Abstract
Objective
To determine the diagnostic performance of standing computerized tomography (SCT) of the knee for osteophytes and subchondral cysts compared to fixed-flexion radiography, using magnetic resonance imaging (MRI) as the reference standard.
Methods
Twenty participants were recruited from the Multicenter Osteoarthritis Study (MOST). Participants' knees were imaged with SCT while standing in a knee-positioning frame, and with PA fixed-flexion radiography and 1T MRI. Medial and lateral marginal osteophytes and subchondral cysts were scored on bilateral radiographs and coronal SCT images using the OARSI grading system and on coronal MRI using Whole Organ MRI Scoring (WORMS). Imaging modalities were read separately with images in random order. Sensitivity, specificity, and accuracy for the detection of lesions were calculated and differences between modalities were tested using McNemar's test.
Results
Participants' mean age was 66.8 years, BMI was 29.6kg/m2 and 50% were women. Of the 160 surfaces (medial and lateral femur and tibia for 40 knees), MRI revealed 84 osteophytes and 10 subchondral cysts. In comparison with osteophytes and subchondral cysts detected by MRI, SCT was significantly more sensitive (93% and 100%; p<0.004) and accurate (95% and 99%; p<0.001 for osteophytes) than plain radiographs (sensitivity: 60% and 10% and accuracy 79% and 94% respectively). For osteophytes, differences in sensitivity and accuracy were greatest at the medial femur (p=0.002).
Conclusions
In comparison with MRI, SCT imaging was more sensitive and accurate for detection of osteophytes and subchondral cysts than conventional fixed-flexion radiography. Additional study is warranted to assess diagnostic performance of SCT measures of joint space width, progression of OA features and the patellofemoral joint.
Keywords: joint loading, biomechanics, osteoarthritis, bone marrow lesions, cartilage loss, knee, weight bearing, Cone Beam Computed Tomography
Introduction
Osteoarthritis (OA) affects over 27 million Americans and is the most prevalent musculoskeletal disease in US adults, resulting in significant mobility limitations[1, 2] and expenditures.[3] The knee is the most commonly affected weight-bearing joint, with 9.3 million US adults suffering from symptomatic knee OA.[1] Despite the high prevalence, knee OA is not readily diagnosed in a sensitive manner. Conventional radiographs have demonstrated poor concurrent validity for features of knee OA compared to both arthroscopy and MRI.[4-7] Some of the reasons for these poor correlations with joint structural damage include the two-dimensional projection of 3D anatomy by radiographs limiting visualization of overlapping structures and poor reproducibility of joint positioning causing imprecision in joint measurements.[7]
Many studies have demonstrated the insensitivity and inaccuracy of radiographs for knee OA features. For example, recent studies have demonstrated that, of knees completely free of radiographic tibiofemoral OA (Kellgren Lawrence grade 0), osteophytes were present in 74% by MRI.[5] Furthermore, direct arthroscopic visualization of knees graded as “completely normal” by radiographs frequently have severe OA (false negatives).[4] Subchondral cysts are fluid-filled cavities that are found in association with OA, but radiographs have been found to miss in a significant number of cases.[8] This insensitivity of radiographs limits the ability both to diagnose and to study this disease, which is defined by the presence of definite osteophytes.[6] As radiographs are the most common means of diagnosing knee OA, failure to detect osteophytes results in underestimation of its prevalence as well as misclassification of knees in clinical studies.
Given the poor sensitivity of the standard diagnostic test for knee OA, there is a compelling need for a more sensitive diagnostic imaging. Due to the need to simultaneously assess for osteophytes in order to diagnose the disease, as well as to assess joint space narrowing and potentially also predict future disease worsening,[9, 10] which can only be assessed while weight bearing, it would be useful if more sensitive diagnostic imaging for bony features of OA also could be completed while weight bearing.
Standing cone-beam CT (SCT) imaging of the knee may provide higher sensitivity and accuracy without significantly increasing the radiation dose, time or cost over conventional radiography. The major advantage of replacing knee radiographs with SCT for evaluation of knee OA is the ability to obtain a three-dimensional (3D) representation of the tibiofemoral and patellofemoral joints in their respective optimal planes using multiplanar reconstructions from a single acquisition. It also allows visualization of areas of the joint surface affected by disease that are poorly seen or not visible on 2D radiographs, thus potentially providing enhanced sensitivity for detection of structural effects of knee OA. Thus, we assessed the diagnostic performance of a proof-of-concept SCT scanner for knee osteophytes and subchondral cysts, compared to fixed-flexion radiography, using MRI as the reference standard.
