Highlights
-
•
Stump appendicitis (SA) is a rare, but noteworthy, diagnosis that warrants early detection.
-
•
Delay in the diagnosis of SA may result in serious complications like stump gangrene, perforation and peritonitis.
-
•
More research is needed to identify strategies to prevent SA.
-
•
We underline the emergent role of lower endoscopy to clarify diagnosis resolve the symptoms.
-
•
Surgeons need to have a heightened awareness of the possibility of SA.
Keywords: Stump appendicitis, Endoscopic feature, Computed tomography
Abstract
Introduction
Today, the diagnosis of SA is usually not considered as the etiology for right lower quadrant pain in patient with history of appendectomy, resulting in delaying making the correct diagnosis and treatment. Obviously, other more common causes should be excluded first.
Discussion
Stump appendicitis (SA) was first described by Rose in 1945. The commonest presenting symptom are abdominal pain (right lower quadrant pain 59%, non specific abdominal pain 16%, and central abdominal pain radiating to the right lower quadrant 14%).
Presentation of case
A 54-year-old appendectomized woman presented with recent history of abdominal pain with periumbilical pain radiating to the right side and in the right iliac fossa, in the absence of fever, vomiting or other symptoms.
Elective colonoscopy revealed appendicular orifice clogged by big fecalith, with hyperemic surrounding mucosa and CT confirmed “stump appendicitis”. After 30 days of therapy with metronidazole 500 mg/day and mesalazine 1000 mg × 2/day, the patient was submitted to surgery and appendectomy was performed, with a specimen of 24 mm stump appendicitis.
Conclusion
SA may well be considered as one of the differential diagnoses of acute right lower abdominal pain even in patients with history of appendicectomy.
1. Introduction
Stump appendicitis is an under reported and poorly defined condition related to of obstruction and inflammation of the residual appendix after appendectomy [1], [2].
2. Presentation of case
A 54-year-old woman presented with history of abdominal pain of 21 days duration, accompanied by dysuria and urinary frequency and with recent (7 days) onset of diarrhea predominantly nocturnal with periumbilical pain radiating to the right side and in the right iliac fossa, in the absence of fever, vomiting or other symptoms. She had undergone laparotomy for acute appendicitis 46 years earlier.
She referred recurrent episodes of abdominal pain for the past 2 years and was being treated as irritable bowel disease (IBD).
Clinical examination was normal, except for a slight tenderness in the right iliac fossa, not associated with guarding or rigidity. Her pulse rate was 74/min; blood pressure 120/80 mm Hg and temperature was 36 °C. Total white cell count was 12,400 mm3 (90% neutrophils), PCR and VES were, respectively, 3 and 5 times the norm. Urine analysis was unremarkable and fecal occult blood test was negative.
2.1. Abdominal ultrasonography was not diagnostic
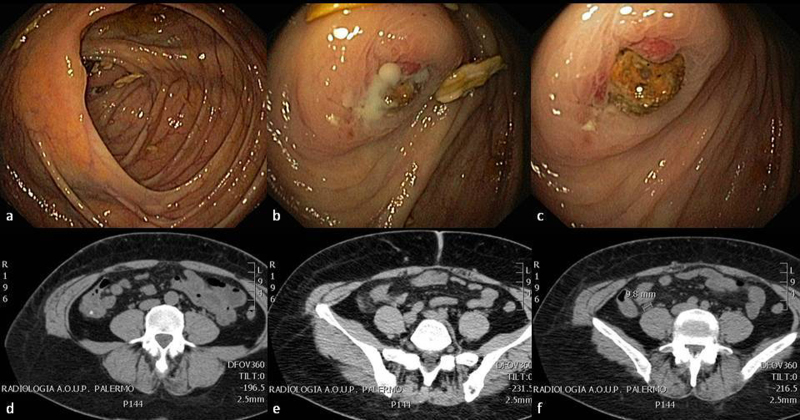
Elective colonoscopy (Fig. 1a) revealed an appendicular orifice clogged by big fecalith, with surrounding mucosa characterized by acute inflammatory phenomena (hyperemia, edema with multiple erosions and extreme mucosal fragility). After water-jet-washing over and around the orifice, a purulent oozing started from the lumen of the stump (about 10 ml). Therefore, several cycles of washing-suction has not been able to completely remove the fecalith (Fig. 1b, c).
