Abstract
Thyroid hormones (TH) play an obligatory role in many fundamental processes underlying brain development and maturation. The developing embryo/fetus is dependent on maternal supply of TH. The fetal thyroid gland does not commence THs synthesis until mid gestation, and the adverse consequences of severe maternal TH deficiency on offspring neurodevelopment are well established. Recent evidence suggests that even more moderate forms of maternal thyroid dysfunction, particularly during early gestation, may have a long-lasting influence on child cognitive development and risk of neurodevelopmental disorders. Moreover, these observed alterations appear to be largely irreversible after birth. It is, therefore, important to gain a better understanding of the role of maternal thyroid dysfunction on offspring neurodevelopment in terms of the nature, magnitude, time-specificity, and context-specificity of its effects. With respect to the issue of context specificity, it is possible that maternal stress and stress-related biological processes during pregnancy may modulate maternal thyroid function. The possibility of an interaction between the thyroid and stress systems in the context of fetal brain development has, however, not been addressed to date.
We begin this review with a brief overview of TH biology during pregnancy and a summary of the literature on its effect on the developing brain. Next, we consider and discuss whether and how processes related to maternal stress and stress biology may interact with and modify the effects of maternal thyroid function on offspring brain development. We synthesize several research areas and identify important knowledge gaps that may warrant further study. The scientific and public health relevance of this review relates to achieving a better understanding of the timing, mechanisms and contexts of thyroid programming of brain development, with implications for early identification of risk, primary prevention and intervention.
Keywords: Fetal programming, pregnancy, thyroid hormones, HPT axis, brain development, stress
The importance of thyroid function for brain development and cognitive function has been appreciated for over a century (Curling, 1850, McCarrison, 1909) and is reflected in initiatives such as the World Health Organization (WHO)’s salt iodinization program and the newborn screening program for congenital hypothyroidism, which are now standard practices in many parts of the world. However, the WHO still considers iodine deficiency, which leads to hypothyroidism, the single most important preventable cause of brain damage worldwide (WHO/UNICEF/ICCIDD, 2007). The most vulnerable groups are pregnant and lactating women and their developing fetuses and neonates, given the crucial importance of iodine to ensure adequate levels of thyroid hormones (TH) for brain maturation. Iodine deficiency in pregnancy is a prevailing problem not only in developing countries, but also in western industrialized nations and other countries classified as free of iodine deficiency (Azizi et al., 2003, Travers et al., 2006, Leung et al., 2013). An explanation may be found in dietary changes. For example, processed foods in the U.S. are prepared with non-iodized salt, and consumption of these foods has increased (Council on Environmental Health et al., 2014). In addition, during pregnancy, iodine requirement is increased by 50-75%, due to a 30-50% increase in renal iodide clearance and trans-placental iodine transfer (Glinoer, 2007, McLeod and McIntyre, 2010). However, only 15-20% of pregnant women take iodide supplements (Council on Environmental Health et al., 2014), which may account for the finding that both in the U.S. and U.K. approximately one third of pregnant women are at least mildly iodine deficient according to WHO criteria (Caldwell et al., 2011, Bath et al., 2013). This circumstance is of prime importance because the fetus receives TH in part from the mother during gestation. There are several causes for insufficient TH availability during development, such as congenital hypothyroidism in the child, but the present review focuses on the impact of maternally-derived THs. During the embryonic and fetal periods of life the critical importance of THs of maternal origin becomes apparent in light of the consideration that while the effects of congenital hypothyroidism can be largely prevented by early postnatal TH substitution therapy, the effects of severe TH deficiency secondary to an inadequate supply from the mother, which include cognitive and motor defects, growth retardation, defects of hearing and speech and other defects, are irreversible after birth (this syndrome is known as neurological cretinism; de Escobar et al., 2004, Gilbert et al., 2012). Moreover, recent evidence additionally suggests that even more subtle forms of maternal thyroid dysfunction during pregnancy may impair her offspring’s cognitive and motor development (Zoeller, 2003, de Escobar et al., 2008, McLeod and McIntyre, 2010). In addition to iodine deficiency, maternal thyroid dysfunction can arise from autoimmune processes (e.g. Hashimoto Thyroiditis) or through environmental contaminants that function as endocrine disruptors (e.g. phtalates, BPA etc.) (Hartoft-Nielsen et al., 2011).
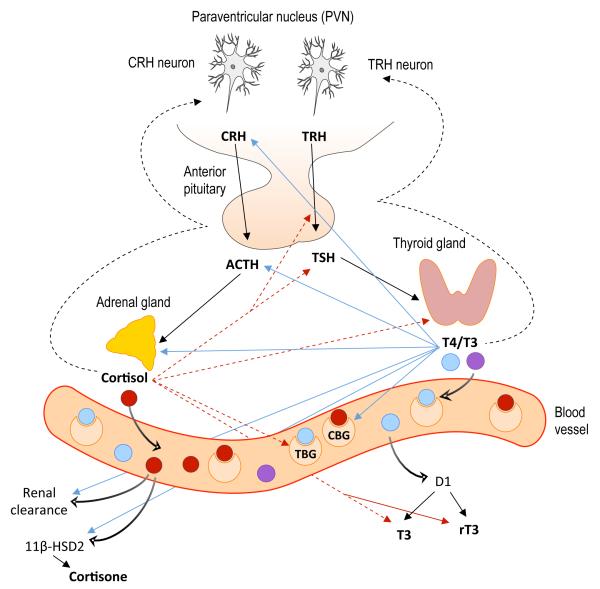
TH-regulated processes are highly evolutionary conserved, and THs and their metabolites are widely distributed in the animal and plant kingdoms. Metamorphosis in amphibians (i.e., the transition from an aquatic to a terrestrial environment) is regulated by TH, including lung maturation for air breathing. Similarly, in humans THs are involved in the maturation of various tissues and organs during transition to extrauterine life (Buchholz, 2015). Even in non-vertebrates that lack endogenous TH production, exogenous THs play a role in the initiation of metamorphosis. For example, in echinoderm larvae, THs from ingested algae act as a plasticity cue providing signals about the nutritional status of the environment (Heyland and Moroz, 2005). More generally, the hypothalamic-pituitary-thyroid (HPT) axis is a complex system that has widespread biological functions during as well as after development, with TH acting on almost every cell in the organism. The HPT axis plays a particularly important role in metabolism and energy expenditure (Kim, 2008, Klieverik et al., 2009) and also interacts with, regulates, and is counter-regulated by signals conveying information about substrate availability and energy demands such as those provided by the stress system, including the hypothalamic-pituitary-adrenal (HPA) axis. The thyroid and adrenal glands both communicate with the hypothalamus and the pituitary gland, and the hormones produced by these two axes closely regulate and counter-regulate one another. Thus, dysregulation of either axis is likely to result in an imbalance of the other. It is for this reason that maternal stress and stress-related biological processes during pregnancy may be important modulators of thyroid function, however, this interaction has been largely overlooked in the current literature on the influence of maternal TH on offspring brain development.
In this review, we first provide a short overview of the HPT axis, its development in the embryo/fetus, and its functional alterations that occur during gestation. We then review the existing literature on the influence of TH on brain and/or cognitive development in animals and humans. In the second part of the review we focus on suboptimal conditions during pregnancy that may alter or interact with maternal thyroid function, including maternal stress and maternal-placental-fetal stress biology.
1. The HPT axis
The HPT axis in humans and all other mammals is controlled centrally by neurons located within the parvocellular region of the paraventricular nucleus of the hypothalamus (PVN) that synthesize and release thyrotropin-releasing-hormone (TRH) into the median eminence. TRH stimulates thyroid-stimulating hormone (TSH) release from the anterior pituitary, which then travels through the peripheral vasculature to stimulate the release of THs from the thyroid gland. The thyroid gland predominantly produces and secretes the prohormone thyroxine (T4), which has low biological activity and functions as a reservoir in the circulation, and to a lesser extent the highly biologically active triiodothyronine (T3). Hereinafter, the term TH will be used when referring to both T4 and T3. The majority of the action of T3 is mediated via a nuclear receptor (thyroid hormone receptor, TR), that exists in four isoforms, two of which bind THs (TRα1 and TRβ2). TRs regulate transcription both in the absence and in the presence of ligand. Without the presence of T3, the unliganded receptor (aporeceptor) recruits corepressors and histone deacetylases, which retain the chromatin in a compact repressed position (Bernal, 2007). However, in the presence of T3, the binding of the hormone to TR initiates transcription by the release of corepressors and by recruiting coactivators and histone acetylases, which assist in the access of transcription apparatus to the promoter regions (Bernal, 2007, Cheng et al., 2010). It has been suggested that during brain maturation the aporeceptor represses specific gene expression until T3 becomes available to the cells in a time-specific manner (Patel et al., 2011). Circulating T3 and T4 are, for the most part, bound to binding proteins such as thyroxin binding globulin (TBG), transthyretin (TTR) or albumin; less than 1% are present in free (unbound) form. Different tissues modulate the impact of circulating THs according to their current needs via three iodothyronine deiodinases (D1, D2, and D3). D1 converts T4 to T3 by outer-ring deiodination and is, as such, responsible for a large fraction of the circulating T3. D1 also is important in iodine recycling from inactive iodothyronines, its preferred substrate being reverse T3 (rT3). D2 catalyzes only outer ring deiodination and is responsible for the local conversion of T4 to active T3 in different tissues including the brain. In fact, approximately 80% of brain T3 is produced locally in the CNS by D2 (Crantz et al., 1982). D3, which is expressed in particular in the brain and the organs of the feto-maternal interface, catalyzes only inner ring deiodination and mainly deactivates T3 and T4 to inactive iodothyronines, such as rT3, which is able to bind to TRs, thus blocking T3 action (Ahmed, 2015, Darras et al., 2015).
