Abstract
Background
Access to primary care could reduce use of more costly health care by uninsured individuals through prevention and early treatment. We analyzed data from a program providing free primary care to test this hypothesis.
Methods
We compared emergency room (ER) visits and hospitalizations among uninsured, low-income adults who received immediate versus delayed access to a program providing free primary care, including labs, X-rays, and specialty consultation. We used surveys to identify ER visits and hospitalizations during the 12 months preceding and following program enrollment or wait list entry.
Results
Hospitalizations decreased from the year before entry to the year following entry in participants with immediate and delayed (6.0% vs 8.8% decrease) access. ER use also decreased in both groups (11.2% vs 15.4%).
Conclusions
Free primary care services and specialty consultation did not reduce use of more costly health care services during its first year. More prolonged availability of primary care might have greater impact.
Keywords: community health, health outcomes, impact evaluation, primary care, program evaluation
Despite increasing political attention, more than 50 million United States residents are currently uninsured.1,2 Although the Affordable Care Act, if implemented in full, will insure 32 million additional Americans, the Congressional Budget Office estimates that 23 million people will remain uninsured. Even excluding undocumented residents, 15 million Americans will remain uninsured in 2019, when the Affordable Care Act is fully implemented. Thus, large numbers of Americans will continue to lack health insurance for the foreseeable future.
Overall, uninsured Americans tend to use less health care,3–6 likely because of high out-of-pocket costs. Although some of this lower use reflects less use of elective procedures, the uninsured may also forego primary care and preventive services.5,7 Perhaps because of this, uninsured individuals, even after controlling for their lower income, are more often diagnosed at an advanced stage of disease when they do present for care.8,9 They are also more likely to be hospitalized for ambulatory care sensitive conditions,10–16 more likely to use an emergency room (ER) as their main source of care,17–19 and more likely to use the ER for nonemergency conditions.20,21 Thus, they may use more expensive, less effective care, with poorer outcomes.22 In other words, the lack of insurance could paradoxically increase overall health care costs, even as it discourages use of some health care services.
Since most uninsured persons are members of the working poor (or their children),23,24 their options are limited. Their income often precludes eligibility for Medicaid; clinics with sliding fee systems, such as Federally Qualified Health Centers, may still be cost-prohibitive.25,26 Moreover, many uninsured individuals are unaware of options that do exist.26,27 Thus, these individuals may simply do without needed health care, use the ER (an expensive default), or seek ad hoc charity care in physician offices. Uninsured individuals with certain serious but chronic conditions, such as diabetes, hypertension, and coronary artery disease may be most likely to avoid care, since these conditions may have no or tolerable symptoms for many years. Physicians, hospitals and health policy makers are often frustrated by these individuals, since their choice to avoid the short term costs of chronic disease management leads to later need for expensive health care for which they cannot pay.
Charity care that is provided in doctor’s offices has been decreasing steadily.28,29 Although there are many reasons for this, one likely contributor is that a provider, while personally willing to forego payment, is unable to provide charity patients with laboratory and radiology services they believe are integral to quality health care. It is certainly less satisfying to practice care they consider suboptimal, even if “Good Samaritan” laws protect them from malpractice concerns. Thus, improved access to such services and coordination of this charity care could improve primary care access.
One delivery model, called Project Access (PA), provides individuals who are not eligible for Medicare or Medicaid, and are financially unable to buy health insurance, access to free high-quality primary and preventive care from volunteer clinicians. PA model programs typically support the volunteer clinicians by providing free basic laboratory and radiology services. A variety of approaches are used to provide participating patients with the drugs needed to manage their chronic conditions at little or no cost. In general, PA does not provide ER or hospital care, but seeks to minimize the frequency with which participants use such services. The PA model has been successfully implemented in dozens of United States communities, ranging in population from less than 20 000 to more than 2 000 000. However, although one rationale for the program is that it will reduce costly ER visits and hospital stays, no methodologically rigorous study has sought to establish such an effect. We therefore sought to determine whether a PA model program, MilwaukeeCares, would reduce ER visits and hospitalizations among persons given immediate access to the program, compared with wait listed controls.
