Synopsis
According to the Institute of Medicine Relieving Pain in America Report and the subsequently released National Pain Strategy, pain affects over 100 million Americans and costs our country in excess of half a trillion dollars per year. We are having a greater appreciation for the complex nature of pain and that it can develop into a disease in itself. As such, we need to focus more efforts on prevention of chronic pain and the need for interdisciplinary approaches particularly for the most persistent pain problems. For the goal of precision pain medicine to be successful, we need to link learning health systems with biomarkers (e.g. genomics, proteomics, patient reported outcomes, brain markers) of chronic pain and its treatment.
Keywords: PRECISION MEDICINE, LEARNING HEALTH SYSTEMS, NATIONAL PAIN STRATEGY, Chronic Pain, Institute of Medicine
Introduction
Perioperative and chronic pain management has advanced significantly over the past couple decades. We are moving beyond the notion of pain as a Cartesian notion where stimulus or injury is directly related to pain. Rather, we have learned that pain is a uniquely individual and subjective experience that involves not only biological but also psychological and social factors. This is illustrated in Figure 1 below demonstrating the multidimensional nature of pain.
Figure 1. Multidimensional aspects of pain.
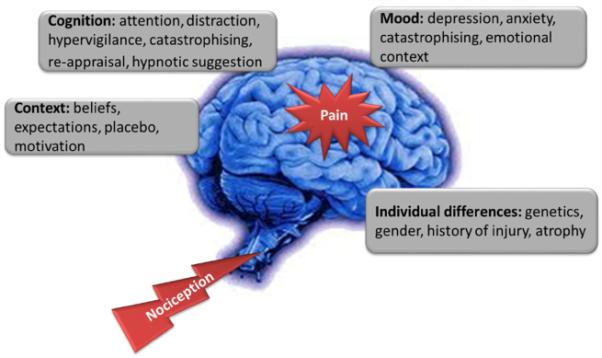
Pain is an integrative sum of nociceptive input (i.e. signals from periphery during injury or surgery) combined with multiple factors that modulate this input to generate the complex and individual experience of pain.
Our increasing knowledge of the mechanisms and factors related to the multidimensional nature of pain has been translated into improved understanding of the care for the patient in pain. We have improved surgeries, interventional procedures, medications, psychology interventions, physical therapy and complementary approaches. We also have a greater appreciation for the need for an interdisciplinary, team based approach to optimize pain care, particularly for more complex cases. This increase in our treatment approaches is particularly important in light of our country’s current prescription opioid epidemic. In fact, opioids are continuing to be moved down the list of approaches as more efficacious treatments are identified.
Despite these advances, we still have millions of people suffering from pain with a cost in the billions to society. Where do we go from here? Two recently released national publications outline a clear path forward for the future of pain assessment, prevention, management and research. The first of these, the Institute of Medicine’s Relieving Pain in America report provides the vision and high level view of the path forward. The second, the National Pain Strategy, shows us how to achieve the vision of optimal pain assessment, prevention and care. Both will be discussed below with emphasis on information relevant for the readers of this journal.
Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research
As part of the 2010 Patient Protection and Affordable Care Act the Institute of Medicine was charged “to increase the recognition of pain as a significant public health problem in the United States.” Accordingly, Health and Human Services, through the National Institutes of Health (NIH), requested that the IOM conduct a study to assess the state of the science regarding pain research, care, and education and to make recommendations to advance the field. The efforts of the multidisciplinary committee that was formed, for which I was honored to be a member, resulted in the IOM report Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. This report was guided by several underlying principles noted in Box 1 below:
Box 1. Relieving Pain in America: Underlying Principles Guiding the IOM Committee.
A moral imperative. Effective pain management is a moral imperative, a professional responsibility, and the duty of people in the healing professions.
Chronic pain can be a disease in itself. Chronic pain has a distinct pathology, causing changes throughout the nervous system that often worsen over time. It has significant psychological and cognitive correlates and can constitute a serious, separate disease entity.
Value of comprehensive treatment. Pain results from a combination of biological, psychological, and social factors and often requires comprehensive approaches to prevention and management.