Materials and Methods
Subjects
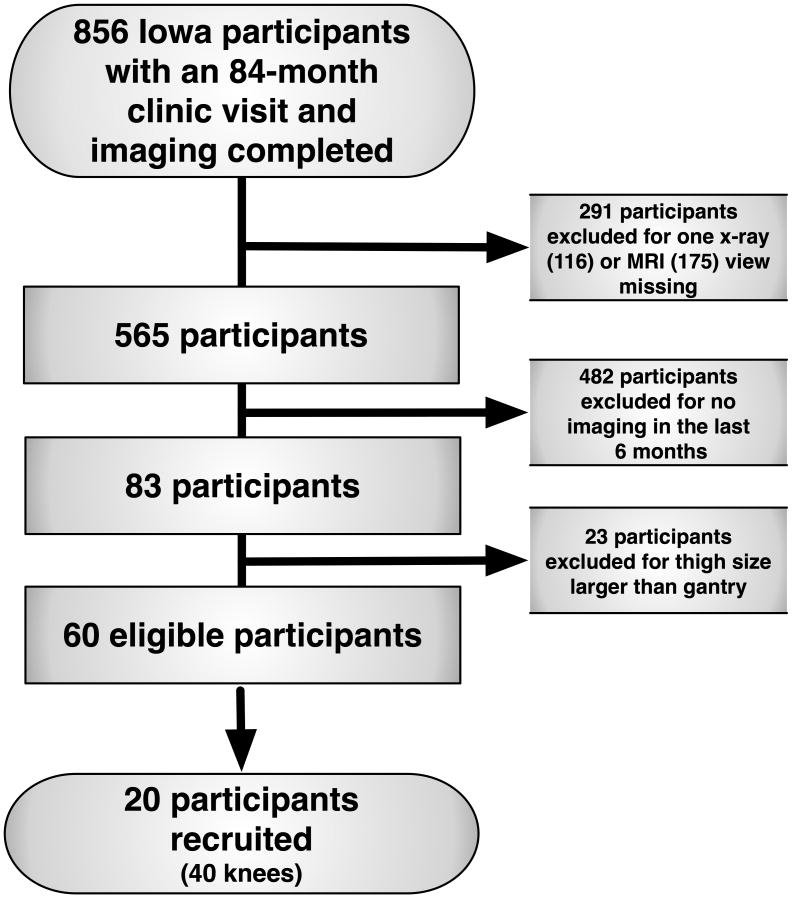
Participants completed an IRB-approved informed-consent process and all methods were HIPPA-compliant. This prospective study was conducted as an ancillary to the 84-month visit of the Multicenter Osteoarthritis Study (MOST), a longitudinal observational study of 3026 community-dwelling adults age 50-79 with knee OA or known risk factors for knee OA.[11] Inflammatory arthritis was an exclusion criterion for participation in MOST as previously described.[11] Both radiographs and 1T MRI were completed on MOST participants at the 84-month clinic visit. Participants in this ancillary study were a convenience sample of those who had bilateral knee radiographs and MRI at the MOST 84-month visit in the 6 months prior (6/8/2012–10/23/2012) to the date when they were recruited to return for acquisition of SCT images for comparison, met MOST reading center quality control criteria, had knees discordant for KL grade (in order to represent a range of OA features and severity), did not have end-stage knee OA (Kellgren/Lawrence (KL) grade <4)[12] or a knee arthroplasty, lived within 25 miles and had a distal thigh width on PA radiographs <38.1cm (SCT gantry width at the time of this study). This thigh width corresponded most commonly with a BMI of 35, allowing representation of >93% of the U.S. population.[13] Out of 83 MOST participants who met inclusion criteria, the first 20 who agreed to return to our center for the ancillary study SCT were recruited (Figure 1).
Fig. 1. Diagram of participants involved.
Image Acquisition
At the 84-month MOST clinic visit, a bilateral, standing fixed-flexion postero-anterior (PA) radiograph of the tibiofemoral compartments was acquired,[14-16] using a protocol in which knees are flexed to 20–30° and feet externally rotated 10° using a plexiglass positioning frame (SynaFlexer).[17] The right and left knees were imaged together on 14 × 17 film with a 183 cm film-to-focus distance. Radiographs were KL graded, with disagreements adjudicated by consensus reading.[12, 14] Knee MRI was completed using a 1-Tesla ONI OrthOne extremity MRI scanner (GE Healthcare, Waukesha, WI) with a circumferential transmit-receive extremity coil. Axial and sagittal fat-suppressed proton density-weighted and coronal short-tau inversion recovery (STIR) sequences were acquired. Our study assessed the coronal STIR sequence (TR=8448ms, TE=17ms, TI=100ms, 3mm slice thickness, 0 mm interslice gap, 34 slices, 256 × 192 matrix, two NEX, 140 × 140 mm FOV, ETL=8) to mirror the PA radiograph readings. [18]
For SCT, a commercial scanner (PedCAT, Curvebeam LLC, Warrington, PA) was modified to enable imaging of bilateral knees in a standing configuration. A custom radiolucent positioning system was used to maintain foot external rotation and knee flexion angles similar to those used for the radiographs. Participants' thighs and hands remained in contact with the unit for stability and prevention of motion. The scanner uses an x-ray tube (Superior SRX-130-20-0.5) with a tungsten target producing pulsed cone-beam x-ray (effective dose equivalent 0.1mSv) on a 30 × 30-cm amorphous silicon flat-panel detector with 194μm pixel size. The detector is used in 2×2 binning mode with 388μm effective pixel size. During CT, 360 images were acquired over a 360° projection angle with two passes for total scan time of 32 seconds (360 pulses × 2 with .012 sec/pulse, resulting in a total exposure time of 8.64 sec). A 3D dataset with isotropic resolution of 0.37mm and FOV of 200×350mm was reconstructed in the coronal plane from initial cone-beam projections. Reconstructed images were uploaded to a PACS as a standard DICOM CT image stack with image matrix of 768 × 768 pixels and 0.37-mm slice thickness.
