Abstract
Background: Cervical cancer is the fourth most common cancer among women worldwide. Organized cervical screening and vaccination against human papilloma virus (HPV) have been successful interventions for prevention of invasive cervical cancer (ICC). Because of cultural and religious considerations, ICC has low incidence in Iran and many other Muslim countries. There is no organized cervical screening in these countries. Therefore, ICC is usually diagnosed in advanced stages with poor prognosis in these countries. We performed a priority setting exercise and suggested priorities for prevention of ICC in this setting.
Methods: We invited experts and researchers to a workshop and asked them to list important suggestions for ICC prevention in Iran. After merging similar items and removing the duplicates, we asked the experts to rank the list of suggested items. We used a strategy grid and Go-zone analysis to determine final list of priorities for ICC prevention in Iran.
Results: From 26 final items suggested as priorities for prevention of ICC, the most important priorities were developing national guidelines for cervical screening and quality control protocol for patient follow-up and management of precancerous lesions. In addition, we emphasized considering insurance coverage for cervical screening, public awareness, and research priorities, and establishment of a cervical screening registry.
Conclusion: A comprehensive approach and implementation of organized cervical screening program is necessary for prevention of ICC in Iran and other low incidence Muslim countries. Because of high cost for vaccination and low incidence of cervical cancer, we do not recommend HPV vaccination for the time being in Iran.
Keywords: Invasive Cervical Cancer (ICC), Priority Setting, Screening, Prevention and Control, Iran
Introduction
Invasive cervical cancer (ICC) is the fourth most common cancer type among females worldwide. 1 Human papilloma virus (HPV) is necessary cause for occurrence of cervical cancer. 2 Organized cervical screening with Pap smear and HPV testing methods has led to prevention of ICC in the high income countries. 3-5 Recently, the HPV vaccination was successfully introduced to prevent infection of HPV oncotypes and eradicate of cervical cancer. 6 However, lack of organized cervical screening programs in low- and middle-income countries (LMICs) has led to disparities and higher mortality to incidence ratios (MIRs) of ICC in these countries. 1
For cultural and religious reasons, Muslim women abstain from sexual intercourse until their marriage and sexual relationship is restricted to their single partners 7-9; therefore, cervical cancer has very low incidence rates in Iran and several other Muslim countries. For instance, the age standardized incidence rate (ASR( of ICC was estimated to be about 5 per 100000 in Iran. 10,11 As a result, ICC is not considered a major public health problem and most of these countries have no organized cervical screening program. Moreover, some Muslim women are reluctant to undergo cervical screening. 7,12-15 Therefore, in spite of a low incidence rate, patients are usually diagnosed in advance stages and experience a poor prognosis. 16
The resources for public health interventions are always limited, especially in the LMICs and public health organizations should choose among several options available to them. Therefore, they face challenges to prioritize among these options and to select the interventions that may have higher impact on improving the public’s health. 17 The World Health Organization (WHO) considered the research priority setting as “the catalyst for public debate, for bringing together different stakeholders, and for creating networks.” 18 In addition, it was postulated that research priority setting leads to consensus about areas where increased research efforts including coordination, collaboration, and investment will increase the benefit to society. 19 Priority setting is not limited to research programs and it is an important concept in public health programs. It is important to prioritize the interventions that have higher impact, in particular in the low resource settings. However, it is important to use an evidence base approach and involve wide range of stakeholders in the priority setting exercise. 19
We used a standard priority setting approach to develop a list of suggestions with higher priorities for ICC prevention in Iran. The results of this study will help the policy-makers, research community, and other stakeholders to take necessary actions and improve prevention of cervical cancer in the country.
Methods
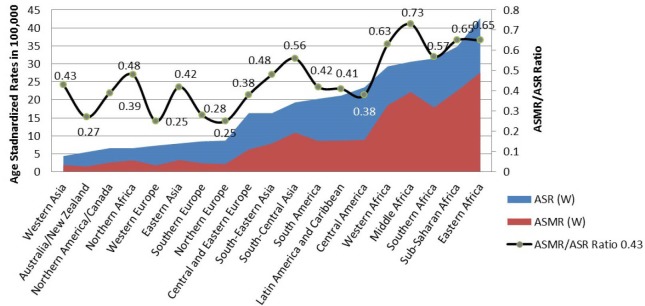
Two teams were involved in this priority setting exercise including the coordinating team and an expert panel. The coordinating team was responsible for methodological issues, literature review and coordination and management of the whole priority setting process. The expert panel was responsible to suggest priority items, participate in the technical and scientific discussion and rank them according to their expertise and the latest scientific evidence. Process of the priority setting exercise was summarized in Figure 1 and described in the following paragraphs.
Figure 1.
Priority Setting Process for Cervical Cancer Prevention in Iran in 2013.