Another form of control over TH action is through selective TH uptake by the tissues. The transport of T4 and T3 in and out of cells is controlled by several classes of transmembrane TH-transporters (THTs), including members of the organic anion transporting peptides family (OATPs), L-amino acid transporters (LATs) and monocarboxylate transporters (MCTs) (Bernal, 2005, Visser et al., 2008). OATP-F is distributed widely in the human brain and is probably localized in the border of brain capillary endothelial cells and in the choroid plexus. It preferentially transports T4 and rT3, whereas T3 is less well transported (Pizzagalli et al., 2002). OATP-F may thus be involved in the transport of T4 through the blood-brain barrier by facilitating uptake of T4 by astrocytes (where T4 is converted to T3), as well as through the choroid plexus by facilitating uptake by tanycytes, and also in rT3 clearance (Bernal, 2005). Among the MCT family, monocarboxylate transporter 8 (MCT8) and MCT10 have been identified as specific TH transporters (Visser et al., 2008). MCT8 is expressed in neurons, which suggests that neuronal uptake of T3 produced in astrocytes is facilitated by this transporter (Heuer et al., 2005). In humans, mutation of this transporter is associated with severe developmental delay and neurological damage from an early age, together with an unusually altered pattern of thyroid hormone levels in blood, a syndrome known as Allan-Hernon-Dudley-Syndrome (Friesema et al., 2004, Kurian and Jungbluth, 2014).
1.1. Changes in THs during gestation – fetal compartment
The onset of thyroid function in the human fetus occurs around 16-20 weeks of gestation (de Escobar et al., 2004, Williams, 2008). However, even before onset of fetal thyroid function, significant levels of T3 and thyroid hormone receptors (TR) can be found in the fetal brain, and levels continue to increase over the course of gestation (Chan et al., 2002, Kester et al., 2004). Thus, active transport of maternal thyroid hormone across the placenta has to occur during this early period of gestation, and TH transporters have been identified in human placental tissue (Chan et al., 2006, Loubiere et al., 2012). Low levels of THs can already be detected in the coelomic fluid at 6 weeks gestational age, and they correlate with maternal levels. Although total levels in fetal fluids are more than 100-fold lower than TH concentrations in the maternal compartment, the unbound fraction is much higher in comparison and reaches levels that are biologically active in adults (Contempre et al., 1993, Calvo et al., 2002). Before the onset of fetal thyroid function in mid gestation, the fetus is completely dependent on maternal TH supply, but a significant transfer of TH from the mother to the fetus also persists during the second half of gestation (Vulsma et al., 1989). The fetal thyroid gland reaches full maturation only towards the end of gestation. In terms of quantity, T4 is the primary TH that gets transferred across the placenta (Calvo et al., 2002), and T4 enters the brain more readily than T3. In the developing brain, D2 and D3 activity (D1 is not present in the brain) and the ontogenic profile of iodothyronine concentrations show time- and region-specific variation (Kester et al., 2004), which suggests that these two enzymes play a role in ensuring the temporal and spatial availability of T3 to differentiating systems while preventing premature exposure to T3 in other systems that develop at a later time point (Dentice et al., 2013). Throughout gestation, T4 and free T4 (fT4) levels in the fetal circulation steadily increase and reach adult levels towards the beginning of the third trimester, whereas T3 and free T3 (fT3) levels remain low during fetal life and show a surge at term (Thorpe-Beeston et al., 1991). Placental D3 activity is highest in the beginning of pregnancy and declines over gestation, likely serving to prevent the fetus from excess TH. However, T4 (the hormone mainly transferred) has low biological activity, and its activation is regulated by and depends on the availability of D2 and D3 in specific tissues, thus preventing premature TH action. An alternative or additional function of placental D3 may be to provide the fetal thyroid with iodine recycled from the metabolism of iodothyronines (Moleti et al., 2014). The fetal thyroid develops the ability to accumulate iodine by 10-12 wks gestation (Burrow et al., 1994). To conclude, maternal T4 levels in early pregnancy appear to be particularly important in the provisioning of the fetal cortex with THs and continue to be relevant throughout gestation.
1.2. Changes in THs during gestation – maternal compartment
Gestational hormonal and metabolic changes induce profound adaptations in maternal HPT physiology. In the first trimester, high levels of human chorionic gonadotropin (hCG) are secreted by the syncytiotrophoblast cells of the blastocyst, which signals the corpus luteum to continue progesterone production, which, in turn, is essential for the maintenance of pregnancy. hCG is structurally similar to TSH and also has thyrotropic effects, leading to a surge in first trimester fT4 and fT3 and a concurrent suppression of circulating TSH. It has been suggested that through this mechanism of regulation of the maternal endocrine system the embryo/fetus ensures adequate levels of substrate for its own development during a time at which the fetal thyroid gland still lacks the capability of synthesizing THs (Glinoer, 1997, Moleti et al., 2014). Rising estrogen concentrations during pregnancy induce increased hepatic synthesis and enhanced sialylation of TBG, which decreases its metabolic clearance rate. This results in a two-fold increase in TBG and increased total T4 and T3 levels throughout pregnancy (accompanied by an enlargement of the maternal thyroid gland by an average of 18%), whereas for most of gestation the free T4 and T3 concentrations remain normal or decline slightly (Braunstein, 2011). In addition, there is a demand on the maternal thyroid through degradation of iodothyronines by D3 in the placenta. To summarize, in order to maintain adequate levels of free T4 and T3, maternal TH production increases by approximately 50% during pregnancy. Pregnant women also have an increased need for iodine for three main reasons: a) increased synthesis of THs by the maternal thyroid gland, b) increased renal clearance of iodide, and c) transfer of iodine to the fetus across the placenta. Interestingly, hCG also stimulates iodine transfer across the placenta from the maternal to the fetal compartment by stimulating the sodium-iodide symporter (NIS) (Arturi et al., 2002). Overall, the additional dose of iodine intake required in pregnancy by to provide an adequate supply for both the mother and her fetus is estimated to be 150 μg/day (Moleti et al., 2014). Insufficient iodine intake leads to a switch towards an increased thyroidal production of T3 and a reduction of T4 production in order to save iodine. This may lead to low levels of T4 and fT4, while TSH concentrations are maintained within the normal range due to the persisting negative feedback of T3. This adaptation may be beneficial to the mother, however, since T4 is the primary TH that crosses the placenta, maternal TH supply to the fetus may be compromised (Moleti et al., 2014).
2. Influence of THs on brain and cognitive development
The brain is an important target of thyroid hormones at all stages of life, however, the maximal vulnerability to an imbalance of thyroid hormone supply occurs during the earliest stages of brain development. The following section reviews the importance of thyroid hormones for brain development and cognitive capabilities. The majority of human studies have been observational in nature, focusing on relatively broad cognitive outcome measures, whereas the mechanisms and molecular underpinnings of the behavioral changes have largely been studied in rodent models. Before focusing on the thyroid hormone availability-related alterations in cortical developmental processes, a short overview is provided below of normal embryonic and fetal brain development.
2.1. Prenatal brain development
The development of the mammalian central nervous system follows a protracted and highly orchestrated chain of events. Understanding the timing of neurodevelopmental events is essential for determining how environmental disturbances during specific developmental time windows can affect certain structures and functions.
Within the first three weeks after human oocyte fertilization three germ layers are formed in the embryo – the ectoderm, mesoderm and endoderm. The brain and spinal cord arise from an area of the ectoderm known as the neural plate. During the formation of these germ layers, a subset of cells that form the upper layer (the later ectoderm), receive signals from migrating cells, which induce their differentiation into neural progenitor cells. First, the progenitor cells divide in a symmetric fashion to produce more neural progenitor cells. Then, in the sixth week of development, the cells begin to divide asymmetrically to produce two different types of cells - another neural progenitor cell, and a neuron. The new neural progenitor cells continue to divide within the ventricular zone. The neurons, however, begin a process of migration that results in the anatomical development of the cortex, which primarily occurs during the fetal period (9 weeks until birth) (Stiles and Jernigan, 2010).