Methods
Description of the MilwaukeeCares Program
MilwaukeeCares is an administrative system that (a) identifies uninsured individuals, (b) identifies health care providers willing to provide free services, and (c) connects the person in need to an appropriate primary health care provider. Uninsured individuals are eligible if they are 18 years old or older, low income (ie, less than 200% of the Federal Poverty Level) and not eligible for other insurance. Typically, patients are screened by the county social worker and referred to MilwaukeeCares if they are not eligible for Wisconsin’s Medicaid program or other insurance programs for low-income adults.
Working with the Medical Society of Milwaukee County and using online, radio, and newspaper public service advertising, MilwaukeeCares recruited physicians willing to supply medical services without charge. These physicians indicated the type and volume of free services they were willing to provide. We identified a large referral lab that provided free basic laboratory services. Similarly, a private radiology group donated the full spectrum of non-invasive ambulatory radiology services, including computed tomography scans and magnetic resonance imaging. The program had no pharmacy component; providers were encouraged to prescribe inexpensive generics, or use pharmaceutical company programs. Similarly, the program was not able to negotiate any arrangements for surgical services, hospitalization or more expensive technologies such as echocardiography or colonoscopy.
Once we had achieved a critical mass of service providers, MilwaukeeCares began to match patient participants to locally available participating providers. Once matched, the patient agreed to use that provider as their primary source of care, though each visit was coordinated through the MilwaukeeCares office. The primary care provider could order MilwaukeeCares radiology and laboratory services much as they would with a private insurer, but relied on their established referral relationships to arrange needed hospital stays, ER visits, operative procedures and ambulatory procedures in a way that would limit patient’s out-of-pocket expenses.
Evaluation Study
Overview
We planned to randomly allocate participants to either immediate enrollment in MilwaukeeCares or enrollment after a 12-month delay. Study personnel advised patients in the delayed care arm regarding usual ways to access care until they were entered into the project. As the random assignment period drew to a close, it became clear that the program administrator had allocated some patients with perceived greater need directly into the “immediate enrollment” group regardless of the group to which they had been randomized. Moreover, we were not able to determine which individuals had been truly randomized to immediate enrollment and which were assigned to immediate enrollment because the coordinator thought they needed it. Thus, although we had planned for a randomized comparison of 2 groups of roughly equal size, the group assigned to immediate access was larger, and nonrandomly assigned.
Study population
We recruited patients through word of mouth, ER social workers, radio ads, and the MilwaukeeCares Internet website. We required that participants be able to complete an English or Spanish language baseline survey; no potential participant was excluded for this reason. Because of the planned evaluation of MilwaukeeCares, all participants provided informed consent. If patients were not eligible for MilwaukeeCares, or declined to participate, they were counseled on alternate sources of health care, including free clinics and Federally Qualified Health Centers.
Data
All participants completed a baseline survey while in the MilwaukeeCares administrative office at the time of their initial enrollment. They completed a follow-up survey 12 months after their initial survey. In the case of individuals assigned to the delayed group, this was at the time they came to the MilwaukeeCares office to be assigned to a primary care physician. Persons assigned to the immediate intervention group were asked to come to the MilwaukeeCares office to complete the survey; if this was not feasible, the survey was administered by phone. When the survey was administered in person, the participant was given a copy of the survey but the study coordinator read the questions and recorded the responses.
The baseline survey included demographics and self reported chronic diseases. Both the baseline and follow up survey asked the respondent to estimate the number of physician visits, ER visits, and hospital admissions in the preceding year. Both surveys also included a measure of health status (Medical Outcomes Study Short Form–36 [SF-36]).30 Surveys were available in English and Spanish.
Analysis
We scored the SF-36 using standard methods, generating both a mental health and physical health subscale at baseline and follow-up. We categorized each patient as having zero or at least one ER visit. We treated hospital stays in the same way. We compared baseline characteristics in the immediate versus delayed enrollment groups using simple χ2 tests, t tests, and nonparametric statistics as appropriate. We used only those participants who completed a follow up survey in our comparison of changes in health care service use and health status from baseline to follow-up.
For our primary analysis, we compared changes in outcomes between the groups assigned to immediate versus delayed MilwaukeeCares access. For binomial outcomes (eg, whether or not the participant used a service), we used a simple McNemar’s test to compare changes in the proportion with the outcome between the 2 groups. For continuous variables we used analysis of variance.
