Abstract
Background
Exposure to the natural environment may improve health behaviors and mental health outcomes such as increased levels of physical activity and lower levels of depression associated with sleep quality. Little is known about the relationship between insufficient sleep and the natural environment.
Purpose
To determine whether exposure to attributes of the natural environment (e.g., greenspace) attenuates the likelihood of reporting insufficient sleep among US adults.
Methods
Multiple logistic regression models were used to explore the association between self-reported days of insufficient sleep (in the past 30 days) and access to the natural environment in a multi-ethnic, nationally representative sample (n=255,171) of US adults ≥18 years of age enrolled in the 2010 Behavioral Risk Factor Surveillance System.
Results
Using 1-to-6 days of insufficient sleep as the referent group for all analyses, lower odds of exposure to natural amenities were observed for individuals reporting 21-to-29 days (OR=0.843, 95% Confidence Interval (CI) = 0.747, 0.951) of insufficient sleep. In stratified analyses, statistically significant lower odds of exposure to natural amenities was found among men reporting7-to-13-days (OR = 0.911, 95% CI = 0.857, 0.968), 21-to-29-days (OR=0.838, 95% CI=0.759, 0.924), and 30-days (OR=0.860, 95%CI=0.784, 0.943) of insufficient sleep. Greenspace access was also protective against insufficient sleep for men and individuals aged 65+.
Conclusions
In a representative sample of US adults, access to the natural environment attenuated the likelihood of reporting insufficient sleep, particularly among men. Additional studies are needed to examine the impact of natural environment exposure on sleep insufficiency across various socio-demographic groups.
Introduction
Adequate sleep has been touted as a critical component of optimal health.1 Individuals attaining adequate or sufficient sleep have been shown to have better cardio-metabolic profiles,2,3 functional capacity,4 lower risk of overweight or obesity and death,5–7 compared to individuals experiencing inadequate or insufficient sleep. In spite of the well-documented benefits of adequate sleep for overall health, many US adults do not meet the recommended 7–8 hours of sleep at night.8 Several population-based studies indicate approximately 40% of US adults sleep less than 7 hours daily.9,10 In addition to sleep disorders,1 socio-environmental and lifestyle factors such as living in an impoverished neighborhood,11,12 shift work,13,1 lower physical activity levels,14 and depression are associated with curtailed sleep.1
One environmental factor that has received less attention in sleep studies is exposure to the natural environment or “natural amenities” - the “physical characteristics of an area that may enhance the location as a place to live.”15 Specific features of an area that may improve health behaviors and mental health outcomes related to sleep duration and quality include access to greenspace, oceanfront or other bodies of water (blue space), as well as sunlight exposure, and temperature. Greater accessibility to green landscapes has been associated with higher levels of physical activity,16,17 which correlates to beneficial sleep patterns.18,19 Access to greenspace has also been shown to confer benefits for mental health,20 including improving cognitive function and reducing anxiety disorders that may result in insufficient sleep.21–24 Among others, environmental factors such as light and thermal environments, as well as access to water, play a pivotal role in shaping human sleep.
Turning to specific aspects of the natural environment, Wheeler et al., (2012) found a gradient of increasing self-reported “good” health with increasing residential proximity to the coast in England.25 Since sleep is considered one of the pillars of good health,26 residing in areas with easy access to oceanfront or bodies of water may support good sleep habits. Alternatively, access to water may enhance health because it increases physical activity.
The thermal environment, which is important for setting our sleep/wake cycles,27 is influenced by ambient temperature.28 Exposure to extremes of the temperature spectrum that is not habitual where the body has an opportunity to adjust, disrupts various stages of rapid eye movement and slow wave sleep cycles, in addition to changes in heart rate.28,29 Humid conditions, in particular, increase the propensity for wakefulness,30 potentially placing individuals who live in areas with higher temperatures at increased risk for insufficient sleep.
Light is the pervasive and prominent zeitgeber (time giver) to resetting biological rhythms.31–34 Light also plays a critical role in modulating sleep patterns and mood.35,36 Several studies have shown that infants exposed to more natural light during the day sleep better at night, and influences the sleep-wake cycle in adulthood as well.37,38 At the other end of the life course, elderly individuals are more likely to have sleep disorders due to limited exposure to daytime light.39,40 Additionally, the influence of light exposure on mood is also evident among individuals with seasonal affective disorder, where lower exposure to light during winter months may reduce the production of melatonin via the pineal gland.41,42 Notably, high exposure to light at night due to shift work may result in adverse health outcomes such as certain forms of cancer, possibly due to the reduction in the secretion of melatonin.43 Thus, exposure to light during daily periods that may not be optimal for the sleep-wake cycle can result in circadian misalignment and increase the risk of sleep disturbances and other adverse health outcomes.
Although various aspects of the natural environment have been shown to influence sleep patterns, few studies have examined these relationships in large population-based samples in the United States. The purpose of this study was to investigate the relationship between exposure to various attributes of the natural environment and sleep insufficiency. We hypothesize that individuals with higher exposure to positive attributes of the natural environment will be less likely to report insufficient sleep.
Methods
The primary data source for this study was derived from the 2010 Behavioral Risk Factor Surveillance System (BRFSS), a yearly, randomized telephone survey of behavioral risk factors among US adults ≥18 years of age.44 A multi-ethnic nationally representative sample of adults (one per household) are sampled from all 50 states, the District of Columbia, Puerto Rico, the US Virgin Islands, and Guam to track trends in health conditions and risk behaviors in the US.44,45 The BRFSS also contains geographically referenced data for participants that permit analysis across US counties to contextualize health risk. The median cooperation rate for the BRFSS in 2010 was 76.9%, while the final response rate was 54.6%.46
To explore sleep insufficiency, the following question from the BRFSS was used, “During the past 30 days, for about how many days have you felt you did not get enough rest or sleep?” Although the BRFSS sample available for analysis included 451,072 participants, after the exclusion of missing data on county codes, pregnant women, and covariates, the final sample used in the present analysis consisted of 245,531 participants.