The early fetal period is characterized by ongoing neuronal proliferation and migration, which leads to the “inside-out” formation of the neocortex into its 6-layered structure. The first post-mitotic cells that migrate from the ventricular zone form the preplate. Towards the end of the embryonic period, the cortical plate develops within the preplate, thereby dividing the preplate into a minor superficial component, the marginal zone containing Cajal-Retzius neurons that secrete the extracellular protein Reelin (which is required for normal inside-to-outside positioning of the migrating neurons), and a large deep component, the subplate. The subplate is assumed to be a key structure in enabling higher inter-cortical connectivity because its size and duration of existence during development increases along with the complexity of the brain and is largest in primates, particularly humans (Luhmann et al., 2009, Kanold and Luhmann, 2010). The first cells to arrive in the cortical plate form the future layer VI. Later-born cells migrate past the already-present cortical cells (dependent on Reelin signaling) and form progressively more superficial layers. Towards the end of the second trimester the six layers of the neocortex are discernible, however, the final form is reached around developmental week 35, with the disappearing of the subplate (Kriegstein and Noctor, 2004, ten Donkelaar and van der Vliet, 2006).
After migrating to their final destination, neurons extend axons and dendrites to make synaptic connections within the developing brain. Outgrowing axons are able to make use of the scaffold formed by earlier axons, so-called pioneers, giving rise to axon fascicles that form the neural circuitry (Robichaux and Cowan, 2014). Synaptogenesis accelerates in the third trimester to approximately 40,000 synapses per minute (Bourgeois, 1997), and around mid-gestation the process of myelination of the axons begins, allowing for more efficient cell-to-cell communication (Abraham et al., 2010). These processes play a critical role in the functional maturation of developing neural circuits and extend well into the postnatal period.
It is important to note that brain change and adaptation are part of a lifelong process. No other organ system remains as plastic and continues to develop over such a prolonged period, but the earliest phases of maturation are particularly important. The concept of fetal programming describes the process by which conditions during critical periods of cellular proliferation, differentiation, and maturation elicit structural and functional changes in cells, tissues, and organ systems that may, independently or through interactions with subsequent developmental conditions, have long-term or permanent consequences. One of the principles of this concept is that organs undergoing rapid developmental changes are especially vulnerable to the influences of environmental conditions, which applies particularly to the brain. First, the embryonic/fetal period is the developmental stage when differentiation of major brain structures occurs in a relatively short amount of time, thereby conferring a greater susceptibility for exposure to environmental perturbations, such as alterations in TH supply. Second, because brain development entails a cascade of bidirectional interactions with the environment, even small or subtle alterations in brain structure or function during fetal life can become progressively and substantially magnified over time to produce long-lasting or permanent deficits. It is, therefore, conceivable that insufficient TH supply during fetal development can have long-term consequences for brain anatomy, connectivity and function.
2.2. Influence of TH deficiency on brain development – evidence from animal studies
A wealth of studies primarily in rodents has characterized the neuroanatomical and functional consequences of thyroid dysfunction during early development. The majority of these studies have focused on the effects of experimentally-induced hypothyroidism via thyroidectomy, administration of an antithyroid drug (methimazole (MMI) or propylthiouracil (PTU)) to pregnant dams throughout gestation and/or lactation, or, alternatively, with the use of genetic models of TH insufficiency, such as TH receptor deletion and mutation. These different methods of inducing TH deficiency during development in animal models are summarized using the term “developmental hypothyroidism.” In general, these methods cause drastic reductions in the levels of circulating T3 and T4, with a corresponding increase in TSH release from the pituitary (a hormone profile consistent with hypothyroidism in humans, see Box 1). Other models have examined the effects of low-dose TH synthesis inhibitor (e.g. PTU) administration, leading to dose-dependent moderate reductions in serum THs, mainly T4 (similar to hypothyroxinemia in humans, see Box 1) (e.g. Gilbert and Sui, 2006, Goodman and Gilbert, 2007). Evidence from this research suggests widespread effects of THs on neuron proliferation, neuronal migration and differentiation, neurite outgrowth and guidance, synaptogenesis and myelination (e.g. Berbel et al., 1994, Hashimoto et al., 2001, Pathak et al., 2011, Mohan et al., 2012, Shimokawa et al., 2014). A comparatively smaller number of studies have investigated the specific effect of maternal thyroid dysfunction by inducing only a transient and often moderate reduction in the maternal thyroid hormone supply before the onset of fetal thyroid function (e.g. Dowling and Zoeller, 2000, Auso et al., 2004, Opazo et al., 2008). These studies provide important evidence for the significance of even mild disruptions in the maternal TH supply for prenatal brain development.
Box 1: Definitions and prevalence of maternal thyroid dysfunction.
Hypothyroxinemia (1.5 – 25%)
Serum fT4 level in the lower 5th or 10th percentile of the reference range with normal TSH concentrations
Overt hypothyroidism (OH, 0.3 – 0.5%)
Elevated serum TSH level in conjunction with a decreased fT4 concentration
Subclinical hypothyroidism (SCH, 2 – 2.5%)
Elevated serum TSH levels with normal fT4 concentrations
Thyroid autoimmunity (10 – 20%)
Presence of TPO- and/or TG-antibodies in the serum, with or without changes in TSH and fT4 concentrations
It is important to note that alterations in the expression of genes directly or indirectly regulated by TH appear to be completely reversible by postnatal TH replacement (Alvarez-Dolado et al., 1998, Alvarez-Dolado et al., 1999, Gilbert et al., 2007, Jahagirdar et al., 2012). However, more substantial alterations in brain developmental trajectories such as migration defects (Auso et al., 2004, Goodman and Gilbert, 2007, Pathak et al., 2011), neuronal morphological alterations (Ruiz-Marcos et al., 1982, Rami et al., 1986) or impaired motor coordination and activity (Shimokawa et al., 2014) seem to require TH replacement starting very soon after the induction of experimental hypothyroidism in order for the effects to be abolished.
2.2.1. Neuron proliferation
The time window for rodent neocortical neurogenesis is from embryonic day (E)12 to 18, which is completed before the start of fetal thyroid function at E17.5. Several genes involved in cell cycle regulation and cell proliferation are found to be regulated by TH in the developing brain (Dowling et al., 2000, Bansal et al., 2005, Morte et al., 2010, Qiu et al., 2010, Wang et al., 2014). In addition, neural progenitors in the VZ of rats express TRα1, Mct8 transporters and deiodinase II, and maternal thyroid hormone deficiency leads to a delay in symmetrical divisions of these progenitors, as well as a reduced cell cycle length and a corresponding reduction of the progenitor pool (Mohan et al., 2012). Interestingly, the evolutionary enlargement of the human cerebral cortex (which is mainly due to an expansion of the surface area, whereas the increase in cortical thickness is relatively modest) is suggested to be the result of an enlarged progenitor pool. According to the radial unit hypothesis, an increase in symmetrical divisions of the neural progenitor cells before the onset of neurogenesis (i.e. a prolongation in duration of the cell cycle) would result in an exponential increase in the number of founder cells that give rise to a larger number of radial cortical columns, which, in turn, results in an expanded laminar structure (Rakic, 2009). In addition, the expansion of a second set of progenitor cells, called basal or intermediate progenitors (which have also been implied in the evolutionary expansion of the neocortex) seems to require TH binding to the extracellular matrix protein integrin αvβ3, a T4 cell surface receptor (Stenzel et al., 2014). Consequently, maternal thyroid hormone deficiency has also been shown to impair the basal or intermediate progenitor pool, which, in turn, leads to a selective loss of upper layer neurons and reduced cortical thickness (Mohan et al., 2012). In a somewhat contradictory finding, Chen et al. (2012) identify maternal thyroid hormones as critical factor for the switch from proliferation to differentiation of embryonic stem cells, i.e. terminating proliferation and promoting differentiation, thereby contributing to the neurogenesis in the telencephalon during early brain development. These discrepancies may be a result of timing-dependent differences of TH signaling in the developing brain (Quignodon et al., 2004).
2.2.2. Neuron migration
Another well-replicated observation in the offspring of hypothyroid rats is related to deficits in neuronal migration in the cerebellum and cerebrum. Heterotopias (i.e. cellular malformations with clusters of neurons in untypical places, a result of defective migration) in the white matter of the corpus callosum and subcortical band heterotopias can be detected in offspring of dams with moderate forms of thyroid disruption (Berbel et al., 2001, Goodman and Gilbert, 2007, Gilbert et al., 2014), and they remain present in adult animals even after returning to an euthyroid state (Powell, 2012). Developmental hypothyroidism has been shown to produce a decrease of neurons in cortical layers I-III and an increase in layers V-VI, thereby resulting in a reduction of radial glial density and loss of neuronal bipolarity, which is crucial for neurons to migrate in radial direction to form the cortical plate (Pathak et al., 2011). Delayed neuronal migration has also been observed in animals exposed to only a transient maternal TH deficiency before the onset of fetal thyroid function (Auso et al., 2004). An increased susceptibility to seizures appears to be a common byproduct of the observed migratory defects (Auso et al., 2004, Gilbert et al., 2014). Thus, TH seems to affect the process of neuronal migration via multiple sites of possible regulation. Most importantly, T3 directly regulates the expression of reelin during development (Alvarez-Dolado et al., 1999, Pathak et al., 2011). Under TH deficiency, reelin and its cell surface receptors apolipoprotein E receptor 2 (ApoER2) and very low--density lipoprotein receptor (VLDLR) are significantly reduced in the neocortex (Pathak et al., 2011). Similarly, in the cerebellum, the expression of reelin and doublecortin (another important factor in neuronal migration) is downregulated in perinatally iodine-deficient and hypothyroid rats (Wang et al., 2012). Reelin is a critical factor in the control of neuronal positioning, and its lack can be studied in the reeler mouse mutant (Rakic and Caviness Jr, 1995).
