Abstract
Introduction
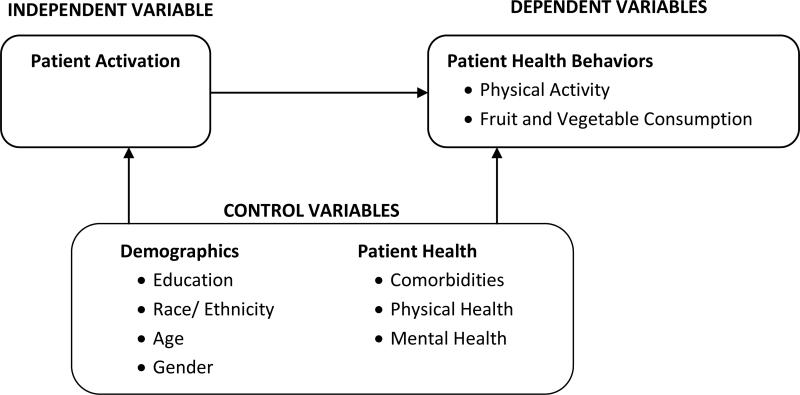
We examine the association of patient activation and physical activity and fruit and vegetable consumption among obese safety net patients.
Methods
Adult obese patients (n=198) of three safety net clinics completed a survey assessing patient activation, physical activity, fruit and vegetable consumption, care experiences, and health status. Multivariate logistic regression models incrementally assessed the adjusted relation of patient activation and physical activity and fruit and vegetable consumption.
Results
In adjusted analyses, higher activated patients had higher odds [Odds ratio (OR) = 1.58, p<0.01] of consuming fruits and vegetables daily than less activated patients. There was no significant association between patient activation and regular physical activity.
Discussion
Engaging in regular physical activity appears to be difficult, even for highly activated patients. In contrast, additional fruit and vegetable consumption is a relatively easier change.
Conclusion
Patient activation was inconsistently associated with two positive health behaviors among obese safety net patients.
Keywords: Patient activation, physical activity, safety net clinics, practice redesign, health behaviors, minority health
Background
As the U.S. health care system has shifted its focus from acute care to chronic care, primary care practices are increasingly interested in more effectively managing the obesity epidemic.1, 2 Obesity is linked to numerous health risks, particularly the development and exacerbation of chronic conditions such as hypertension, diabetes, high cholesterol, and more. 3 Delivery system design and self-management support are the Chronic Care Model (CCM) components most consistently associated with positive patient outcomes.4, 5 Self-management support for obese and chronically ill patients, however, has been especially challenging for primary care practices to integrate, particularly safety net clinics serving vulnerable, low-income patients. In national surveys of physician organizations, few small and medium-sized primary care practices had self-management supports available for chronically ill patients.5, 6 To inform the implementation of self-management resources for obese safety net patients, we examined the relation of patient activation and health behaviors in the early stages of a practice redesign. The goals of the practice redesign were to support patient goal-setting to increase physical activity through structured support from trained medical assistants (MAs) as extensions of patients’ routine primary care visits, and to connect patients to clinic and community resources for physical activity improvement.
Conceptual framework
Practice stakeholders from three county-run primary care safety net clinics in Northern California were interested in understanding baseline patient activation among obese patients targeted for health coaching by MAs. Safety net clinics, such as county-run clinics for the poor and underserved, federally qualified health centers (FQHCs), and other practices, all tend to serve high proportions of vulnerable patients with high rates of chronic disease, including many racial and ethnic minorities. Patients need to be engaged and have a high level of interest and involvement in improving their health to effectively engage in goal-setting for behavior change.7, 8 Patient activation, an important component of patient engagement, encompasses patient ability and readiness to self-manage multiple dimensions of their health. Patient activation has been linked to positive health behaviors: more highly activated patients are shown to engage in positive health care and health behaviors such as preventive screenings, regular physical activity, and eating healthy foods.8-10 Additionally, higher quality clinician-patient communication has been linked to higher patient activation and better health outcomes.11-13
Limited evidence, however, exists about the relation of patient activation and health behaviors among the racially and ethnically diverse low-income safety net patient population that may face more barriers in translating their high activation into positive health behaviors. Based on previous evidence of the impact of patient activation in other populations, we hypothesized that more highly activated obese patients would be more likely to engage in regular physical activity and consume more fruits and vegetables compared to less activated obese patients.