Guided by the literature examining socio-demographic determinants of sleep patterns,47 covariates in our analysis included age as a continuous variable, and categorical variables for gender, employment status, race/ethnicity (Black, White, Asian, Hispanic), level of education, number of children, smoking status, alcohol use, body mass index, asthma status, general health status, income level, disability status, physical activity and emotional support.
Natural Amenities
Participants with geographically-referenced data were assigned an amenity score based on a natural amenity index developed by the USDA Economic Research Service.15 The index was developed to reflect the natural landscape of counties in the lower 48 states, including varied topography such as lakes, oceanfront and climate to encompass all four seasons in the United States. The index uses standardized z-scores of mean hours of sunlight, mean relative humidity, mean temperature, and proportion of water, in addition to a topography variation scale that accounts for the basic land formations (e.g., hills and mountains) in each county. The scores for average temperature, mean hours of sunlight, and mean relative humidity span a 29-year period (1941 – 1970). A score of 1 to 7 was then assigned to each county based on the sum of the z-scores of each of the natural amenities. A higher score corresponds to higher levels of natural amenities.
Greenspace
Access to greenspace was measured using the normalized difference vegetation index (NDVI). The NDVI is a well-established vegetation index used to measure vegetation biomass, greenness, and dominant species.48,49 The NDVI scores are typically estimated based on the ratio between reflectivity in the red, and near infrared bands, where chlorophyll pigment strongly absorbs radiation in the red band, and is highly reflective in the near-infrared band.49 The 2006 16-day Moderate-Resolution Imaging Spectroradiometer (MODIS) data from the Global Land Cover Facility website was used to assign NDVI scores for each participant using the geographically weighted centroid of each county, as home addresses are not publicly available from the BRFSS.50 The MODIS dataset includes stretched NDVI values that range from 0–250 by adjusting the original NDVI values, which typically range from −1 to + 1 using the formula (NDVI score*200) + 50. Higher NDVI scores represent higher access to greenspace.
Statistical Analysis
The primary independent variables were access to natural amenities and greenspace defined as continuous variables above, while sleep insufficiency was the primary outcome variable for all analyses. Socio-demographic, lifestyle and psychosocial control variables were examined using frequency distributions and summarized either as counts and percentages for categorical variables or as means (± standard deviations) for continuous variables. Multivariate logistic regression models were fit in STATA 12 (Stata, version 12) by categorizing insufficient sleep into five groups as 6 days or less (referent group), 7–13 days, 14–20 days, 21–29 days, and 30 days. These categories were selected based on pre-established cut-off points for insufficient sleep using population-based US samples.51–53 Race, age and sex-specific differences on the influence of access to the natural environment on insufficient sleep were also examined in stratified analyses. Sample weights developed for the 2010 BRFSS were used in all analyses 44 to account for the complex sampling design, and statistical significance was set at the p <0.05 level.
Results
Table 1 presents characteristics of the sample (n=245,531). The mean NDVI score was 89.08 (±51.21), and the mean natural amenities score was 3.49 (±1.02). The sample was primarily non-Hispanic White (80%), with non-Hispanic Blacks and Hispanics constituting 8.5% and 6.6%, respectively. Women comprised 64% of the study population and approximately 33% of individuals were considered obese, based on a body mass index (BMI) of greater than or equal to 30 kg/m2. Current smokers constituted less than 30% of the sample, and approximately 50% reported more than 2 weeks of insufficient sleep. The mean age was 56.6 years (±15.17. Less than 1 week was the most common number of days reported by participants (33.7%) as experiencing insufficient sleep.
Table 1.
Summary characteristics of the study sample, BRFSS 2010 sleep insufficiency analysis, n=245531
| Variable | N | Percent | |
|---|---|---|---|
| Race | |||
| White | 195,110 | 80.34 | |
| Black | 20685 | 8.52 | |
| Asian | 2996 | 1.23 | |
| Hispanic | 15,983 | 6.58 | |
| All others | 8080 | 3.33 | |
| Total | 242,854 | 100.00 | |
| Sex | |||
| Male | 88068 | 35.87 | |
| Female | 157,463 | 64.13 | |
| Total | 245,531 | 100.00 | |
| Heavy Alcohol Use* | |||
| No | 237,209 | 97.82 | |
| Yes | 5276 | 2.18 | |
| Total | 242,485 | 100.00 | |
| Smoking Status | |||
| Never | 126,888 | 51.87 | |
| Former Smokers | 65,198 | 26.65 | |
| Current Smokers | 52,563 | 21.49 | |
| Total | 244,649 | 100.00 | |
| Body Mass Index Category | |||
| <25 | 81,442 | 33.17 | |
| 25–29 | Overweight | 83,578 | 34.04 |
| >=30 | Obese | 80,509 | 32.79 |
| Total | 245,529 | 100.00 | |
| Employment Status | |||
| Unemployed/Retired/Homemaker | 105,065 | 42.93 | |
| Employed | 139,672 | 57.07 | |
| Total | 244,737 | 100.00 | |
| Marital status | |||
| Never Married | 31,057 | 12.69 | |
| Divorced/Separated/Widowed | 68,498 | 27.99 | |
| Married | 145,190 | 59.32 | |
| Total | 244,745 | 100.00 | |
| Days of Insufficient Sleep in 30 days | |||
| <=6 days | 82,618 | 33.65 | |
| 7 to 13 days | 45,962 | 18.72 | |
| 14 to 20 days | 48,381 | 19.70 | |
| 21 to 29 days | 28,242 | 11.50 | |
| 30 days | 40,328 | 16.42 | |
| Total | 245,531 | (100%) | |
| Age [median] (std dev) | 245,531 | 56.60 [57] (15.17) | |
|
Greenspace Score Mean [median] (std dev) |
242130 | 89.08 [51] (51.21) | |
|
Natural Amenity Index Mean [median] (std dev) |
243304 | 3.49[3] (1.02) | |
>2 drinks per day for men; >1 drink per day for women
Natural Amenities
With the exception of individuals reporting 14-to-20 days (OR=1.122 95% CI=1.012, 1.244; p<0.05) and 30-days (OR=1.072, 95% CI=0.947, 1.213; p>0.05) of insufficient sleep, individuals reporting 7-to-13 days (OR=0.923, 95%CI=0.797,1.069), and 21-to-29 days (OR=0.843, 95%CI = 0.747, 0.951; p<0.01) had lower odds of access to natural amenities, compared to individuals reporting 1-to-6 days of insufficient sleep (Table 2).