2.2.3. Neuron differentiation
In addition to cell migration, thyroid hormones regulate the differentiation of neurons, oligodendrocytes, astrocytes and microglia. Developmental hypothyroidism causes decreased expression of the neurotrophin brain-derived neurotrophic factor (BDNF) and neurotrophic factor-3 (NT-3) (Lindholm et al., 1993, Koibuchi et al., 1999), insulin-like growth factor-I (IGF-I) (Elder et al., 2000), actin-related protein 2/3 complex subunit 5 (ARPC5), and collapsin response mediator protein-2B (CRMP2B) (Liu et al., 2013), as well as the presynaptic plasma membrane protein synaptosomal associated protein of 25 kDa (SNAP-25) (Zhang et al., 2008), all of which are important regulators of neuronal differentiation, neurite outgrowth and synaptogenesis. In contrast, the expression of several genes involved in cell adhesion, including tenascin-C, L1/Ng-CAM, TAG-1 and neural cell adhesion molecule (NCAM) appears to be upregulated by a lack of TH in the developing brain in a region- and time-specific fashion (Iglesias et al., 1996, Alvarez-Dolado et al., 1998, Alvarez-Dolado et al., 2000, Alvarez-Dolado et al., 2001). These molecules are implicated in neuronal migration as well as neurite outgrowth, axonal guidance and fasciculation. Indeed, L1/Ng-CAM overexpression has been associated with an altered pattern of fasciculation (Kunz et al., 1998).
The effects of TH on gene expression are paralleled by morphologic alterations, with some classes of neurons being more strongly affected by hypothyroidism. For example, poor dendritic arborization, altered distribution of dendritic spines, and fewer synaptic connections can be observed in the pyramidal cells of the neocortex and hippocampus (Ruiz-Marcos et al., 1982, Rami et al., 1986) and in the Purkinje cells of the cerebellum (Hashimoto et al., 2001, Shimokawa et al., 2014).
2.2.4. Myelination
The differentiation of oligodendrocytes, the glial cells that perform myelination of the axons in the central nervous systems, is strongly TH-dependent (Rodriguez-Pena, 1999). TH deficiency leads to delayed myelination and decreased expression of major myelin proteins myelin basic protein (MBP), proteolipid protein (PLP), myelin-associated glycoprotein (MAG), 2′,3′-cyclic nucleotide 3′-phosphodiesterase (CNP) (Rodriguez-Pena et al., 1993, Ibarrola and Rodriguez-Pena, 1997). The expression of the MBP gene is directly regulated by T3 via a TRE in the promoter region (Farsetti et al., 1992). These alterations affect the maturation of interhemispheric connections, which is reflected in a substantial decrease in the number of myelinated axons in the anterior commissure and the corpus callosum in developmentally hypothyroid rats, while the total number of axons is not affected (Berbel et al., 1994, Ferraz et al., 1994). A reduction in white matter volume and percent white matter has been observed in developmentally hypothyroid rats, and these changes largely persist even after the animal is returned to an euthyroid state (Powell, 2012).
2.2.5. Interneurons and neural circuits
Another population of neurons that is strongly affected by TH deficiency is γ-aminobutyric acid (GABA)-ergic interneurons in the neocortex, hippocampus and cerebellum. GABA is the primary inhibitory neurotransmitter in the mature CNS, regulating excitatory glutamatergic activity, but during the early stages of development it mainly acts as an excitatory neurotransmitter and as a trophic factor involved in developmental processes, including cell proliferation, migration, and synaptogenesis. In addition, GABAergic interneurons are responsible for the generation of the first primitive patterns of network activity (Ben-Ari, 2002, Ben-Ari et al., 2007). In particular, a subpopulation of parvalbumin (PV)-containing GABAergic neurons and their axonal and dendritic processes is reduced in the hippocampus and neocortex of developmentally hypothyroid rats and TRα1-deficient or -mutant mice (Berbel et al., 1996, Guadano-Ferraz et al., 2003, Gilbert et al., 2007, Wallis et al., 2008, Sawano et al., 2013). This effect persists into adulthood and can be elicited even with more moderate degrees of TH insufficiency (Gilbert et al., 2007). PV-positive cells consist of basket and chandelier cells mainly located in the pyramidal cell layer that form dense clusters around pyramidal cells and contribute to fast-spiking, perisomatic (i.e. they synapse directly on the soma) input onto pyramidal cells. A reduction in the expression of the Ca2+-binding protein PV and a impaired development of axonal and dendritic arborization may affect the firing properties of the cells and decrease the inhibitory control of glutamatergic neurons. Indeed, functional deficits of the GABA-mediated inhibition (i.e. disinhibition) in the dentate gyrus (DG) have been demonstrated to accompany these alterations (Gilbert et al., 2007, Wallis et al., 2008). Transient maternal TH deficiency also alters tangential migration of neurons derived from the medial ganglionic eminence, which includes PV-positive GABAergic interneurons (Cuevas et al., 2005). In addition to PV, TH targets both pre- and postsynaptic components of the GABAergic system in the developing hippocampus. Developmental hypothyroidism leads to a 50% reduction of glutamic acid decarboxylase 65 (GAD65), the enzyme responsible for converting glutamate to GABA, along with a 37% reduction in GAD65-positive cells and processes (Sawano et al., 2013). The rise in K+/Cl− cotransporter (KCC2) protein, a postsynaptic component essential for the switching of GABAergic neurotransmission from excitatory to inhibitory (Ben-Ari, 2002), between postnatal day (P)10 and 15 is absent in hypothyroid animals, suggesting a significant delay in the timing of the switch (Sawano et al., 2013). TH deficiency also decreases the proliferation and delays the maturation of the precursors of cerebellar GABAergic interneurons, with effects on the number of mature GABAergic neurons and GABAergic terminals (Manzano et al., 2007). Conversely, treatment of neuronal cultures from E16 embryonic rats with T3 results in functional maturation of early cortical networks with higher spontaneous burst activity, increased growth of glutamatergic and GABAergic synapses, an increase in the relative density of GABAergic neurons, as well as increased somatic and axonal growth of large GABAergic interneurons, due to neurothrophic actions of T3 and T3-mediated increases in neuronal activity (Westerholz et al., 2010). The effects of TH on PV-expressing GABAergic interneurons may be partly mediated by their effect on neurotrophin expression. Neurotrophins have been implicated in regulating survival, differentiation, and maturation of GABAergic interneurons, as well as their mature inhibitory function (Woo and Lu, 2006).
Tangentially migrating GABAergic neurons also form a subpopulation of subplate neurons, a transient structure in the developing brain with an important role in the guidance of ingrowing thalamocortical axons and the maturation of intra- and extracortical circuits (Hoerder-Suabedissen and Molnar, 2015). Subplate abnormalities have been shown in rats with maternal hypothyroidism with likely effects on cortical connectivity (Jahagirdar et al., 2012, Navarro et al., 2014). Supporting the role of TH for these processes, developmental hypothyroidism has been associated with a substantial reduction in thalamocortical axonal arborization, potentially due to an asynchrony in the maturation of thalamocortical afferents and their cortical targets (Ausó et al., 2001, Berbel et al., 2014).
2.2.6. Synaptic plasticity
THs play an important role in synaptic plasticity and long-term potentiation (LTP). Developmental hypothyroidism or iodine-deficiency decreases the expression of neurogranin/RC3, a calmodulin-binding protein which is abundant in the hippocampal regions CA1, CA3 and DG throughout development and which plays a crucial role in regulating the post-synaptic availability of calmodulin and the subsequent activation of calmodulin-dependent pathways, including Ca2+/calmodulin-dependent protein kinase II (CaMKII) (Dowling and Zoeller, 2000, Dong et al., 2010). Adult rats that were TH-deficient during development exhibit impairments in synaptic transmission and LTP in the DG and CA1 region, even after relatively moderate disruptions of thyroid function (Gilbert and Paczkowski, 2003, Gilbert and Sui, 2006, Opazo et al., 2008, Wang et al., 2013).
2.2.7. Neurochemistry
TH may also alter the biochemistry of the brain. Widespread decreases in monoamines (norepinephrine, epinephrine, dopamine and serotonin) and acetylcholinesterase, as well as increases in GABA, have been documented in the cerebrum, cerebellum and medulla oblongata of developmentally hypothyroid rats (Ahmed et al., 2010).
Taken together, these studies converge to suggest that a lack of THs during prenatal and early postnatal development can result in significantly altered cortical cytoarchitecture, delayed cortical maturation, and abnormal intra- and extracortical structural and functional connectivity.