Need for interdisciplinary approaches. Given chronic pain’s diverse effects, interdisciplinary assessment and treatment may produce the best results for people with the most severe and persistent pain problems.
Importance of prevention. Chronic pain has such severe impacts on all aspects of the lives of its sufferers that every effort should be made to achieve both primary prevention (e.g., in surgery for broken hip) and secondary prevention (of the transition from the acute to the chronic state) through early intervention.
Wider use of existing knowledge. While there is much more to be learned about pain and its treatment, even existing knowledge is not always used effectively, and thus substantial numbers of people suffer unnecessarily.
The conundrum of opioids. The committee recognizes the serious problem of diversion and abuse of opioid drugs, as well as questions about their usefulness long-term, but believes that when opioids are used as prescribed and appropriately monitored, they can be safe and effective, especially for acute, post-operative, and procedural pain, as well as for patients near the end of life who desire more pain relief.
Roles for patients and clinicians. The effectiveness of pain treatments depends greatly on the strength of the clinician-patient relationship; pain treatment is never about the clinician’s intervention alone, but about the clinician and patient (and family) working together.
Value of a public health and community-based approach. Many features of the problem of pain lend themselves to public health approaches--a concern about the large number of people affected, disparities in occurrence and treatment, and the goal of prevention cited above. Public health education can help counter the myths, misunderstandings, stereotypes, and stigma that hinder better care.
From Institute of Medicine (U.S.). Committee on Advancing Pain Research Care and Education. Relieving pain in America : a blueprint for transforming prevention, care, education, and research. Washington, D.C.: National Academies Press; 2011. xvii, 364 p. p.; with permission.
One of the charges to the IOM Pain Committee was to “review and quantify the public health significance of pain”. We commissioned an econometric study that estimated that an astounding 100 million American adults are affected by chronic pain, exceeding the numbers of those affected by diabetes, cancer and heart disease combined. [1] These estimates of chronic pain are an overall underestimate as they do not include adults affected by acute pain, children with either acute or chronic pain, or adults living in long-term care facilities, in the military, or in prison. [2] Furthermore, pain affects millions of Americans throughout their lifetime, increases disability, consumes resources in the health care system, and results in a significant economic burden for the entire nation. The staggering socioeconomic burden of pain is thought to exceed half a trillion dollars per year. Overall, chronic pain has significant effects on the individual relating to physical functioning, quality of life, and psychological well-being.
To address the problem of pain, we put forward that our nation should adopt a population-level prevention and management strategy and tasked HHS with developing a comprehensive plan with specific goals, actions, stakeholders and timeframes. This plan should:
heighten awareness about pain and its health consequences;
emphasize the prevention of pain;
improve pain assessment and management in the delivery of health care and financing programs of the federal government;
use public health communication strategies to inform patients on how to manage their own pain; and
address disparities in the experience of pain among subgroups of Americans.
One of the key messages was that better data on pain is needed. Data on pain prevalence, incidence and treatments. This data includes characteristics of both acute and chronic pain and factors that lead pain after surgery to develop into chronic pain. We are only starting to better understand the factors that lead patients to develop persistent postsurgical pain and persistent use of opioids. [3-5]. Much of that knowledge points to factors that patients bring to the operating room (e.g. catastrophizing, early adverse life events, depression, anxiety) or an injury that contribute significantly to the development of persistent pain and opioid use. The IOM report also called for increased efforts on preventative measures that would reduce the incidence of persistent pain after surgery and injury.
The IOM Pain Report also called for tailoring pain care to each person’s experience with an emphasis on self- management where possible. Coordinated, interdisciplinary pain assessment and care for those with complex pain should be better incentivized financially and promoted. Furthermore, education amongst both persons with pain and those who provide pain care needs to be enhanced. The IOM Pain Report called for a redesign of educational programs to foster an understanding of the complex biological and psychosocial aspects to pain and the multimodal approach to treatment. This redesign of pain curriculum crosses all medical specialties including surgery, medicine, physical and occupational therapy, nursing, and all other groups that care for the person in pain. And although we called for increased research on the mechanisms responsible for pain and the development of safe and effective treatments, we also recognized that there is a wealth of existing knowledge. We must ensure that this knowledge is transmitted to people suffering from pain and to the providers who care for them.