Table 2.
Days of Sleep Insufficiency per Month and Odds of Exposure to Natural Amenities^, BRFSS, 2010, (N=245,531)
| Categories of Insufficient Sleep | Multivariable Odds Ratio Entire Sample (95% Confidence Intervals) |
Multivariable Odds Ratio For Women (95% Confidence Intervals) |
Multivariable Odds Ratio For Men (95% Confidence Intervals) |
Multivariable Odds Ratio For Whites (95% Confidence Intervals) |
Multivariable Odds Ratio For Blacks (95% Confidence Intervals) |
|---|---|---|---|---|---|
| 1–6 Days | 1 (referent) | 1 (referent) | 1 (referent) | 1 (referent) | 1 (referent) |
| 7–13 days | 0.923 [0.797,1.069] | 1.041 [0.880,1.231] | 0.911** [0.857,0.968] | 0.907 [0.775,1.061] | 1.018 [0.900,1.151] |
| 14–20 days | 1.122* [1.012,1.244] | 1.243** [1.091,1.418] | 0.989 [0.944,1.036] | 1.264*** [1.141,1.399] | 0.894 [0.779,1.025] |
| 21–29 days | 0.843** [0.747,0.951] | 0.925 [0.805,1.064] | 0.838*** [0.759,0.924] | 0.956 [0.844,1.084] | 0.825 [0.690,1.011] |
| 30 days | 1.072 [0.947,1.213] | 1.331*** [1.146,1.546] | 0.860** [0.784,0.943] | 1.111 [0.970,1.273] | 1.047 [0.924,1.186] |
p < 0.05,
p < 0.01,
p < 0.001;
Refers to an index with scores for mean temperature, humidity, hours of sunlight, overall topography, and percent of water at the county level
adjusted for age (years), gender (men, women), marital status (divorced, separated, widowed, married), race (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, other), education (< high school, > high school), employment status (employed, unemployed/retired, homemaker, student), number of children, physical activity (any physical activity in the past month), smoking, income level, asthma (no, yes), general health status (excellent, good, very good, fair, poor), emotional support (never, sometimes, rarely), disability (no, yes), body mass index categories (<25, 25–29, ≥30 kg/m2), heavy alcohol use (yes, no). In the stratified analyses for gender and race, these variables were not controlled for. In the stratified analyses for gender and race, these variables were not controlled for.
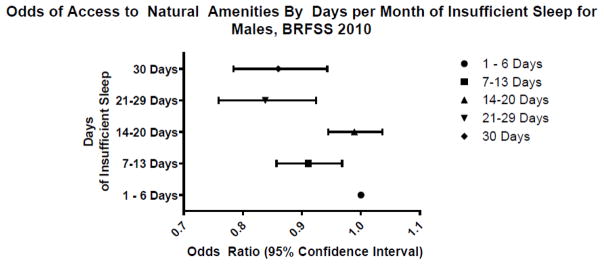
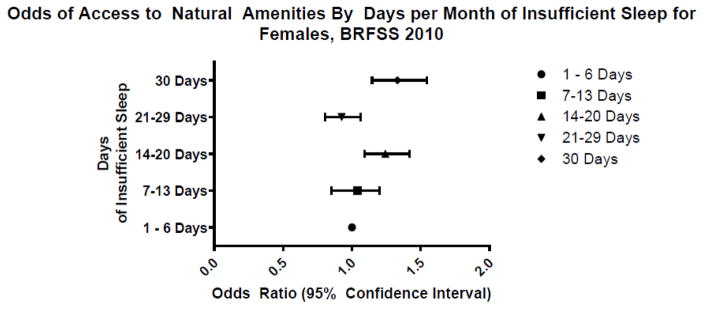
Males reporting 7-to-13 days (OR=0.911, 95% CI = 0.857, 0.968; p<0.01), 21-to-29 days (OR=0.838, 95% CI = 0.759, 0.924; p<0.001), or 30 days (OR=0.860, 95% CI = 0.784, 0.943; p<0.01) of insufficient sleep, had lower odds of access to natural amenities compared to individuals reporting 1-to-6 days of insufficient sleep (Figure 1). We found a significant trend in these findings (p<0.05). Among females, higher odds of access to natural amenities for individuals reporting 14-to-20 days (OR=1.243, 95% CI = 1.091, 1.418; p<0.01), or 30 days (OR=1.331, 95% CI =1.146, 1.546; p<0.001) of insufficient sleep were observed, compared to individuals reporting 1-to-6 days of insufficient sleep (Figure 2).
Figure 1.
Odds of Access to Natural Amenities by Days of Insufficient Sleep for Males
Figure 2.
Among Whites, individuals reporting 14-to-20 days of insufficient sleep were more likely to have higher odds of access to natural amenities (OR=1.264, 95% CI = 1.141, 1.399; p<0.001) compared to individuals reporting 1-to-6 days of insufficient sleep. There were no statistically significant associations observed between various categories of insufficient sleep and odds of exposure to natural amenities for Blacks. Asians reporting 30 days (OR=1.214, 95%CI, 1.004, 1.467; p<0.05) and Hispanics reporting 14-to-21 days (OR=1.128, 95% CI=1.042, 1.220; p<0.01) of insufficient sleep had higher odds of exposure to natural amenities (data not shown).
