Abstract
OBJECTIVES
To assess the relationship between the number of primary care providers (PCPs) in an area and emergency department (ED) visits by older adults.
DESIGN
Population-based cross-sectional observational study.
SETTING
Nonfederal EDs in North Carolina in 2010.
PARTICIPANTS
All older adults (n = 640,086) presenting to a nonfederal ED in North Carolina in 2010.
MEASUREMENTS
The primary outcome was the number of ED visits by older adults in each ZIP code per 100 adults aged 65 and older living in that ZIP code. A secondary outcome was the number of ED visits not resulting in hospital admission per 100 older adults. The primary predictor variable was the number of PCPs per 100 older residents for each ZIP code. Covariates included those representing healthcare need (Medicare hospitalizations, nursing home beds), predisposing factors for healthcare use (race, education, population density of older adults), and enabling factors (distance to the nearest ED).
RESULTS
In a multivariable regression model corrected for spatial clustering, ZIP code characteristics associated with ED visits included more hospitalizations by Medicare beneficiaries, more nursing home beds, and closer proximity to an ED. Number of PCPs per 100 older adult residents in each ZIP code was not associated with ED use, and the 95% confidence limit indicates at most a small effect of PCP availability on ED use.
CONCLUSION
These findings suggest that primary care availability has at most a limited effect on ED use by older adults in North Carolina.
Keywords: geriatrics, primary health care, emergency medicine, delivery of health care
U.S. emergency department (ED) visits by adults aged 65 and older increased from 15.9 million in 2001 to 19.8 million in 2009.1 Although the ED is an essential site of care for individuals with acute illness and injury, ED visits are more costly than primary care visits, and ED visits by older adults with complex medical histories and preferences of care may be less efficient than visits to primary care providers (PCPs), who typically already know the individual. Thus, number of ED visits has been identified as a possible measure of PCP performance,2 and reducing the number of these visits has been identified as a desirable outcome in randomized trials. These trials have demonstrated that greater access to primary care for chronically ill older adults can reduce ED visits, hospitalizations, and the cost of care.3–5 Despite the success of these interventions in selected populations, the relationship between availability of primary care and ED use in a general population of older adults has not been described.
In older adults, individual-level characteristics associated with higher rates of ED use include perceived poor health status, previous hospitalization, older age, African-American race, less education, lower income, lack of social support, and urban residence.6–12 These studies failed to account for distance needed to travel for treatment, a known determinant of healthcare use by older adults in rural communities.13 In addition, most of these studies have focused on small populations receiving care in a single healthcare system. The extent to which sociodemographic factors contribute to large-scale variations in ED use by older adults is unknown. Identifying and characterizing areas with high ED use by older adults and, in particular, understanding the effect of PCP availability on ED use has the potential to provide insights into the effect of increasing the availability of primary care on ED use in this growing population.
PURPOSE OF THIS INVESTIGATION
The purposes of this study were to describe geographic variation in ED use by older adults across an entire state and to assess whether the number of PCPs practicing in an area was associated with a lower ED visit rate.
METHODS
Study Design
Emergency department use by individuals aged 65 and older across the state of North Carolina was analyzed at the ZIP code level. Data from the North Carolina Disease Event Tracking and Epidemiological Collection Tool (NC DETECT) were collapsed from individual-level data into ZIP code–level data and then merged with all other data obtained on the ZIP code level, using ZIP code as the linkage variable. The institutional review board at the University of North Carolina at Chapel Hill exempted the study from formal review.
Primary Predictor: PCPs
The primary predictor variable was number of PCPs per 100 older residents for each ZIP code. The North Carolina Health Professions Data System records the number and type of physicians practicing in each ZIP code in North Carolina each year. PCPs were defined as physicians practicing internal medicine, family medicine, or geriatrics and those in general practice. Pediatricians, obstetricians, and physicians in training were not included. Data from 2011 were used for number of PCPs in each ZIP code because, before 2011, data were autopopulated from the prior year. These values and the population aged 65 and older in each ZIP code were used to calculate the primary predictor variable.
Covariates
Results of prior research and the conceptual framework of Andersen’s behavioral model of health services use were used to select covariates for adjusting the relationship between PCP availability and ED use by older adults.11,14 Covariates included those representing healthcare need (Medicare hospitalizations, nursing home beds), predisposing factors for healthcare use (race, education, population density of older adults), and enabling factors (distance to nearest ED). All covariates were measured at the ZIP code level.