Patients with multiple chronic conditions sometimes have physical limitations that make regular exercise difficult to initiate and maintain. We hypothesized that obese patients with clinical comorbidities that were highly activated would be less likely to engage in physical activity compared to highly activated patients with fewer comorbidities.
Methods
Data Collection
English- and Spanish-language surveys were mailed using a three-wave protocol to eligible patients at the three safety net clinics during the early implementation period in April to June 2012. The first mailing included a $10 gift card as a pre-completion incentive. In order to maintain patient privacy, patients were assigned random identifiers that were used to label the questionnaires. In order to keep patient responses confidential and anonymous to researchers, and due to the safety net organization's IRB office concerns about providing patient address information to researchers without their consent, questionnaires were mailed to patients by staff from the participating clinics. Completed questionnaires were mailed directly to the research team without any patient-identifying information. All study procedures and survey instruments were reviewed and approved by the IRBs at both UCLA and the county health system.
Participants
A random sample of adult patients (n=393) were selected from the three safety net clinics’ administrative databases with the following restrictions: at least two clinic encounters in the past 12 months, age 18 and over, and body mass index (BMI) of 30 to 34. These inclusion criteria were used to target mildly obese patients that were most likely to be ready to make health behavior changes through health coaching and be exposed to practice changes as part of their ongoing care. We excluded patients with conditions that directly impacted weight, including pregnancy in the last year, hyperthyroidism, and cancer. Of the initial sample of 393 obese patients, 8.4% (n=33) surveys were returned due to invalid addresses. The analytic sample includes a total of 198 respondents for an adjusted survey response rate of 55.3%.
Measures
The survey included previously validated questions of patient activation, physical activity, fruit and vegetable consumption, clinician-patient communication, health status, and demographics.
Main independent variable
The Patient Activation Measure (PAM) was developed by Hibbard, et al., as a way to quantify patient activation.14-16 PAM is validated in different populations and has been shown to be reliable with a Cronbach's alpha of 0.87.14, 15, 17, 18 The levels of activation are similar to the Transtheoretical Model, where individuals progress through stages before changing their behavior, such as quitting smoking.19 Individuals are thought to move through these stages of activation in order, although stages may change with time and stressful circumstances could lower patient activation.14, 17
We measured patient activation was measured using the PAM-13, a validated short form of the PAM.15 In our patient sample, the PAM-13 continuous measure had a Cronbach's alpha of 0.94 and the continuous measure was used for the regression analyses. Because practice stakeholders were interested in assessing differences in health behaviors by patient activation “levels,” the overall composite score was also categorized into a 4-part ordinal variable, representing lower vs. higher activation levels. An individual in the lowest level of activation is a passive participant in health care decisions. An individual in the second level of activation has the knowledge and confidence to take a more active role in their health care, but has not yet acted on it. In the third level of activation, the patient plays an active role in making health care decisions with their providers. The highest level of activation describes a patient who has the knowledge and confidence to take action about their own health care, even during times of stress.14
Outcome measures
The association of patient activation and two different patient-reported health behaviors were examined: physical activity and fruit and vegetable consumption. Patients’ physical activity level was measured using two questions adapted from the Exercise Vital Sign that assesses the frequency and duration of moderate to vigorous physical activity.20 A patient was categorized as physically active if they reported at least 150 minutes per week, which meets the national recommended level of physical activity for adults. Fruit and vegetable consumption, based on the Starting the Conversation21 survey, was assessed as a secondary outcome measure. Regular fruit and vegetable consumption was defined as eating fruits and vegetables at least seven times per week.
Other independent variables
Clinician-patient communication
We used the core communication composite of the Clinician and Group version of the Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) survey to assess the clinician-patient communication.22, 23 The responses to the questions were re-scaled to 0-100 and averaged to create the composite measure, where higher scores indicated higher quality clinician-patient communication.
General Health
The SF-12v2, a previously validated measure of overall health, was used to measure health status and limitations to daily activities due to emotional or physical health issues.24
Demographics
The questionnaire also covered patient demographics, including level of education, race and ethnicity, primary language spoken at home, and self-reported chronic conditions. Clinic administrative data provided age, gender, and BMI. Spanish translations were available for measures on patient experiences, patient activation, Medical Outcomes Study 12-Item Short Form Version 2 (SF-12v2), height, weight, diet, language preference and education. The remaining measures of physical activity, chronic conditions and race were independently translated by two research staff bilingual and biliterate in Spanish who then reached a consensus about the proper translation from English to Spanish.