2.3. Functional consequences of TH deficiency – evidence from animal studies
The described neuroanatomical alterations may well explain the behavioral changes and cognitive dysfunctions observed in animals exposed to developmental hypothyroidism.
2.3.1. Motor function and activity
Congenitally hypothyroid mutant rdw rats show severe impairment of motor coordination and balance, a probable result of morphological alterations in the cerebellum, as well as a general hypoactivity (Shimokawa et al., 2014). Preweaning hypoactivity and impaired neuromotor competence have also been observed in offspring of dams with experimentally-induced hypothyroidism, but the hypoactivity may transition into motor hyperactivity after termination of antithyroid drug treatment (Goldey et al., 1995, Brosvic et al., 2002, Darbra et al., 2003, Axelstad et al., 2008). Thus, the observed hypoactivity may be a direct result of a low TH level, which promotes energy conservation without long-term alterations in brain function. In contrast, the increase in locomotor activity observed after weaning may be the result of a permanently altered dopamine signaling (Beninger, 1983).
2.3.2. Cognition
Changes in the monoaminergic system may also affect attentional processes, which, in turn, could impair cognitive performance at several levels. For example, developmental hypothyroidism has been shown to disrupt signal detection performance via impairment of visual attention (Hasegawa and Wada, 2013). A shorter attention span may also be the underlying cause of the poor performance of rats exposed to developmental hypothyroidism in active and passive avoidance learning (Darbra et al., 2003, Negishi et al., 2005). In addition, the adaption to a change in response requirement (which is tested using a reversal learning paradigm) appears to be affected in developmentally hypothyroid rats and persists long after returning to an euthyroid (normal thyroid function) state (Brosvic et al., 2002, Gilbert and Sui, 2006).
Alternatively, impaired learning may be the result of long-term deficits in memory consolidation. For example, the effects of developmental TH-deficiency on synaptic plasticity and LTP may explain the impaired spatial learning in the Morris water maze observed in adult rats after recovery of their TH-concentrations. Effects have been reported even in animals with a more subtle TH disruption during development; while most eventually managed to acquire the task, it took these animals significantly longer time to do so (Gilbert and Sui, 2006, Opazo et al., 2008). Early postnatal T4 treatment (P7) did improve learning and memory performance, while late postnatal T4 treatment (P21) failed to show an effect (Reid et al., 2007), supporting the critical role of TH during certain developmental time windows.
2.3.3. Affect
Developmentally hypothyroid rats seem to experience less anxiety to novelty, which may contribute to the impaired avoidance learning observed in these animals (Darbra et al., 2003, Negishi et al., 2005). In contrast, congenitally hypothyroid mutant rdw rats show increased anxiety and depression in response to novel surroundings, likely a result of a reduction in monoamines (Shimokawa et al., 2014). Again, these differences could be due to the current thyroid status in these animals. While rdw rats are permanently hypothyroid, rats exposed to developmental hypothyroidism are usually euthyroid at the time of testing.
2.4. Influence of TH deficiency on neurodevelopment – evidence from human studies
Human studies on the neurodevelopmental consequences of TH deficiency are typically based on various indicators of maternal thyroid dysfunction. Box 1 provides definitions and prevalence rates during pregnancy of the different forms of thyroid dysfunction that are associated with TH deficiency. The true prevalence of isolated maternal hypothyroxinemia is difficult to determine because wide differences exist between studies and regions. Hypothyroxinemia affects more women in mildly to moderately iodine deficient regions, where the prevalence may increase over the course of gestation (Moleti et al., 2011). Only a small proportion (7%) of women with hypothyroxinemia are thyroid autoantibody positive, whereas thyroid autoantibodies have been detected in approximately half of women with subclinical hypothyroidism (SCH) and 80% of women with overt hypothyroidism (OH) (Moleti et al., 2011, Stagnaro-Green et al., 2011). In addition, thyroid autoantibodies are detectable in 10-20% of euthyroid women. These women are more likely to develop increased TSH concentrations over the course of pregnancy as well as postpartum thyroiditis (Stagnaro-Green et al., 2011).
We first provide here an overview of cognitive changes and motor development in the children of mothers with TH deficiency. Next, we review the available child imaging data on changes in brain morphology, and finally we summarize observations on child psychopathological conditions.
2.4.1. Cognition and motor development
Support in humans for an influence of prenatal maternal thyroid dysfunction on child behavior, motor and cognitive ability comes from a wide range of primarily observational studies, summarized in Table 1. Findings suggest that different forms of moderate or mild maternal thyroid dysfunction are associated with a range of child neurodevelopmental outcomes, including intelligence or general cognition, verbal development, reaction time, and motor performance. In addition, the timing during gestation of exposure to maternal TH deficiency seems to be an important modulator of these effects. In particular, maternal hypothyroxinemia (i.e. fT4 concentrations below the normal limits with normal TSH concentrations) appears to have a larger effect when it is present during early pregnancy. All but one of the studies (i.e., Grau et al., 2015) that investigated the effect of low maternal fT4 levels around the end of the first trimester (12/13 weeks gestational age (i.e., before onset of fetal thyroid function) report impaired cognitive and motor functioning in exposed children (Pop et al., 1999, Pop et al., 2003, Kooistra et al., 2006, Henrichs et al., 2010, Costeira et al., 2011, Finken et al., 2013, Julvez et al., 2013, Ghassabian et al., 2014a). In contrast, studies examining maternal hypothyroxinemia in mid- or late pregnancy reveal mixed results. A study comparing 99 hypothyroxinemic women in the second trimester with 99 matched euthyroid controls did not observe an effect on the children’s scores of the Bayley Scales of Infant Development at 2 years of age (Craig et al., 2012). This association was, however, observed in children of women with first trimester hypothyroxinemia (Pop et al., 2003, Costeira et al., 2011). In these studies, fT4 concentrations later in pregnancy were not independently associated with child cognitive outcomes, however, in one study the lowest developmental scores were observed in the children of mothers whose fT4 levels were low in the first trimester and decreased further over pregnancy (Pop et al., 2003). Four other studies report no associations between low fT4 levels in the second or third trimester and cognitive or motor functioning in children of different ages (Pop et al., 1999, Kooistra et al., 2006, Chevrier et al., 2011, Grau et al., 2015). However, a study in a small sample (Vermiglio et al., 2004) did find a positive correlation between maternal fT4 levels in mid-pregnancy and IQ scores in the offspring, and another study (Suarez-Rodriguez et al. 2012) measured fT4 levels at term (37 weeks GA) and observed a mean difference of 6.1 points on the general cognitive index of the McCarthy Scales between children of hypothyroxinemic mothers and control children. A recent meta-analysis (that did not distinguish effects between different assessment time points) concluded that low maternal fT4 concentrations are associated with an approximately three-fold increased risk of delayed child cognitive development (Wang et al., 2015).
Table 1.
Observational studies investigating the effect of maternal thyroid dysfunction during pregnancy on child neurocognitive and psychomotor outcomes.