Medicare claims data on all hospitalizations from each ZIP code in North Carolina in 2010 were used to calculate the number of hospitalizations of Medicare beneficiaries per 100 older adults in each ZIP code. The number of nursing home beds in each ZIP code was obtained from the Online Survey, Certification and Reporting data network.15 Medicare hospitalizations per 100 older adults and number of nursing home beds per 100 older adults were used as measures of the average health condition of older adults living in each ZIP code.
ZIP code–level demographic data were obtained from the U.S. Census: population aged 65 and older, percentage of white residents aged 65 and older, and percentage of residents aged 25 and older with a college degree. Population density of adults aged 65 and older per square mile was calculated for each ZIP code. Latitude and longitude coordinates for the geographic center of each ZIP code and for the 113 EDs covered by the NC DETECT database16 were used to calculate the distance to the nearest ED in miles.
Outcomes: ED Visits
The number of ED visits by adults aged 65 and older from each ZIP code and the disposition (admitted, transferred, discharged) for each participant was obtained from the NC DETECT database. The NC DETECT database consists of data for each ED visit to all 113 civilian EDs in North Carolina, including but not limited to demographic characteristics (age, sex), ZIP code of residence, arrival date and time, hospital transport mode, chief complaint, and disposition. These data are collected to allow for public health surveillance and research such as this study. The primary outcome was number of ED visits by older adults in each ZIP code per 100 older adult residents in each ZIP code. The secondary outcome was number of ED visits by older adults for which the participant was discharged home after the ED visit in each ZIP code per 100 older adult residents in each ZIP code. Although not all ED visits that are discharged are nonurgent, this secondary outcome was chosen because it identifies a subset of visits that are more likely to be for ambulatory care conditions and thus more likely to be sensitive to the availability of PCPs. Individuals missing age or ZIP code data were excluded from the analysis because their inclusion would not allow visit categorization according to age or ZIP code. Individuals who were not from North Carolina were excluded from analysis because these individuals would not be expected to have access to a PCP in North Carolina, and distance to the nearest ED could not be calculated. Twenty-four ZIP codes were excluded from the analysis because there was no corresponding ZIP code in the shape file used to map the ZIP codes (n = 5), no older adults living in the ZIP code (n = 7), or no ED visits by older adults from that ZIP code (n = 12).
Data Analysis
Spatial autocorrelation in geographic data sets can cause a lack of independence of observations for each area and significant bias in model estimates.17 The extent of spatial autocorrelation (clustering) for each variable was characterized using Moran’s I, a correlation measure with a theoretical range of 1 to +1.17 A value close to 0 indicates that the geographic distribution of the values is random. Positive values indicate a similarity of attribute values between neighboring ZIP codes. The probability that a Moran’s I value was significantly different from 0 was tested using a Monte Carlo simulation with 499 permutations.18 Each variable was also mapped to examine spatial patterning.
The relationship between number of PCPs per 100 older adults and number of ED visits per 100 older adults was first estimated using an aspatial linear regression model. Because the Moran’s I values for the outcome, a number of the covariates, and the residuals from the aspatial regression were significantly greater than 0, the relationship was then estimated using a multivariable spatial error regression (including a spatially lagged error term) and multivariable spatial lag regression (including a spatially lagged dependent variable). In different ways, these two spatial regression models accommodate the lack of independence in the data such that the regression parameters of interest are estimated using an unbiased and efficient maximum likelihood estimator.19 For these analyses, “neighbors” were defined as ZIP code areas that have common boundaries with a given focal ZIP code (first-order queen adjacency).19 These models were adjusted for covariates. The relationship between ED visits per 100 older adults and percentage admitted or transferred was also examined using aspatial scatter plot analysis, spatial error, and spatial lag regression without adjusting for covariates.
Geographically weighted regression (GWR) was used to visually inspect spatial variation in the relationship between PCP availability and ED visits by older adults for each ZIP code after adjustment.20 A Leung test was used to provide a statistical test of variation in this relationship.21 GWR was also used to assess spatial variation in the extent to which the proposed model explained variation in ED use.