Step 1- Literature Review
We reviewed the literature and assessed international and regional incidence and mortality rates of ICC, and different strategies for cervical prevention worldwide. In addition, we used data from Globocan 2012 and compared the incidence and mortality rate of ICC in different countries. 20 In addition, we studied incidence and mortality rates as well as the mortality to incidence ratio (MIR) of ICC in low incidence Muslim countries.
Step 2- Team building
We identified and nominated national scientists with expertise in cervical cancer prevention. In addition, we identified policy-makers and organizations that were involved in cervical screening in the country. The expert were comprised of 19 clinicians (ie, 3 cancer surgeons, 2 pathologists, 3 medical oncologist, 4 gynecologist, 1 radiotherapist, 2 nurse practitioner, and 4 obstetricians), 3 faculty members from nursing and midwifery department, 2 epidemiologists, 2 experts in health policy and management, 1 health economist, and 3 officers from the Ministry of Health and Medical Education (MoHME).
Step 3- Priority Setting
Item Generation
We invited all the experts to a 3-day workshop, held in October 2013 at the Cancer Institute of Iran. Overall, 30 individuals (68% female and 32% male) from different disciplines participated in the workshop. The workshop was organized with a grant from Union International Cancer Control (UICC) and the lectures were provided by both international and local speakers. During the workshop, we provided latest information and evidences about cervical cancer prevention in Iran and other countries, international variation about burden of cervical cancer, recommendations about cervical screening programs, screening tests (ie, Pap smear, HPV testing, visual inspection with acid acetic), HPV vaccination, guidelines on management of cervical precancerous lesions, and comparison of opportunistic and organized cervical screening program.
A few days before the workshop, we asked all invitees to prepare and bring their suggestions about improvement of ICC prevention program in Iran to the meeting. Specifically, we asked them to answer the following questions:
1) What are the three priorities for improvement of ICC prevention in Iran?
2) What are the most challenging issues about ICC prevention in Iran?
On the first day of the workshop, we presented detailed information about methodology of the priority setting and clarified their role in the process. Afterwards, we provided a list of most recommendations for ICC prevention which had been extracted from literature as well as the responses we received from the participants before the workshop. We asked the participants to review the initial list and add additional items if necessary.
Item Reduction and Clustering
The list of items that were generated in previous steps was comprised of 83 subjects. We reduced the list down to 26 items after elimination of duplicates and merging of overlapping items. The final list was categorized into 5 clusters:
1) Planning of ICC prevention program
2) Implementation of the programs
3) Quality control program
4) Epidemiological and clinical research
5) Training and health promotion activities.
Ranking
In the second day of the workshop, the participants reviewed the final list and ranked them in 2 dimensions of importance and feasibility, using a 1-9 point Likert scale system, in which score one denoted as the least important/feasible and score 9 denoted as the most important/feasible intervention for improvement of cervical cancer prevention in Iran.
Re-ranking
One month after the first round of the ranking, we invited the expert panel to the second meeting and asked them to review the results of initial ranking and confirm or revise them if necessary. The results were discussed in the second meeting and the panelists ranked the items again for second round.
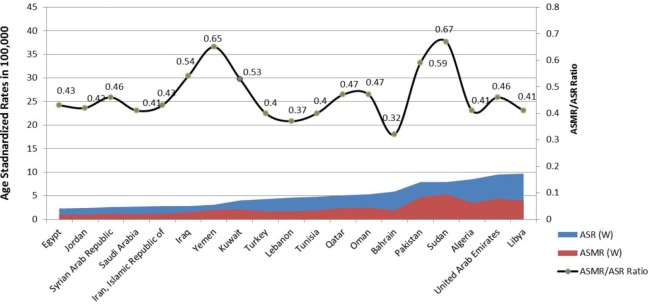
Go-Zone Analysis
We used a scatter plot to create go-zone figures, in which we plotted the average of the importance (Y axis) against feasibility (X axis) scores (Figure 2). 21 The figure was divided into four quadrants (zones) through two perpendicular lines indicating the average of X and Y axes. The four-quadrant scatter plot categorized the items into four groups. The most important and feasible items were located in the right-upper quadrant (RUQ) and the least important and feasible items were located in the left-lower quadrant (LLQ). Finally, the items which were located in the RUQ considered as the top priorities for prevention of ICC in Iran. We used Excel and SPSS version 17.0 software for statistical analyses.
Figure 2.