Finally, the IOM committee noted that research has made remarkable gains in characterizing the biological, cognitive, and psychological mechanisms of pain, and the future promises advances in a number of fields—from genomic and cellular through behavioral mechanisms. However, many gaps persist, and developing more effective and less risky pain treatments remains a major challenge. Additional challenges exist in translating the mechanistic knowledge into treatments due to regulatory barriers. The IOM Pain Report called for better coordination of across NIH institutes and centers by improving study section decision-making on pain proposals, and by exploring a range of potential public-private initiatives.
The Relieving Pain in America Report offered a blueprint for transforming prevention, care, education, and research, with the goal of providing relief for people with pain in America. It offered specific priorities and timelines and called for HHS to develop a subsequent strategy that should be comprehensive in scope, inclusive in its development, expeditious in its implementation, and practical in its application. Most importantly, the strategy was to be far-reaching. That was the charge given to the National Pain Strategy Task Force.
The National Pain Strategy
Following the release of the IOM report, the Assistant Secretary for HHS asked the Interagency Pain Research Coordinating Committee (IPRCC) to oversee creation of the National Pain Strategy. Guided and coordinated by an oversight panel, expert working groups explored six important areas of need identified in the IOM recommendations—population research, prevention and care, disparities, service delivery and reimbursement, professional education and training, and public awareness and communication (Figure 2). The working groups comprised 80 experts from a broad array of relevant public and private organizations, including health care providers, insurers, and people with pain and their advocates.
Figure 2.
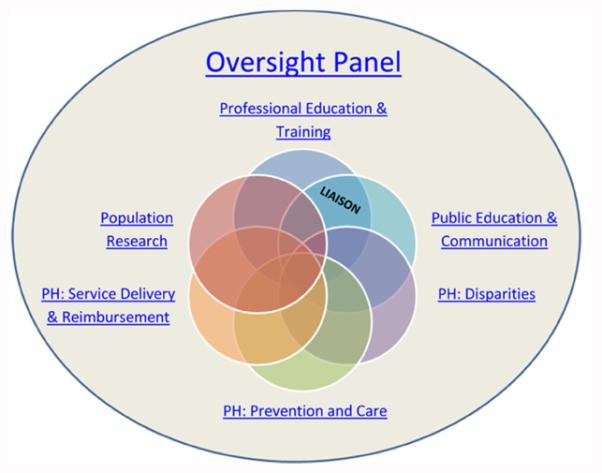
Structure of the National Pain Strategy Task force including Oversight Panel and six Working Groups.
From National Institutes of Health (NIH). The Interagency Pain Research Coordinating Committee. National Pain Strategy. Available at: http://iprcc.nih.gov/National_Pain_Strategy/oversight_panel.htm.
The goal of the NPS was to develop a strategic plan to transform pain prevention, care, and education in our country. As contrasted by the IOM Pain Report, the NPS was to be a “tactical report” with three specific, meaningful, and measureable deliverables from each working group. At the time of this writing, the draft NPS report was released for public commentary with an expected final release in later 2015. While the entire report is important, for the sake of space, I will highlight specific sections that will be critical for readers of this journal. The information that follows will draw from the draft report, recognizing the final version may have changes. Much of this information is drawn directly from the NPS report.
Population Research
The IOM report noted that over 100 million Americans experience chronic pain to some extent. This number encompasses those who have chronic pain of mild impact to those that are highly impacted by their pain. It is therefore important to differentiate people with high-impact chronic pain from those who sustain normal activities although experiencing chronic pain. To accomplish this goal, the NPS first introduced the term “High impact chronic pain” and defined it as pain “associated with substantial restriction of participation in work, social, and self-care activities for six months or more.” This concept of high impact chronic pain will have significant bearing for those who care for patients with hand conditions, as it is those patients who are thought to be the highest utilizers of health care resources. The challenge will be to identify those patients likely to develop into high impact pain after surgery, and develop preventative measures to reduce this occurrence.