Image Interpretation
A musculoskeletal radiologist with greater than 12 years of experience with the semiquantitative knee OA feature reading protocols scored marginal osteophytes and subchondral cysts on bilateral PA radiographs and bilateral SCT images (coronal reconstructions) according to the OARSI grading system[19] and dichotomized into either present (grade 1 or above) or absent (grade 0) on each of 8 articular surfaces in each participant (left and right, medial and lateral, femur and tibia). For SCT, the reader selected 1–2 coronal images at the tibial spine prominence that best demonstrated the medial and lateral marginal osteophytes.
SCT images had coded identifiers that did not match the separate coded identifiers on other imaging modalities in order to blind the reader. All images were read in a random order and with a 2-week interval between radiographs and SCT images. Coronal STIR MRIs were read for the same features, by the same experienced musculoskeletal radiologist, with a >4-week interval from reading other modalities. No other clinical information was available to the reader. For MRI, the Whole Organ MRI Score (WORMS) for osteophytes and subchondral cysts was used.[20] For comparison between the WORMS readings on MRI and OARSI grading[19] on radiographs and SCT, the following equivalencies were adopted: WORMS 0=OARSI 0, WORMS 1 and 2=OARSI 1, WORMS 3 and 4=OARSI 2, and WORMS 5, 6 and 7=OARSI 3. The radiologist also noted whether meniscal extrusions were visualized on the PA radiographs, the 1–2 SCT coronal images at the tibial spine prominence and on the MRI.
Statistical Analyses
The presence of marginal osteophytes and subchondral cysts detected with conventional radiography and SCT were compared with those detected with MRI for all surfaces combined and according to articular surface. MRI findings were considered the reference standard. Sensitivity, specificity, and accuracy and 95% confidence intervals for the detection of those lesions were calculated. We tested for statistically significant differences between radiograph and SCT for sensitivity, specificity, and accuracy using McNemar's test (e.g. for sensitivity by determining if the ratio of pairs discordant between SCT and radiography for true positives and false negatives favored one or the other modality). P-values were not calculated if the findings for radiographs and SCT had no discordant pairs.
For knees in which a feature was present on either radiograph or SCT, marginal logistic regression models were used to compare positive (PPV) and negative predictive values (NPV) (i.e. proportion of feature present or absent on MRI, between the knees in which the feature was detected on radiographs or SCT). Some knees had a feature detected on both radiographs and SCT, and we used generalized estimating equations (GEE) to control for the correlation between the two observations per knee. For models that did not converge, the p-value comparing PPV or NPV was not available. Statistical significance was defined at alpha=0.05. Spearman correlation coefficients were calculated to compare the severity of features on OARSI grading on SCT imaging with the severity by WORMS on MRI.
Results
Participants
Ten women (mean±SD age 65.8±5.6, range 57–76; mean±SD BMI 30.0±5.2kg/m2, range: 23.0–37.9kg/m2) and 10 men (mean±SD age 67.7±5.9, range 60–79; mean±SD BMI 29.2±5.0kg/m2, range: 23.7–38.0kg/m2) were recruited. Of the 40 knees, KL grades on standard fixed-flexion radiographs were: KL0 (N=9), KL1 (N=12), KL2 (N=10), KL3 (N=9).
Overall Diagnostic Performance
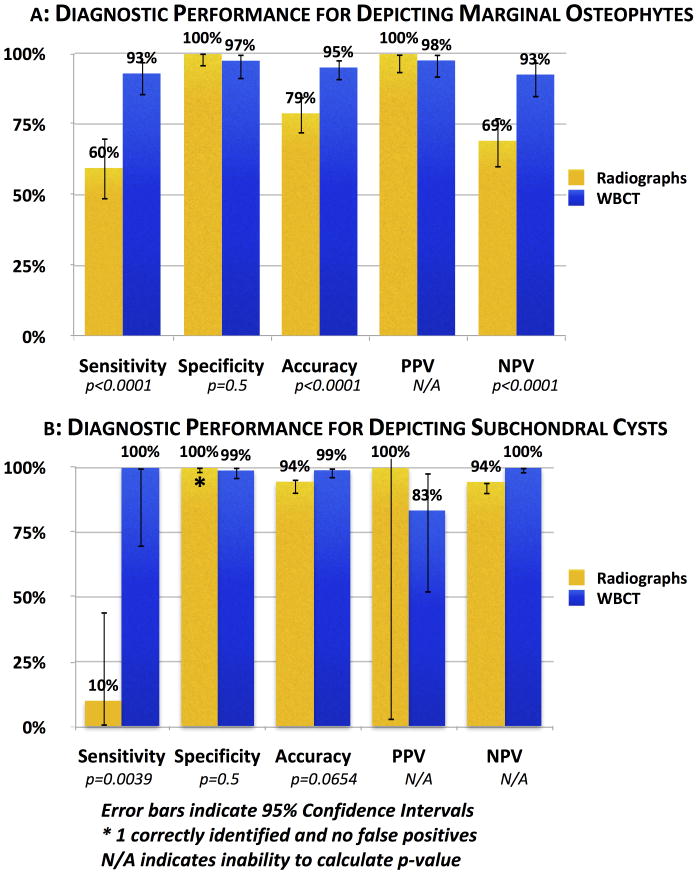
Of the 160 surfaces (medial and lateral femur and tibia for 40 knees), MRI revealed 84 osteophytes and 10 subchondral cysts (Table 1). In comparison with osteophytes and subchondral cysts detected by MRI, SCT was significantly more sensitive and accurate than plain radiographs (Figure 2a and 2b). A low rate of subchondral cysts as well as a low rate of false positive osteophytes on radiographs limited ability to compare specificity between the modalities overall and by surface.