Go-Zone Analysis for 26 Suggested Statements. Each numbers indicates an ID of the suggested item (see Table )
Results
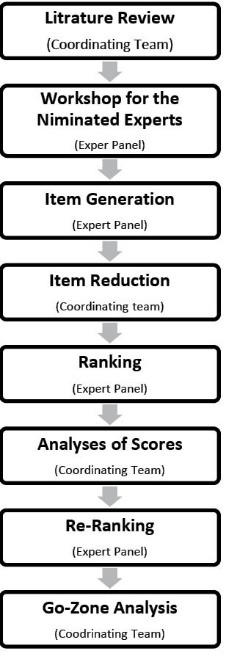
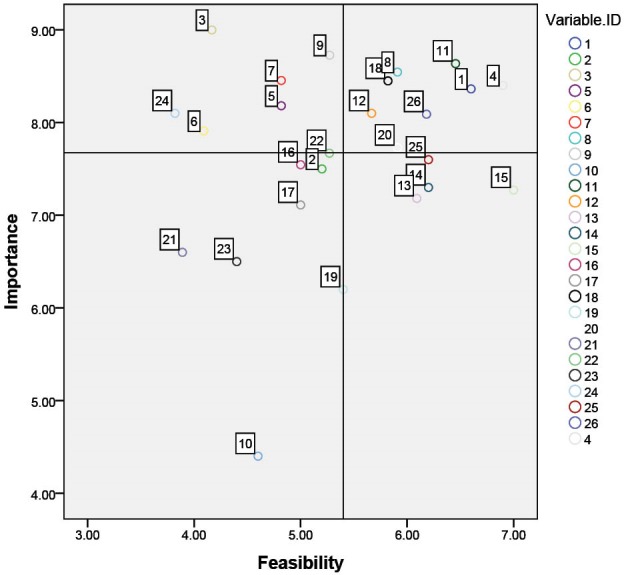
We observed the lowest incidence rates of ICC for Western Asia (ASR=4.4), Australia and New Zealand (ASR=5.5), North Africa (ASR=6.6), North America and Canada (ASR=6.6), and Western Europe (ASR=7.3). However, MIR was higher in Western Asia (MIR=0.43), and North Africa (MIR=0.48) compared to Australia (MIR=0.27), Western Europe (MIR=0.25), and North American (0.25) (Figure 3). African countries had the highest incidence and mortality rates of ICC. Evaluation of ICC statistics in Muslim countries which mostly located in the Middle East and North Africa, showed that although the ASR of ICC was low in most of the Muslim countries, MIR was higher than 0.40 in all countries, except for Bahrain in which the MIR was 0.32 (Figure 4).
Figure 3.
International Variation of Age Standardized Incidence (ASR) and Mortality (ASMR) Rates Per 100000 Women and ASMR/ASR Ratio (Source: Globocan 2012)
Figure 4.
Age Standardized Incidence (ASR) and Mortality (ASMR) Rates Per 100000 Women and ASMR/ASR Ratio Among Low Incidence Muslim Countries (Source: Globocan 2012).
In overall, 26 suggestions were provided by the expert panel for improvement of cervical cancer prevention in Iran (Table ). The suggested actions were categorized in six areas including (1) planning, (2) program implementation, (3) quality control program, (4) research, and (5) health promotion and training.
Table . Suggested Statements Clustered and Ranked Based on Importance and Feasibility for Each Cluster .
| Clusters | Statements in Each Cluster (Statement ID) | Importance | Feasibility |
| Planning | Developing a national ICC prevention guideline and defining appropriate screening test, starting age and interval for regular screenings (1) | 8.4 | 6.6 |
| Developing protocols for screening process and follow-up of the patients with precancerous lesions (2) | 7.5 | 5.2 | |
| Implementation of screening programs | Using an electronic registration system for screening data (8) | 8.6 | 5.9 |
| Coverage of cervical screening by insurance companies (4) | 8.4 | 6.9 | |
| Providing necessary equipment and resources to laboratories for screening test (kits, instruments, personnel, and etc.) (7) | 8.5 | 4.8 | |
| Engagement of family physicians and healthcare system in cervical screening (5) | 8.2 | 4.8 | |
| Elimination of legal boundaries and implementing an organize cervical screening by MoHME (3) | 9.0 | 4.1 | |
| Using appropriate screening strategy to increase the participation rate in the screening program (6) | 7.9 | 4.1 | |
| Quality control program | Developing quality control protocols for the process of patient follow-up (ie, management of precancerous lesions and the treatment of cancer patients) (11) | 8.6 | 6.5 |
| Developing quality assurance protocols for laboratories that are involved in the screening program (9) | 8.7 | 5.3 | |
| Developing quality assurance protocols for management of the screening program in terms of accuracy and coverage (10) | 4.4 | 4.6 | |
| Research | Evaluating the role of partners/husbands in participation of women in cervical screening (18) | 8.5 | 5.8 |
| Conducting cost-effectiveness study for HPV vaccination in Iran (12) | 8.1 | 5.7 | |
| Regular monitoring of the incidence and prevalence of precancerous lesions (20) | 7.7 | 5.9 | |
| Evaluation of benefits and requirement for using Liquid Base Cytology technique for cervical screening test (15) | 7.3 | 7.0 | |
| Identifying the incentives and barriers for participation in cervical cancer screening in the country (14) | 7.3 | 6.2 | |
| Nationwide study of survival rate and prognostic factors for cervical cancer (22) | 7.7 | 5.3 | |
| Determining the risk factors of cervical cancer specially determining variations in high risk behaviors associated with the incidence of cervical cancer among young people (13) | 7.2 | 6.1 | |
| Identifying the knowledge, attitude, and practice of target group women and healthcare providers about cervical cancer screening programs (16) | 7.6 | 5.0 | |
| Determining the prevalence of HPV infection and precancerous lesions among high-risk groups (17) | 7.1 | 5.0 | |
| Conducting a demonstration project for organized screening program in a selected province (24) | 8.1 | 3.8 | |
| Accurate assessment of the incidence, prevalence and mortality of cervical cancer (23) | 6.5 | 4.4 | |
| Evaluation of sero-epidemiology of HPV infection in general population (21) | 6.6 | 3.9 | |
| Research on epidemiology of genital warts (19) | 6.2 | 5.4 | |
| Health promotion and training | Increasing public awareness about cervical cancer screening through mass media (Internet, TV, radio, newspapers, etc.) (26) | 8.1 | 6.2 |
| Training of clinicians and other healthcare providers about cervical screening programs (25) | 7.6 | 6.2 |
Abbreviations: ICC, invasive cervical cancer; MoHME, Ministry of Health and Medical Education; HPV, human papilloma virus.
