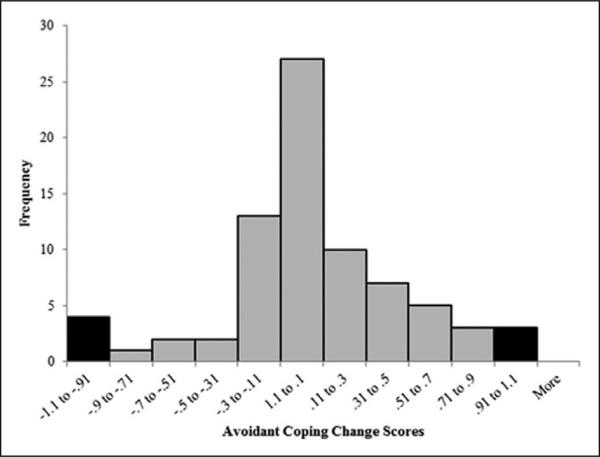
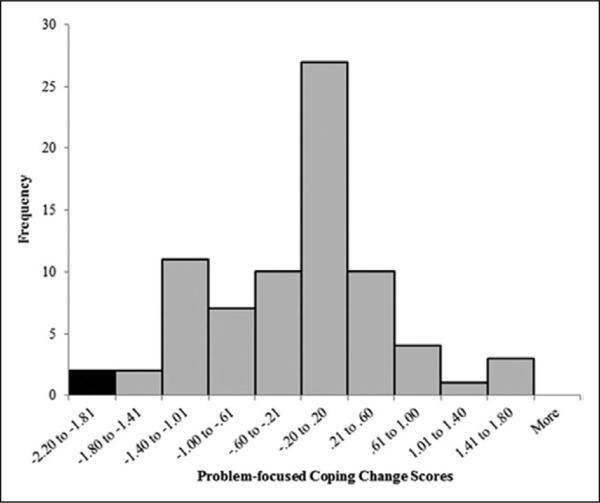
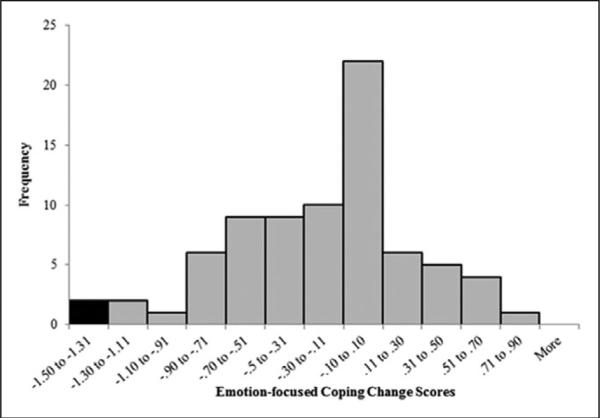
Problem-focused coping scores were highest among the three coping strategies at enrollment and 30 days after hospital discharge as shown in Table 2. Group problem-focused and emotion-focused coping mean scores decreased significantly over time while avoidant coping scores remained statistically unchanged from enrollment to 30 days after hospital discharge. Change scores for the coping strategies demonstrated moderate variation (Figs. 2, 3, and 4). RCI revealed four participants (5%) had a statistically significant decrease in avoidant coping use between T1 and T2, and three individuals (4%) experienced a significant increase over time (RCI < 1.96 and RCI > 1.96, respectively, p < 0.05). Two FDMs (3%) demonstrated a statistically significant decrease in problem-focused coping over time and two participants (3%) reported a decrease in emotion-focused coping use from T1 to T2 based on RCI analysis with no individuals endorsing a significant increase in either coping strategy. Female FDMs used higher amounts of avoidant coping at enrollment (T1) than men (female: M = 1.60, sd = 0.33; male: M = 1.37, sd = 0.37; p = 0.02), but the difference was no longer detected at 30 days following hospital discharge (female: M = 1.63, sd = 0.44; male: M = 1.56, sd = 0.51; p = ns). No other differences in the use of coping strategies were found among FDM characteristics.
Table 2.