We then used a propensity score technique to adjust for imbalance due to nonrandom assignment to the 2 groups among the people who completed the randomized comparison period (ie, completed the follow-up survey).31 First, using one logistic regression model we identified baseline factors that were significantly associated with assignment to the immediate enrollment group (intervention group) versus delayed enrollment (control) and dropouts. Another logistic regression predicted enrollment to control group versus intervention and dropouts. We used these models to estimate (a) the propensity of a participant to be enrolled in the intervention group and not drop out and (b) the propensity of a participant to be enrolled in the control group and not drop out. We then used regression analyses to compare outcomes between the 2 groups after weighting each observation by the inverse probability of their propensity to be in that group. This weighting scheme made the distribution of covariates in the control and in the intervention groups approximately equal to the baseline distribution of covariates. The study was approved by the institutional review board of the Medical College of Wisconsin. All analyses were completed using PC SAS Version 9.2.
Results
We recruited a total of 105 physicians representing 25 specialties. Most of the providers practiced alone or in small groups. One large area firm donated the services of their staff model panel of employee health physicians. Administrative barriers made participation very difficult for providers who were members of the 3 largest Milwaukee area physician groups. We enrolled 278 patients into the study, 194 of whom received immediate access to MilwaukeeCares services. The baseline characteristics of those allocated to immediate and delayed access are presented in Table 1. Persons assigned to immediate access were more likely to report having diabetes, hypertension, and high cholesterol and less likely to have full time employment. Despite this, there was no difference between the 2 groups in physician office visits, ER use or hospitalizations.
Table 1.
Comparison of Persons Assigned to Immediate Versus Delayed MilwaukeeCares Access.
| Patient Characteristics | Timing of MilwaukeeCares Enrollment
|
Pb | |
|---|---|---|---|
| Immediate (n = 194); n (%)a | Delayed (n = 93); n (%)a | ||
| Insured past 12 months | .3589 | ||
| Yes | 91 (50.0) | 41 (45.1) | |
| No | 91 (50.0) | 50 (54.9) | |
| Time lacking health insurance (months) | .5315 | ||
| 0–6 | 68 (39.3) | 29 (32.2) | |
| 6–12 | 25 (14.5) | 14 (15.6) | |
| >12 | 80 (46.2) | 47 (52.2) | |
| Employment status | .0419* | ||
| Part-time | 57 (31.0) | 26 (28.3) | |
| Full-time | 42 (22.8) | 34 (37.0) | |
| No response | 85 (46.2) | 32 (34.8) | |
| Hours/week at this job | .0412* | ||
| Not applicable | 80 (43.5) | 28 (30.4) | |
| 0–20 | 27 (14.7) | 9 (9.8) | |
| 21–40 | 67 (36.4) | 46 (50.0) | |
| >40 | 10 (5.4) | 9 (9.8) | |
| Student status | .3613 | ||
| Yes, full-time | 7 (3.8) | 8 (8.7) | |
| Yes, part-time | 16 (8.7) | 7 (7.6) | |
| No | 160 (87.0) | 77 (83.7) | |
| No response | 1 (0.5) | 0 (0.0) | |
| Education attained | .2718 | ||
| Eighth grade or less | 34 (18.5) | 10 (10.9) | |
| Some high school | 39 (21.2) | 16 (17.4) | |
| High school graduate or GED | 57 (31.0) | 34 (37.0) | |
| Some college | 54 (29.3) | 32 (34.8) | |
| Marital status | .0118* | ||
| Single and never married | 65 (35.7) | 48 (52.2) | |
| Married | 63 (34.6) | 15 (16.3) | |
| Separated | 11 (6.0) | 4 (4.4) | |
| Divorced | 31 (17.0) | 16 (17.4) | |
| Widowed | 12 (6.6) | 9 (9.8) | |
| Ethnicity | .0494* | ||
| No, not Hispanic | 119 (66.1) | 72 (78.3) | |
| Yes, Hispanic | 61 (33.9) | 20 (21.7) | |
| Race | .1781 | ||
| Caucasian | 78 (42.9) | 39 (42.4) | |
| African American | 77 (42.3) | 47 (51.1) | |
| American Indian or Alaskan | 27 (14.8) | 6 (6.5) | |
| Place for health care | .7145 | ||