In age-stratified analysis, among 26-to-64 year olds, individuals reporting 21–29 days of insufficient sleep were less likely to have exposure to natural amenities compared to individuals reporting <6 days of insufficient sleep (OR=0.992, 95% CI=0987,0998; p<0.05). For participants >65, the impact was even greater, with individuals reporting much lower exposures to natural amenities if reporting 21–29 days (OR = 0.586, 95% CI=0.488, 0.705, p<0.001) or 30 days (0.840, 95% CI =0.759, 0.929, p<0.001) of insufficient sleep. (Results not shown).
Greenspace
Individuals reporting 1-to-6 days of insufficient sleep were used as the reference group for all analyses (Table 3). Individuals reporting 7-to-13 days (OR=0.995, 95% CI = 0.988, 1.002; p>0.05), or 21-to-29 days (OR=0.991, 95% CI = 0.986, 0.9996; p<0.001) of insufficient sleep had lower odds of access to greenspace. Individuals reporting 14-to-20 days of insufficient sleep were statistically indistinguishable from individuals reporting 1 to 6 days of insufficient sleep.
Table 3.
Days of Sleep Insufficiency per Month and Odds of Greenspace Access BRFSS, 2010, (N=245,531)+
| Categories of Insufficient Sleep | Multivariable Odds Ratio Entire Sample (95% Confidence Intervals) |
Multivariable Odds Ratio For Women (95% Confidence Intervals) |
Multivariable Odds Ratio For Men (95% Confidence Intervals) |
Multivariable Odds Ratio For Whites (95% Confidence Intervals) |
Multivariable Odds Ratio For Blacks (95% Confidence Intervals) |
|---|---|---|---|---|---|
| 1–6 Days | 1 (referent) | 1 (referent) | 1 (referent) | 1 (referent) | 1 (referent) |
| 7–13 days | 0.995 [0.988,1.002] | 1.002 [0.994,1.010] | 0.991*** [0.987,0.995] | 0.995 [0.987,1.002] | 1.002 [0.999,1.006] |
| 14–20 days | 1.004 [0.999,1.009] | 1.009** [1.003,1.015] | 0.996*** [0.993,0.998] | 1.012*** [1.007,1.017] | 0.987*** [0.981,0.993] |
| 21–29 days | 0.991*** [0.986,0.996] | 0.997 [0.989,1.004] | 0.984*** [0.979,0.990] | 0.999 [0.994,1.005] | 0.975*** [0.971,0.980] |
| 30 days | 1.005 [0.999,1.011] | 1.015*** [1.009,1.021] | 0.991*** [0.986,0.996] | 1.006 [1.000,1.013] | 1.007** [1.002,1.011] |
p < 0.05,
p < 0.01,
p < 0.001;
Refers to an index with scores for mean temperature, humidity, hours of sunlight, overall topography, and percent of water at the county level. In the stratified analyses for gender and race, these variables were not controlled for.
adjusted for age (years), gender (men, women), marital status (divorced, separated, widowed, married), race (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, other), education (< high school, > high school), employment status (employed, unemployed/retired, homemaker, student), number of children, physical activity, smoking, income level, asthma (no, yes), general health status (excellent, good, very good, fair, poor), emotional support (never, sometimes, rarely), disability (no, yes), body mass index categories (<25, 25–29, ≥30 kg/m2), heavy alcohol use (yes, no).
In stratified analyses (Table 3), compared to males reporting 1-to-6 days of insufficient sleep, males reporting 7-to-13 days (OR=0.991, 95% CI = 0.987, 0.995; p<0.001), 14-to-20 days (OR=0.996, 95% CI = 0.993, 0.998; p<0.001), 21-to-29 days (OR = 0.984, 95% CI,0.979, 0.990; p<0.001) or 30 days (OR=0.991, 95% CI = 0.986, 0.996; p<0.001) of insufficient sleep, all had lower odds of access to greenspace. Among females, however, individuals reporting 14-to-20 days (OR=1.009, 95% CI = 1.003, 1.015; p<0.01) or 30 days (OR=1.015, 95%CI = 1.009, 1.021; p<0.001) of insufficient sleep had higher odds of greenspace access compared to individuals reporting 1-to-6 days of insufficient sleep.
Among Whites, individuals reporting 14-to-20 days of insufficient sleep had higher odds of access to greenspace compared to individuals reporting 1-to-6 days of insufficient sleep (P<0.001). Among Blacks, however, we found that individuals reporting 14-to-20 days (OR = 0.987, 95% CI = 0.981, 0.993, p<0.001) or 21-to-29 days (OR=0.975, 95%CI, 0.971, 0.980, p<0.001) of insufficient sleep, had lower odds of exposure to greenspace, while individuals reporting 30 days of insufficient sleep (OR=1.007, 95% CI = 1.002, 1.011; p<0.01) had similar odds of exposure to greenspace compared to individuals reporting 1-to-6 days of insufficient sleep. There were no significant associations found between access to greenspace and sleep insufficiency among Asians or Hispanics (results not shown).