Coping Strategies Used by Family Decision Makers and Comparison Over Time
| Coping Strategy | T1 Mean (sd) | T2 Mean (sd) | Test t (76) | p |
|---|---|---|---|---|
| Avoidant | 1.55 (0.34) | 1.61 (0.46) | 1.29 | 0.20 |
| Emotion focused | 2.82 (0.45) | 2.66 (0.53) | 2.98 | 0.00 |
| Problem focused | 3.10 (0.74) | 2.88 (0.72) | 2.53 | 0.01 |
T1 = enrollment, sd = sd of mean Brief COPE scores, T2 = 30 d after hospital discharge or death.
Figure 2.
Distribution of avoidant coping change scores. Black bars indicate Reliable Change Index of < –1.96 or > 1.96 (p < 0.05).
Figure 3.
Distribution of problem-focused coping change scores. Black bars indicate Reliable Change Index of < –1.96 (p < 0.05).
Figure 4.
Distribution of emotion-focused coping change scores. Black bars indicate Reliable Change Index of < –1.96 (p < 0.05).
At enrollment (T1), all of the coping strategies demonstrated moderate correlations with each other but avoidant coping was the only strategy to have a significant positive relationship with IES-R score (r = 0.27, p < 0.01) (Table A4, Supplemental Digital Content 1, http://links.lww.com/CCM/B207). Coping strategies 30 days following hospital discharge (T2) continued to exhibit significant positive correlations with each other and all three coping strategies demonstrated a positive relationship with IES-R score (avoidant coping: r = 0.60; emotion-focused coping: r = 0.23; problem-focused coping: r = 0.38; p < 0.05). Furthermore, longitudinal correlations between the coping strategies at T1 and T2 demonstrated moderately positive correlations within a particular type of coping strategy but weaker positive correlations between different T1 and T2 coping strategies (Table A4, Supplemental Digital Content 1, http://links.lww.com/CCM/B207). Additionally, T1 problem-focused coping had no significant relationship to T2 avoidant coping (r = 0.08, p > 0.05).
Predictors of PTSD Symptom Severity
A stepwise regression model identified avoidant coping change score, problem-focused coping change score, patient death, and the child FDM role as significant predictors of higher IES-R scores (Table 3). Parents serving as FDM for their children approached statistical significance (B = 7.83, p = 0.09). The model was moderately strong in predicting severity of later PTSD symptoms accounting for 40% of the variance in IES-R score [F (6, 70) = 14.05; p = 0.000].
Table 3.
Predictors of Impact of Event Scale-Revised Score (Stepwise Regression Model)
| Model | B | se | β | t | p |
|---|---|---|---|---|---|
| Constant | 15.51 | 2.35 | – | 6.61 | 0.00 |
| Avoidant coping change score | 9.42 | 3.64 | 0.26 | 2.59 | 0.01 |
| Problem-focused coping change score | 7.89 | 1.95 | 0.38 | 4.04 | 0.00 |
| Relationship child vs spouse | 11.77 | 3.23 | 0.34 | 3.65 | 0.00 |
| Relationship parent vs spouse | 7.83 | 4.50 | 0.17 | 1.74 | 0.09 |
| Patient death at 30 d | 10.21 | 3.20 | 0.32 | 3.20 | 0.00 |
Dependent variable = Impact of Event Scale-Revised score, Model summary: R2 = 0.40; F (7,69) = 11.31, p < 0.001.
T1 coping strategies were poor predictors of IES-R score with an R2 of 0.09, F (3, 73) = 2.35, and p = 0.08. When the variables of FDM relationship to patient and patient outcome (deceased/alive) identified in the stepwise regression were added, the model provided a statistically significant explanation of IES-R score variance [F (7,69) = 4.14, p = 0.001] with patient death being the only independent predictor of higher posttraumatic stress symptom severity (Table A5, Supplemental Digital Content 1, http://links.lww.com/CCM/B207). In contrast, T2 coping strategy use did explain a statistically significant amount of the variance in IES-R score [F (3, 73) = 19.41, p < 0.001, R2 = 0.44]. When patient outcome and FDM relationship to patient were added, the variance in IES-R score explained by the model increased slightly (R2 = 0.50). Avoidant coping and problem-focused coping at T2 were independent predictors of higher IES-R score, whereas death of the patient was no longer a significant independent predictor of IES-R score (Table A6, Supplemental Digital Content 1, http://links.lww.com/CCM/B207).