| First author (year) |
Design and Subjects |
Thyroid Function | Neurobehavioral Outcome | Results | ||||
|---|---|---|---|---|---|---|---|---|
| Biomarkers | Dysfunction | GA at assessment |
Test | Age at assessment |
||||
|
Maternal
hypothyroxinemia |
Craig (2012) | Longitudinal; N = 198 mother- child pairs |
TSH, fT4 | fT4 < 3rd percentile and TSH < 3.5 mU/l (n = 99) |
2nd trimester | Bayley Scales of Infant Development (MDI and PDI) |
2 years | Children of hypothyroxinemic mothers did not have significantly lower scores on any of the Bayley subscales. |
| Finken (2013) | Longitudinal; N = 1765 mother-child pairs (ABCD cohort) |
TSH, fT4 | fT4 < 10th percentile (n = 175) |
Median (range) = 90 (83 - 100) days (12.9 weeks GA) |
Amsterdam Neuropsychological Tasks (ANT) |
Mean (SD) = 5.7 (0.5) |
Maternal hypothyroxinemia was associated with reduced performance in the baseline speed reaction time task (41.3 ms slower) but not in other tasks; children exposed to maternal hypothyroidism, i.e. fT4 < 10th percentile and TSH > 90th percentile (n = 44) had a 71.3 ms slower response speed. |
|
| Ghassabian (2014a) | Longitudinal; N = 3727 mother-child pairs (Generation R cohort) |
TSH, fT4, TPO-Ab |
fT4 < 5th percentile and TSH < 2.5 mU/L (n = 129) |
Mean (SD) = 13.5 (2.0) weeks GA |
SON-R 2 ½ - 7 (non- verbal intelligence) |
Mean (SD) = 6.2 (0.5) years |
Children of mothers with hypothyroxinemia had an IQ 4.3 points lower than controls. |
|
| Henrichs (2010) | Longitudinal; N = 3659 mother-child pairs (Generation R cohort) |
TSH, fT4 | fT4 < 10th percentile and TSH < 1 SD above the gestational age- specific mean (mild hypothyroxi- nemia, n = 311)/ fT4 < 5th percentile and TSH < 1 SD above the gestational age- specific mean (severe hypothyroxinemia, n = 157) |
Mean (SD) = 13.3 (1.7) weeks GA |
MCDI (verbal development); LDS (verbal development); PARCA (nonverbal cognitive development) |
18 months (MCDI) and 30 months (LDS, PARCA) |
Both mild and severe maternal hypothyroxinemia were associated with a higher risk of expressive language delay across all ages (OR 1.4 and 1.8 respectively); severe hypothyroxinemia was also associated with a higher risk of nonverbal cognitive delay (OR 2.0); continuous fT4 levels were negatively associated with language delay at 30 months. |
|
| Julvez (2012) | Longitudinal; N = 1761 mother-child pairs |
TSH, fT4 | fT4 < 10th percentile/ fT4 < 5th percentile/ fT4 < 2.5th percentile |
Median (range) = 13 (8 – 20) weeks GA |
Bayley Scales of Infant Development (MDI and PDI) |
Median (range) 14 (11 – 23) months |
Children of mothers with fT4 < 5th percentile had significantly lower MDI scores (3.4 points); self- reported pre-pregnancy thyroid disorder without medical treatment was also associated with lower MDI scores (5.5 points). |
|
| Kooistra (2006) | Longitudinal; N = 204 mother- child pairs |
TSH, fT4 | fT4 < 10th percentile at 12 weeks GA, TSH not elevated (n = 108) |
12, 24 and 32 weeks GA |
Neonatal Behavioral Assessment Scale |
3 weeks | Infants of women with hypothyroxinemia at 12 weeks gestation had significantly lower scores on the orientation index compared with controls but not on other subscales; maternal TSH and fT4 later in pregnancy were not significant predictors of newborn performance. |
|
| Pop (1999) | Longitudinal; N = 220 mother- child pairs |
TSH, fT4, TPO-Ab |
fT4 < 10th percentile at 12 weeks/ fT4 < 5th percentile |
12 and 32 weeks GA |
Bayley Scales of Infant Development (MDI and PDI) |
10 months | Children of women with fT4 < 5th and fT4 < 10th percentile had significantly lower PDI scores (14.1 and 7.4 points respectively); levels at 32 weeks were not associated with MDI or PDI; continuous fT4 was positively correlated with PDI scores. |
|
| Pop (2003) | Longitudinal; N = 125 mother- child pairs |
TSH, fT4 | fT4 < 10th percentile and TSH < 2 mU/l at 12 weeks GA (n = 63) |
12, 24 and 32 weeks GA |
Bayley Scales of Infant Development (MDI and PDI) |
1 and 2 years | Children of hypothyroxinemic women at 12 weeks GA had significantly lower PDI and MDI scores at both 1 and 2 years of age (all between 8 and 10 points lower); children of mothers whose fT4 levels decreased further over pregnancy had the lowest scores; continuous fT4 levels at 12 weeks GA were positively associated with PDI and MDI scores. |
|
| Suarez-Rodriguez (2012) | Longitudinal; N = 70 mother- child pairs |
TSH, fT4 | fT4 < 10th percentile and TSH < 5 mU/l (n = 37) |
37 weeks GA | McCarthy Scales of Children’s Abilities |
38 – 60 months | Children of hypothyroxinemic mothers had a significantly lower score on the general cognitive index (6.1 points) and on perceptual-manipulative and memory subscales. |
|
|
Maternal
hypothyroidism (subclinical or overt) |
Haddow (1999) | Longitudinal; N = 186 mother- child pairs |
TSH, T4, fT4, TPO-Ab |
TSH > 98th percentile, partly treated (n = 62) |
2nd trimester | WISC; Test of Language Development; PIAT-R (reading recognition and comprehension); Conners’ Continuous Performance Test (sustained vigilance, attention); Developmental Test of Visual-Motor Integration (visual perception, fine motor skills); grooved pegboard test (visual–motor coordination) |
7 – 9 years | Children from hypothyroid mothers performed less well on all tests, but only Conners’ Continuous Performance Test and the word discrimination subscale of the Test of Language Development reached significance; children from mothers whose hypothyroidism was untreated showed significantly lower performance on most tests, specifically their mean IQ score on the WISC was 7 points lower, and 19 % had an IQ score of 85 or lower as compared to 5% of the control children. |
| Klein (2001) | Longitudinal; N = 172 mother- child pairs |
TSH, T4, fT4, TPO-Ab |
TSH ≥ 99.85th percentile (group 3, n = 20), and TSH >98th and <99.85th percentile (group 2, n = 28) |
Mean = 17 weeks GA |
WISC | Mean (SD) = 8 (0.5) years |
Children from mothers with the highest TSH concentrations had significantly lower IQ scores than controls (mean (SD) 107 (13) vs. 97 (14)) and a significantly higher incidence of IQs of 1 SD or more below the control mean (adjusted OR 4.7); children of mothers with TSH >98th and < 99.85th percentile had intermediate scores but did not differ significantly from the other two groups; continuous measures of TSH showed a significant negative association with IQ score. |
|
| Murcia (2011) | Longitudinal; N = 691 mother- child pairs |
TSH, urinary iodine |
TSH > 4 mU/l (n = 24) |
Mean (SD) = 12.4 (0.66) weeks GA |
Bayley Scales of Infant Development (MDI and PDI) |
11 – 16 months | Children of mothers with TSH > 4 mU/l had an increased risk of a PDI score < 85 (OR 3.5) but not MDI. |
|
|
Maternal thyroid
autoimmunity |
Pop (1995) | Longitudinal; N = 230 mother- child pairs |
TSH, fT4, fT3, TPO-Ab |
TPO-Ab > 100 U/ml but euthyroid |
32 weeks GA | McCarthy Scales of Children’s Abilities |
Mean (SD) = 4.8 (0.3) years |
Children of euthyroid women with elevated TPO-Ab titers had significantly lower scores on four of the six subscales, in particular on the general cognitive index (10.5 points). |
|
Maternal iodine
deficiency |
Bath (2013) | Longitudinal; N = 1040 mother-child pairs (ALSPAC cohort) |
Urinary iodine |
Urinary iodine < 150 μg/l (n = 646) |
Median (range) = 10 (9 – 12) weeks GA |
WISC (abbreviated), Neale Analysis of Reading Ability |
8 years (WISC) and 9 years (Neale) |
Children of mothers with low iodine levels had a significantly higher risk for suboptimum cognitive outcomes (i.e. scores in the bottom quartile) on the subscales verbal IQ, reading accuracy, and reading comprehension; mean total IQ was also significantly lower in these children (3.4 points). |
| Ghassabian (2014b) | Longitudinal; N = 1525 mother-child pairs (Generation R cohort) |
Urinary iodine |
Urinary iodine < 150 μg/g cre- atinine (n = 188) |
Mean (SD) = 13.28 (1.85) weeks GA, range 6.07– 17.93 weeks |
SON-R 2 ½ - 7 (non- verbal intelligence), receptive subtest of the Taaltest voor Kinderen (language comprehension) |
Mean (SD) = 6.0 (0.3) years |
After adjustment for possible confounders, there was no relation between maternal low UIC and children’s non-verbal IQ or language comprehension. |
|
|
Multiple or
undefined thyroid dysfunction |
Chevrier (2011) | Longitudinal; N = 287 mother- child pairs |
TSH, T4, fT4 | - | Mean (SD) = 26.9 (3.4) weeks GA |
Bayley Scales of Infant Development (MDI and PDI), PLS, WPPSI, McCarthy Scales of Children’s Abilities, Woodcock- Johnson Test of Cognitive Ability, WRAVMA, KCPT, PPVT |
6 (Bayley, PLS), 12 (Bayley, PLS), 24 (Bayley), and 60 months (WPPSI, McCarthy, Woodcock- Johnson, WRAVMA, KCPT, PPVT) |
Maternal T4 and fT4 levels were not significantly associated with any child outcome; Increasing maternal TSH was related to better performance on the MDI and on the auditory comprehension subscale of the PLS at 12 months. |
| Costeira (2011) | Longitudinal; N = 86 mother- child pairs from a mildly iodine- deficient area |
TSH, T4, fT4, T3, fT3, urinary iodine |
TSH > 90th percentile/ T4, fT4, T3, or fT3 < 10th percentile/ urinary iodine <50 μg/l |
12, 24 and 32 weeks gestation |
Bayley Scales of Infant Development (MDI and PDI) |
12, 18 and 24 months |