| Doctor’s or nurse practitioner’s | 61 (33.3) | 28 (30.4) | |
| office | |||
| Public health clinic | 55 (30.1) | 22 (23.9) | |
| Hospital emergency room | 20 (10.9) | 13 (14.1) | |
| Internet | 3 (1.6) | 1 (1.1) | |
| No usual place | 44 (24.0) | 28 (30.4) | |
| Hospitalized in past 12 months | .5183 | ||
| Yes | 27 (14.7) | 13 (14.3) | |
| No | 157 (85.3) | 78 (85.7) | |
| Times hospitalized in past 12 months | .8495 | ||
| 0 | 156 (87.2) | 74 (86.1) | |
| 1 | 19 (10.6) | 9 (10.5) | |
| ≥2 | 4 (2.2) | 3 (3.5) | |
| Emergency room visits in past 12 months | .3848 | ||
| None | 127 (69.4) | 55 (59.8) | |
| 1 | 31 (16.9) | 24 (26.1) | |
| 2–3 | 16 (8.7) | 9 (9.8) | |
| 4–9 | 9 (4.93) | 4 (4.3) | |
| Office visits in past 12 months | .1522 | ||
| None | 30 (16.5) | 19 (20.7) | |
| 1 | 41 (22.5) | 27 (29.3) | |
| 2–3 | 46 (25.3) | 27 (29.3) | |
| 4–9 | 42 (23.1) | 14 (15.2) | |
| 10–12 | 10 (5.5) | 5 (5.4) | |
| ≥13 | 13 (7.1) | 0 (0.0) | |
| Medical conditions present | |||
| Hypertension | 84 (43.3) | 31 (33.3) | .0475* |
| High cholesterol | 58 (29.9) | 15 (16.1) | .0221* |
| Prior stroke | 7 (3.6) | 1 (1.1) | .1912 |
| Known heart disease | 22 (11.3) | 9 (9.7) | .5739 |
| Mental health trouble | 15 (7.7) | 8 (8.6) | .8184 |
| Current or past cancer | 11 (5.7) | 3 (3.2) | .5381 |
| Weight problem | 44 (22.7) | 14 (15.1) | .2273 |
| Diabetes | 42 (21.6) | 8 (8.6) | .0038* |
Numbers in a category may not add up to the total because of missing responses.
Significant P values are denoted with an asterisk (*). All comparisons use Fisher’s exact test or χ2 tests as appropriate.
At 1 year, 203 participants (71 from the delayed access group) completed the follow-up survey. In this group, the proportion of participants with hospital stays or ER visits during the preceding year decreased from baseline to followup (13% vs 6% for hospitals, P = .03; 32% vs 19% for ER visits, P < .0001). Participants were more likely to have made at least one physician office visit during follow-up, but this change was not significant (85% vs 88%, P = .32). There was no change in either mental health or physical health components of the SF-36.
We present our bivariate comparisons of outcomes in Table 2 and Figure 1. The proportion of participants reporting hospitalizations decreased during the year of follow-up in both groups (from 14.0% to 8.0% in the immediate access group and from 11.5% to 2.7% in the delayed access group). The decrease in proportion with an ER visit was also similar in the immediate and delayed access groups. The number of patients with at least one office visit increased by a similar amount in both groups (88.6% to 91.8% in the immediate access group vs 85.3% to 87.5% in the delayed access group, P = .92). Similarly, the proportion of participants who had more visits during the follow-up year was similar in the 2 groups (40% in the immediate group vs 34.3% in the delayed group, P = .53)
Table 2.
Health Care Service Use and Health Status During the Baseline Year and Follow-up Among Persons Completing the Followup Survey.a
| Patient Characteristics | Timing of MilwaukeeCares Enrollment
|
Pb | |||
|---|---|---|---|---|---|
| Immediate
|
Delayed
|
||||
| Baseline (%) | Follow-up (%) | Baseline (%) | Follow-up (%) | ||
| Hospitalized in past 12 months | —c | ||||
| Yes | 14.0 | 8.0 | 11.5 | 2.7 | |
| No | 86.0 | 92.0 | 88.5 | 97.3 | |
| 1+ Emergency room visit in past 12 months | .84 | ||||
| Yes | 28.6 | 17.4 | 38.1 | 22.7 | |
| No | 71.4 | 82.6 | 61.9 | 87.3 | |
| Office visits in past 12 months | .92 | ||||
| None | 11.4 | 8.2 | 14.7 | 12.5 | |
| 1 | 20.5 | 18.1 | 26.9 | 27.6 | |
| 2–3 | 30.0 | 35.7 | 34.7 | 31.5 | |
| 4–9 | 25.5 | 29.9 | 17.3 | 27.1 | |
| 10–12 | 12.7 | 8.2 | 6.3 | 1.3 | |
P values reflect comparison of immediate versus delayed access groups, using weighted results. Percentages are based on unweighted data from participants with both baseline and follow-up data.