Nine sensitivity analyses were performed. Because the definition of PCPs included physicians who could provide care to individuals of any age, an alternate definition of the primary exposure variable was tested, defined as the number of PCPs per 100 adults (aged ≥18) living in the ZIP code, rather than per 100 older adults. A square root transformation for the number of PCPs, nursing home beds, and population density was tested because of the skewed distribution in the scatter plots for these variables. The presence of a nonlinear relationship between the number of PCPs and ED visits by older adults was assessed for by visual inspection of a scatter plot and by estimating a model in which the number of PCPs was represented using three indicator variables (representing four categories). The contribution of this categorical variable to the model was assessed by comparing it with a model without this variable using an F-test. A model that included an interaction between race and education was examined because the map suggested greater ED use in the coastal plain area (ZIP codes with an elevation of less than approximately 150 feet above sea level), an area with high percentages of minorities and individuals with less formal education.22 Estimates of ED use in rural areas may be inflated because transfer rates are higher in these regions, resulting in two ED visits for each individual experiencing an ED-to-ED transfer. To address this, the analyses were repeated after excluding individuals whose ED visit resulted in transfer based on disposition data provided in the NC DETECT data set. Doing this ensured that all visits that resulted in an ED-to-ED transfer were counted as only a single ED visit. Because participants might cross multiple ZIP codes to receive primary care, spatial regressions were also estimated using a third-order queen adjacency definition of neighboring ZIP codes. Because the GWR analysis indicated that the model had greater explanatory power in the eastern and central parts of the state than in the mountains, the model was estimated separately for these two regions. The analysis was also repeated with the inclusion of the 12 ZIP codes with no ED visits by older adults. Finally, to better understand the effect of sociodemographic factors on ED visits rates by older adults, a model was estimated that did not include Medicare hospitalizations, a variable that accounted for much of the variation in the models.
Maps were created using ArcGIS 10.0 (Esri, Redlands, CA). Aspatial regressions were conducted in Stata IC 11.0 (Stata Corp, College Station, TX); spatial regressions were conducted in GeoDa version 0.9.3 (GeoDa Center, Temple, AZ). GWR and the Leung test were conducted using R software version 3.0.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
During 2010, 4,507,808 visits were made to the 113 non-federal NC EDs contributing data to NC DETECT, 722,144 (16.0%) of which were made by individuals aged 65 and older. Excluding individuals who were missing age or ZIP code data or who were not from a North Carolina residential ZIP code left 640,086 ED visits by adults aged 65 and older from 716 ZIP codes (Figure 1) with a total older adult population of 1,199,905 (12.9%). These visits and this population were the basis for all subsequent analyses. Most of these ED visits were by individuals who were white (80.7%) or black (16.5%); 98.0% had some form of health insurance. There were 4,695 PCPs practicing in these 716 residential ZIP codes, 52.3% of whom were family physicians, 45.2% internists, 1.5% geriatricians, and 0.9% general practitioners (Table 1, Figure 2A–G).
Figure 1.
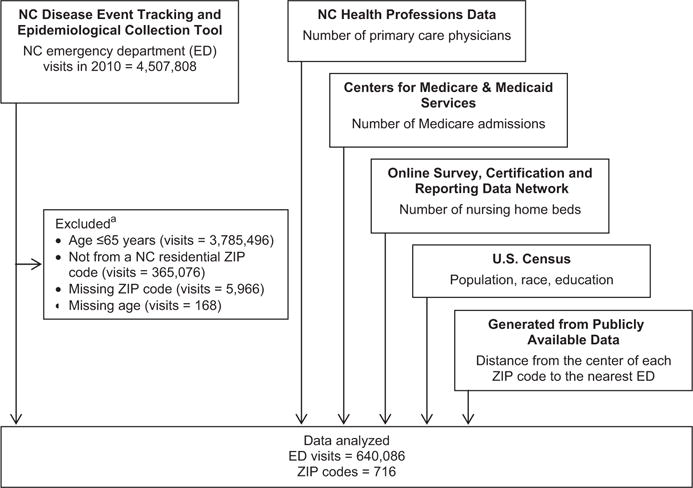
Diagram of sources of data for analysis. aCategories are not mutually exclusive. NC = North Carolina.
Table 1.
Description of ZIP Code-Level Predictors and Outcomes
| ZIP Code-Level Characteristic | Mean ± SD | 5th–95th Percentile | Moran’s I | P-Valuea |
|---|---|---|---|---|
| Predictor | ||||
| Number of primary care providers per 100 older adults | 0.3 ± 0.5 | 0.0–1.0 | 0.18 | <.001 |
| Medicare hospitalizations per 100 older adults | 41.6 ± 16.3 | 23.6–62.6 | 0.16 | <.001 |
| Number of nursing home beds per 100 older adults | 2.6 ± 6.2 | 0.0–10.7 | −0.05 | .029 |
| Percentage white of older adults | 79.8 ± 18.3 | 41.8–99.3 | 0.66 | <.001 |
| Percentage with college degree of aged ≥25 | 13.0 ± 8.2 | 4.5–31.3 | 0.64 | <.001 |
| Population density (per square mile) | 428.9 ± 807.7 | 19.7–1,959.1 | 0.57 | <.001 |
| Distance to closest ED, miles | 5.2 ± 3.9 | 0.6–12.4 | 0.46 | <.001 |
| Outcome | ||||
| ED visits per 100 older adults | 57.0 ± 25.2 | 28.9–88.9 | 0.16 | <.001 |
| ED visits resulting in discharge per 100 older adults | 30.5 ± 15.6 | 13.9–51.0 | 0.18 | <.001 |
Probability that Moran’s I value was significantly different from zero tested with Monte Carlo simulation with 499 permutations.