Data analysis
Multivariate logistic regression models were estimated using a nested approach. Because we were concerned about overfitting models due to the modest sample size, we examined four separate regression models assessing the relation of patient activation and each outcome. The first model assessed the relation of patient activation and each outcome. The second model added the CG-CAHPS clinician-patient communication composite. The third model added demographic covariates. The final model added patient health factors. A correlation matrix indicated no strong correlations (all less than 0.40) among covariates used in the regression models.
To assess the extent to which more highly activated patients with a greater number of clinical co-morbidities were less likely to be physically active compared to other patients, an interaction term to account for the relationship between each patient activation level and the patients’ comorbidity count was included. Importantly, BMI was not included in regression analyses because the sample was restricted to patients within a limited range of BMI scores (30-34). Analyses were conducted using Stata 12; odds ratios (OR) were evaluated for main effects and predicted probabilities (PP) were evaluated for interaction effects.
Sensitivity analyses
PAM scoring guidelines recommend caution when considering PAM scores with all PAM item responses at the ceiling (100 score) or the floor (0 score). We re-ran analyses using this restricted sample and examined the extent to which these results (n=177) differed from the main analytic sample (n=198). We examined the extent to which results differed when restricting the sample accordingly.
Results
Table 1 compares patient characteristics based on patient activation level. The mean PAM score among respondents was 63.2 (SD=22.0), which is within the third level of activation (second highest). The largest proportion (38%) of respondents scored in the highest level of the four levels of activation. Spanish-speaking Latinos had higher mean PAM scores (mean=66.8, SD=24.5) than English-speaking Latinos (mean=59.1, SD=18.6). Most of the individuals with a college degree or higher scored within the highest two levels of activation, but there are no significant differences in education by activation level (see Table 1). Patients with more comorbidities tended to be more activated. For example, more diabetic patients were in activation “level three” compared to activation “level one.” Based on a two-sample t-test, there were no statistically significant differences between survey respondents and non-respondents in terms of age, gender, or preferred language.
Table 1.
Population Characteristics Stratified by Patient Activation Level (N=198)
| Characteristic | Overall | Level 1 | Level 2 | Level 3 | Level 4 | P-valuea |
|---|---|---|---|---|---|---|
| Overall Population (%) | 100 | 18 | 11 | 33 | 38 | |
| Clinic (%) | 0.83 | |||||
| A | 30 | 31 | 33 | 33 | 23 | |
| B | 27 | 34 | 19 | 23 | 31 | |
| C | 41 | 34 | 48 | 42 | 45 | |
| PATIENT-PROVIDER RELATIONSHIP | ||||||
| Clinician-patient communication (modified CG-CAHPS score 0-100) | 89.5 | 82.0 | 80.6 | 89.0 | 95.6 | 0.00a |
| Trust clinicians at clinic (%) | 89 | 77 | 74 | 93 | 96 | 0.00*** |
| DEMOGRAPHICS | ||||||
| Race/Ethnicity (%) | 0.04 | |||||