Fig. 1.
(a) Cecum, appendicular orifice and ileo-cecal valve; (b) purulent oozing from appendicular orifice; (c) inflammatory phenomena of mucosa surrounding appendicular orifice; (d) fecalith; (e) pericaecal fat stranding; (f) cecal lymphadenopathy.
With the clear suspect of stump appendicitis, abdominoplevic CT scan showed, in the right iliac fossa, a 2 cm tubular structure adjacent to the cecum, with inflammatory features, suspect for appendiceal remnant (dilated, fluid filled and with an obstructing fecalith in its lumen) with pericaecal fat stranding, a thickened caecal wall and single pericaecal lymphadenopathy (Fig. 1d–f).
After 30 days of therapy with metronidazole 500 mg/day and mesalazine 1000 mg × 2/day, the patient was submitted to surgery and appendectomy was performed: the pathology revealed acute stump appendicitis and periappendicitis with abscess formation. The stump measured 24 mm in length.
The patient had no postoperative complications and was discharged home on postoperative day 2.
3. Discussion
Stump appendicitis (SA) was first described by Rose in 1945 and Baumgartner in 1949; a medline based literature review revealed 61 reported cases of SA; the patients' age range was 8–72 years (mean age 37 ± 2 years) of which 64.5% were male. The commonest presenting symptom is abdominal pain (right lower quadrant pain 59%, non specific abdominal pain 16%, and central abdominal pain radiating to the right lower quadrant 14%). The initial appendicectomy operation was open in about 65% of the patients and the time interval between the initial operation and re-operation was between 9 weeks and 50 years. 45% of the patients had preoperative computed tomography scan and this was diagnostic of SA in about 27.5% of the cases (pericecal inflammatory changes, cecal wall thickening, and abscess formation and fluid in the right paracolic gutter) [1], [2], [3].
Today, the diagnosis of SA is usually not considered as the etiology for right lower quadrant pain in patient with history of appendectomy, resulting in delaying making the correct diagnosis and treatment. Obviously, other more common causes should be excluded first.
In conclusion, stump appendicitis is a rare entity and patients can present with vague symptoms of abdominal pain, nausea, and vomiting.
Diagnosis can be made with abdominal ultrasound or, better, computed tomography scan.
SA may well be considered as one of the differential diagnoses of acute right lower abdominal pain even in patients with history of appendicectomy.
Conflict of interest
The Authors report no conflict of interest in this work; besides, the authors report that are no disclosures relevant to this publication.
Funding
None.
Ethical approval
Approved by Ethical Committee of Policlinico “Paolo Giaccone”—Prot. 258/2015. The manuscript received ethical approval from Hospital committee.
Consent
The patient has provided written consent to the publication of the case report and pictures.
Disclosure
This article has not been presented nor published elsewhere, and no financial support has been obtained in its preparation.
Authors contribution
Dr. G.G.: Literature search, manuscript writing, design and image providing.
Dr. G.D.C.: Literature search, case writing and image providing.
Dr. B.C.: Writing and image providing.
Prof. G.M.: Comments and data analysis.
All the authors (G.D.C., G.G., B.C. and G.M.) revised the manuscript and agree on its conclusions.
Declaration of Helsinki
The Authors have been respected the Declaration of Helsinki as a statement of ethical principles for medical research involving human subjects, including research on identifiable human material and data.
Guarantor
Girolamo Geraci.
References
- 1.Awe J.J.A., Soliman A.M., Gourdie R.W. Stump appendicitis: an uncompleted surgery, a rare but important entity with potential problems. Case. Rep. Surg. 2013;2013:972596. doi: 10.1155/2013/972596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanona H., Al Samaree A., Nice C., Bhattacharya V. Stump appendicitis: a review. Int. J. Surg. 2012;10:425–428. doi: 10.1016/j.ijsu.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Subramanian A., Liang M.K. A 60-year literature revive of stump appendicitis: the need of a critical review. Am. J. Surg. 2012;203(4):503–507. doi: 10.1016/j.amjsurg.2011.04.009. [DOI] [PubMed] [Google Scholar]