ED = emergency department.
Figure 2.
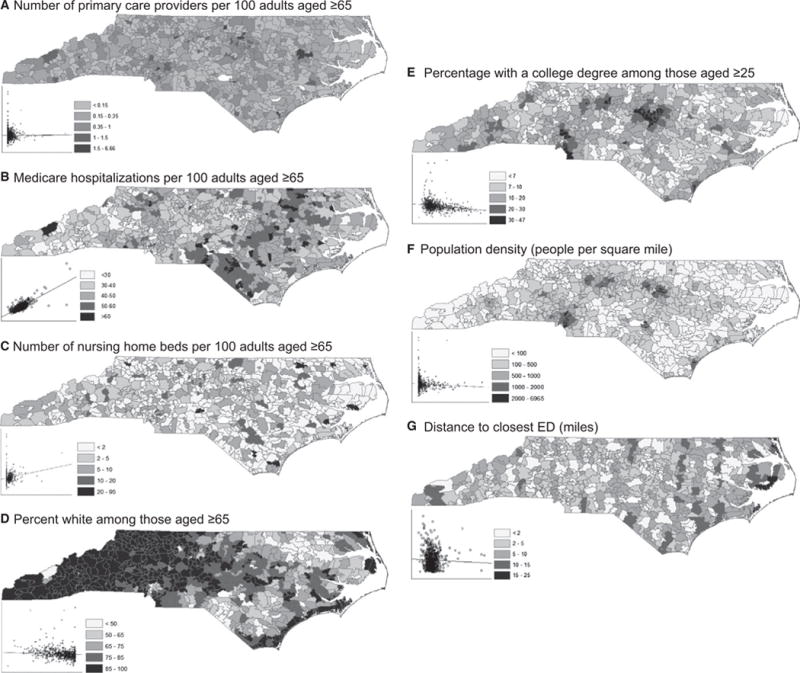
Maps of ZIP code–level characteristics. Scatterplots show the number of emergency department (ED) visits per 100 adults aged ≥65 (y-axis) according to the ZIP code characteristic (x-axis). (A) Number of primary care providers per 100 adults aged ≥65. (B) Medicare hospitalizations per 100 adults aged ≥65. (C) Number of nursing home beds per 100 adults aged ≥65. (D) Percentage white of those aged ≥65. (E) Percentage with a college degree of those aged ≥25. (F) Population density (people per square mile). (G) Distance to closest ED (miles).
The number of ED visits per 100 older adults in each ZIP code ranged from 0.9 to 280 (Figure 3). The 5% of ZIP codes with the lowest ED visit rates had fewer than 30 visits per 100 older adults; the 5% of ZIP codes with the highest ED visit rates had more than 85 visits per 100 older adults. A cluster of high ED visit rates was located in the coastal plain region (P < .001).
Figure 3.
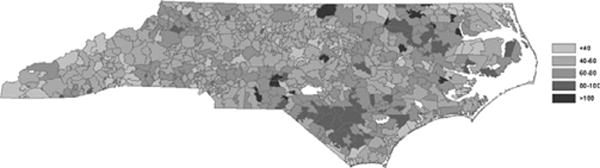
Map of emergency department visits by those aged ≥65 per 100 residents aged ≥65 for each ZIP code (n = 716) in North Carolina in 2010.
An aspatial multivariable regression identified several factors associated with ED visits per 100 older adults (Table 2). The Moran’s I value of 0.966 (P < .001) for the residuals from this aspatial model revealed a systematic pattern of correlated residuals, suggesting the presence of missing variables, other forms of spatial dependence, or both and indicated the need for spatial regression analyses.19,23 The Lagrange multiplier statistics indicated only a slight preference for a spatial error regression model over a spatial lag regression model, so both models were estimated.
Table 2.