Table 1. Overall Frequency of Knee OA Features Detected by Radiography and WBCT in Comparison with MRI.
| X-ray vs. MRI | |||
|---|---|---|---|
| Feature | Absent on MRI | Present on MRI | |
| Osteophytes | Not Detected On X-Ray | 76 | 34 |
| Detected On X-Ray | 0 | 50 | |
| Subchondral Cysts | Not Detected On X-Ray | 150 | 9 |
| Detected On X-Ray | 0 | 1 | |
| SCT vs. MRI | |||
| Absent on MRI | Present on MRI | ||
| Osteophytes | Not Detected On SCT | 74 | 6 |
| Detected On SCT | 2 | 78 | |
| Subchondral Cysts | Not Detected On SCT | 148 | 0 |
| Detected On SCT | 2 | 10 | |
Fig. 2. a Diagnostic Performance for Depicting Marginal Osteophytes.
b Diagnostic Performance for Depicting Subchondral Cysts
Error bars indicate 95% Confidence Intervals
*1 correctly identified and no false positives
N/A indicates inability to calculate p>value
Surface-Specific Diagnostic Performance for Marginal Osteophytes
Of the 84 osteophytes detected by MRI, 21 were on a lateral femur, 25 were on a medial femur, 14 were on a lateral tibia and 24 were on a medical tibia. In comparison with osteophytes detected by MRI, SCT was more sensitive and accurate than plain radiographs (Table 2). For marginal osteophytes, the greatest differences in sensitivity and accuracy were detected at the medial femur with SCT demonstrating higher sensitivity (p=0.002), accuracy (p=0.002) and negative predictive value (p<0.001) than fixed-flexed radiographs. For the medial femur, medial tibia, lateral femur and lateral tibia respectively, 25%, 20%, 20% and 10% of the osteophytes detected on SCT imaging (OARSI grade ≥1) were not detected on radiographs (OARSI grade 0). OARSI osteophyte grades for all knee on all modalities are presented in Table 3A and details on the knees with OARSI grades that differed between radiographs and SCT imaging are presented in Table 3B. Twenty-four of the 28 marginal osteophytes that were detected by SCT, but not detected on fixed-flexed radiographs, were OARSI grade 1 on MRI and the majority were located on the medial femur and tibia (Table 4). The correlations between OARSI osteophyte severity on SCT imaging and WORMS osteophyte scores on MRI were 0.89, 0.89, 0.94, and 0.95 for the medial femur, medial tibia, lateral femur and lateral tibia respectively. A representative example of a weight-bearing fixed-flexed radiograph and SCT image is presented in Figure 3.
Table 2. Diagnostic Performance of Radiography and WBCT in Depicting Marginal Osteophytes by Surface {95% CI}.
| Modality and Location | Prevalence | Sensitivity zy* | Specificity | Accuracy* | PPV | NPV‡ |
|---|---|---|---|---|---|---|
| Radiography | ||||||
| Medial femur | 12/40 (30.0%) | 48.0% | 100% | 67.5% | 100% | 53.6% |
| Medial tibia | 14/40 (35.0%) | 58.3% | 100% | 75.0% | 100% | 61.5% |
| Lateral femur | 15/40 (37.5%) | 71.4% | 100% | 85.0% | 100% | 76.0% |
| Lateral tibia | 9/40 (22.5%) | 64.3% | 100% | 87.5% | 100% | 83.9% |
| WBCT | ||||||
| Medial femur | 22/40 (55.0%) | 88.0% (p=0.002) | 100% | 92.5% (p=0.002) | 100% | 83.3% (p<0.001) |
| Medial tibia | 22/40 (55.0%) | 91.7% (p=0.008) | 100% | 95.0% (p=0.008) | 100% | 88.9% (p<0.001)‡ |
| Lateral femur | 23/40 (57.5%) | 100% (p=0.031) | 89.5% | 95.0% (p=0.289) | 91.3% | 100% |
| Lateral tibia | 13/40 (32.5%) | 92.9% (p=0.125) | 100% | 97.5% (p=0.125) | 100% | 96.3% (p=0.003) |
p-values for differences between radiograph and WBCT from McNemar's test;
p-values for differences between radiograph and WBCT from logistic regression (GEE);
where not provided, p-values could not be calculated; MRI prevalences were 25/40, 24/40, 21/40 and 14/40 for the medial femur, medial tibia, lateral femur and lateral tibia respectively.