| Latino – Spanish speaking | 38 | 26 | 38 | 42 | 43 | |
| Latino – English speaking | 30 | 31 | 52 | 28 | 23 | |
| Non-Latino White | 14 | 23 | 5 | 6 | 19 | |
| Non-Latino Other | 14 | 20 | 5 | 23 | 15 | |
| Primary language spoken at home (%) | 0.55 | |||||
| English | 44 | 51 | 33 | 41 | 46 | |
| Spanish | 38 | 29 | 38 | 45 | 36 | |
| Other | 18 | 20 | 29 | 14 | 18 | |
| Female (%) | 70 | 73 | 70 | 77 | 63 | 0.35 |
| Age (years) | 49 | 49 | 46 | 50 | 49 | 0.51 |
| Education (%) | 0.01** | |||||
| Less than high school | 42 | 28 | 55 | 53 | 38 | |
| High school graduate/ GED | 23 | 33 | 35 | 15 | 23 | |
| Some college | 23 | 33 | 10 | 26 | 20 | |
| College graduate or more | 11 | 6 | 0 | 6 | 19 | |
| Length of time attended clinic (%) | 0.83 | |||||
| <6 months | 4 | 3 | 0 | 2 | 5 | |
| 6 months – 1 year | 4 | 9 | 10 | 3 | 1 | |
| 1 year – 3 years | 47 | 54 | 43 | 46 | 46 | |
| 3 years – 5 years | 22 | 11 | 24 | 29 | 22 | |
| > 5 years | 23 | 23 | 24 | 21 | 26 | |
| HEALTH | ||||||
| Number of comorbidities (%) | 0.82 | |||||
| 0 | 13 | 9 | 14 | 11 | 12 | |
| 1 | 24 | 26 | 24 | 30 | 19 | |
| 2 | 20 | 29 | 19 | 17 | 18 | |
| 3+ | 44 | 37 | 43 | 42 | 52 | |
| Diabetes (%) | 41 | 26 | 33 | 53 | 42 | 0.05* |
| Hypertension (%) | 48 | 43 | 43 | 52 | 51 | 0.76 |
| High cholesterol (%) | 47 | 49 | 38 | 45 | 51 | 0.72 |
| BMI (kg/m2) | 32.3 | 32.4 | 32.3 | 32.3 | 32.3 | 0.37 |
| SF-12 Dimensions (mean score) | ||||||
| Physical Component Summary Score | 42.1 | 40.0 | 42.7 | 41.6 | 43.1 | 0.08* |
| Mental Component Summary Score | 42.0 | 39.9 | 41.2 | 44.2 | 41.5 | 0.13 |
p<0.10
p<0.05
p<0.01
Chi-square analysis or one-way ANOVA
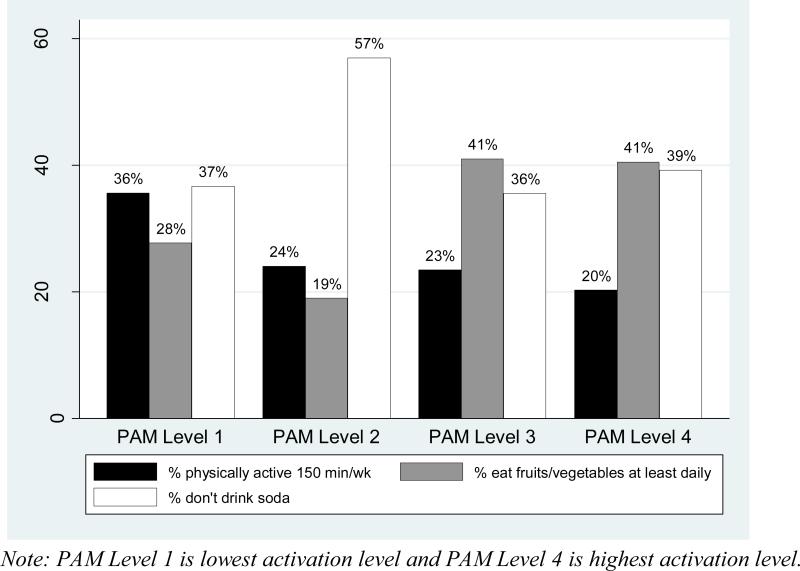
Physical activity
There was no association between physical activity and patient activation in unadjusted or adjusted analyses (see Table 2). However, in adjusted analyses, relative to males, females had fewer odds of being physically active (OR=0.40, p<0.05) and older patients had fewer odds of being physically active (OR=0.58, p<0.05). Since the unadjusted model with the interaction of patient activation and comorbidities was not statistically significant, the interaction variable was dropped from the analyses.
Table 2.
Comparison of Odds Ratios of Patient Activation Level on Physical Activity
| VARIABLE | MODEL 1 | MODEL 2 | MODEL 3 | MODEL 4 |
|---|---|---|---|---|
| PATIENT ACTIVATION LEVEL | ||||
| PAM-13 | 1.04 (0.73, 1.49) | 1.11 (0.74, 1.66) | 0.94 (0.63, 1.42) | 0.96 (0.63, 1.49) |
| PATIENT-PROVIDER RELATIONSHIP | ||||
| Clinician-patient communication (modified CG-CAHPS score) | 0.80 (0.55, 1.16) | 0.94 (0.62, 1.43) | 0.93 (0.61, 1.42) | |
| DEMOGRAPHICS | ||||
| Race/ ethnicity | ||||
| Latino – Spanish speaking | 2.48 (0.48, 12.80) | 2.50 (0.47, 13.28) | ||
| Latino – English speaking | 1.29 (0.28, 5.94) | 1.33 (0.28, 6.31) | ||
| Non-Latino White | Ref | Ref | ||
| Non-Latino Other | 0.82 (0.14, 4.72) | 0.89 (0.15, 5.37) | ||
| Female | 0.42** (0.17, 0.99) | 0.40** (0.16, 0.98) | ||
| Age | 0.63** (0.43, 0.93) | 0.58** (0.38, 0.89) | ||
| Education | ||||
| Less than high school | Ref | Ref | ||
| High school graduate/ GED | 0.50 (0.13, 1.93) | 0.45 (0.12, 1.77) | ||
| Some college | 0.83 (0.23, 3.07) | 0.89 (0.23, 3.42) | ||
| 4-year college degree or more | 1.72 (0.41, 7.21) | 1.79 (0.42, 7.56) | ||