Multivariable Regression Results Describing the Relationship Between ZIP Code–Level Characteristics and Number of Emergency Department (ED) Visits by Those Aged 65 and Older per 100 Adult Residents Aged 65 and Older in North Carolina in 2010
| ZIP Code-Level Characteristic | Ordinary Least Squares Regression | Multivariable Spatial Error Regression | Multivariable Spatial Lag Regression | |||
|---|---|---|---|---|---|---|
| Coefficient | P-Value | Coefficient | P-Value | Coefficient | P-Value | |
| Primary care providers per 100 older adults | −1.20 | .33 | −1.46 | .21 | −1.18 | .33 |
| Medicare hospitalizations per 100 older adults | 1.16 | <.001 | 1.19 | <.001 | 1.15 | <.001 |
| Nursing home beds per 100 older adults | 0.73 | <.001 | 0.83 | <.001 | 0.76 | <.001 |
| Percentage white of aged ≥65 | −4.42 | .19 | −3.52 | .40 | 0.50 | .88 |
| Percentage with a college degree of aged ≥25 | 2.08 | .82 | 2.32 | .82 | 8.63 | .34 |
| Population density (per square mile) | −1.6 × 10−3 | .08 | −7.7 × 10−4 | .41 | −1.1 × 10−3 | .22 |
| Distance to closest ED, miles | −0.52 | <.001 | −0.49 | .002 | −0.44 | .002 |
| Spatial regression parameter | – | – | 0.49 | <.001 | 0.19 | <.001 |
| R2 for modela | 0.651 | 0.713 | 0.670 | |||
Of the two spatial regressions estimated, the spatial error model was slightly favored over the spatial lag model based on the larger coefficient of determination (0.713 vs 0.670) and the larger spatial parameter estimate (0.49 vs 0.19). Spatial model estimates provided results similar to those of the aspatial model (Table 2). Interpreting the spatial error model, there was an average of 1.19 more ED visits per 100 older adults for each additional Medicare hospitalization. For each additional nursing home bed per 100 older adults, there were an additional 0.73 ED visits per 100 older adults. The number of PCPs per 100 older adults was not significantly associated with ED visits per 100 older adults; the estimate for the relationship was 1.46 (95% confidence interval = 3.74–0.82). A smaller effect of PCP availability on ED visits was observed with an outcome of ED visits resulting in discharge (Table S1, Figure S1).
The relationship between the number of PCPs and ED visits generated from the GWR output indicated a stronger negative relationship (more PCPs associated with few ED visits) in the southeastern part of the state. A formal test of the difference between the high and low values for this relationship across the state using the Leung test found no evidence of a difference.
Sensitivity analyses did not identify a set of assumptions under which there was a significant relationship between PCP availability and ED use by older adults. Defining the exposure variable as PCPs per 100 adults (aged ≥18) yielded no significant relationship. The interaction between race and education was not significant. The scatterplot of the primary exposure variable and the outcome did not suggest an important nonlinear relationship, and the addition of the primary exposure using categorical variables did not significantly improve model fit. In the coastal plain and Piedmont model, number of Medicare hospitalizations, number of nursing home beds, percentage of white older adults, and proximity of ZIP code to an ED were significant predictors of number of ED visits per 100 older adults. Similar results were seen in the coastal plan and Piedmont region when the outcome was defined as ED visits resulting in discharge per 100 older adults. In the mountain region, only number of Medicare hospitalizations predicted number of ED visits per 100 older adults or ED visits resulting in discharge per 100 older adults. In models in which Medicare hospitalizations was not included as a covariate, PCP presence was still not associated with ED visits, but other factors were: percentage minority, percentage with less than a college education, nursing home beds per 100 older adults, and proximity of ZIP code to an ED.
DISCUSSION
Large variations in ED use by older adults were observed across North Carolina, with a concentrated area of high use in the coastal plain. The population-adjusted proportion of PCPs was not significantly associated with ED use by older adults, and the model did not identify any areas where the relationship between PCP presence and ED use by older adults was statistically significant. Furthermore, sensitivity analyses that explored alternative definitions of important variables or analytical approaches did not identify a significant relationship between PCP presence and ED use by older adults. The lower bound of the 95% confidence interval for this relationship suggests that, for each additional PCP, there were at most four fewer ED visits by older adults over the course of 1 year. Thus, for example, the results suggest that adding 1,000 PCPs would decrease ED visits by older adults by at most 3,740, which is less than 1% of annual ED visits by older adults in the state. The estimate of the effect of PCP presence on older adult ED visits resulting in discharge was even smaller. These estimates suggest that increasing the number of PCPs in the state would have a small effect on ED use by older adults.