Table 3A. Number of Knees with Each OARSI Osteophyte Grade On Each Modality (N=40 knees).
| OARSI Grade | Modality | Medial femur | Medial tibia | Lateral femur | Lateral tibia |
|---|---|---|---|---|---|
| 0 | MRI | 15 | 16 | 19 | 26 |
| SCT | 18 | 18 | 17 | 27 | |
| Radiographs | 28 | 26 | 25 | 31 | |
| 1 | MRI | 18 | 18 | 12 | 10 |
| SCT | 17 | 17 | 15 | 9 | |
| Radiographs | 6 | 11 | 12 | 7 | |
| 2 | MRI | 7 | 6 | 7 | 3 |
| SCT | 5 | 5 | 6 | 3 | |
| Radiographs | 6 | 3 | 3 | 1 | |
| 3 | MRI | 0 | 0 | 2 | 1 |
| SCT | 0 | 0 | 2 | 1 | |
| Radiographs | 0 | 0 | 0 | 1 |
Table 3B. Percent of OARSI Osteophyte Grades That Differed Between Radiographs and SCT.
| Location | OARSI Grade on Radiographs | OARSI Grade on SCT | Percent* (N=40) |
|---|---|---|---|
|
| |||
| Medial femur | 0 | 1 | 25.0% |
|
| |||
| Medial tibia | 0 | 1 | 17.5% |
| 0 | 2 | 2.5% | |
| 1 | 2 | 2.5% | |
|
| |||
| Lateral femur | 0 | 1 | 17.5% |
| 0 | 2 | 2.5% | |
| 1 | 2 | 10.0% | |
| 2 | 3 | 5.0% | |
|
| |||
| Lateral tibia | 0 | 1 | 10.0% |
| 1 | 2 | 5.0% | |
Percentages reflect the knees with OARSI osteophyte grades discordant between radiographs and SCT imaging. All discordance reflected a more severe grade detected on SCT imaging than on radiographs.
Table 4. WORMS Scores for Knees With Osteophytes Not Visualized on Radiographs (OARSI Grade 0) That Were Visualized on WBCT (OARSI Grade 1 or Above).
| Location | WORMS Grade 1 on MRI | WORMS Grade 2 on MRI |
|---|---|---|
| Medial femur | 22.5% | 2.5% |
| Medial tibia | 20.0% | 0.0% |
| Lateral femur | 10.0% | 5.0% |
| Lateral tibia | 7.5% | 2.5% |
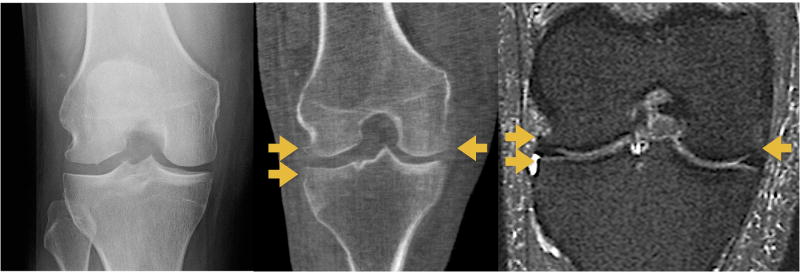
Fig. 3. Fixed Flexion Radiograph and SCT Coronal Image (64 year-old Male).
Fixed flexion radiograph (Left) with no osteophytes visualized. SCT coronal image (Center) and MR coronal Image (Right) with osteophytes visualized on the medial and lateral femur and lateral tibia (arrows), which are not visualized on radiography due to overlapping bony contours.
Surface-Specific Diagnostic Performance for Subchondral Cysts
Of the 10 subchondral cysts, 1 was on the lateral femur, 3 were on a medial femur, 2 were on a lateral tibia and 4 were on a medical tibia. In comparison with cysts detected by MRI, SCT was more sensitive and accurate than plain radiographs (Table 5). Eleven out of 12 subchondral cysts detected by SCT were not detected on fixed-flexed radiographs. All of these were OARSI grade 1 and the majority of them were located on the medial femoral (N=3) and lateral tibial (N=3) surfaces, while the lateral femur (N=2) and medial tibia (N=2) also had subchondral cysts visible on SCT but not on radiographs. The correlations between OARSI subchondral cyst severity on SCT imaging and WORMS subchondral cyst scores on MRI were 1.00, 1.00, 0.70, and 0.81 for the medial femur, medial tibia, lateral femur and lateral tibia respectively. The imperfect correlations occurred where subchondral cysts were detected on SCT but not detected on MRI.
Table 5. Diagnostic Performance of Radiography and WBCT for Visualizing Subchondral Cysts by Surface {95% CI}.
| Modality and Location | Prevalence | Sensitivity* | Specificity* | Accuracy* | PPV* | NPV* |
|---|---|---|---|---|---|---|
| Radiography | ||||||
| Medial femur | 0/40 (0%) | 100% | 100% | 92.5% | - | 92.5% |
| Medial tibia | 1/40 (2.5%) | 25.0% | 100% | 92.5% | 100% | 92.3% |
| Lateral femur | 0/40 (0%) | 100% | 100% | 97.5% | - | 97.5% |
| Lateral tibia | 0/40 (0%) | 100% | 100% | 95.0% | - | 95.0% |
| WBCT | ||||||
| Medial femur | 3/40 (7.5%) | 100% | 100% | 100% | 100% | 100% |
| Medial tibia | 4/40 (10.0%) | 100% | 100% | 100% | 100% | 100% |
| Lateral femur | 2/40 (5.0%) | 100% | 97.4% | 97.5% | 50.0% | 100% |
| Lateral tibia | 3/40 (7.5%) | 100% | 97.4% | 97.5% | 66.7% | 100% |
Where p-values could be calculated, there were no statistically significant differences between radiograph and WBCT; MRI prevalences were 3/40, 4/40, 1/40 and 2/40 for the medial femur, medial tibia, lateral femur and lateral tibia respectively.
Visualization of Medial Meniscal Extrusions
MRI detected two and SCT detected six medial meniscal extrusions. No meniscal extrusions were visualized on fixed-flexed radiographs.