| HEALTH | ||||
| Comorbidities (at least one) | 2.36 (0.51, 10.85) | |||
| SF-12 Dimensions | ||||
| Physical Component Summary Score | 0.87 (0.54, 1.41) | |||
| Mental Component Summary Score | 0.74 (0.47, 1.18) | |||
| MODEL FIT STATISTICS | ||||
| Log likelihood | −95.71 | −89.05 | −78.53 | −76.02 |
| AIC | 195.43 | 184.10 | 179.07 | 180.03 |
| Pseudo R2 | 0.00 | 0.00 | 0.10 | 0.12 |
| Pr >chi2 | 0.82 | 0.50 | 0.07 | 0.10 |
| Observations | 193 | 185 | 180 | 174 |
* p<0.10
p<0.05
Fruit and vegetable consumption
Higher patient activation was related to greater fruit and vegetable consumption. In the unadjusted model, patients with higher patient activation scores had greater odds (OR=1.58, p<0.01) of greater fruit and vegetable consumption (see Table 3). The significance of this relationship attenuated (p<0.10) with the inclusion of covariates. In adjusted analyses, the only statistically significant covariate relationship with fruit and vegetable consumption was race/ethnicity (see Table 3). Relative to non-Latino Whites, English-speaking Latinos (OR=0.17, p<0.01) and individuals in the Other racial/ethnic category had lower odds (OR=0.08, p<0.01) of consuming fruits and vegetables regularly.
Table 3.
Comparison of Odds Ratios of Patient Activation Level on Daily Fruit and Vegetable Consumption
| VARIABLE | MODEL 1 | MODEL 2 | MODEL 3 | MODEL 4 |
|---|---|---|---|---|
| PATIENT ACTIVATION LEVEL | ||||
| PAM-13 | 1.58*** (1.13, 2.22) | 1.54** (1.07, 2.23) | 1.39* (0.94, 2.04) | 1.48* (0.97, 2.25) |
| PATIENT-PROVIDER RELATIONSHIP | ||||
| Clinician-patient communication (modified CG-CAHPS score) | 1.09 (0.74, 1.62) | 1.35 (0.87, 2.11) | 1.26 (0.82, 1.95) | |
| DEMOGRAPHICS | ||||
| Race/ ethnicity | ||||
| Latino – Spanish speaking | 0.46 (0.14, 1.57) | 0.47 (0.13, 1.66) | ||
| Latino – English speaking | 0.22*** (0.07, 0.69) | 0.17*** (0.05, 0.56) | ||
| Non-Latino White | Ref | Ref | ||
| Non-Latino Other | 0.07*** (0.01, 0.38) | 0.08*** (0.01, 0.41) | ||
| Female | 0.69 (0.31, 1.51) | 0.61 (0.27, 1.37) | ||
| Age | 0.91 (0.63, 1.31) | 0.82 (0.55, 1.23) | ||
| Education | ||||
| Less than high school | Ref | Ref | ||
| High school graduate/ GED | 0.73 (0.24, 2.18) | 0.72 (0.23, 2.21) | ||
| Some college | 0.64 (0.20, 2.06) | 0.58 (0.16, 2.04) | ||
| 4-year college degree or more | 0.63 (0.15, 2.56) | 0.65 (0.16, 2.73) | ||
| HEALTH | ||||
| Comorbidities (at least one) | 1.81 (0.43, 7.62) | |||
| SF-12 Dimensions | ||||
| Physical Component Summary Score | 0.86 (0.54, 1.35) | |||
| Mental Component Summary Score | 0.99 (0.63, 1.56) | |||
| MODEL FIT STATISTICS | ||||
| Log likelihood | −111.91 | −105.53 | −92.68 | −87.37 |
| AIC | 227.81 | 217.05 | 207.36 | 202.74 |
| Pseudo R2 | 0.03 | 0.04 | 0.13 | 0.15 |
| Pr >chi2 | 0.01 | 0.02 | 0.00 | 0.00 |
| Observations | 189 | 181 | 176 | 170 |
p<0.10
p<0.05
p<0.01
Sensitivity analyses
Using the restricted sample (removing PAM scores at the ceiling and floor), the results remained fairly consistent in the model examining physical activity, with a slight change in magnitude of the odds and statistical significance for females (OR=0.41, p<0.10) and older patients (OR=0.66, p<0.10). The results from the model examining fruit and vegetable consumption remained consistent with the restricted sample (data not shown).