Additionally, the National Pain Strategy Population Strategy Working Group recommended specific steps to a) increase the precision of information about chronic pain prevalence overall, for specific types of pain, and in specific population groups; b) develop the capacity to gather information electronically about pain treatments, their usage, costs, and effectiveness; and c) enable tracking changes in pain prevalence, impact, and treatment over time, allowing evaluation of population-level interventions and identification of emerging needs.
Prevention and Care
The Prevention and Care Working group noted that we need to place greater emphasis on prevention of acute and chronic pain throughout the health care system, in environments where injuries are likely to occur, and for people at increased risk of developing chronic pain. This has particular relevance for those caring for persons with hand conditions. There is a call for more standardized assessment tools and outcome measures through the development of new, rigorously researched approaches. Recommendations were also made to improve pain self-management programs that can help affected individuals improve their knowledge, skills, and confidence to prevent, reduce, and cope with pain.
Disparities
The Disparities Working Group noted that there are groups where pain is more prevalent including people with limited access to health care services, racial and ethnic minorities, people with low income or education, and those at increased risk because of where they live or work. The NPS recommends efforts that would increase understanding of the impact of bias and would support effective strategies to overcome it; an increase in access to high-quality pain care for vulnerable population groups; and improvements in communication among patients and health professionals.
Service Delivery and Reimbursement
Evidence suggests that poor quality care and higher health care costs are associated with clinical practice variations, inadequate tailoring of pain therapies, and reliance on relatively ineffective and potentially high risk treatments. The Service Delivery and Reimbursement working group recommended a comprehensive biopsychosocial approach to pain care that is grounded in scientific evidence, integrated, multimodal, and interdisciplinary while, at the patient level is tailored to individual needs. The group noted research and demonstration efforts are needed that build on current knowledge, develop new knowledge, and support further testing and diffusion of model delivery systems.
Professional Education and Training
Strikingly, while pain is one of the most common reasons for health care visits, most health profession’s education programs do not provide adequate pain education. The Professional Education and Training working group noted a need to improve discipline-specific core competencies, including basic knowledge, assessment, effective team-based care, empathy, and cultural competency. Educational program accreditation bodies and professional licensure boards can require pain teaching and clinician learning at the undergraduate and graduate levels. The National Pain Strategy also recommends development of a web-based pain education portal that would contain up-to-date, comprehensive, and easily accessed educational materials.
Public Education and Communication
There is a need for greater understanding—among members of the public and people with pain alike—of important aspects of chronic pain. The Public Education and Communication working group recommended a national public awareness campaign involving many relevant public and private partners, including people with pain and their advocates, to address stigma and misperceptions about chronic pain. Additionally, the group called for a safe-use education campaign targeting people with pain whose care includes prescription medications is recommended.
National Pain Strategy Vision
The NPS also set forth the following vision statement. “If the objectives of the National Pain Strategy are achieved, the nation would see a decrease in prevalence across the continuum of pain, from acute, to chronic, to high-impact chronic pain, and across the life span from pediatric through geriatric populations, to end of life, which would reduce the burden of pain for individuals, families, and society as a whole. Americans experiencing pain—across this broad continuum —would have timely access to a care system that meets their biopsychosocial needs and takes into account individual preferences, risks, and social contexts. In other words, they would receive patient-centered care.
Implementation of the National Pain Strategy will require us to work closely with HHS to advocate leadership from their Department. We will need HHS to lead in tasking the relevant stakeholders with implementation of the strategic goals, establishing accountability for progress, and identification and allocation of resources to advance the Strategy. Importantly, this will also require collaboration among healthcare providers, with persons suffering with pain, professional societies and advocacy groups, researchers, employers, payers, elected officials and the media – all on a scale we have not done before. To be successful, we must all be part of the dialogue and the solution, and speak with one voice. Successful implementation of these strategic goals will create the cultural transformation in pain prevention, care, and education called for in the IOM Pain Report and called for by the American public.