Discussion
The results indicate that SCT has greater sensitivity, accuracy and negative predictive value for diagnosis of osteophytes and greater sensitivity and possibly accuracy for diagnosis of subchondral cysts in comparison with fixed-flexion knee radiographs. The superior diagnostic performance of SCT over radiographs is consistent with the limited ability of a 2D radiographic technique to fully evaluate the knee joint margins and resolve overlapping structures.These findings suggest that SCT may be an attractive replacement for weight-bearing knee radiographs—maintaining the strengths of that modality, while circumventing some limitations by assuring optimal joint surface assessment and providing improved visualization of knee OA pathological features. While MRI also may detect these features, in general clinical practice, currently MRI is not completed while standing. In contrast, the space, time and economic requirements of SCT would permit widespread clinical use.
SCT compared favorably with regard to time, space and radiation dose. PA radiographs required approximately 5–7 minutes to acquire and 5 minutes to read. SCT required 4 minutes to acquire and less than 5 minutes to read. Once SCT data were loaded, the lack of superimposed features on the central coronal slice led to less uncertainty than with radiographs, allowing greater efficiency in OARSI scoring of osteophytes and subchondral cysts. In clinical practice, reviewing all images for additional features likely would require greater time. The space required for SCT image acquisition also was less than for plain radiographs. The SCT scanner is 150×122×119cm (length×width×height), 182 kg and operates on a standard power outlet, whereas the radiographs required greater space due to the 183 cm distance of the film from the x-ray generator and larger space occupied by the machine.
In comparison with an effective dose of 0.04-0.05mSv for fixed-flexion knee radiographs (two lateral images and a bilateral PA view with potential need to repeat if beam angle requires correction), the radiation dose for SCT of bilateral knees in our study was 0.1mSv (conservative estimate of the upper limit of exposure). This dose is equivalent to 10 days of average background radiation at sea level or that experienced by an airline passenger in 2 U.S. cross-country flights.[21] The absolute dose within the center of the beam for the SCT for two knees was 1.174 mSv, which compares favorably with the dose reported for standard multidetector CT for one or two knees (27–40 mSv).[22] Therefore, the reduced time for both image acquisition and interpretation with SCT, in addition to the greater accuracy and magnitude of information available in a 3D imaging dataset were achieved without a clinically significant increase in radiation dose in comparison with radiographs. In addition, acquisition of MRI of knees generally costs greater than 10 times as much as acquisition of SCT of the knees.[23]
The diagnostic performance of knee radiography, with respect to MRI, in our study was comparable with that found in other studies. The sensitivity of radiographs for detecting osteophytes seen on MRI was slightly higher in a tomosynthesis study by Hayashi (71–95%)[8] and in a radiographic study by Kijowski (67%).[24] Findings of the current study concurred with previously reported sensitivity (∼25%) and specificity of radiographs (97–100%) for detecting subchondral cysts.[8] The higher sensitivity and specificity in the lateral tibiofemoral compartment also is consistent with others.[8, 24] Based on osteophytes, in this sample, a higher proportion of knees would be diagnosed with OA by SCT than by radiographs.
SCT images were reformatted in the coronal plane to compare with weight-bearing fixed-flexed radiographs. However, future studies could utilize axial or sagittal images to examine anterior and posterior marginal osteophytes, subchondral cysts, subchondral sclerosis or other features that may not be evident on plain radiographs.[7] This enhanced capability to evaluate the knee while standing may also provide greater precision in grading of the severity and progression of knee OA pathology, but this has yet to be evaluated.
In the current study, osteophytes and subchondral cysts were defined as either present or absent. However, the ability to obtain immediate multiplanar reconstructions from SCT could be used to rapidly measure the lesion volume to provide finer detail regarding the severity and progression of OA than current grading systems. Further studies would be required to assess the validity of such methodology and the time course over which changes can be measured. This advance could improve capacity to stratify patients for clinical trials and more responsively detect the outcomes of clinical therapies.
Using SCT, six meniscal extrusions were visualized. Four of these were not detected by MRI, most likely because the MRI was non-weight bearing. The implication of the ability to visualize meniscal extrusions is that it enables more precise classification of knee pathology than is possible with plain radiographs and could permit sub-typing of KL3 phenotypes, which are poorly characterized on radiographs,[25] as well as risk for incident radiographic knee OA[26] and progression of cartilage loss.[27, 28] The higher prevalence of meniscal extrusions detected by SCT than by MRI could indicate under-detection when the knee is imaged non-weight bearing.[29]
Our study of bony changes was conducted because in clinical practice and for research, standing imaging is essential to accurately view the joint space and bony changes are assessed concurrently. Future research should assess the reproducibility and responsiveness to progression of pathology over time, especially joint space narrowing, since this is a potentially important advantage of SCT over radiography. The capacity to clearly image the joint while standing, and obtain a more functional relationship of the patella to the femoral trochlea than a non-weightbearing view, could enhance understanding of joint anatomy and pathology.
Additional factors that influenced the predictive value related to the ability of radiographs and CT to identify the bony features. In defining MRI as the reference standard, we found some “false positives” on SCT. An alternative explanation is that the coronal STIR MRI sequence available for our study produced false negative results for smaller osteophytes and subchondral cysts.