Top priorities for ICC prevention in Iran which were located in the URQ and were both important and feasible include:
Developing a national guideline and defining appropriate screening test, starting age and interval for regular screenings (item 1);
Developing quality control protocols for follow-up and management of the patients with precancerous lesions and cervical cancer patients (item 11);
Conducting a cost-effectiveness study for HPV vaccination in Iran (item 12);
Coverage of the cervical screening by insurance companies (item 4);
Using an electronic registration system for cervical screening program (item 8);
Evaluating the role of partners/husbands in cervical screening (item 18);
Increasing public awareness about cervical cancer screening through mass media, including internet, TV, radio, newspapers, and etc. (item 26);
Regular monitoring of the incidence and prevalence of precancerous lesions (item 20).
Discussion
Incidence rate of ICC is relatively low in Iran and other Muslim countries; however, the patients are diagnosed in advanced stages and experience poor prognosis, leading to a high MIR in these countries. In this study, we defined priorities for ICC prevention in Iran. The most important priorities were developing a national guideline for organized cervical screening program, and a quality control protocol for cervical screening processes, including the follow-up and management of patients with precancerous lesions.
Development of a national program for ICC prevention was the most important suggestion. It was emphasized that the new plan should consider the best strategy for the type of screening test, starting age for screening, and screening intervals. In addition, development of the national guideline for management of precancerous lesions and patient follow-ups were prioritized in this study. According to current screening guideline in Iran, all women above 21 years of age who had sexual activity are recommended to attend cervical screening every three years. Cervical screening is offered in healthcare centers all over the country; however, there is no active invitation or awareness program to increase motivation of the women to participate in the screening. Women who are health conscious and those who visit a gynecologist or an obstetrician for any reason are advised to participate in cervical screening. 11 Therefore, most women particularly those from low socio-economic groups who are usually at a higher risk for cervical cancer refrain from participation in the screening program. This type of program which is called “opportunistic screening” was shown as non-efficient approach for prevention of ICC. In the opportunistic screening, the coverage is usually low and ICC prevention program is inefficient, leading to the diagnosis of ICC patients in advanced stages. 1,9,22 Sancho-Garnier et al 23 reported that most of the extended Middle East and North African (MENA) countries that lack national guideline and resources for the management of abnormal lesions. They showed that the main obstacle to develop such a national program in these countries has been the lack of political understanding and providing necessary resources for cervical screening program.
There is a wide variation in the cervical screening strategies in different countries. 24 The main variations are related to type of screening test, starting age, and screening intervals. HPV testing, Pap smear tests, and visual inspection with acetic acid (VIA), are three types of screening tests that are used for cervical screening worldwide. 1 Sensitivity, specificity and cost-effectiveness are important parameters for decision about type of the test, starting age, and screening intervals in the ICC prevention program. Because of the low incidence rate of cervical cancer in Iran, there are several proposals to increase the starting age from 21 to 30 or 35 years and increase the screening interval from 3 years to 5 years. 11,25 A cost-effective analysis will suggest optimal strategy vis-à-vis cervical screening in Iran and other Muslim countries.