Future Needs: Learning Health Systems and Precision Pain Medicine
The future of pain assessment, prevention and treatment will require improvements in clinical education, public and institutional policies and population-level epidemiologic, health services, social science, medical informatics, implementation, basic biomedical, and other relevant research, informed by clinician/scientist interactions. I will focus on one area where our group is working to advance the recommendations of the IOM Pain Report and the NPS.
As noted previously, despite an increase in the number of available pain therapies, more than 100 million people in the U.S. still live with pain. Little is known about which treatments are best for which patient or even about the efficacy and safety of various treatments over time. In recognizing this conundrum, the IOM Pain Report called for “greater development and use of patient outcome registries that can support point-of-care treatment decision making, as well as for aggregation of large numbers of patients to enable assessment of the safety and effectiveness of therapies.” Coinciding with this call for patient registries is the recognition that Learning Health Systems (LHSs) are an important aspect of the future of medicine [6]. Learning health systems combine science, informatics, incentives and culture that are then aligned for continuous improvement and innovation The Institute of Medicine recently extolled the virtues of LHSs [7], and in 2013 the National Science Foundation convened a workshop where it was declared that LHSs can rapidly inform decisions that have transformative effects on improving health [8].
The IOM has called for LHSs to use data with advanced analytics to transform care. However, there have been technological barriers to the implementation of LHSs. The Stanford-NIH Collaborative Health Outcomes Information Registry (CHOIR; http://CHOIR.stanford.edu) was developed in response to the IOM pain report and the National Pain Strategy, which emphasized the need to improve the collection and reporting of data on pain (Figure 3). The military has also developed a system to address this need called Pain Assessment Screening Tool and Outcomes Registry (PASTOR). [9] The rest of this discussion will use CHOIR as a model platform. CHOIR is an open source, open standard, free, secure, electronic, learning healthcare system is designed to capture detailed, longitudinal patient-reported outcomes data on physical, psychological, and social health. CHOIR was developed to: inform point of care decision making, provide software based decision making, and act as a platform for (1) comparative effectiveness research, (2) longitudinal outcomes research, and (3) practice based evidence trials.
Figure 3.
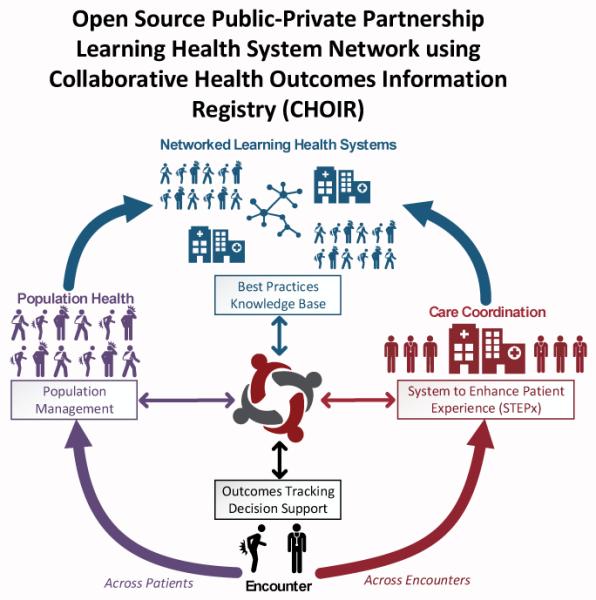
Courtesy of Ming-Chih Kao, PhD, MD, Palo Alto, CA.
While traditional narrowly focused biomedical approach to medical treatment have been successful for some diseases (e.g. infectious diseases), there is a need to efficiently characterize the multidimensional nature of our patients in chronic disease management. Increasingly there is greater awareness in the roles of psychological and social factors in disease incidence, magnitude, and persistence, as well as its associated costs of care. In concert, there are increasingly needs to measure and monitor psychological and social factors in order to better manage these complex diseases. CHOIR integrates NIH Patient Reported Outcomes Measurement Information System (PROMIS) measures to efficiently and rapidly capture 15-20 domains of physical, psychological and social functioning.