The association between days of insufficient sleep and exposure to green space was less robust compared to the association between days of insufficient sleep and natural amenities by age. Individuals age 65 or older, however, had less access to greenspace when reporting 21–29 days of insufficient sleep (OR =0.971, 95% CI =0.963, 0.980, p<0.001) or 30 days of insufficient sleep (OR=0.989, 95% CI =0.984, 0.995, P<0.001). (Results not shown)
Discussion
Exposure to positive attributes of the natural environment (e.g., greenspace, oceanfront), and the lower risk of adverse health outcomes such as cardiovascular disease,54 mental health,55 and overall general health (de Vries et al., 2003),56 has resulted in recent investigations exploring similar associations with sleep.20 Consistent with the findings of Astell-Burt et al. (2013)57 in an Australian sample, we found individuals with lower odds of access to the natural environment (greenspace and natural amenities) reporting more days of insufficient sleep. However, with the exception of males, we did not find a consistent trend across increasing categories of days of insufficient sleep with natural amenities. Compared to males reporting 1 to 6 days of insufficient sleep, all males reporting a week or more of insufficient sleep had lower odds of access to the natural environment. This finding may be due to the positive impact of physical activity on sleep quality,18 where men are not only more likely to exercise, but also to exercise outdoors, compared to women;58,59 although we controlled for physical activity, the crude measure in the 2010 BRFSS (which is dichotomous) could allow unmeasured variation in physical activity to explain this relationship for males. Additionally, greenspace access has been shown to have a greater impact on mental health, which influences sleep insufficiency, 24 among individuals that are more physically active.20 A longitudinal study exploring the impact of greenspace access on mental health outcomes, also found a protective effect for men, but not for women.60 Women are also more likely to report insomnia, anxiety and depression,61,62 all factors that may also increase sleep insufficiency. As such, the natural environment may have less of an impact on sleep insufficiency for women, which may explain why we did not observe statistically significant protective odds for access to greenspace or natural amenities for women in this sample. Women may also have concerns regarding safety and outdoor activities, which may limit the time spent with exposure to nature, compared to men, or women’s access to nature may be limited for other reasons.
Lower odds of exposure to natural amenities were associated with 1 week and 3 weeks of insufficient sleep, but not 14-to-20 or 30 days. Similar results were found for access to greenspace, with individuals reporting 7- to-13 days, and 21-to-29-days of insufficient sleep having lower odds of access to greenspace, compared to 1-to-6-days. The positive associations observed between exposure to the natural environment and fewer days of reported insufficient sleep are aligned with studies demonstrating the restorative effect of exposure to nature on psychosocial factors associated with sleep (e.g., stress),63–66.51 which may improve sleep sufficiency. In a study comparing individuals engaged in Shinrin-yoku (forest walking/breathing), to individuals walking in urban city environments, researchers found improved physiological outcomes for the Shinrin-yoku group, such as decreased salivary cortisol, blood pressure, pulse rate, and lower parasympathetic nerve activity67, which all play a role in sleep sufficiency.68 The lower humidity found in the forest environments was also correlated with lower fatigue scores among participants, which might explain why individuals (particularly men) with higher odds of exposure to natural amenities in our study reported fewer days of insufficient sleep.67
Interestingly, across the entire sample and in sub-group analyses, individuals reporting 21–29 days of insufficient sleep consistently had lower odds of access to greenspace and natural amenities compared to individuals reporting less than 1 week of insufficient sleep. Although this finding was not statistically significant for women or all racial/ethnic groups, 3 weeks may be a threshold where access to the natural environment possibly confers benefits for sleep sufficiency independent of individual-level factors. Adults may be able to find other ways to cope with limited sleep for less than 3 weeks, but environmental factors such as a restorative natural environment may be needed to improve sleep sufficiency. Prospective studies using objective measures of habitual sleep, over either longer and shorter periods of time, however, are needed to further explore this hypothesis. Given the positive impact of greenspace and the natural amenities on other health outcomes influenced by sleep such as diabetes,69 our study has important implications for population-based health programs concerned with developing policies to improve the “outdoor” environment as a mechanism for reducing adverse health outcomes.70 Additional factors (e.g., air quality) in the natural environment may be important to consider with respect to influences on sleep quality for racial ethnic groups, especially since we found that higher levels of exposure to positive attributes of the natural environment did not result in better sleep quality for Whites. The stronger protective effect observed for individuals aged 65+ with exposure to the natural amenities compared to younger adults is consistent with studies indicating that exposure to aspects of the natural environment (e.g., light), may improve sleep patterns.39,40
Although there are many strengths of this study, there are also several limitations. Our exposure measurements were derived at the county-level rather than smaller units of geography (e.g., census tracts), which may capture better the actual environment used by participants. Another assumption was that proximity to the natural environment was equated with utilization, as there were no questions in the secondary data sources used to assess actual use or time spent in the natural environment for each participant. Although we examined access to greenspace separately from our index of natural amenities, it was not possible to disentangle which other aspects of natural amenities (e.g., access to water, or living in a county with warm temperatures) exerted the greatest influence on sleep insufficiency. We were also unable to control for the number of children in a household based on stages of human development (e.g., infants and toddlers vs. teenagers), where caregiving responsibilities at each stage may differentially impact parental/adult sleep quality. Moreover, there are differences in the time frame of the environmental measures and the primary outcome. The natural amenities index uses mean environmental scores (e.g., temperature) for January and July, so we compared the temperatures for these months for 2010, and then for the time period for the index, 1941 – 1970 from the US National Oceanic and Atmospheric Administration. We did not find significant differences – for example, the mean July temperature for 1941–1970 was 73.58°F while for 2010, it was 74.71°F. Perhaps most troubling, this study, like prior, related studies, is cross-sectional, thus limiting causal associations due to the differences in the timing between the primary exposure and outcome. Additionally, we did not account for aspects of the social environment (e.g., crime) that could potentially negate (e.g., lower likelihood of exploring one’s environment) the positive impact of exposure to the natural environment. Sleep insufficiency was also based on self-reports, thus it is difficult to validate objectively these observations.
Notwithstanding these limitations, this study makes a meaningful contribution to the literature as one of the few studies examining the influence of the natural environment on sleep insufficiency in the US. Our composite measure of natural amenities relied on approximately 3 decades of data on the natural environment, thus providing a more stable measure of the environment. We also used a well-established, nationally representative sample of the US population.
Conclusion
In a nationally representative sample of US adults, access to natural amenities and greenspace was shown to attenuate the likelihood of reporting insufficient sleep, particularly for men. Our findings suggest a link between our natural environment and health and the need to preserve its future. Additional studies may be needed to determine whether this relationship holds at smaller levels of geography and to disentangle whether specific characteristics of the natural environment may be more likely to improve sleep sufficiency across various socio-demographic groups.
Highlights.
Exposure to the natural environment influences sleep quality.
Insufficient sleep among men and individuals aged 65+ was attenuated by the natural environment.