Interventions that increase access to PCPs for older adults with chronic illness or disabilities have estimated decreases in ED visits rates of 18% to 40%.3–5,24 The findings of the current study do not directly contradict these findings, which evaluate intensive primary care efforts in chronically ill populations, although they indicate that the reductions observed in these trials are smaller than the large variation in ED use by older adults present across a population and suggest that, in North Carolina, primary care availability as currently provided to older adults has, at most, a small effect on ED use.
These findings are consistent with prior evidence that availability of primary care does not reduce ED visits.25–28 The strongest such evidence comes from the Oregon experiment, in which Medicaid coverage was associated with greater, rather than less, ED use,29 although in that experimental study, those receiving the intervention not only had better access to primary care, but also experienced lower out-of-pocket cost for ED visits. In the current study, the cost of an ED visit would be fairly consistent across the study population, because almost all individuals aged 65 and older in North Carolina have Medicare coverage.
There are several possible explanations for the absence of a strong negative relationship between primary care availability and ED use by older adults. First, primary care and emergency care are not substitutes. EDs provide access to the expertise of physicians trained to assess for life-threatening illness and injury, as well as laboratory testing, advanced imaging, and specialist consultation. Effective PCPs recognize the value of EDs as important referral sites for older adults requiring expedited evaluation for common but potentially life-threating problems, such as falls, acute neurological symptoms, and acute chest or abdominal pain.30 Second, the mechanism by which primary care might decrease ED visits by older adults is by preventing episodic deteriorations in health, providing timely care for acute problems that can be addressed in a primary care office, or shaping expectations and attitudes toward health-care use for older adults with advanced chronic illness. Achieving any of these is challenging. With regard to the last, policies to support substantive conversation between PCPs and chronically ill older adults regarding health priorities and the appropriate use of medical care are needed,31 but whether such policies would decrease ED visits by older adults is unknown. Third, it is possible that the current number of PCPs in North Carolina is below the threshold that would be required to have an effect on ED visits by older adults.
The full model explained approximately 70% of the spatial variation in ED use by older adults, exceeding that from a prior individual-level model containing more-detailed health information.6 The negative association between distance from the ED and ED use has been previously described for pediatric emergency care32 and may be partially explained by the distance decay effect—the concept that those who live further from a healthcare resource use it less.13 Further research is needed to determine what, if any, substitutes for emergency care older adults who live far from an ED use; to examine the relationship between PCP availability and ED use by older adults in other areas of the country; and to more closely investigate the decision-making processes of older adults and their caregivers regarding when and where to seek care.
This study has several limitations. The number of PCPs practicing in a ZIP code is an imperfect measure of the number of PCPs caring for or available to care for older adults. PCPs in some areas may preferentially care or not care for older adults based on their expertise, the insurance coverage of the local population, and other factors. Because geriatricians are a small percentage of PCPs in North Carolina, primary care provided by geriatricians was not differentiated from that provided by nongeriatricians, but geriatricians may have a greater effect on ED use by older adults than nongeriatrician care providers.33 Distance to the nearest ED was defined using linear distance (as the crow flies), not by distance along roads or estimated travel time, and it is not known whether the nearest ED was the one that older adults in each ZIP code generally used. People often travel across numerous ZIP codes to access primary care, but estimates of the relationship between PCP presence and ED visits by older adults did not change when neighboring ZIP codes were defined as those within two or three ZIP codes of each other. All ED visits in the state of North Carolina in 2010 were examined. It is possible that PCP presence is significantly associated with ED visits in other parts of the country or that this relationship has changed over time. It is likely that analysis across larger regions or using individual-level, rather than ZIP code–level, data would provide additional insights into the relationship between PCP availability and ED use by older adults. Finally, income and insurance data were not available at the ZIP code level; these factors might influence ED use and should be examined in future research.
CONCLUSION
Large variations in ED visit rates by older adults across North Carolina were observed, but a significant effect of PCP presence on ED use was not found. These results provide further evidence that primary care is not a substitute for emergency care and challenge the notion that ED visits are an appropriate quality-of-care metric for PCPs or can be substantively decreased solely by increasing the availability of PCPs.
Supplementary Material
Figure S1. Map of Emergency Department Visits Resulting in Discharge by Those Aged 65 Years or Older per 100 Residents Aged 65 Years or Older for Each ZIP Code (n = 716) in North Carolina in 2010.