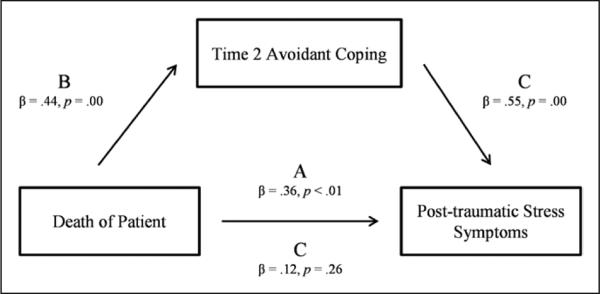
Having identified that T2 avoidant and problem-focused coping were significant predictors of PTSD symptom severity, we then tested whether these coping strategies mediated the relationship between patient death and later PTSD symptoms. Using the method described by Baron and Kenny (43), we tested path A (Fig. 5), demonstrating a significant relationship between death of the patient and IES-R score. In path B, we performed regression analysis between patient death with T2 avoidant coping and T2 problem-focused coping. Patient death was a significant predictor of T2 avoidant coping but not of T2 problem-focused coping (β = 0.03, p = 0.77). To complete the test for mediation, IES-R score was regressed on avoidant coping and patient death shown in path C, demonstrating a mediating effect of avoidant coping between patient death and PTSD symptoms.
Figure 5.
Mediation by T2 avoidant coping between patient death and posttraumatic stress disorder symptoms.
DISCUSSION
The findings of the current study corroborate those of other investigators concerning the high prevalence of PTSD symptoms in FDMs of critically ill patients. Using the data and recommendations published by Creamer et al (40), 23% of FDMs had IES-R scores highly predictive of PTSD (IES-R > 33) and 42% had scores that demonstrate clinically significant symptoms of PTSD (IES-R > 24). Several investigators have reported PTSD symptom prevalence rates ranging from 33% to 69% within the first 6 months after ICU hospitalization (7–10, 13–18). However, comparison between studies is difficult due to differences in sample populations, instruments used to measure PTSD symptoms, timing of symptom measurement, and analysis of instrument score.
Our study examined PTSD symptoms exclusively in FDMs. The sample of FDMs was predominantly female, Caucasian, and spouses similar to other studies (7, 9, 16). The FDM role has been associated with a higher prevalence of PTSD symptoms in French populations (8, 15). However, this relationship is less clear in other ICU family populations. Some studies investigating post-ICU family PTSD symptoms do not differentiate between family members who did or did not participate in the decision-making process (9, 10, 14, 17, 18). Gries et al (9) reported that discordance between decision-making preferences and actual decision-making role was associated with increased PTSD symptoms, and thus, the impact of the role of FDM may be a significant risk factor.
We found patient outcome and relationship of the FDM to the patient as the only noncoping patient or FDM variables with a statistically significant association with severity of PTSD symptoms. Azoulay et al (8) also reported an association between patient death and PTSD symptoms. Our study also found that FDMs who were children of the patient had higher IES-R scores than other FDMs. Azoulay et al (8) reported a higher prevalence of PTSD symptoms among adult children of ICU patients. However, given the largely disparate findings in other studies, a firm association between the FDM-patient relationship and PTSD symptoms is elusive (9, 18). Furthermore, FDM gender was not significantly associated with PTSD symptom prevalence or severity in the present study as has been demonstrated by other authors and in other PTSD patient populations (8, 9, 44). However, the majority of FDMs in this study were female, which may have limited the ability to demonstrate a relationship between gender and PTSD symptoms.