Preserving the natural environment may be important for improving sleep quality.
Acknowledgments
We thank the NHLBI for supporting the Behavioral Medicine and Sleep Program to Increase Diversity among Individuals engaged in Health Related Research (PRIDE). We also acknowledge support from the following NIH grants:R01MD004113, R25HL105444, and K24HL2222315-01, as well as the James Scholar Program at the University of Illinois-Urbana Champaign.
Footnotes
None of the study sponsors played any role in the study design, collection, analysis or interpretation of data, writing the manuscript, or the decision to submit the manuscript.
Financial Disclosures
DGT has no financial disclosures.
KNT has no financial disclosures.
MK has no financial disclosures.
NJW has no financial disclosures.
SKP has no financial disclosures.
GJL has no financial disclosures.
Conflict of Interest Statements
DGT has no conflicts of interest to report. DGT was supported by NIH R25HL105444 and research funds from the Department of Kinesiology and Community Health, University of Illinois at Urbana-Champaign.
KNT has no conflicts of interest to report. KNT was supported by research funds to DGT from the Department of Kinesiology and Community Health, University of Illinois at Urbana-Champaign.
MK has no conflicts of interest to report. MK was supported by the James Scholar Program at the University of Illinois at Urbana Champaign.
NJW has no conflicts of interest to report. NJW was supported by NIH grants R01MD004113 and R25HL105444.
SKP has no conflicts of interest to report. SKP was supported by NIH grants R01MD004113, R25HL105444, and R01MD007716.
GJL has no conflicts of interest to report. GJL was supported by NIH grants R01MD004113, R25HL105444, and R01MD007716.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Diana S. Grigsby-Toussaint, Department of Kinesiology and Community Health, Division of Nutritional Sciences, University of Illinois at Urbana-Champaign, Champaign, IL.
Kedir N. Turi, Department of Kinesiology and Community Health, University of Illinois at Urbana-Champaign, Champaign, IL
Mark Krupa, Department of Geography, University of Illinois at Urbana-Champaign, Champaign, IL
Natasha J. Williams, Center for Healthful Behavioral Change, New York University School of Medicine, New York, NY.
Seithikurippu K. Pandi-Perumal, Center for Healthful Behavioral Change, New York University School of Medicine, New York, NY
Girardin Jean-Louis, Center for Healthful Behavioral Change, New York University School of Medicine, New York, NY
References
- 1.Colten HR, Altevogt BM, editors. Institute of Medicine (US) Committee on Sleep Medicine and Research. Washington (DC): The National Academies Press; 2006. Sleep disorders and sleep deprivation: an unmet public health problem. [PubMed] [Google Scholar]
- 2.Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res. 2012;21(4):427–33. doi: 10.1111/j.1365-2869.2011.00990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 4.Brimah P, Oulds F, Olafiranye O, Ceide M, Dillon S, Awoniyi O, Nunes J, Jean-Louis G. Sleep duration and reported functional capacity among black and white US adults. J Clin Sleep Med. 2013;9(6):605–9. doi: 10.5664/jcsm.2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jean-Louis G, Williams NJ, Sarpong D, Pandey A, Youngstedt S, Zizi F, Ogedegbe G. Associations between inadequate sleep and obesity in the US adult population: analysis of the national health interview survey (1977–2009) BMC Public Health. 2014;14:290. doi: 10.1186/1471-2458-14-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 7.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 8.Perry GS, Patil SP, Presley-Cantrell LR. Raising Awareness of Sleep as a Healthy Behavior. Prev Chronic Dis. 2013;10:130081. doi: 10.5888/pcd10.130081. http://www.cdc.gov/Other/disclaimer.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Unhealthy sleep-related behaviors — 12 States, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(8):233–8. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities— United States, 2005–2008. MMWR Morb Mortal Wkly Rep. 2011;60(8):239–42. [PubMed] [Google Scholar]
- 11.Hale L, Do DP. Re: “Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study”. Am J Epidemol. 2007;165(2):231–2. doi: 10.1093/aje/kwk080. [DOI] [PubMed] [Google Scholar]
- 12.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51(3–4):275–8. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 13.Berkmn LF, Buxton O, Ertel K, Okechukwu C. Managers’ practices related to work-family balance predict employee cardiovascular risk and sleep duration in extended care settings. J Occup Health Psychol. 2010;5(3):316–29. doi: 10.1037/a0019721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McClain JJ, Lewin DS, Laposky AD, Kahle L, Berrigan D. Associations between physical activity, sedentary time, sleep duration and daytime sleepiness in US adults. Prev Med. 2014;66:68–73. doi: 10.1016/j.ypmed.2014.06.003. pii: S0091-7435(14)00203-5 Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.USDA Economic Research Service. Natural Amenities Scale. 2012 www.ers.usda.gov/data-products/natural-amenities-scale.aspx#.U7esaUB1jbh.