Strengths of our study included the highly standardized radiograph and MRI acquisition methods, which have been used to evaluate over 6,000 knees at 4 visits.[11] The degree of meticulous care taken in acquiring these images likely exceeds that for clinical knee joint imaging. Therefore, the magnitude of differences in diagnostic performance between SCT and radiographs detected in our study may underestimate those found in clinical settings. Secondly, the radiologist who interpreted the images had over a decade of experience reading images from the radiograph and MRI protocols used in our study. Thus, he may have detected more subtle findings on radiographs than would have been detected by a less experienced reader.
Limitations of our study included sampling only 40 knees. This sample size was more than sufficient to detect differences in diagnostic performance for osteophytes, while including a variety of knee OA pathological severities, but larger samples could provide additional information regarding diagnostic performance for subchondral cysts. An implicit limitation in deriving predictive value is the substantial dependence on prevalence. The low prevalence of subchondral cysts (N=10) led to a lower positive predictive value for SCT than would have resulted in a sample in which the prevalence was higher.
In addition, although the specificity was high, the test performance may not have been optimally assessed, considering that very few modifications were made to the foot and ankle scanner. Optimization of the x-ray beam generator as well as the image processing software is likely to improve the imaging capabilities of SCT for the knee beyond those of the proof-of-concept unit used for our study. In addition, the ability of radiography to identify features of knee OA may have been limited by the use of only a single PA view, rather than multiple views.[14] However, each PA radiograph was compared with a coronal reconstructed image from SCT, allowing a fair comparison, although a much greater volume of information was contained in the SCT data that were not used. We attempted to minimize potential reader bias through blinding the reader to participant identifiers that could be used to link images from different modalities and also by spacing out the readings in time. However, the presence of only a single reader was a limitation. In studies of OA, inter-observer disagreement is an important issue and therefore future studies should utilize multiple readers. Finally, the reliability of radioanatomic positioning of the knee joint and measurement of joint space width[30-32] and the ability to assess OA progression precisely and sensitively are important potential advantages of SCT that were not addressed in our study.
Conclusion
In conclusion, SCT imaging appears to be more sensitive and accurate for detection of osteophytes and subchondral cysts than conventional fixed-flexion radiography. Additional study would be necessary to assess diagnostic performance of SCT measures of joint space narrowing, progression of OA features and patellofemoral joint morphologic changes.
Acknowledgments
The authors thank the participants of the Multicenter Osteoarthritis (MOST) Study who volunteered their time as well as Tricia Feldick and Natalie Glass for essential assistance with recruitment and data collection. The MOST study was funded by the National Institutes of Health through the National Institute on Aging: Felson (Boston University) – AG18820, Lewis (University of Alabama at Birmingham – AG18947, Torner (University of Iowa) – AG18832 and Nevitt (University of California at San Francisco) – AG19069.
All authors report grants from National Institute on Aging. In addition, NA Segal: editorial honoraria for CME publications (Springer SMB LLC); AGuermazi: President and co- owner of the Boston Core Imaging Lab (BICL), a company providing MRI reading services to academic researchers and to industry and provides consulting services to Genzyme.
Footnotes
Financial and competing interests disclosure: The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
- 1.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nevitt MC, Lane N. Body weight and osteoarthritis. Am J Med. 1999;107:632–3. doi: 10.1016/s0002-9343(99)00297-1. [DOI] [PubMed] [Google Scholar]
- 3.March LM, Bachmeier CJ. Economics of osteoarthritis: a global perspective. Baillieres Clin Rheumatol. 1997;11:817–34. doi: 10.1016/s0950-3579(97)80011-8. [DOI] [PubMed] [Google Scholar]
- 4.Brandt KD, Fife RS, Braunstein EM, Katz B. Radiographic grading of the severity of knee osteoarthritis: relation of the Kellgren and Lawrence grade to a grade based on joint space narrowing, and correlation with arthroscopic evidence of articular cartilage degeneration. Arthritis Rheum. 1991;34:1381–6. doi: 10.1002/art.1780341106. [DOI] [PubMed] [Google Scholar]
- 5.Guermazi A, Niu J, Hayashi D, Roemer FW, Englund M, Neogi T, et al. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study) BMJ. 2012;345:e5339. doi: 10.1136/bmj.e5339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guermazi A, Hayashi D, Roemer FW, Felson DT. Osteoarthritis: a review of strengths and weaknesses of different imaging options. Rheum Dis Clin North Am. 2013;39:567–91. doi: 10.1016/j.rdc.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Guermazi A, Roemer FW, Felson DT, Brandt KD. Unresolved questions in rheumatology: motion for debate: osteoarthritis clinical trials have not identified efficacious therapies because traditional imaging outcome measures are inadequate. Arthritis Rheum. 2013;65:2748–58. doi: 10.1002/art.38086. [DOI] [PubMed] [Google Scholar]
- 8.Hayashi D, Xu L, Roemer FW, Hunter DJ, Li L, Katur AM, et al. Detection of osteophytes and subchondral cysts in the knee with use of tomosynthesis. Radiology. 2012;263:206–15. doi: 10.1148/radiol.12111649. [DOI] [PubMed] [Google Scholar]