We emphasized that cervical screening should be free of charge with a full insurance coverage for all women. Otherwise, most of the Iranian women cannot afford cost of cervical screening test and follow-up procedures. Cronjé et al found that affordability and coverage were the most important obstacles for implementation of national cervical screening programs in low resource countries. 23,26 Since 2014, Iranian government has increased the health insurance coverage and all the inpatient costs in the governmental hospitals became free for all patients. Under this reform, management of the patients with precancerous lesion will be covered by insurance benefit packages in Iran. However, screening test and evaluation of the screening samples is not covered yet and could be a major barrier for implementation of an organized screening program. Choosing a cost-effective strategy for cervical screening and decision about type of test, starting age and screening intervals are necessary parameters for estimation of the screening cost and introduction of the screening service in the insurance package. 27 Therefore, the panel suggested starting the negotiation with the insurance companies to cover the cost of screening in their benefit package.
Lack of awareness was reported to be a major factor that may influence participation of women in cervical screening. 28,29 In addition to the affordability and access to cervical screening service, awareness and positive attitudes of women and their families about cervical screening is an important factor for success of screening program. 30-32 Several studies have reported that Iranian women have little information about cervical screening and importance of ICC prevention. 31,33 This study emphasizes that health promotion activity should be prioritized in the new organized program and use appropriate health promotion model for motivation of general population and participation of women in the screening program.
The other important priority was improvement of cancer registry, and considering a registration system for screening program. Iran has a national pathology-based cancer registry program. However, studies showed that quality of this registry is not convincing in Iran. 34 Only one population-based cancer registry (PBCR) which is established in Golestan province in the northeast of Iran has so far met the standard criteria and received approval from International Agency for Research on Cancer (IARC). The results of Golestan province PBCR was published in the IARC book “Cancer in Five Continents, Version X” in 2013. 20 ASR of cervical cancer in Golestan province and in the report of PBCR of Tehran was about 5-6 per 100000, 11,35 which was about 50% higher than rates reported by the national pathology-based cancer registry in Iran, 36 indicating that pathology-based registry underestimate the incidence rate in Iran. Therefore, improvement of PBCR is necessary for evaluation of the cervical cancer prevention program. In addition, we suggested establishing a cervical screening registry and registration of women who participate for screening and their follow-ups. Such a system would be an important component of the screening program and can help public health managers to work efficiently. 37 Screening registry will provide information about timing of screening visits for target women, compliance, and follow-up information about women with abnormal screening tests. Linkage of screening registry and cancer registry data would provide opportunity for regular audit of screening program. 38,39
Bivalent HPV vaccine immunizes women against HPV 16, and 18, and quadrivalent vaccine additionally protects against genotypes 6, and 11. Both vaccines has shown efficacy of over 90% against persistent HPV infection. 40 Several high-income countries have introduced HPV vaccination and try to increase the coverage of vaccination. HPV vaccination could be an effective intervention for ICC prevention in developing world in which screening is available or effective. 41 However, cost of the vaccine is considerably high and the price is a major barrier for administration of the vaccine in developing countries including Iran. Because of the low incidence rate of cervical cancer and very high cost for HPV vaccination, it was not considered as a priority for the time being in Iran. Instead, the panel members suggested conducting a cost-effective study for HPV vaccination in Iran. After this workshop, Khatibi et al 42 evaluated cost-effectiveness of the quadrivalent vaccine and found that HPV vaccination was not cost-effective for Iran.However, the situation may be changed in the future, when the incidence rate of cervical cancer is higher or a cheaper vaccine is available.
This study was the first exercise to develop list of priorities for ICC prevention in Iran. The identified priorities introduce comprehensive recommendations covering all aspects of ICC prevention in Iran, including the program planning, quality assurance, public awareness, and research. The attendees in our meetings were multidisciplinary group, including academic and non-academic experts in the field of ICC prevention. However, we faced some limitations in this study. One of the most important principles in priority setting for public health issues is the involvement of community and taking the viewpoint of the general public. 43-45 Unfortunately, we could not involve community members in this study because the workshop was a scientific event which was conducted in English. We suggest involvement of the community, including health women, and cervical cancer patients in the future analyses.
Conclusion
This priority setting exercise provided important suggestions for prevention of ICC in Iran. Our recommendations can be generalized to other low incidence Muslin countries that lack an organize ICC prevention program. This study implied that policy-makers should prioritize implementation of organized cervical cancer prevention, through development of a national guideline for cervical screening. In addition, implementing a quality assurance program for all procedures of ICC prevention is necessary to make sure that the program will efficiently decrease the burden of cervical cancer. HPV vaccination was not considered a priority for the time being in Iran.
Acknowledgements
This study was conducted in the Cancer Research Center of the Cancer Institute of Iran and supported by Tehran University of Medical Sciences, Tehran, Iran. We would like to thank Dr. Par Sparen for his collaboration in our project as lecturer and his scientific contribution. We, also acknowledge the Union for International Cancer Control (UICC), Geneva, Switzerland for providing a workshop grant (ICRETT Fellowship, 2012) and covering the expenses for travel of the international experts to Iran.
Ethical issues
We did not have any human or animal subjects in this study and did not obtain ethical approval. Therefore, we did not need obtaining ethics approval from the ethics committee in Iran.