The study also presents new data on the coping strategies used by ICU FDMs during and after the ICU experience. FDMs used all three coping strategies to varying degrees during the study period. The use of problem-focused coping was highest at both time points followed by emotion-focused with avoidant coping being the least utilized (2, 45–47). FDMs may become more comfortable with the ICU environment and rely less on problem and emotion-focused coping strategies over time, possibly influenced by improvement in their family member's condition. Alternatively, problem and emotion-focused coping may be insufficient or ineffective to meet the stress demands of the ICU illness resulting in persistent use of avoidant coping over time, which may explain the decrease in the use of problem, and emotion-focused strategies over time while use of avoidant coping remained stable. However, FDMs did not demonstrate significant propensity to change from the use of one coping strategy in favor of another. Additionally, the relationship between coping strategy use and PTSD symptoms severity increased over time. These findings suggest a subset of FDMs continued to use sustained or higher levels of coping strategies and those who used higher levels of coping strategies (avoidant and problem-focused coping) over time also tended to be the FDMs experiencing higher amounts of PTSD symptoms.
Positive associations between coping strategies and PTSD symptoms have been described in other PTSD populations with avoidant coping having the strongest positive association with PTSD symptoms (26, 27, 36, 48, 49). Some authors have presumed the presence of PTSD symptoms causes the use of avoidant coping (36, 50). However, other authors have reported avoidant coping as a predictor of later PTSD symptoms in populations of Gulf War victims, domestic violence victims, and traumatic injury victims (51–53). A recent study measured coping strategy in 56 mothers of premature infants in the neonatal ICU (31). Mothers were assessed with the Brief COPE at 7–10 days after ICU admission and the Davidson Trauma Scale 1 month after ICU discharge. Avoidant coping use was associated with an increased risk of later PTSD symptoms (RR = 1.09; 95% CI, 1.02–1.15; p = 0.008).
Our findings suggest that the relationship between coping strategies and PTSD symptoms in our sample arises during and after the ICU hospitalization rather than as an early antecedent predictor of PTSD symptoms. The presumably high stress of the ICU experience, influenced in part by the outcome of the patient, mobilizes coping strategies. The use of avoidant coping in response to ongoing ICU and post-ICU stressors may play a role in sustaining and accelerating PTSD symptom severity as has been shown in other traumatic stress populations (27, 51, 53). Problem-focused coping has been associated with negative psychological health outcomes from acute stress-ors but positive health outcomes with chronic stressors, suggesting psychological difficulty in the short term but improved psychological adjustment in the long term (22, 26, 36). Since patient death did not have a significant association with T2 problem-focused coping, use of problem-focused coping may have been related to other factors in the ICU and post-ICU course. Discharge of the patient from the ICU or hospital may represent a new stress environment where problem-focused coping is often used at higher levels than other coping strategies. The uncontrollability and unpredictability of the ICU and post-ICU course may overwhelm FDMs who preferentially use problem-focused coping strategies, resulting in higher PTSD symptomatology.
Our study had several limitations. First, the study sample was small and relatively homogeneous. Second, the sample may be biased in that refusal rates and attrition were high. It is possible that FDMs who used higher rates of early avoidant coping declined participation of the study. Furthermore, FDMs experiencing the highest degree of PTSD symptoms may have been lost due to attrition. Furthermore, baseline coping use by FDMs prior to ICU admission is not accounted for in the analysis. Prior psychiatric history of ICU FDMs was not obtained in the current study. Previous history of anxiety or depression is a risk factor for PTSD and could be a significant confounding variable in the analysis of the current study (44). Data were collected from FDMs in several different types of ICU, which introduces the possibility of specific ICU factors influencing the results. Fourth, the study relied on self-report measures to assess PTSD and coping strategies. The IES-R instrument does not make the diagnosis of PTSD but identifies the severity of PTSD symptoms experienced. Future studies with ICU family members may benefit from a formal clinician administered examination for PTSD.
CONCLUSIONS
The relationship between coping strategy and PTSD symptoms is important for several reasons. It may provide a mechanism that helps to explain the effect of FDM and ICU variables on subsequent development of PTSD symptoms. Second, it may provide an opportunity for focused interventions that target maladaptive coping strategies to diminish later PTSD symptoms. Coping strategies are amenable to treatment interventions, and interventions to diminish avoidant coping use have been associated with reductions in PTSD symptoms (54–56). Replication of the study findings in a larger more heterogeneous population would be helpful to examine the extent to which coping strategies may influence weaker relationships that our study did not identify between risk factors and PTSD symptom development. A larger study would also allow further psychometric testing of the Brief COPE in the ICU family population. Finally, longitudinal studies with later post-ICU time points are needed to determine whether the relationships between coping strategies and PTSD symptoms persist.