The NIH PROMIS measures have been integrated into CHOIR to maximize efficiency in data capture through cloud-based computation with adaptive algorithms for items with wide dynamic range, and computerized adaptive testing. This testing has been shown to reduce patient response burden by as much as 70% and facilitate continued patient participation. An additional strength of PROMIS measures is that they permit for comparisons of individual patients against national population norms. [9, 10]
While evidence-based medicine is the standard for supporting clinical-decision making, the paucity of prospective, placebo-controlled randomized trials in pain medicine has generated an urgent need to accurately and consistently measure relevant patient outcomes with the goal of defining the most safe and effective treatments. There is a need to standardize the assessment and reporting of outcomes to allow for comparison across studies and different patient populations. In addition to prospective, placebo-controlled randomized trials, which can be difficult to generalize due to participant homogeneity, and require a large amount of resources (due to sample size), systematic practice-based evidence may provide more useful data in the form of prospective, observational, cohort studies. [11] Standardized data capture can be included as part of ongoing routine clinical hand and pain management from both patients and providers. CHOIR was developed to allow for low-cost, large, prospective, observational studies on thousands of patients in a “real-world” clinic setting. CHOIR, and other LHSs, have the potential to address many fundamental questions regarding pain treatment and efficacy, and will allow for further characterization of optimal patients for specific therapies.[11, 12]
In addition to the broad research utility of CHOIR, the system provides computer-assisted documentation, which has proven indispensable and invaluable in delivering comprehensive, targeted interdisciplinary pain treatment. The platform is designed to be customizable to different settings (inpatient and ambulatory), providers, and disease conditions. Use of CHOIR will facilitate real-time comparison of patient data to clinic, national, and disease-specific norms. CHOIR has demonstrated efficiency, low-cost, and minimal burden to staff, providers, and patients, while augmenting clinical care. CHOIR provides rapid real-time, longitudinal feedback to clinicians regarding standardized quantitative outcomes to guide decision-making regarding various treatments. [11]
President Obama has recently called for a Precision Medicine Initiative. Precision medicine is an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person. While President Obama has called for a near-term focus of precision medicine to be cancers, the long-term aim is to apply this knowledge to the whole range of health and disease – including pain management. [13] This effort will require a further advances in molecular biology, ‘omics (e.g. genomics, metabolomics, proteomics), and bioinformatics. Learning health systems will play a significant role in integrating this systems based information to derive accurate prevention and treatment recommendations. These learning health systems and precision pain medicine are within our grasp. Successful implementation will ultimately realize the call by the IOM Relieving Pain in America Report to provide everyone the best pain assessment, prevention and treatment.
Key Points.
- Chronic pain affects 100 million Americans and costs our country half a trillion dollars per year.
- Chronic pain can be a disease in itself. We need to better understand the complex mechanisms of pain and translate these mechanisms into safe and effective therapies.
- We need to increase and incentivize the use of interdisciplinary, team based assessment of chronic pain, particularly in complex cases.
- For a precision pain medicine approach, we need improved data that characterizes the individual pain experience and the outcomes of treatments.