Competing interests
Authors declare that they have no conflict of interests and warrant that this manuscript is the result of all authors’ original research.
Authors’ contributions
AM, RGh, MH, AN, AR, and KZ contributed as the methodologist and research team. All authors were involved in the processes of the priority setting study. OM and EW were international experts and provided latest scientific evidence to the workshop participants. AM prepared the first draft of the manuscript and updated the paper according to the comments from authors. All authors appraised the paper and provided their suggestions for improvement of the paper. KZ was principle investigator and guarantees the originality of the material.
Authors’ affiliations
1Cancer Research Center, Cancer Institute of Iran, Tehran University of Medical Sciences, Tehran, Iran. 2Oslo Centre for Biostatistics and Epidemiology, Institute of Basic Medical Sciences, University of Oslo, Oslo, Norway. 3Department of Genecology Oncology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran. 4Department of Reproductive Health, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran. 5Cancer Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran. 6Deputy of Public Health, Maternal Office, Ministry of Health and Medical Education, Tehran, Iran. 7Radiotherapy Research Center, Cancer Institute of Iran, Tehran University of Medical Sciences, Tehran, Iran. 8Central Reference Laboratory, Ministry of Health and Medical Education, Tehran, Iran. 9Department of Pathology, Faculty of Medicine, Tehran University of Medical Sciences, Tehran, Iran. 10Department of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. 11Faculty of Allied Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran. 12Department of Health Management and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. 13Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden. 14Department of Community Medicine, Faculty of Health Sciences, University of Tromsø, The Arctic University of Norway, Tromsø, Norway. 15Department of Research, Cancer Registry of Norway, Institute of Population-Based Cancer Research, Oslo, Norway. 16Department of Genetic Epidemiology, Folkhälsan Research Center, Helsinki, Finland. 17Department of Gynecology and Obstetrics, Odense University Hospital, Odense, Denmark. 18Cancer Model Research Center, Cancer Institute of Iran, Tehran University of Medical Sciences, Tehran, Iran.
Key messages
Implications for policy makers
Policy-makers, scientific community, governmental agencies, private sectors, and non-governmental organizations (NGOs) should contribute to the planning and implementation of an organized cervical cancer prevention program. Cervical cancer screening and treatment services should be accessible and affordable for all women in the country
Improvement of population-based cancer registry program and establishment of cervical screening registry are necessary for regular monitoring and evaluation of the screening program and should be prioritized in parallel to screening program.
Funding agencies should support research priorities suggested in this study. The results from these studies can be used for improvement of invasive cervical cancer (ICC) prevention in the future.
Implications for public
We suggested prioritizing public awareness and providing necessary information to the women about cervical cancer prevention and importance of regular attendance in the cervical screening program. Women should consider the criteria of the national guideline for attendance in the screening program, including starting age, and screening intervals. As emphasized in this study, follow-up and management of the abnormal tests and precancerous lesions is crucial. Women who receive an abnormal result from screening test, must attend the healthcare centers or hospitals for further evaluation and necessary treatment. Otherwise, they may miss the opportunity for timely diagnosis and treatment of cancer. Unfortunately, the cancer patients with a delayed diagnosis would have poor prognosis and high mortality rate compared to the patients who are diagnosed earlier.
Citation: Majidi A, Ghiasvand R, Hadji M, et al. Priority setting for improvement of cervical cancer prevention in Iran. Int J Health Policy Manag. 2016;5(4):225–232. doi:10.15171/ijhpm.2015.201
References
- 1. Nathalie B, O’Neal Eckert L, Andreas U, Paul B. Comprehensive Cervical Cancer Control: A Guide to Essential Practice . 2nd ed. Austuralia: World Health Organization; 2014. [PubMed]
- 2.Walboomers JM, Jacobs MV, Manos MM. et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 3.Campbell CMP, Menezes LJ, Paskett ED, Giuliano AR. Prevention of invasive cervical cancer in the United States: past, present, and future. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1402–1408. doi: 10.1158/1055-9965.EPI-11-1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnholtz-Sloan J, Patel N, Rollison D, Kortepeter K, MacKinnon J, Giuliano A. Incidence trends of invasive cervical cancer in the United States by combined race and ethnicity. Cancer Causes Control. 2009;20(7):1129–1138. doi: 10.1007/s10552-009-9317-z. [DOI] [PubMed] [Google Scholar]
- 5.Vaccarella S, Lortet-Tieulent J, Plummer M, Franceschi S, Bray F. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013;49(15):3262–3273. doi: 10.1016/j.ejca.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 6.Zwaveling S, Mota SCF, Nouta J. et al. Established human papillomavirus type 16-expressing tumors are effectively eradicated following vaccination with long peptides. J Immunol. 2002;169(1):350–358. doi: 10.4049/jimmunol.169.1.350. [DOI] [PubMed] [Google Scholar]
- 7.Dikshit R, Gupta PC, Ramasundarahettige C. et al. Cancer mortality in India: a nationally representative survey. Lancet. 2012;379(9828):1807–1816. doi: 10.1016/s0140-6736(12)60358-4. [DOI] [PubMed] [Google Scholar]
- 8.Wasti S, Ahmed W, Jafri A, Khan B, Sohail R, Hassan S. Analysis of cervical smears in a Muslim population. Ann Saudi Med. 2004;24:189–192. doi: 10.5144/0256-4947.2004.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badar F, Anwar N, Meerza F, Sultan F. Cervical carcinoma in a Muslim community. Asian Pac J Cancer Prev. 2007;8(1):24. [PubMed] [Google Scholar]
- 10. GLOBOCAN 2012. Estimated Cancer Incidence, mortality and prevalence worldwide in 2012; 2014. http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.