Supplementary Material
Acknowledgments
Dr. Petrinec received support for article research from the National Institutes of Health (NIH). Her institution received grant support (5NR01NR013322). Dr. Mazanec consulted for End-of-Life Nursing Education Consortium (receives an honorarium for teaching as a faculty member of the national ELNEC); received grant support from Cleveland Veterans Administration Medical Center (is the education/research coordinator on a specialty care cancer grant at the Veterans Administration); disclosed other relationships; received support for article research from the NIH, Wellcome Trust, Howard Hughes Medical Institute, and other; and disclosed work for hire and government work. Dr. Burant consulted for Analysis of Moment Structures Beta Tester, lectured for the Preconference Midwest Nursing Research Society Workshop 2014, and received support for article research from the NIH. His institution received grant support for Mapping the Complexity of End of Life Transitions in Chronically Critically Ill, CD4+ T and for B cell mechanisms of influenza vaccine nonresponsiveness in older adults (1 R01 AI 108972-01 NIH/National Institute of Allergy and Infectious Diseases). His institution received other support (International Psychogeriatric Association, work at VA Geriatric Research Education and Clinical Centers and VA project, “Chronic Renal Disease [CK] Advanced Practice Registered Nurse [APRN]–RN Care Management Support Team Pilot” an operational project supporting the strategic plan for the Chief Officer of Nursing in the Office of Nursing Services in FY2014–2015 and R01 NR013322-02). Dr. Daly is currently receiving a grant (#1RO1NR013322-01) from the NIH, which was the sole funding source for this study, and is employed by Case Western Reserve University (Faculty of CWRU). Her institution received grant support from National Institute of Nursing Research (5NR01NR013322 and a pending NINR grant).
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website (http://journals.lww.com/ccmjournal).
Dr. Hoffer has disclosed that he does not have any potential conflicts of interest.
REFERENCES
- 1.Auerbach SM, Kiesler DJ, Wartella J, et al. Optimism, satisfaction with needs met, interpersonal perceptions of the healthcare team, and emotional distress in patients’ family members during critical care hospitalization. Am J Crit Care. 2005;14:202–210. [PubMed] [Google Scholar]
- 2.Chui WY, Chan SW. Stress and coping of Hong Kong Chinese family members during a critical illness. J Clin Nurs. 2007;16:372–381. doi: 10.1111/j.1365-2702.2005.01461.x. [DOI] [PubMed] [Google Scholar]
- 3.McAdam JL, Dracup KA, White DB, et al. Symptom experiences of family members of intensive care unit patients at high risk for dying. Crit Care Med. 2010;38:1078–1085. doi: 10.1097/CCM.0b013e3181cf6d94. [DOI] [PubMed] [Google Scholar]
- 4.Paparrigopoulos T, Melissaki A, Efthymiou A, et al. Short-term psychological impact on family members of intensive care unit patients. J Psychosom Res. 2006;61:719–722. doi: 10.1016/j.jpsychores.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Pielmaier L, Walder B, Rebetez MM, et al. Post-traumatic stress symptoms in relatives in the first weeks after severe traumatic brain injury. Brain Inj. 2011;25:259–265. doi: 10.3109/02699052.2010.542429. [DOI] [PubMed] [Google Scholar]
- 6.Lemiale V, Kentish-Barnes N, Chaize M, et al. Health-related quality of life in family members of intensive care unit patients. J Palliat Med. 2010;13:1131–1137. doi: 10.1089/jpm.2010.0109. [DOI] [PubMed] [Google Scholar]
- 7.Anderson WG, Arnold RM, Angus DC, et al. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008;23:1871–1876. doi: 10.1007/s11606-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azoulay E, Pochard F, Kentish-Barnes N, et al. FAMIREA Study Group: Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171:987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 9.Gries CJ, Engelberg RA, Kross EK, et al. Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest. 2010;137:280–287. doi: 10.1378/chest.09-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones C, Skirrow P, Griffiths RD, et al. Post-traumatic stress disorder-related symptoms in relatives of patients following intensive care. Intensive Care Med. 2004;30:456–460. doi: 10.1007/s00134-003-2149-5. [DOI] [PubMed] [Google Scholar]