Footnotes
THE AUTHOR HAS NOTHING TO DISCLOSE
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Institute of Medicine (U.S.) Relieving pain in America : a blueprint for transforming prevention, care, education, and research. xvii. National Academies Press; Washington, D.C.: 2011. Committee on Advancing Pain Research Care and Education; p. 364. [PubMed] [Google Scholar]
- 2.Pizzo PA, Clark NM. Alleviating suffering 101--pain relief in the United States. The New England journal of medicine. 2012;366(3):197–9. doi: 10.1056/NEJMp1109084. doi: 10.1056/NEJMp1109084. PubMed PMID: 22256802. [DOI] [PubMed] [Google Scholar]
- 3.Carroll I, Barelka P, Wang CK, Wang BM, Gillespie MJ, McCue R, et al. A pilot cohort study of the determinants of longitudinal opioid use after surgery. Anesthesia and analgesia. 2012;115(3):694–702. doi: 10.1213/ANE.0b013e31825c049f. Epub 2012/06/26. doi: 10.1213/ANE.0b013e31825c049f. PubMed PMID: 22729963. [DOI] [PubMed] [Google Scholar]
- 4.Carroll I, Hah J, Mackey S, Ottestad E, Kong JT, Lahidji S, et al. Perioperative interventions to reduce chronic postsurgical pain. Journal of reconstructive microsurgery. 2013;29(4):213–22. doi: 10.1055/s-0032-1329921. doi: 10.1055/s-0032-1329921. PubMed PMID: 23463498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hah JM, Mackey S, Barelka PL, Wang CK, Wang BM, Gillespie MJ, et al. Self-loathing aspects of depression reduce postoperative opioid cessation rate. Pain Med. 2014;15(6):954–64. doi: 10.1111/pme.12439. doi: 10.1111/pme.12439. PubMed PMID: 24964916; PubMed Central PMCID: PMC4083472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Friedman CP, Wong AK, Blumenthal D. Achieving a nationwide learning health system. Sci Transl Med. 2010;2(57):57cm29. doi: 10.1126/scitranslmed.3001456. Epub 2010/11/12. doi: 10.1126/scitranslmed.3001456. PubMed PMID: 21068440. [DOI] [PubMed] [Google Scholar]
- 7.(IOM) IoM Characteristics of a Continuously Learning Health Care System. http://www.iom.edu/Reports/2012/Best-Care-at-Lower-Cost-The-Path-to-Continuously-Learning-Health-Care-in-America/Table.aspx 2012 [updated 9/12; cited 2014]
- 8.Friedman C, Rubin J, Brown J, Buntin M, Corn M, Etheredge L, et al. Toward a science of learning systems: a research agenda for the high-functioning Learning Health System. Journal of the American Medical Informatics Association : JAMIA. 2014 doi: 10.1136/amiajnl-2014-002977. doi: 10.1136/amiajnl-2014-002977. PubMed PMID: 25342177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cook KF, Buckenmaier C, 3rd, Gershon RC. PASTOR/PROMIS (R) pain outcomes system: what does it mean to pain specialists? Pain Manag. 2014;4(4):277–83. doi: 10.2217/pmt.14.25. doi: 10.2217/pmt.14.25. PubMed PMID: 25300385. [DOI] [PubMed] [Google Scholar]
- 10.Gershon RC, Rothrock N, Hanrahan R, Bass M, Cella D. The use of PROMIS and assessment center to deliver patient-reported outcome measures in clinical research. J Appl Meas. 2010;11(3):304–14. PubMed PMID: 20847477; PubMed Central PMCID: PMC3686485. [PMC free article] [PubMed] [Google Scholar]
- 11.Bruehl S, Apkarian AV, Ballantyne JC, Berger A, Borsook D, Chen WG, et al. Personalized medicine and opioid analgesic prescribing for chronic pain: opportunities and challenges. The journal of pain : official journal of the American Pain Society. 2013;14(2):103–13. doi: 10.1016/j.jpain.2012.10.016. doi: 10.1016/j.jpain.2012.10.016. PubMed PMID: 23374939; PubMed Central PMCID: PMC3564046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sturgeon JA, Darnall BD, Kao MC, Mackey SC. Physical and psychological correlates of fatigue and physical function: a Collaborative Health Outcomes Information Registry (CHOIR) study. The journal of pain : official journal of the American Pain Society. 2015;16(3):291–8. doi: 10.1016/j.jpain.2014.12.004. e1. doi: 10.1016/j.jpain.2014.12.004. PubMed PMID: 25536536; PubMed Central PMCID: PMC4352393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collins FS, Varmus H. A new initiative on precision medicine. The New England journal of medicine. 2015;372(9):793–5. doi: 10.1056/NEJMp1500523. doi: 10.1056/NEJMp1500523. PubMed PMID: 25635347. [DOI] [PMC free article] [PubMed] [Google Scholar]