- 11.Khorasanizadeh F, Hassanloo J, Khaksar N. et al. Epidemiology of cervical cancer and human papilloma virus infection among Iranian women - analyses of national data and systematic review of the literature. Gynecol Oncol. 2013;128(2):277–281. doi: 10.1016/j.ygyno.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 12.Bhurgri Y, Nazir K, Shaheen Y. et al. Patho-epidemiology of cancer cervix in Karachi South. Asian Pac J Cancer Prev. 2007;8(3):357. [PubMed] [Google Scholar]
- 13.Wong YL, Chinna K, Mariapun J, Shuib R. Correlates between risk perceptions of cervical cancer and screening practice. Prev Med. 2013;57:S24–S26. doi: 10.1016/j.ypmed.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 14.De Alba I, Hubbell FA, McMullin JM, Sweningson JM, Saitz R. Impact of US citizenship status on cancer screening among immigrant women. J Gen Intern Med. 2005;20(3):290–296. doi: 10.1111/j.1525-1497.2005.40158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sengul D, Altinay S, Oksuz H, Demirturk H, Korkmazer E. Population-based cervical screening outcomes in Turkey over a period of approximately nine and a half years with emphasis on results for women aged 30-34. Asian Pac J Cancer Prev. 2014;15:2069–2074. doi: 10.7314/APJCP.2014.15.5.2069. [DOI] [PubMed] [Google Scholar]
- 16.Behnamfar F, Azadehrah M. Factors associated with delayed diagnosis of cervical cancer in iran-a survey in isfahan city. Asian Pac J Cancer Prev. 2014;16(2):635–639. doi: 10.7314/apjcp.2014.15.5.2069. [DOI] [PubMed] [Google Scholar]
- 17.Mitton C, Donaldson C. Health care priority setting: principles, practice and challenges. Cost Eff Resour Alloc. 2004;2(1):3. doi: 10.1186/1478-7547-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization (WHO). Priority Setting Methodologies in Health Research:A workshop convened by WHO’s Cluster on Information, Evidence and Research (IER), its Department for Research Policy and Cooperation (RPC) and the Special Programme for Research and Training in Tropical Diseases (TDR). Geneva: WHO; 2008.
- 19.Bryant J, Sanson-Fisher R, Walsh J, Stewart J. Health research priority setting in selected high income countries: a narrative review of methods used and recommendations for future practice. Cost Eff Resour Alloc. 2014;12:23. doi: 10.1186/1478-7547-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Forman D, Bray F, Brewster D, et al. Cancer Incidence in Five Continents. Lyon: IARC; 2013.