Logistic regression for emergency room visits and hospitalizations, controlling for baseline use. McNemar’s test for whether or not the number of office visits increased from baseline to follow-up.
There were too few events to perform a valid comparison of the decrease in hospitalizations.
Figure 1.
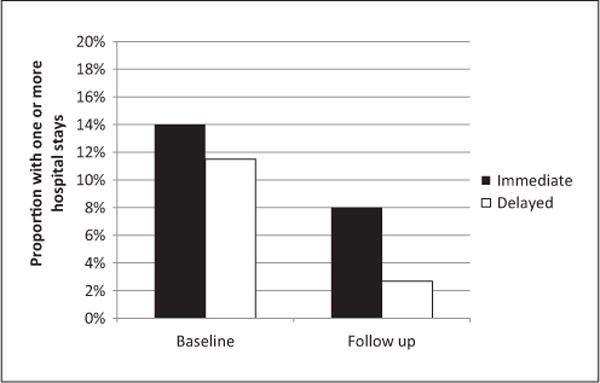
Hospitalization rates in baseline and follow-up years, among participants with immediate versus delayed MilwaukeeCares access.
Propensity Weighted Analysis
The likelihood that a person was assigned to the immediate group and completed follow-up was increased by the presence of diabetes and the lack of full-time employment. The probability that a person was assigned to the delayed group and completed follow-up was predicted with the same 2 variables. Other characteristics significantly different between the delayed and immediate control groups reported in Table 1 lose their significance when we control for diabetes and employment status. In our inverse probability weighted analyses, we continued to find that persons assigned to immediate versus delayed MilwaukeeCares access had similar decreases in the likelihood they would use the ER. There were too few hospitalizations to statistically test the equivalence of the decrease in hospitalization rates in the 2 groups in this analysis.
Discussion
This is the first study to use a randomized trial design to examine the effect of coordinated free care in a PA model program on ER and hospital use. Although both ER and hospital use decreased among study participants, the drop was similar among persons given immediate access to MilwaukeeCares and those whose access was delayed. Moreover, study participation did not significantly impact the frequency of office visits or the functional status as measured by the SF-36 in either group.
There are several potential reasons why this carefully developed program failed to demonstrate the expected outcomes. First, because some participants were given immediate access because of perceived need, the immediate access group had more chronic conditions than the delayed group. Although we adjusted for measured differences between the groups with a propensity weighted analysis, such analyses may not adjust for unmeasured differences between the groups. Second, to ensure that the delayed group was not harmed, we provided them with detailed instructions on alternative approaches to receiving care. This direct face-to-face counseling may have significantly increased their ability to get care through other charity resources. In effect, they may have been able to get much of what MilwaukeeCares had to offer, but through other channels. In fact, the 2 groups had similar and substantial use of physician office visits, the type of health care that PA programs seek to encourage. It is also possible that the immediate group, with more structured access to care, would have improved recall of ER and hospital use during the follow-up period. We must also acknowledge that our sample size was relatively small because of funding limitations; future studies should use larger sample sizes. Finally, we suspect that 1 year is too short of a period for improved primary care to make a substantial difference in health outcomes.
The MilwaukeeCares program implemented a model of coordinated care similar to models used in dozens of communities nationwide following its development in Buncombe County, North Carolina. Although projects based on this model have won awards for service and innovation, evaluations focus on surveys that document patient and provider satisfaction with the organizational structure.27,32–34 Reports of its effectiveness are typically limited to descriptions of the number and dollar value of services provided to clients, without clear evidence of changes in health, or changes in use of other types of health care resources.35
We acknowledge that our study has methodological limitations. Most obviously, our planned randomized comparison was thwarted by the well-meaning, but scientifically problematic, decision by the program administrator to override randomization of eligible subjects when she judged they needed immediate access to MilwaukeeCares. Second, our negative experience may reflect an unusually active network of charity primary care providers and may not generalize to other cities. Alternatively, although MilwaukeeCares was able to engage many physicians covering a broad range of specialties, we were not able to negotiate agreements for free access to complex diagnostic and therapeutic technologies. This range of services is less than has been achieved in some communities. It is possible that more ER and hospital use could have been avoided if such services were available through MilwaukeeCares providers. Finally, we acknowledge that we did not collect all relevant endpoints. Thus, we do not have data regarding total costs, use of important preventive services or improvement in intermediate endpoints such as blood pressure or glycosylated hemoglobin. All these would be useful additions for future studies.