Discussion
Among obese safety net patients, there was no relationship between patient activation and regular physical activity. This is in contrast with previous research in more socioeconomically advantaged patient populations, where more highly activated patients are more likely to engage in regular physically activity.8, 14, 25, 26 We hypothesized that highly activated obese patients with clinical comorbidities would be less likely to engage in regular physical activity compared to highly activated obese patients without clinical comorbidities, Our results indicate that the presence of comorbidities does not impact physical activity behavior in this population.
More highly activated patients were much more likely to consume of fruits and vegetables regularly, which is consistent with other research among non-safety net patients.14 The strong and positive relationship between patient activation and fruit and vegetable consumption in comparison to physical activity may be because the health behavior is relatively easy to adopt. Regular fruit and vegetable consumption only requires the addition of food to existing meals, whereas increasing physical activity requires integrating a new daily routine requiring exertion. Even when safety net patients are highly activated, regular physical activity may not be possible due to safety concerns which presents an immediate and pressing health concern.27 Further research into assessing low-income, obese patients for physical activity behavior change is needed to better inform future interventions.
Patient activation was relatively high in our obese safety net patient sample. The average participant scored within activation level three, indicating they had some self-management skills but still needed support for self-management during times of stress or change.10, 11, 28 This population of both English- and Spanish-speakers has a similar distribution of activation scores as those reported in previous studies in English-speaking populations. In contrast to other published findings, Spanish-speaking Latinos in this study have a higher PAM score than English-speaking Latinos, which may possibly be related to regional differences in the Latino populations studied, since Latinos in this population tended to have family roots in Mexico while the Latino populations described in the other studies may have had more diverse backgrounds.29, 30 Also inconsistent with previous research,31, 32 the Latino patients in this study averaged a slightly higher unadjusted mean PAM score than non-Latino Whites. Although previous studies speculated that Latino patients might have lower activation scores due to a lack of engagement with their health care providers, the clinics in this study may have made additional efforts to engage Latino patients due to the high proportion of Latino patients at the clinics. This hypothesized increase in engagement could have positively influenced patient activation scores. There was also limited relation of clinician-patient communication and health behaviors, again contrasting previous publications that found that providers familiar with their patients’ medical histories are likely to be more invested in the care of their patients.11, 33 Despite significant relationships between patient activation and clinician-patient communication in bivariate analyses, clinician-patient communication was not associated with regular physical activity or fruit and vegetable consumption in adjusted analyses.
Our results should be considered in light of some limitations. First, it is possible that patients may have overreported their physical activity and activation,10 The normal distributions observed of these variables reduces the likelihood of social desirability response bias, i.e., we would have observed skewed data otherwise. Second, the small sample size may also present insufficient statistical power to detect clinically meaningful relationships, i.e., the interaction of clinical comorbidities and patient activation. For that reason, we chose to note statistically significant findings at the p<0.10 level. Despite the small sample size, this study is novel in its examination of PAM and health behaviors among the safety net patient population. We are not aware of other published studies in this area. Future research should examine the relation of patient activation and health behaviors in larger samples of low-income patients and use a longitudinal perspective to examine differences in health behavior change by activation level.
New Contribution to the Literature
Patient activation has previously been associated with positive health behaviors such as aerobic exercise and receiving preventive cancer screenings, as well as more favorable emotional health.9, 17, 18 Our findings in a safety net population differ from previous research. While greater patient activation was related to more regular fruit and vegetable consumption, higher patient activation did not translate into greater regular physical activity in our study. Our study adds to the limited knowledge about the relationship between patient activation and health behaviors among low-income, diverse safety net clinic patients. As noted in past studies, the relation of patient activation and positive health behaviors is sometimes not linear.34 The relationship between patient activation and greater fruit and vegetable consumption may have been due to the relative ease of translating activation into behavior change for eating behavior compared to more difficult tasks like increasing physical activity.
Fig. 1.
Conceptual Model
Fig. 2.
Distribution of Outcome Variables by Patient Activation Level
Acknowledgements
The authors would like to thank Lindsay Kimbro and Socorro Ochoa for their assistance in the questionnaire development and translation process. Thanks to Ms. Kimbro, Ms. Ochoa, and clinic leaders for their assistance in the data collection process. Finally, thanks to the patients for their interest and participation in the survey process.