Low urinary iodine concentrations in the first and third trimester were associated with lower MDI scores at (18 and) 24 months and lower PDI scores at 18 months; fT4 < 10th percentile in the first trimester was associated with lower PDI scores at 18 and 24 months and with an increased OR of 2.1 for having a child mildly or significantly delayed (PDI < 84). |
|
| Grau (2015) | Longitudinal; N = 455 mother- child pairs (N = 289 at follow- up) |
TSH, fT4, fT3, TPO-Ab, urinary iodine |
fT4 < 10th percentile and TSH < 5 mU/l (subgroup 1, n = 47) / fT4 > 10th percentile, urinary iodine < 150 μg/l or TPO-Ab positive (subgroup 2, n = 369) |
End of first and end of second trimester |
Brunet-Lezine scale; WISC |
Mean (SD) = 1.08 (0.03) years (Brunet-Lezine) and 7.3 (0.25) years (WISC) |
Maternal hypothyroxinemia and continuous fT4 was not associated with scores on the Brunet-Lezine scale or the WISC. |
|
| Li (2010) | Longitudinal; N = 213 mother- child pairs |
TSH, T4, fT4, TPO-Ab |
TSH > 97.5th percentile, T4 and fT4 normal, TPO- Ab negative (subclinical hypothyroidism, n = 18) / T4 < 2.5th percentile, TSH and fT4 normal, TPO-Ab negative (hypothyroxinemia , n = 19) / TPO-Ab > 50 U/ml, TSH, T4 and fT4 normal (elevated TPO-Ab, n = 34) |
16 – 20 weeks GA |
Bayley Scales of Infant Development (MDI and PDI) |
25 – 30 months | Children of women from all three case groups had significantly lower scores on the MDI (8.9 – 10.5 points) and the PDI (7.5 – 10 points); the three risk factors (increased TSH, decreased T4, elevated TPO-Ab) were independently associated with lower intellectual and motor development. |
|
| Oken (2009) | Longitudinal; N = 500 mother- child pairs |
TSH, T4, TPO-Ab |
TSH > 2.5 mU/l / TPO-Ab > 2 U/ml |
Mean 10.2 weeks GA |
VRM, PPVT, WRAVMA |
6 months (VRM) and 3 years (PPVT, WRAVMA) |
Maternal thyroid function was not associated with child cognitive test scores. |
|
| Pharoah (1984) | Longitudinal; N = 20 mother-child pairs from a severly iodine- deficient area |
T4, T3 | - | Any time during index pregnancy |
PDCT, Pegboard, peg transfer, bead threading |
Mean (range) = 11.3 (10.3 – 11.9) years |
Maternal T4 was positively associated with test scores on PDCT and the three motor performance tasks (but not T3). |
|
| Vermiglio (2004) | Longitudinal; N = 27 motherchild pairs (n = 16 from a moderately iodine-deficient area A and n = 11 from an iodine-sufficient area B) |
TSH, fT4, T4, fT3, T3, TBG, T4/TBG ratio |
- | 5-10 weeks GA, 11-14 weeks GA, and 18-20 weeks GA |
WISC | 8-10 years | The children’s IQ score was positively related to maternal FT4 (r = .56) and inversely related to maternal TSH values (r = −.63) at midgestation, when both area A and B were combined. |
|
| Williams (2012) | Longitudinal; N = 143 mothers and their N = 166 children born preterm |
TSH, T4, fT4, TPO-Ab, Tg- Ab |
- | At delivery | McCarthy Scales of Children’s Abilities |
5.5 years | Each mU/l increment of maternal TSH level at delivery was associated with significant decrements in the general cognitive index (3.2 points) and the verbal and perceptual performance subscales; each pmol/l decrease in fT4 was associated with significant increments in the general cognitive index (1.5 points), quantitative subscale and motor scale; maternal T4 levels were not associated with the McCarthy Scales. |
|
Abbreviations. KCPT = Conner’s Kiddie Continuous Performance Test; LDS = Language Development Survey; MCDI = MacArthur Communicative Development Inventory; MDI = Mental Development Index; PARCA = Parent Report of Children’s Abilities; PDCT = Pacific Design Construction Test; PDI = Psychomotor Development Index; PIAT-R = Peabody Individual Achievement Test, revised; PLS = Preschool Language Scale; PPVT = Peabody Picture Vocabulary Test; SON-R 2 ½ - 7 = Snijders-Oomen Niet-verbale intelligentie test, revisie; VRM = Visual Recognition Memory Test; WISC = Wechsler Intelligence Scale for Children; WPPSI = Wechsler Preschool and Primary Scale of Intelligence; WRAVMA = Wide Range Assessment of Visual Motor Ability
Results on the consequences of maternal total T4 on child cognitive development are mixed. In a study from China, children of women with T4 concentrations < 2.5th percentile in the early second trimester had significantly lower scores on both the mental developmental index (MDI) and the psychomotor developmental index (PDI) of the Bayley Scales of Infant Development in early childhood compared to children whose mothers had normal T4 concentrations during pregnancy (Li et al., 2010). Likewise, a study in a relatively small sample of mother-child dyads from a severely iodine-deficient region in Papua New Guinea found maternal prenatal T4 levels to be positively associated with test scores on cognitive and motor performance tasks (Pharoah et al., 1984). In contrast, two other studies found no association between low T4 levels in early pregnancy (Oken et al., 2009) or at delivery (Williams et al., 2012) and child cognitive functioning. It is likely that total T4 levels in the maternal circulation do not adequately reflect the supply with TH to the fetus because the vast majority of circulating T4 is bound to carrier proteins. An assessment of fT4 seems to be preferable in order to estimate the effect of a low maternal TH status on child neurodevelopment.
To date, research in humans has not focused strongly on the effects of maternal hypothyroidism (defined as elevated TSH levels with (overt) or without (subclinical) a corresponding decrease in circulation fT4 levels). In fact, the majority of studies investigating maternal hypothyroxinemia, use elevated TSH concentrations as an exclusion criterion in accordance with the definition of isolated hypothyroxinemia. Based on the rather sparse evidence, increased TSH levels usually appear to be associated with poorer child cognitive outcome irrespective of the assessment time point (Haddow et al., 1999, Klein et al., 2001, Vermiglio et al., 2004, Li et al., 2010, Murcia et al., 2011, Williams et al., 2012, Finken et al., 2013), although one study observed better cognitive performance with increasing maternal TSH (Chevrier et al., 2011). The effect in this latter study is likely driven by very low rather than high TSH levels, because only approximately 5% of the women had TSH concentrations > 2.5 mU/l and none had TSH > 5.2 mU/l, whereas 15% of women had TSH levels < 0.8 mU/l (Chevrier et al., 2011). Thus, high concentrations of maternal TSH at any point during pregnancy appear to negatively impact child neurodevelopment.
Other maternal conditions that are associated with TH deficiency such as iodine deficiency and thyroid autoimmunity have also been related to poorer child cognitive outcomes (Pop et al., 1995, Bath et al., 2013). Ghassabian et al. (2014b) did not find a clear relationship between low maternal urinary iodine levels in early pregnancy and child cognitive outcomes, which may be due to the low prevalence of even mild iodine deficiency in the study population.
There have been only a few interventional studies examining the effects of maternal iodine supplementation on infant neurocognitive function (reviewed in Taylor et al., 2014), and only one randomized control trial (RCT) comparing children of hypothyroid or hypothyroxinemic mothers that received L-thyroxine supplementation during pregnancy with children of mothers with thyroid dysfunction that did not receive a treatment (Lazarus et al., 2012). All of the studies investigating iodine supplementation were conducted in Spain, which is considered to have adequate iodine status in the general population, although some areas are mildly iodine-deficient (Lazarus, 2014). Velasco et al. (2009) report that children of euthyroid mothers supplemented with 300 μg of iodine from the first trimester and throughout lactation showed better behavioral and psychomotor performance than children of untreated mothers. Likewise, Berbel et al. (Berbel et al., 2009) observed a higher developmental quotient in children whose mothers received iodine supplementation from the beginning of pregnancy (group 1) compared to children of women receiving treatment from the beginning of the 2nd trimester (group 2) or the end of gestation through lactation (group 3). However, these effects could as likely be the result of maternal hypothyroxinemia as that of iodine supplementation, because group 1 included only women with fT4 > 20th percentile whereas groups 2 and 3 included mildly hypothyroxinemic women (thus the results could have been due to their lower fT4 levels instead of their delayed substitution with iodine). The single RCT did not find an association between maternal iodine supplementation and child neurocognitive development (Santiago et al., 2013). Likewise, Lazarus et al. (2012) did not observe a benefit of maternal treatment of thyroid dysfunction with 150 μg of L-thyroxine (L-T4) per day on child IQ at age 3 years. The study was criticized for having started treatment too late in pregnancy to potentially exert a positive effect on infant neurocognitive development (median 13 weeks 3 days gestational age) and to have used only a very global measure of cognitive function, namely IQ (Brent, 2012). As of now, the evidence provided by the few existing clinical intervention trials is insufficient to make any clear inferences of the putative benefits of iodine of T4 supplementation during pregnancy to women with milder forms of thyroid dysfunction.