In addition to addressing our primary study questions, we believe that our experience with MilwaukeeCares provides some important lessons for others who seek to implement a similar program. First, we believe that the lack of clear “buy in” from the leadership of large physician groups put the program’s long-term viability at risk. Physicians in these groups (the majority of Milwaukee physicians), were precluded from participation by their employee contract. Conversely, smaller physician groups, a single specialty radiology group, and a local industry made substantial contributions of time and resources. Anecdotally, they viewed the MilwaukeeCares program as an opportunity rather than an obligation. Similarly, the fact that the original grant originated at an academic medical center that was itself a “player” in the city’s health care marketplace made it challenging to engage other hospitals and hospital affiliated physician groups in the project. This made it difficult to identify a sponsor to pick up even the modest ongoing administrative cost of the program. Indeed, in the absence of ongoing grant funding, the administrative infrastructure for MilwaukeeCares could not be sustained and the program has ended.
We also note that reduced cost is not the primary reason for PA model programs; for many participants, this was their first experience with coordinated care. Anecdotally, individual participants reported dramatic results; specific examples include the ability to return to work, initiate diabetes treatment, and achieve hypertension control. Others became aware of major health problems (eg, coronary artery disease) for the first time.
Our results are consistent with some prior research in which enhanced access to care led to increased service use.36 Given our anecdotal evidence that new conditions were uncovered in the course of the intervention, it is plausible that our intervention may have led to some hospitalizations even as it prevented others. Similarly, there is evidence that more than one year of enhanced access is needed before the health status of those with poor access catches up to the general population.37 In future research patient-specific data, including drops in blood pressure or hemoglobin A1c should be evaluated. It would also be useful to look at the real savings that working poor experience in these systems (not just value of donated services).
In summary, although there is good face validity to the premise that provision of coordinated pro bono care to needy patients will improve “hard outcomes,” the proof of this remains elusive. The massive RAND Health Insurance Study was also unable to show that free care provided better outcomes than programs that had variable attached costs.38 We believe that this lack of hard evidence is of more than academic interest, since such programs entail administrative costs that require ongoing funding. Other projects should be carefully evaluated to confirm that they are delivering changes that are important to the overall health of their patients, and in a way that is cost effective to our health system.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article:
This project was funded by the Healthier Wisconsin Partnership Program, a component of the Advancing a Healthier Wisconsin endowment at the Medical College of Wisconsin; statistical analysis was supported by Grant No. 1UL1RR031973 from the Clinical and Translational Science Award (CTSI) program of the National Center for Research Resources, National Institutes of Health. We received expert administrative support in preparing this report from Kristyn Ertl, BA.
Biographies
Ted MacKinney is an Associate Professor of Medicine in the Division of General Internal Medicine at the Medical College of Wisconsin in Milwaukee. He has lived and worked between Milwaukee and Nepal since 1991. He is currently working in Nepal, developing a Nepalese residency training program for physicians seeking to become specialists in internal medicine.
Alexis M. Visotcky, MS, is a staff Biostatistician in the Division of Biostatistics of the Institute for Health and Society at the Medical College of Wisconsin in Milwaukee. She is expert in multiple statistical methods. She has participated in a range of federally funded grants.
Sergey Tarima, PHD, is an Assistant Professor of Biostatistics in the Division of Biostatistics of the Institute for Health and Society at the Medical College of Wisconsin in Milwaukee. His research interest is optimizing use of additional information in statistical estimation.