Table S1. Multivariable Regression Results Describing the Relationship Between ZIP Code-Level Characteristics and the Number of Emergency Department (ED) Visits for Patients Aged 65 Years or Older Who Were Discharged Home per 100 Adult Residents Aged 65 Years or Older in North Carolina in 2010.
Acknowledgments
Dr. Platts-Mills was supported by the University of North Carolina’s Institute on Aging and National Institute on Aging (NIA), National Institutes of Health Award K23AG038548. Katherine Hunold was supported by NIA Award 5-T35-AG038047–03 through the University of North Carolina Summer Research in Aging for Medical Students.
Sponsor’s Role: The National Institutes of Health had no role in the design, methods, data collection, analysis, or preparation of this paper.
Footnotes
Conflict of Interest: The authors do not have any conflict of interest related to this subject matter.
Author Contributions: Hunold, Platts-Mills: study concept and design, data preparation, data analysis and interpretation, preparation of manuscript. Richmond, Voss: data analysis and interpretation, preparation of manuscript. Waller, Cutchin: interpretation of data, preparation of manuscript.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article:
Please note: Wiley-Blackwell is not responsible for the content, accuracy, errors, or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.Pines JM, Mullins PM, Cooper JK, et al. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc. 2013;61:12–17. doi: 10.1111/jgs.12072. [DOI] [PubMed] [Google Scholar]
- 2.Kahane CJ. Injury Vulnerability and Effectiveness of Occupant Protection Technologies for Older Occupants and Women (Report No DOT HS 811 766) Washington, DC: U.S. Department of Transportation National Highway Traffic Safety Administration; 2013. [Google Scholar]
- 3.Counsell SR, Callahan CM, Clark DO, et al. Geriatric care management for low-income seniors: A randomized controlled trial. JAMA. 2007;298:2623–2633. doi: 10.1001/jama.298.22.2623. [DOI] [PubMed] [Google Scholar]
- 4.Scott JC, Conner DA, Venohr I, et al. Effectiveness of a group outpatient visit model for chronically ill older health maintenance organization members: A 2-year randomized trial of the cooperative health care clinic. J Am Geriatr Soc. 2004;52:1463–1470. doi: 10.1111/j.1532-5415.2004.52408.x. [DOI] [PubMed] [Google Scholar]
- 5.Coleman EA, Eilertsen TB, Kramer AM, et al. Reducing emergency visits in older adults with chronic illness. A randomized, controlled trial of group visits. Eff Clin Pract. 2001;4:49–57. [PubMed] [Google Scholar]
- 6.Bazargan M, Bazargan S, Baker RS. Emergency department utilization, hospital admissions, and physician visits among elderly African American persons. Gerontologist. 1998;38:25–36. doi: 10.1093/geront/38.1.25. [DOI] [PubMed] [Google Scholar]
- 7.Shah MN, Rathouz PJ, Chin MH. Emergency department utilization by noninstitutionalized elders. Acad Emerg Med. 2001;8:267–273. doi: 10.1111/j.1553-2712.2001.tb01303.x. [DOI] [PubMed] [Google Scholar]
- 8.Walter-Ginzburg A, Chetrit A, Medina C, et al. Physician visits, emergency room utilization, and overnight hospitalization in the old-old in Israel: The Cross-Sectional and Longitudinal Aging Study (CALAS) J Am Geriatr Soc. 2001;49:549–556. doi: 10.1046/j.1532-5415.2001.49112.x. [DOI] [PubMed] [Google Scholar]
- 9.Wolinsky FD, Liu L, Miller TR, et al. Emergency department utilization patterns among older adults. J Gerontol A Biol Sci Med Sci. 2008;63A:204–209. doi: 10.1093/gerona/63.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hastings SN, George LK, Fillenbaum GG, et al. Does lack of social support lead to more ED visits for older adults? Am J Emerg Med. 2008;26:454–461. doi: 10.1016/j.ajem.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 11.McCusker J, Karp I, Cardin S, et al. Determinants of emergency department visits by older adults: A systematic review. Acad Emerg Med. 2003;10:1362–1370. doi: 10.1111/j.1553-2712.2003.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 12.Lishner DM, Rosenblatt RA, Baldwin LM, et al. Emergency department use by the rural elderly. J Emerg Med. 2000;18:289–297. doi: 10.1016/s0736-4679(99)00217-6. [DOI] [PubMed] [Google Scholar]
- 13.Arcury TA, Gesler WM, Preisser JS, et al. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005;40:135–155. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 15.American Health Care Association. What is OSCAR data? American Health Care Association [on-line] Available at http://www.ahcancal.org/research_data/oscar_data/Pages/WhatisOSCARData.aspx Accessed August 26, 2013.