- 9.Segal NA, Anderson DD, Iyer KS, Baker J, Torner JC, Lynch JA, et al. Baseline articular contact stress levels predict incident symptomatic knee osteoarthritis development in the MOST cohort. J Orthop Res. 2009;27:1562–8. doi: 10.1002/jor.20936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Segal NA, Kern AM, Anderson DD, Niu J, Lynch J, Guermazi A, et al. Elevated tibiofemoral articular contact stress predicts risk for bone marrow lesions and cartilage damage at 30 months. Osteoarthritis Cartilage. 2012;20:1120–6. doi: 10.1016/j.joca.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Segal NA, Nevitt MC, Gross KD, Hietpas J, Glass NA, Lewis CE, et al. The Multicenter Osteoarthritis Study: opportunities for rehabilitation research. PM R. 2013;5:647–54. doi: 10.1016/j.pmrj.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Wye G, Kerker BD, Matte T, Chamany S, Eisenhower D, Frieden TR, et al. Obesity and diabetes in New York City, 2002 and 2004. Preventing chronic disease. 2008;5:A48. [PMC free article] [PubMed] [Google Scholar]
- 14.Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, et al. A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol. 2008;35:2047–54. [PMC free article] [PubMed] [Google Scholar]
- 15.Botha-Scheepers S, Dougados M, Ravaud P, Hellio Le Graverand MP, Watt I, Breedveld FC, et al. Effect of medial tibial plateau alignment on serial radiographs on the capacity to predict progression of knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:272–6. doi: 10.1016/j.joca.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 16.Radiography Working Group of the O-OIW. Le Graverand MP, Mazzuca S, Lassere M, Guermazi A, Pickering E, et al. Assessment of the radioanatomic positioning of the osteoarthritic knee in serial radiographs: comparison of three acquisition techniques. Osteoarthritis Cartilage. 2006;14(Suppl A):A37–43. doi: 10.1016/j.joca.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 17.Peterfy C, Li J, Zaim S, Duryea J, Lynch J, Miaux Y, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol. 2003;32:128–32. doi: 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 18.Roemer FW, Guermazi A, Javaid MK, Lynch JA, Niu J, Zhang Y, et al. Change in MRI-detected subchondral bone marrow lesions is associated with cartilage loss: the MOST Study. A longitudinal multicentre study of knee osteoarthritis. Ann Rheum Dis. 2009;68:1461–5. doi: 10.1136/ard.2008.096834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 20.Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–90. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Cosmic Radiation During Flights. United States Environmental Protection Agency; [Accessed 7 January, 2014]. http://www.epa.gov/radtown/cosmic.html. [Google Scholar]
- 22.Carrino JA, Al Muhit A, Zbijewski W, Thawait GK, Stayman JW, Packard N, et al. Dedicated cone-beam CT system for extremity imaging. Radiology. 2014;270:816–24. doi: 10.1148/radiol.13130225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. [Accessed 7/14/15];Centers for Medicare & Medicaid Services Physician Fee Schedule. http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.
- 24.Kijowski R, Blankenbaker DG, Stanton PT, Fine JP, De Smet AA. Radiographic findings of osteoarthritis versus arthroscopic findings of articular cartilage degeneration in the tibiofemoral joint. Radiology. 2006;239:818–24. doi: 10.1148/radiol.2393050584. [DOI] [PubMed] [Google Scholar]
- 25.Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54:502–6. doi: 10.1016/s0009-9260(99)90846-2. [DOI] [PubMed] [Google Scholar]
- 26.Badlani JT, Borrero C, Golla S, Harner CD, Irrgang JJ. The effects of meniscus injury on the development of knee osteoarthritis: data from the osteoarthritis initiative. Am J Sports Med. 2013;41:1238–44. doi: 10.1177/0363546513490276. [DOI] [PubMed] [Google Scholar]
- 27.Berthiaume MJ, Raynauld JP, Martel-Pelletier J, Labonte F, Beaudoin G, Bloch DA, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–63. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ding C, Martel-Pelletier J, Pelletier JP, Abram F, Raynauld JP, Cicuttini F, et al. Knee meniscal extrusion in a largely non-osteoarthritic cohort: association with greater loss of cartilage volume. Arthritis Res Ther. 2007;9:R21. doi: 10.1186/ar2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stehling C, Souza RB, Hellio Le Graverand MP, Wyman BT, Li X, Majumdar S, et al. Loading of the knee during 3.0T MRI is associated with significantly increased medial meniscus extrusion in mild and moderate osteoarthritis. Eur J Radiol. 2012;81:1839–45. doi: 10.1016/j.ejrad.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wirth W, Duryea J, Hellio Le Graverand MP, John MR, Nevitt M, Buck RJ, et al. Direct comparison of fixed flexion, radiography and MRI in knee osteoarthritis: responsiveness data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2013;21:117–25. doi: 10.1016/j.joca.2012.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mercier C, Piperno M, Vignon E, Brandt K, Hochberg M, Hellio Le Graverand MP. In normal knees, joint space width (JSW) is correlated with the intermargin distance (IMD), a measure of medial tibial plateau alignment. Variations in IMD explain variability in JSW in serial radiographs. Joint Bone Spine. 2013;80:183–7. doi: 10.1016/j.jbspin.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Hellio Le Graverand MP, Clemmer RS, Brunell RM, Hayes CW, Miller CG, Vignon E. Considerations when designing a disease-modifying osteoarthritis drug (DMOAD) trial using radiography. Semin Arthritis Rheum. 2013;43:1–8. doi: 10.1016/j.semarthrit.2012.11.006. [DOI] [PubMed] [Google Scholar]