- 21.Viergever RF, Olifson S, Ghaffar A, Terry RF. A checklist for health research priority setting: nine common themes of good practice. Health Res Policy Syst. 2010;8:36. doi: 10.1186/1478-4505-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Eyd GJ, Shaik RB. Rate of opportunistic pap smear screening and patterns of epithelial cell abnormalities in pap smears in Ajman, United arab emirates. Sultan Qaboos University Medical Journal. 2012;12(4):473. doi: 10.12816/0003173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sancho-Garnier H, Khazraji YC, Cherif MH. et al. Overview of cervical cancer screening practices in the Extended Middle East and North Africa countries. Vaccine. 2013;31:G51–G57. doi: 10.1016/j.vaccine.2012.06.046. [DOI] [PubMed] [Google Scholar]
- 24.Nahvijou A, Hadji M, BaratiMarnani A. et al. A systematic review of economic aspects of cervical cancer screening strategies worldwide: discrepancy between economic analysis and policymaking. Asian Pac J Cancer Prev. 2014;15(19):8229–8237. [PubMed] [Google Scholar]
- 25.Khodakarami N, Farzaneh F, Yavari P, Khayamzadeh M, Taheripanah R, Akbari ME. The New Guideline for Cervical Cancer Screening in Low Risk Iranian Women. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2014;17(95):8–17. [In Persian]. [Google Scholar]
- 26.Cronjé H. Cervical screening strategies in resourced and resource-constrained countries. Best Pract Res Clin Obstet Gynaecol. 2011;25(5):575–584. doi: 10.1016/j.bpobgyn.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Nahvijou A, Sari AA, Zendehdel K, Marnani AB. Management of precancerous cervical lesions in iran: a cost minimizing study. Asian Pac J Cancer Prev. 2014;15(19):8209. doi: 10.7314/apjcp.2014.15.19.8209. [DOI] [PubMed] [Google Scholar]
- 28.Nwankwo K, Aniebue U, Aguwa E, Anarado A, Agunwah E. Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women: a call for education and mass screening. Eur J Cancer Care (Engl) 2011;20(3):362–367. doi: 10.1111/j.1365-2354.2009.01175.x. [DOI] [PubMed] [Google Scholar]
- 29.Eaker S, Adami HO, Sparen P. Reasons women do not attend screening for cervical cancer: a population-based study in Sweden. Prev Med. 2001;32(6):482–491. doi: 10.1006/pmed.2001.0844. [DOI] [PubMed] [Google Scholar]
- 30.Jalalvandi M, Khodadoostan M. Married women and pap smear, what they know? how they do? Iran J Nurs. 2005;18(41):139–144. [Google Scholar]
- 31.Farzaneh F, Shirvani HE, Barouti E, Salehpour S, Khodakarami N, Alizadeh K. Knowledge and attitude of women regarding the human papillomavirus (HPV) infection, its relationship to cervical cancer and prevention methods. Med J Malaysia. 2011;66(5):468–473. [PubMed] [Google Scholar]
- 32.Abedian Z, Dormahammadi M. Investigating awareness, attitude and practice of women who referred to health centers of Mashhad city toward Pop smear. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2013;15(36):22–28. [Google Scholar]
- 33.Javanmanesh F, Dadkhah F, Zarepour N. Knowledge and awareness among Iranian women regarding the pap smear. Med J Islam Repub Iran. 2008;22(2):68–73. [Google Scholar]
- 34.Zendehdel K, Sedigh Z, Hassanloo J, Nahvijou A. Audit of a nationwide pathology-based cancer registry in Iran. BCCR. 2011;2:7–13. [Google Scholar]
- 35.Etemadi A, Sadjadi A, Semnani S, Nouraie SM, Khademi H, Bahadori M. Cancer registry in Iran: a brief overview. Arch Iran Med. 2008;11(5):577–580. [PubMed] [Google Scholar]
- 36.Zendehdel K. Completeness and underestimation of cancer mortality rate in Iran: a report from Fars province in Southern Iran. Arch Iran Med. 2015;18(3):160. [PubMed] [Google Scholar]
- 37.Arbyn M, Anttila A, Jordan J. et al. European Guidelines for Quality Assurance in Cervical Cancer Screening Second edition--summary document. Ann Oncol. 2010;21(3):448–458. doi: 10.1093/annonc/mdp471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andrae B, Kemetli L, Sparen P. et al. Screening-preventable cervical cancer risks: evidence from a nationwide audit in Sweden. J Natl Cancer Inst. 2008;100(9):622–629. doi: 10.1093/jnci/djn099. [DOI] [PubMed] [Google Scholar]
- 39.Azerkan F, Sparen P, Sandin S, Tillgren P, Faxelid E, Zendehdel K. Cervical screening participation and risk among Swedish-born and immigrant women in Sweden. Int J Cancer. 2012;130(4):937–947. doi: 10.1002/ijc.26084. [DOI] [PubMed] [Google Scholar]
- 40.Cutts FT, Franceschi S, Goldie S. et al. Human papillomavirus and HPV vaccines: a review. Bull World Health Organ. 2007;85(9):719–726. doi: 10.2471/blt.06.038414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stanley M. Human papillomavirus vaccines versus cervical cancer screening. Clin Oncol. 2008;20(6):388–394. doi: 10.1016/j.clon.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 42.Khatibi M, Rasekh HR, Shahverdi Z. Cost-effectiveness evaluation of quadrivalent human papilloma virus vaccine for hpv-related disease in Iran. Iran J Pharm Res. 2014;13(Suppl):225. [PMC free article] [PubMed] [Google Scholar]
- 43.Chalmers I, Bracken MB, Djulbegovic B. et al. How to increase value and reduce waste when research priorities are set. Lancet. 2014;383(9912):156–165. doi: 10.1016/s0140-6736(13)62229-1. [DOI] [PubMed] [Google Scholar]
- 44. Neema S. Community participation in essential national health research process: Uganda’s Experience. Report for COHRED’s Working Group on Community Participation. Makerere Institute of Social Science, Makerere University, Uganda; 1999.
- 45. Mbewu A, Mngomezulu K. Health Research in South Africa. The South African Health Review. Durban: Health Systems Trust; 1999.