Jeff Whittle, MD, MPH is a Staff Physician at the Clement J. Zablocki VA Medical Center and a Professor of Medicine in the Division of General Internal Medicine at the Medical College of Wisconsin, both in Milwaukee. His research has focused on racial disparities, access to care and chronic disease self management. His work has been funded by the VA, the National Institutes of Health, the Agency for Healthcare Research and Quality, the Health Services Resource Administration and the American Heart Association.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.DeNavas-Walt C, Proctor B, Smith J. Income, Poverty, and Health Insurance Coverage in the United States: 2010. Washington, DC: Government Printing Office; 2011. ((US Census Bureau, Current Population Reports, P60-239)). [Google Scholar]
- 2.Overview of the Uninsured in the United States: A Summary of the 2011 Current Population Survey. Washington, DC: US Department of Health and Human Services; 2011. US Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation. (ASPE issue brief) http://aspe.hhs.gov/health/reports/2011/cpshealthins2011/ib.pdf. Accessed February 4, 2013. [Google Scholar]
- 3.Broyles RW, McAuley WJ, Baird-Holmes D. The medically vulnerable: their health risks, health status, and use of physician care. J Health Care Poor Underserved. 1999;10:186–200. doi: 10.1353/hpu.2010.0498. [DOI] [PubMed] [Google Scholar]
- 4.Ross JS, Bradley EH, Busch SH. Use of health care services by lower-income and higher-income uninsured adults. JAMA. 2006;295:2027–2036. doi: 10.1001/jama.295.17.2027. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman C, Paradise J. Health insurance and access to health care in the United States. Ann N Y Acad Sci. 2008;1136:149–160. doi: 10.1196/annals.1425.007. [DOI] [PubMed] [Google Scholar]
- 6.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey 2009. Vital Health Stat 10. 2010;(249):1–207. [PubMed] [Google Scholar]
- 7.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069. doi: 10.1001/jama.284.16.2061. [DOI] [PubMed] [Google Scholar]
- 8.Naik AM, Joseph K, Harris M, Davis C, Shapiro R, Hiotis KL. Indigent breast cancer patients among all racial and ethnic groups present with more advanced disease compared with nationally reported data. Am J Surg. 2003;186:400–403. doi: 10.1016/s0002-9610(03)00282-4. [DOI] [PubMed] [Google Scholar]
- 9.Arora P, Obrador GT, Ruthazer R, et al. Prevalence, predictors, and consequences of late nephrology referral at a tertiary care center. J Am Soc Nephrol. 1999;10:1281–1286. doi: 10.1681/ASN.V1061281. [DOI] [PubMed] [Google Scholar]
- 10.Billings J, Teicholz N. Uninsured patients in District of Columbia hospitals. Health Aff (Millwood) 1990;9:158–165. doi: 10.1377/hlthaff.9.4.158. [DOI] [PubMed] [Google Scholar]
- 11.Billings J, Anderson GM, Newman LS. Recent findings on preventable hospitalizations. Health Aff (Millwood) 1996;15:239–249. doi: 10.1377/hlthaff.15.3.239. [DOI] [PubMed] [Google Scholar]
- 12.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–311. [PubMed] [Google Scholar]
- 13.Oster A, Bindman AB. Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med Care. 2003;41:198–207. doi: 10.1097/01.MLR.0000045021.70297.9F. [DOI] [PubMed] [Google Scholar]
- 14.Chang CF, Mirvis DM, Waters TM. The effects of race and insurance on potentially avoidable hospitalizations in Tennessee. Med Care Res Rev. 2008;65:596–616. doi: 10.1177/1077558708318283. [DOI] [PubMed] [Google Scholar]
- 15.Clancy CM. The persistent challenge of avoidable hospitalizations. Health Serv Res. 2005;40:953–956. doi: 10.1111/j.1475-6773.2005.00442.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weissman JS, Gatsonis C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992;268:2388–2394. [PubMed] [Google Scholar]
- 17.Begley CE, Vojvodic RW, Seo M, Burau K. Emergency room use and access to primary care: evidence from Houston, Texas. J Health Care Poor Underserved. 2006;17:610–624. doi: 10.1353/hpu.2006.0098. [DOI] [PubMed] [Google Scholar]