This research was funded by the NIH/National Heart, Lung, and Blood Institute: California Comparative Effectiveness and Outcomes Improvement (CEOI) Center Grant #RC2HL101811. Author AuYoung was supported by the UCLA Graduate Division Dissertation Year Fellowship.
Footnotes
We have no conflicting or competing interests to report.
References
- 1.Coleman K, Austin BT, Brach C, Wagner EH. Evidence On The Chronic Care Model In The New Millennium. Health Affairs. 2009;28:75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rothman AA, Wagner EH. Chronic Illness Management: What is the Role of Primary Care? Ann Intern Med. 2003:183. doi: 10.7326/0003-4819-138-3-200302040-00034. [DOI] [PubMed] [Google Scholar]
- 3.Desouza CV, Padala PR, Haynatzki G, Anzures P, Demasi C, Shivaswamy V. Role of Apathy in the Effectiveness of Weight Management Programmes. Diabetes, Obesity, and Metabolism. 2012:14. doi: 10.1111/j.1463-1326.2011.01544.x. [DOI] [PubMed] [Google Scholar]
- 4.Tsai AC, Morton SC, Mangione CM, Keeler EB. A Meta-Analysis of Interventions to Improve Care for Chronic Illnesses. Am J Managed Care. 2005:11. [PMC free article] [PubMed] [Google Scholar]
- 5.Rittenhouse DR, Casalino LP, Shortell SM, et al. Small And Medium-Size Physician Practices Use Few Patient-Centered Medical Home Processes. Health Affairs. 2011;30:1575–84. doi: 10.1377/hlthaff.2010.1210. [DOI] [PubMed] [Google Scholar]
- 6.Shortell SM, Gillies R, Siddique J, et al. Improving Chronic Illness Care: A Longitudinal Cohort Analysis of Large Physician Organizations. Medical Care. 2009:42. doi: 10.1097/MLR.0b013e31819a621a. [DOI] [PubMed] [Google Scholar]
- 7.Carman KL, Dardess P, Maurer M, et al. Patient And Family Engagement: A Framework For Understanding The Elements And Developing Interventions And Policies. Health Affairs. 2013;32:223–31. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 8.Hibbard JH, Greene J. What The Evidence Shows About Patient Activation: Better Health Outcomes And Care Experiences; Fewer Data On Costs. Health Affairs. 2013;32:207–14. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 9.Greene J, Hibbard JH. Why Does Patient Activation Matter? An Examination of the Relationships Between Patient Activation and Health-Related Outcomes. Journal of General Internal Medicine. 2011;27:520–6. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rask KJ, Ziemer DC, Kohler SA, Hawley JN, Arinde FJ, Barnes CS. Patient Activation Is Associated With Healthy Behaviors and Ease in Managing Diabetes in an Indigent Population. The Diabetes Educator. 2009;35:622–30. doi: 10.1177/0145721709335004. [DOI] [PubMed] [Google Scholar]
- 11.Alexander JA, Hearld LR, Mittler JN, Harvey J. Patient-Physician Role Relationships and Patient Activation among Individuals with Chronic Illness. Health Services Research. 2012;47:1201–23. doi: 10.1111/j.1475-6773.2011.01354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tarn DM, Young HN, Craig BM. Development of the patient approach and views toward healthcare communication (PAV-COM) measure among older adults. BMC Health Services Research. 2012;12:289. doi: 10.1186/1472-6963-12-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood) 2010;29:1310–8. doi: 10.1377/hlthaff.2009.0450. [DOI] [PubMed] [Google Scholar]
- 14.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Services Research. 2004:39. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and Testing of a Short Form of the Patient Activation Measure. Health Services Research. 2005;40:1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hibbard JH, Mahoney E. Toward a theory of patient and consumer activation. Patient Education and Counseling. 2010;78:377–81. doi: 10.1016/j.pec.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 17.Chubak J, Anderson ML, Saunders KW, et al. Predictors of 1-Year Change in Patient Activation in Older Adults with Diabetes Mellitus and Heart Disease. Journal of the American Geriatrics Society. 2012;60:1316–21. doi: 10.1111/j.1532-5415.2012.04008.x. [DOI] [PubMed] [Google Scholar]