- 16.Coutts C, Chapin T, Horner M, Taylor C. County-Level Effects of green space access on physical activity. J Phys Act Health. 2013;10(2):232–40. doi: 10.1123/jpah.10.2.232. [DOI] [PubMed] [Google Scholar]
- 17.Grigsby-Toussaint D, Chi SH, Fiese BH. Where they live how they play: neighborhood greenness and outdoor physical activity among preschoolers. Int J Health Geogr. 2011;14(10):66. doi: 10.1186/1476-072X-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brand S, Gerber M, Beck J, Hatzinger M, Puhse U, Holsboer-Trachsler E. High exercise levels are related to favorable sleep patterns and psychological functioning in adolescents: a comparison of adolescents and controls. J Adolesc Health. 2010;46(2):133–141. doi: 10.1016/j.jadohealth.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Ueno LM, Drager LF, Rodrigues AC, Rondon MU, Braga Am, Mathias W, Krieger EM, et al. Effects of exercise training in patients with chronic heart failure and sleep apnea. Sleep. 2009;32(5):637–647. doi: 10.1093/sleep/32.5.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Astell-Burt T, Feng X, Kolt GS. Mental health benefits of neighbourhood green space are stronger among physically active adults in middle-to-older age: evidence from 260,061 Australians. Prev Med. 2013;57(5):601–6. doi: 10.1016/j.ypmed.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 21.Wells NM. At Home with Nature, Effects of “Greenness” on Children’s Cognitive Functioning. Environ Beh. 2002;32(6):775–95. [Google Scholar]
- 22.Kuo FE, Taylor AF. A potential natural treatment for attention-deficit/hyperactivity disorder: evidence from a national study. Am J Public Health. 2004;94(9):1580–6. doi: 10.2105/ajph.94.9.1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nutsford D, Pearson AL, Kingham S. An ecological study investigating the association between access to urban green space and mental health. Public Health. 2013;127(11):1005–11. doi: 10.1016/j.puhe.2013.08.016. 20. Wells, N At home with nature: effects of greenness on children’s cognitive functioning. [DOI] [PubMed] [Google Scholar]
- 24.Vaessen TJ, Overeem S, Sitskoom MM. Cognitive complaints in obstructive sleep apnea. Sleep Med Rev. 2014 doi: 10.1016/j.smrv.2014.03.008. S1087-0792(14)00041-0. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 25.Wheeler B, White M, Stahl-Timmins W, Depledge M. Does living by the coast improve health and wellbeing? Health and Place. 2012;18(5):1198–201. doi: 10.1016/j.healthplace.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 26.Buxton OM, Broussard JL, Zahl AK, Hall M. Effects of Sleep Deficiency on Hormones, Cytokines, and Metabolism. In: Redline S, Berger N, editors. Impact of Sleep and Sleep Disturbances on Obesity and Cancer. Effects of Sleep Deficiency on Hormones, Cytokines, and Metabolism. New York: Springer; 2014. [Google Scholar]
- 27.Gilbert SS, van den Heuvel CJ, Ferguson SA, Dawson D. Thermoregulation as a sleep signaling system. Sleep Med Rev. 2004;8:81–93. doi: 10.1016/S1087-0792(03)00023-6. [DOI] [PubMed] [Google Scholar]
- 28.Okamoto-Mizuno K, Mizuno K. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol. 2012;31:14. doi: 10.1186/1880-6805-31-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okamoto-Mizuno K, Mizuno K, Michie S, Maeda A, Iizuka S. Effects of humid heat exposure on human sleep stages and body temperature. Sleep. 1999;22:767–73. [PubMed] [Google Scholar]
- 30.Okamoto-Mizuno K, Mizuno K. Sleep and environment. Treatment Strategies – Resp. 2011;2:87–89. [Google Scholar]
- 31.Hollwich F. The Influence of ocular light perception on metabolism in man and in animal. New York: Springer-Verlag; 1979. [Google Scholar]
- 32.Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;210(4475):1267–69. doi: 10.1126/science.7434030. [DOI] [PubMed] [Google Scholar]
- 33.Wetterberg L. Light and biological rhythms. J Int Med. 1994;235(1):5–19. doi: 10.1111/j.1365-2796.1994.tb01027.x. [DOI] [PubMed] [Google Scholar]
- 34.Brzezinski M. Melatonin in humans. NEJM. 1997;336(3):186–195. doi: 10.1056/NEJM199701163360306. [DOI] [PubMed] [Google Scholar]
- 35.Dumont M, Beaulieu C. Light exposure in the natural environment: Relevance to mood and sleep disorders. Sleep Med. 2007;8:557–565. doi: 10.1016/j.sleep.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 36.Partonen T, Pandi-Perumal SR. Seasonal Affective Disorder: Practice and Research. New York: Oxford University Press; 2009. [Google Scholar]
- 37.Harrison Y. The relationship between daytime exposure to light and night-time sleep in 6–12 week old infants. J Sleep Res. 2004;13:345–352. doi: 10.1111/j.1365-2869.2004.00435.x. [DOI] [PubMed] [Google Scholar]
- 38.Mongrain V, Paquet J, Dumont M. Contribution of the photoperiod at birth to the association between season of birth and diurnal preference. Neuroscience Letters. 2006;406:113–116. doi: 10.1016/j.neulet.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 39.Mishima K, Okawa M, Shimizu T, Hishikawa Y. Diminished melatonin secretion in the elderly caused by insufficient environmental illumination. J Clinl Endocrinol Metab. 2001 Jan;186:129–134. doi: 10.1210/jcem.86.1.7097. [DOI] [PubMed] [Google Scholar]
- 40.Shochat T, Martin J, Marler M, Ancoli-Israel S. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res. 2000 Dec;9(4):373–379. doi: 10.1046/j.1365-2869.2000.00221.x. [DOI] [PubMed] [Google Scholar]
- 41.Kasper S, Wehr TA, Bartko JJ, Gaist PA, Rosenthal NE. Epidemiological findings of seasonal changes in mood and behavior. Arch Gen Psychiatry. 1989 Sep;46:823–833. doi: 10.1001/archpsyc.1989.01810090065010. [DOI] [PubMed] [Google Scholar]
- 42.Wehr TA, Duncan WC, Sher L, Aeschbach D, Schwartz PJ, Turner EH, Postolache TT, Rosenthal NE. A circadian signal of change in season in patients with seasonal affective disorder. Arch Gen Psychiatry. 2001 Dec;58:1108–1114. doi: 10.1001/archpsyc.58.12.1108. [DOI] [PubMed] [Google Scholar]
- 43.Schernhammer ES, Schulmeister K. Melatonin and cancer risk: does light at night compromise physiologic cancer protection by lowering serum melatonin levels? Br J Cancer. 2004 Mar;90:941–943. doi: 10.1038/sj.bjc.6601626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Surveillance for Certain Health Behaviors Among States and Selected Local Areas — United States, 2010. MMWR. 2013;62(SS1-251) [PubMed] [Google Scholar]
- 45.Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment: Recommendations from the behavioral risk factor surveillance team. Morbidity and Mortality Weekly Report. 2003 May;52(RR-9):1–12. [PubMed] [Google Scholar]
- 46.Behavioral Risk Factor Surveillance System 2010 Summary Data Quality Report. CDC; 2010. ftp://ftp.cdc.gov/pub/data/brfss/2010_summary_data_quality_report.pdf’. [Google Scholar]
- 47.Knutson KL. Sociodemographic and cultural determinants of sleep deficiency: Implications for cardiometabolic risk. Soc Sci Med. 2013;79:7–15. doi: 10.1016/j.socscimed.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mašková Z, Zemek F, Květ J. Normalized difference vegetation index (NDVI) in the management of mountain meadows. Boreal Env Res. 2008;13:417–32. [Google Scholar]
- 49.Williams D. Landstat-7 Science Data Users Handbook. Greenbelt, MD: NASA/Goddard Space Flight Center; 2005. http://landsathandbook.gsfc.nasa.gov/pdfs/Landsat7_Handbook.pdf. [Google Scholar]
- 50.Global Land Cover Facility. Earth Science Daily Interface. http://glcfapp.glcf.umd.edu:8080/esdi/index.jsp.