- 18.Newton MF, Keirns CC, Cunningham R, Hayward RA, Stanley R. Uninsured adults presenting to US emergency departments: assumptions vs data. JAMA. 2008;300:1914–1924. doi: 10.1001/jama.300.16.1914. [DOI] [PubMed] [Google Scholar]
- 19.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. A national study of chronic disease prevalence and access to care in uninsured U.S. adults. Ann Intern Med. 2008;149:170–176. doi: 10.7326/0003-4819-149-3-200808050-00006. [DOI] [PubMed] [Google Scholar]
- 20.Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. JAMA. 1994;271:1909–1912. [PubMed] [Google Scholar]
- 21.Grumbach K, Keane D, Bindman A. Primary care and public emergency department overcrowding. Am J Public Health. 1993;83:372–378. doi: 10.2105/ajph.83.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker DW, Sudano JJ, Albert JM, Borawski EA, Dor A. Lack of health insurance and decline in overall health in late middle age. N Engl J Med. 2001;345:1106–1112. doi: 10.1056/NEJMsa002887. [DOI] [PubMed] [Google Scholar]
- 23.Hoffman C, Schlobohm A. Uninsured in America: A Chart Book. 2nd. Washington, DC: The Henry J. Kaiser Family Foundation; 2000. [Google Scholar]
- 24.Collins SR, Davis K, Doty MM, Kriss JL, Holmgren AL. Gaps in Health Insurance: An All-American Problem. New York, NY: The Commonwealth Fund; 2006. [Google Scholar]
- 25.Ahmed SM, Lemkau JP, Nealeigh N, Mann B. Barriers to healthcare access in a non-elderly urban poor American population. Health Soc Care Community. 2001;9:445–453. doi: 10.1046/j.1365-2524.2001.00318.x. [DOI] [PubMed] [Google Scholar]
- 26.May JH, Cunningham PJ, Hadley J. Most uninsured people unaware of health care safety net providers. Issue Brief Cent Stud Health Syst Change. 2004;(90):1–4. [PubMed] [Google Scholar]
- 27.Ahmed SM, Maurana CA. Reaching out to the underserved: a successful volunteer program. Am J Public Health. 2000;90:439–440. doi: 10.2105/ajph.90.3.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cunningham PJ, Grossman JM, St Peter RF, Lesser CS. Managed care and physicians’ provision of charity care. JAMA. 1999;281:1087–1092. doi: 10.1001/jama.281.12.1087. [DOI] [PubMed] [Google Scholar]
- 29.Isaacs SL, Jellinek P. Is there a (volunteer) doctor in the house? Free clinics and volunteer physician referral networks in the United States. Health Aff (Millwood) 2007;26:871–876. doi: 10.1377/hlthaff.26.3.871. [DOI] [PubMed] [Google Scholar]
- 30.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 31.Curtis LH, Hammill BG, Eisenstein EL, Kramer JM, Anstrom KJ. Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med Care. 2007;45(10 suppl 2):S103–S107. doi: 10.1097/MLR.0b013e31806518ac. [DOI] [PubMed] [Google Scholar]
- 32.Ablah E, Wetta-Hall R, Burdsal CA. Assessment of patient and provider satisfaction scales for project access. Qual Manag Health Care. 2004;13:228–242. doi: 10.1097/00019514-200410000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Ahmed SM, Maurana CA. Reaching out to the underserved: a collaborative partnership to provide health care. J Health Care Poor Underserved. 1999;10:157–168. doi: 10.1353/hpu.2010.0277. [DOI] [PubMed] [Google Scholar]
- 34.Uhlig PN. A call to leadership: Project Access—helping the uninsured community by community. Ann Thorac Surg. 2000;70:354–355. doi: 10.1016/s0003-4975(00)01742-2. [DOI] [PubMed] [Google Scholar]
- 35.Blewett LA, Ziegenfuss J, Davern ME. Local access to care programs (LACPs): new developments in the access to care for the uninsured. Milbank Q. 2008;86:459–479. doi: 10.1111/j.1468-0009.2008.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions. N Engl J Med. 1996;334:1441–1447. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 37.Baker DW, Feinglass J, Durazo-Arvizu R, Witt WP, Sudano JJ, Thompson JA. Changes in health for the uninsured after reaching age-eligibility for Medicare. J Gen Intern Med. 2006;21:144–149. doi: 10.1111/j.1525-1497.2006.00576.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brook RH, Ware JE, Jr, Rogers WH, et al. Does free care improve adults’ health results from a randomized controlled trial. N Engl J Med. 1983;309:1426–1434. doi: 10.1056/NEJM198312083092305. [DOI] [PubMed] [Google Scholar]