- 11.Kross EK, Engelberg RA, Gries CJ, et al. ICU care associated with symptoms of depression and posttraumatic stress disorder among family members of patients who die in the ICU. Chest. 2011;139:795–801. doi: 10.1378/chest.10-0652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siegel MD, Hayes E, Vanderwerker LC, et al. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med. 2008;36:1722–1728. doi: 10.1097/CCM.0b013e318174da72. [DOI] [PubMed] [Google Scholar]
- 13.Garrouste-Orgeas M, Coquet I, Périer A, et al. Impact of an intensive care unit diary on psychological distress in patients and relatives. Crit Care Med. 2012;40:2033–2040. doi: 10.1097/CCM.0b013e31824e1b43. [DOI] [PubMed] [Google Scholar]
- 14.Jones C, Bäckman C, Griffiths RD. Intensive care diaries and relatives’ symptoms of posttraumatic stress disorder after critical illness: A pilot study. Am J Crit Care. 2012;21:172–176. doi: 10.4037/ajcc2012569. [DOI] [PubMed] [Google Scholar]
- 15.Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356:469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 16.McAdam JL, Fontaine DK, White DB, et al. Psychological symptoms of family members of high-risk intensive care unit patients. Am J Crit Care. 2012;21:386–393. doi: 10.4037/ajcc2012582. quiz 394. [DOI] [PubMed] [Google Scholar]
- 17.Pillai L, Ambike D, Husainy S, et al. The prevalence of post-traumatic stress disorder symptoms in relatives of severe trauma patients admitted to the intensive care unit. Indian J Crit Care Med. 2006;10:181–186. [Google Scholar]
- 18.Pillai L, Aigalikar S, Vishwasrao SM, et al. Can we predict intensive care relatives at risk for posttraumatic stress disorder? Indian J Crit Care Med. 2010;14:83–87. doi: 10.4103/0972-5229.68221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: Validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 20.McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: Occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51:591–598. doi: 10.1034/j.1600-0579.2003.00201.x. [DOI] [PubMed] [Google Scholar]
- 21.Prendergast TJ, Claessens MT, Luce JM. A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med. 1998;158:1163–1167. doi: 10.1164/ajrccm.158.4.9801108. [DOI] [PubMed] [Google Scholar]
- 22.Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: A meta-analytic review. J Behav Med. 2002;25:551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- 23.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer; New York, NY: 1984. [Google Scholar]
- 24.Ben-Zur H. Coping, distress, and life events in a community sample. Int J Stress Manage. 2005;12:188–196. [Google Scholar]
- 25.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 26.Glass K, Flory K, Hankin BL, et al. Are coping strategies, social support, and hope associated with psychological distress among hurricane Katrina survivors? J Soc Clin Psychol. 2009;28:779–795. [Google Scholar]
- 27.Krause ED, Kaltman S, Goodman LA, et al. Avoidant coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. J Trauma Stress. 2008;21:83–90. doi: 10.1002/jts.20288. [DOI] [PubMed] [Google Scholar]
- 28.Smith NG, Tarakeshwar N, Hansen NB, et al. Coping mediates outcome following a randomized group intervention for HIV-positive bereaved individuals. J Clin Psychol. 2009;65:319–335. doi: 10.1002/jclp.20547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psychooncology. 2002;11:93–102. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- 30.Ullman SE, Townsend SM, Filipas HH, et al. Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychol Women Q. 2007;31:23–37. [Google Scholar]
- 31.Shaw RJ, Bernard RS, Storfer-Isser A, et al. Parental coping in the neonatal intensive care unit. J Clin Psychol Med Settings. 2013;20:135–142. doi: 10.1007/s10880-012-9328-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wartella JE, Auerbach SM, Ward KR. Emotional distress, coping and adjustment in family members of neuroscience intensive care unit patients. J Psychosom Res. 2009;66:503–509. doi: 10.1016/j.jpsychores.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 33.Carver CS. You want to measure coping but your protocol's too long: Consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 34.Coolidge FL, Segal DL, Hook JN, et al. Personality disorders and coping among anxious older adults. J Anxiety Disord. 2000;14:157–172. doi: 10.1016/s0887-6185(99)00046-8. [DOI] [PubMed] [Google Scholar]