- 51.Geiger SD, Sabanayagam C, Shankar A. The Relationship between Insufficient Sleep and Self-Rated Health in a Nationally Representative Sample. J Environ Public Health. 2012;2012:518263. doi: 10.1155/2012/518263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention (CDC) Perceived insufficient rest or sleep among adults-United States, 2008. Journal of the American Medical Association. 2009;302:2532–2539. [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention (CDC) Perceived insufficient rest or sleep—four states, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:200–203. [PubMed] [Google Scholar]
- 54.Pereira G, Foster S, Martin K, Christin H, Boruff BJ, Knuiman M, Giles-Corti B. The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health. 2012;12:466. doi: 10.1186/1471-2458-12-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hartig T, Evans GW, Jamner LD, Davis DS, Garling T. Tracking restoration in natural and urban field settings. J Environ Psych. 2003;23:109–23. [Google Scholar]
- 56.de Vries S, Verheij RA, Groenewegen PP, Spreeuwenberg P. Natural environments -- healthy environments? An exploratory analysis of the relationship between greenspace and health. Environ Plan A. 2003;35(10):1717–31. [Google Scholar]
- 57.Astell-Burt T, Feng X, Kolt GS. Does access to neighbourhood green space promote a healthy duration of sleep? Novel findings from a cross-sectional study of 259,319 Australians. BMJ Open. 2013;3(8):e003094. doi: 10.1136/bmjopen-2013-003094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roman CG, Chalfin A. Fear of walking outdoors. A multilevel ecologic analysis of crime and disorder. Am J Prev Med. 2008 Apr;34(4):306–12. doi: 10.1016/j.amepre.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 59.Wanko NS, Brazier CW, Young-Rogers D, Dunbar VG, Boyd B, George CD, Rhee MK, el-Kebbi IM, Cook CB. Exercise preferences and barriers in urban African Americans with type 2 diabetes. Diabetes Educ. 2004;30(3):502–13. doi: 10.1177/014572170403000322. [DOI] [PubMed] [Google Scholar]
- 60.Astell-Burt T, Mitchell R, Hartig T. The association between green space and mental health varies across the lifecourse. A longitudinal study. J Epidemiol Community Health. 2014;68(6):578–83. doi: 10.1136/jech-2013-203767. [DOI] [PubMed] [Google Scholar]
- 61.Van den Berg JF, Miedema HM, Tulen JH, Hofman A, Neven AK, Tiemeier H. Sex differences in subjective and actigraphic sleep measures: a population-based study of elderly persons. Sleep. 2009;32(10):1367–75. doi: 10.1093/sleep/32.10.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Voderholzer U, Al-Shajlawi A, Weske G, Feige B, Riemann D. Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depress Anxiety. 2003;17(3):162–72. doi: 10.1002/da.10101. [DOI] [PubMed] [Google Scholar]
- 63.Kaplan R, Kaplan S. The Experience of nature: A Psychological Perspective. New York: Cambridge University Press; 1989. [Google Scholar]
- 64.Kaplan S. The restorative benefits of nature: toward an integrative framework. J Environ Psych. 1995;15:169–182. [Google Scholar]
- 65.Ulrich RS. View through a window may influence recovery from surgery. Science. 1983;224:420–21. doi: 10.1126/science.6143402. [DOI] [PubMed] [Google Scholar]
- 66.Ulrich RS, Simons RF, Losito BD, Fiorito E, Miles MA, Zelson M. Stress recovery during exposure to natural and urban environments. J Environ Psych. 1991;11:201–30. [Google Scholar]
- 67.Park BJ, Tsunetsugu Y, Kasetani T, Kagawa T, Miyazaki Y. The physiological effects of Shinrin-yoku (taking in the forest atmosphere or forest bathing): evidence from field experiments in 24 forests across Japan. Environ Health Prev Med. 2010;15(1):18–26. doi: 10.1007/s12199-009-0086-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kalsbeek A, Yi CX, la Fleur SE, Buijs RM, Fliers E. Suprachiasmatic nucleus and autonomic nervous system influences on awakening from sleep. Int Rev Neurobiol. 2010;93:91–107. doi: 10.1016/S0074-7742(10)93004-3. [DOI] [PubMed] [Google Scholar]
- 69.Astell-Burt T, Feng X, Kolt GS. Is neighborhood green space associated with a lower risk of type 2 diabetes? Evidence from 267,072 Australians. Diabetes Care. 2014;37(1):197–201. doi: 10.2337/dc13-1325. [DOI] [PubMed] [Google Scholar]
- 70.Godbey G. Understanding and enhancing the relationship. Resources for the Future (RFF); 2009. Outdoor recreation, health and wellness. http://www.rff.org/documents/RFF-DP-09-21.pdf. [Google Scholar]