- 16.Hakenewerth AM, Waller AE, Ising AI, et al. North Carolina Disease Event Tracking and Epidemiologic Collection Tool (NC DETECT) and the National Hospital Ambulatory Medical Care Survey (NHAMCS): Comparison of emergency department data. Acad Emerg Med. 2009;16:261–269. doi: 10.1111/j.1553-2712.2008.00334.x. [DOI] [PubMed] [Google Scholar]
- 17.Getis A. A history of the concept of spatial autocorrelation: A geographer’s perspective. Geograph Analysis. 2008;40:297–309. [Google Scholar]
- 18.Anselin L, Syabri I, Kho Y. GeoDa: An introduction to spatial data analysis. Geograph Analysis. 2006;38:5–22. [Google Scholar]
- 19.Anselin L. Spatial Econometrics: Methods and Models. Dordrecht: Kluwer Academic Publishers; 1998. [Google Scholar]
- 20.Fotheringham AS, Brunsdon C, Charlton M. Geographic Weighted Regression: The Analysis of Spatially Varying Relationships. Chichester: Wiley; 2002. [Google Scholar]
- 21.Leung Y, Mei C, Zhang W. Statistical tests for spatial nonstationarity based on the geographically weighted regression model. Environ Plan A. 2000;32:9–32. [Google Scholar]
- 22.U.S. Census Bureau. State and County QuickFacts [on-line] Available at http://www.quickfacts.census.gov/qfd/states/37/3707720.html Accessed June 30, 2014.
- 23.LeSage J. Introduction to Spatial Econometrics. Boca Raton, FL: CRC Press; 2009. [Google Scholar]
- 24.Rasch EK, Gulley SP, Chan L. Use of emergency departments among working age adults with disabilities: A problem of access and service needs. Health Serv Res. 2013;48:1334–1358. doi: 10.1111/1475-6773.12025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weber EJ, Showstack JA, Hunt KA, et al. Are the uninsured responsible for the increase in emergency department visits in the United States? Ann Emerg Med. 2008;52:108–115. doi: 10.1016/j.annemergmed.2008.01.327. [DOI] [PubMed] [Google Scholar]
- 26.Smulowitz PB, Lipton R, Wharam JF, et al. Emergency department utilization after the implementation of Massachusetts health reform. Ann Emerg Med. 2011;58:225–234. doi: 10.1016/j.annemergmed.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 27.Block L, Ma S, Emerson M, et al. Does access to comprehensive outpatient care alter patterns of emergency department utilization among uninsured patients in East Baltimore? J Prim Care Community Health. 2013;4:143–147. doi: 10.1177/2150131913477116. [DOI] [PubMed] [Google Scholar]
- 28.Conti MS. Effect of Medicaid disease management programs on emergency admissions and inpatient costs. Health Serv Res. 2013;48:1359–1374. doi: 10.1111/1475-6773.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taubman SL, Allen HL, Wright BJ, et al. Medicaid increases emergency-department use: Evidence from Oregon’s health insurance experiment. Science. 2014;343:263–268. doi: 10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Platts-Mills TF, Glickman SW. Measuring the value of a senior emergency department: Making sense of health outcomes and health costs. Ann Emerg Med. 2014;63:525–527. doi: 10.1016/j.annemergmed.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larson DG, Tobin DR. End-of-life conversations: Evolving practice and theory. JAMA. 2000;284:1573–1578. doi: 10.1001/jama.284.12.1573. [DOI] [PubMed] [Google Scholar]
- 32.Ludwick A, Fu R, Warden C, et al. Distances to emergency department and to primary care provider’s office affect emergency department use in children. Acad Emerg Med. 2009;16:411–417. doi: 10.1111/j.1553-2712.2009.00395.x. [DOI] [PubMed] [Google Scholar]
- 33.D’Arcy LP, Stearns SC, Domino ME, et al. Is geriatric care associated with less emergency department use? J Am Geriatr Soc. 2013;61:4–11. doi: 10.1111/jgs.12039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Map of Emergency Department Visits Resulting in Discharge by Those Aged 65 Years or Older per 100 Residents Aged 65 Years or Older for Each ZIP Code (n = 716) in North Carolina in 2010.
Table S1. Multivariable Regression Results Describing the Relationship Between ZIP Code-Level Characteristics and the Number of Emergency Department (ED) Visits for Patients Aged 65 Years or Older Who Were Discharged Home per 100 Adult Residents Aged 65 Years or Older in North Carolina in 2010.