- 35.Cooper C, Katona C, Livingston G. Validity and reliability of the brief COPE in carers of people with dementia: The LASER-AD Study. J Nerv Ment Dis. 2008;196:838–843. doi: 10.1097/NMD.0b013e31818b504c. [DOI] [PubMed] [Google Scholar]
- 36.Schnider KR, Elhai JD, Gray MJ. Coping style use predicts post-traumatic stress and complicated grief symptom severity among college students reporting a traumatic loss. J Couns Psychol. 2007;54:344–350. [Google Scholar]
- 37.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Weiss DS, Marmar CR. The impact of event scale-revised. In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma and PTSD. Guilford; New York, NY: 1997. pp. 399–411. [Google Scholar]
- 39.American Psychiatric Association . DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders. Text Revision American Psychiatric Association; 2000. [Google Scholar]
- 40.Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale-Revised. Behav Res Ther. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 41.Beck JG, Grant DM, Read JP, et al. The Impact of Event Scale-Revised: Psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord. 2008;22:187–198. doi: 10.1016/j.janxdis.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 43.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 44.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- 45.Braun UK, Beyth RJ, Ford ME, et al. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med. 2008;23:267–274. doi: 10.1007/s11606-007-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vig EK, Starks H, Taylor JS, et al. Surviving surrogate decision-making: What helps and hampers the experience of making medical decisions for others. J Gen Intern Med. 2007;22:1274–1279. doi: 10.1007/s11606-007-0252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agård AS, Harder I. Relatives’ experiences in intensive care–finding a place in a world of uncertainty. Intensive Crit Care Nurs. 2007;23:170–177. doi: 10.1016/j.iccn.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 48.Oflaz F, Hatipoğlu S, Aydin H. Effectiveness of psychoeducation intervention on post-traumatic stress disorder and coping styles of earthquake survivors. J Clin Nurs. 2008;17:677–687. doi: 10.1111/j.1365-2702.2007.02047.x. [DOI] [PubMed] [Google Scholar]
- 49.Pacella ML, Irish L, Ostrowski SA, et al. Avoidant coping as a mediator between peritraumatic dissociation and posttraumatic stress disorder symptoms. J Trauma Stress. 2011;24:317–325. doi: 10.1002/jts.20641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Coyne JC, Racioppo MW. Never the Twain shall meet? Closing the gap between coping research and clinical intervention research. Am Psychol. 2000;55:655–664. doi: 10.1037//0003-066x.55.6.655. [DOI] [PubMed] [Google Scholar]
- 51.Benotsch EG, Brailey K, Vasterling JJ, et al. War zone stress, personal and environmental resources, and PTSD symptoms in Gulf War veterans: A longitudinal perspective. J Abnorm Psychol. 2000;109:205–213. [PubMed] [Google Scholar]
- 52.Mellman TA, David D, Bustamante V, et al. Predictors of post-traumatic stress disorder following severe injury. Depress Anxiety. 2001;14:226–231. doi: 10.1002/da.1071. [DOI] [PubMed] [Google Scholar]
- 53.Sharkansky EJ, King DW, King LA, et al. Coping with Gulf War combat stress: Mediating and moderating effects. J Abnorm Psychol. 2000;109:188–197. [PubMed] [Google Scholar]
- 54.Butler AC, Chapman JE, Forman EM, et al. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 55.Sikkema KJ, Ranby KW, Meade CS, et al. Reductions in traumatic stress following a coping intervention were mediated by decreases in avoidant coping for people living with HIV/AIDS and childhood sexual abuse. J Consult Clin Psychol. 2013;81:274–283. doi: 10.1037/a0030144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zayfert C, Becker CB. Cognitive-Behavioral Therapy for PTSD: A Case Formulation Approach. Guilford Press; 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.