- 18.Munson GW, Wallston KA, Dittus RS, Speroff T, Roumie CL. Activation and Perceived Expectancies: Correlations with Health Outcomes Among Veterans with Inflammatory Bowel Disease. Journal of General Internal Medicine. 2009;24:809–15. doi: 10.1007/s11606-009-1002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson SS, Paiva AL, Cummins CO, et al. Transtheoretical Model-based multiple behavior intervention for weight management: Effectiveness on a population basis. Preventive Medicine. 2008;46:238–46. doi: 10.1016/j.ypmed.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sallis R. Developing healthcare systems to support exercise: exercise as the fifth vital sign. British Journal of Sports Medicine. 2011;45:473–4. doi: 10.1136/bjsm.2010.083469. [DOI] [PubMed] [Google Scholar]
- 21.Paxton AE, Strycker LA, Toobert DJ, Ammerman AS, Glasgow RE. Starting The Conversation. American Journal of Preventive Medicine. 2011;40:67–71. doi: 10.1016/j.amepre.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Browne K, Roseman D, Shaller D, Edgman-Levitan S. ANALYSIS & COMMENTARY Measuring Patient Experience As A Strategy For Improving Primary Care. Health Affairs. 2010;29:921–5. doi: 10.1377/hlthaff.2010.0238. [DOI] [PubMed] [Google Scholar]
- 23.Anastario MP, Rodriguez HP, Gallagher PM, et al. A Randomized Trial Comparing Mail versus In-Office Distribution of the CAHPS Clinician and Group Survey. Health Services Research. 2010;45:1345–59. doi: 10.1111/j.1475-6773.2010.01129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jenkinson C, Layte R, Jenkinson D, et al. A Shorter Form Health Survey: Can the SF-12 Replicate Results From the SF-36 in Longitudinal Studies? Journal of Public Health Medicine. 1997:19. doi: 10.1093/oxfordjournals.pubmed.a024606. [DOI] [PubMed] [Google Scholar]
- 25.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do Increases in Patient Activation Result in Improved Self-Management Behaviors? Health Services Research. 2007;42:1443–63. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harvey L, Fowles JB, Xi M, Terry P. When activation changes, what else changes? the relationship between change in patient activation measure (PAM) and employees’ health status and health behaviors. Patient Education and Counseling. 2012;88:338–43. doi: 10.1016/j.pec.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 27.Drieling RL, Ma J, Stafford RS. Evaluating clinic and community-based lifestyle interventions for obesity reduction in a low-income Latino neighborhood: Vivamos Activos Fair Oaks Program. BMC Public Health. 2011;11:98. doi: 10.1186/1471-2458-11-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deen D, Lu WH, Weintraub MR, Maranda MJ, Elshafey S, Gold MR. The impact of different modalities for activating patients in a community health center setting. Patient Education and Counseling. 2012;89:178–83. doi: 10.1016/j.pec.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Alegría M, Sribney W, Perez D, Laderman M, Keefe K. The Role of Patient Activation on Patient–Provider Communication and Quality of Care for US and Foreign Born Latino Patients. Journal of General Internal Medicine. 2009;24:534–41. doi: 10.1007/s11606-009-1074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lubetkin EI, Lu W-H, Gold MR. Levels and Correlates of Patient Activation in Health Center Settings: Building Strategies for Improving Health Outcomes. Journal of Health Care for the Poor and Underserved. 2010;21:796–808. doi: 10.1353/hpu.0.0350. [DOI] [PubMed] [Google Scholar]
- 31.Cunningham PJ, Hibbard J, Gibbons CB. Raising Low 'Patient Activation' Rates Among Hispanic Immigrants May Equal Expanded Coverage In Reducing Access Disparities. Health Affairs. 2011;30:1888–94. doi: 10.1377/hlthaff.2009.0805. [DOI] [PubMed] [Google Scholar]
- 32.Cunningham PJ, Hibbard JH. How Engaged Are Consumers in Their Health and Health Care, and Why Does It Matter? Center for Studying Health System Change; Washington, D.C.: 2008. [PubMed] [Google Scholar]
- 33.Otero-Sabogal R, Arretz D, Siebold S, et al. Physician-Community Health Worker Partnering to Support Diabetes Self-Management in Primary Care. Quality in Primary Care. 2010:18. [PubMed] [Google Scholar]
- 34.Dixon A, Hibbard J, Tusler M. How Do People with Different Levels of Activation Self-Manage their Chronic Conditions? Patient. 2009:2. doi: 10.2165/11313790-000000000-00000. [DOI] [PubMed] [Google Scholar]