Based on the evidence reviewed above, it seems reasonable to generally conclude there is an association of maternal thyroid dysfunction with suboptimal child neurodevelopmental outcomes, however it is important to note there is considerable heterogeneity across studies. These studies differ with respect to the study populations; some studies have subjects from iodine-deficient regions (Pharoah et al., 1984, Costeira et al., 2011), one study only includes children born preterm (Williams et al., 2012) and there also are large differences in ethnicity across studies, which is a source of variability of TH levels (Aoki et al., 2007, Korevaar et al., 2013). In addition, the criteria used to define hypothyroidism or hypothyroxinemia differ widely across studies. For example, Craig et al. (2012) define maternal hypothyroxinemia as fT4 concentrations < 3rd percentile and TSH levels < 3.5 mU/l, whereas in the study by Pop et al. (2003) hypothyroxinemia was defined as fT4 levels < 10th percentile and TSH < 2.0 mU/l, and the Suarez-Rodriguez et al. (2012) study considered TSH concentrations < 5.0 mU/l as normal. Thus, the same subjects may be classified as subclinically or overtly hypothyroid, hypothyroxinemic or normal depending on the respective cut-offs used across studies. Another major contributor to the heterogeneity is the timing of the assessment in not only maternal thyroid function in pregnancy but also age of assessment of child neurodevelopmental outcomes (the latter ranging between 3 weeks (Kooistra et al., 2006) and 9 or 10 years of age (Haddow et al., 1999, Vermiglio et al., 2004) with only a few having longitudinal follow-up assessments at later ages (Pop et al., 2003, Oken et al., 2009, Henrichs et al., 2010, Chevrier et al., 2011, Costeira et al., 2011, Grau et al., 2015)). These differences across studies make it very difficult to disentangle the differential effects of the pre- and postnatal environment on the developing brain. Having a baseline neurodevelopmental assessment at or shortly after birth and several follow-up assessments over infancy, childhood and potentially longer would be the optimal way to differentiate the impact of maternal thyroid dysfunction during pregnancy from postnatal factors such as postnatal iodine deficiency, child thyroid function, and effects of other postnatal exposures. On the other hand, alterations in neurocognitive and psychomotor functioning may not be observable in newborns, either because differences may be only modest at birth but may become larger over time and thus only become apparent in later childhood, or because the underpinnings of cognitive function cannot be reliably measured in newborns. It is important to appreciate that the absence of overt behavioral abnormalities at birth does not imply the absence of underlying brain structural or functional abnormalities. For example, an examination of post-mortem brains from a 30 week old fetus as well as a child with a mutation in the MCT8 transporter (which leads to TH deficiency selectively in the brain) showed that brain damage is already present during the fetal period, while behavioral alterations may become apparent only at later stages of life (Lopez-Espindola et al., 2014).
2.4.2. Brain Morphology
Obvious limitations preclude the study of the developing human brain at a cellular or molecular level. However, rapid advances over the last two decades in imaging techniques now afford the opportunity in human fetuses, newborns, infants and children to characterize many aspects of structural and function brain maturation and development. As yet, such research is lacking on the association of maternal thyroid dysfunction in pregnancy on newborn and infant brain structure. A recent study by Samadi et al. (2015) found morphological alterations in the corpus callosum of 9-12 year old children born to mothers who were hypothyroid prior to or during pregnancy and did not receive the recommended L-T4 dose increase in pregnancy (Stagnaro-Green et al., 2011). In the same cohort, two studies by Willoughby et al. (Willoughby et al., 2014a, b) reported smaller left and right hippocampal volumes in children of mothers diagnosed with hypothyroidism, which, in turn, were associated with deficits in memory function. However, Ghassabian et al. (2014a) did not observe an association between maternal hypothyroxinemia in early pregnancy and global brain measures including brain volume, cortical thickness, and surface area in 8 year old children. Clearly, more imaging studies are needed, and preferably longitudinal studies with a baseline assessment in newborns, to elucidate the specific effects of maternal thyroid dysfunction on child neurodevelopment. Of particular importance are imaging studies investigating the effect of maternal thyroid function on structural and functional network development, because THs seem to have a critical impact on early circuit formation and myelination, and the maturation of the white matter is assumed to be the underlying factor of the emerging cognitive capabilities during development (Nagy et al., 2004).
2.4.3. Psychopathology
Maternal thyroid dysfunction during pregnancy has been linked to an increased risk for neurodevelopmental disorders in the offspring, particularly, autism spectrum disorders (ASD) and attention-deficit hyperactivity disorder (ADHD) (see Table 2). Increased maternal TSH levels, maternal hypothyroxinemia, elevated titers of TPO-antibodies, and mild iodine deficiency have been associated with child ADHD diagnosis or symptoms such as impaired executive functions (Vermiglio et al., 2004, Ghassabian et al., 2011, Ghassabian et al., 2012, van Mil et al., 2012, Pakkila et al., 2014, Modesto et al., 2015). Interestingly, a human mutation in the thyroid receptor-β (TRβ) gene that underlies the “resistance to thyroid hormone” (RTH) syndrome also is closely associated with ADHD (Hauser et al., 1993). Transgenic mice expressing a human mutant TRβ display all the defining symptoms of ADHD, including inattention, hyperactivity, and impulsivity (Siesser et al., 2006) – behavior that also is exhibited in rodents exposed to perinatal hypothyroidism, as discussed earlier (Darbra et al., 2003, Negishi et al., 2005). It is possible that these observed associations are a consequence of the long-lasting changes in the dopaminergic and/or noradrenergic system produced by an early deficiency of TH (Ahmed et al., 2010).
Table 2.
Observational studies investigating the effect of maternal thyroid dysfunction during pregnancy on child psychopathology.
| First author (year) |
Design and Subjects |
Thyroid Function | Psychopathology | Results | ||||
|---|---|---|---|---|---|---|---|---|
| Biomarkers | Dysfunction | GA at assessment |
Assessment | Age at assessment |
||||
|
Maternal
hypothyroidism (subclinical or overt) |
Andersen (2014b) | Retrospective; N = 542 100, all live-born singletons born between 1980 and 1990 in Denmark |
- | Hospitaldiagnosed or treated hypothyroidism before 1996 (N = 3979) (information obtained from DNHR and DNPR) |
- | Prescription of anxiolytics, antipsychotics, and antidepressants at least twice (information obtained from DNPR) |
15- 31 years | Maternal hypothyroidism was associated with an increased risk of prescription of anxiolytics and antipsychotics (adjusted hazard ratio (aHR) 1.23 and 1.22 respectively). |
| Päkkilä (2014) | Longitudinal; N = 5131 mother child-pairs (Northern Finland Birth Cohort 1986) |
TSH, fT4, TPO-Ab |
TSH > 3.1 mU/l (first trimester) or TSH > 3.5 mU/l |
Mean (SD) = 10.7 (2.8) weeks GA |
Rutter B2 scale (teacher-rated); combined ADHD symptoms defined as total Rutter B2 scores of ≥9 and 3 or more points from ADHD questions |
8 years | In general, there were no significant differences in the odds of ADHD symptoms in children born to mothers with high and normal serum TSH, but girls had a 1.4-fold odds of combined ADHD symptoms with every natural log increase in maternal TSH. |
|
|
Maternal
hypothyroxinemia |
Modesto (2015) | Longitudinal; N = 3873 mother-child pairs (Generation R cohort) |
TSH, fT4, TPO-Ab |
fT4 < 5th percentile and TSH < 2.5 mU/l (n = 127) |
Mean (SD) = 13.6 (1.9) weeks GA |
CPRS-R:S | Mean (SD) = 8.1 (0.2) years |
Children of hypothyroxinemic women had higher scores on the ADHD index (7% increase) but not on the Oppositional scale compared to nonexposed children. |
| Roman (2013) | Longitudinal; N = 4039 mother-child pairs (Generation R cohort) |
TSH, fT4, TPO-Ab |
fT4 < 10th percentile and TSH < 2.5 mU/l (n =295)/ fT4 < 5th percentile and TSH < 2.5 mU/l (n = 136) |
Mean (SD) = 13. 4 (1.9) weeks GA |
PDP subscale of the CBCL 1½ -5, SRS; probable autism defined by a PDP score > 98th per- centile and SRS score in the top 5% of the sample (n = 81) |
6 years | Severe maternal hypothyroxinemia (fT4 < 5th percentile) was associated with an increased risk of having a probable autistic child (adjusted Odds Ratio (aOR) = 3.89) and with higher scores on the PDP and SRS |
|
| Vermiglio (2004) | Longitudinal; N = 27 mother- child pairs (n = 16 from a moderately iodine-deficient area A and n = 11 from an iodine-sufficient area B) |
TSH, fT4, T4, fT3, T3, TBG, T4/TBG ratio |
fT4 < 2.5th percentile and TSH < 4 mU/l |
5-10 weeks GA, 11-14 weeks GA, and 18-20 weeks GA |
ADHD (diagnosis based on DSM-IV) |
18-36 months and 8-10 years |
Maternal hypothyroxinemia occurred in eight (50%) of the women from area A and only transiently in one woman from area B; seven of the eight hypothyroxinemic mothers from area A had children diagnosed with ADHD; 11 of the 16 children from area A were diagnosed with ADHD whereas none from area B were affected. |
|
|
Maternal thyroid
autoimmunity |
Ghassabian (2012) | Longitudinal; N = 3139 mother-child pairs (Generation R cohort) |
TSH, fT4, TPO-Ab |
TPO-Ab > 100 mU/l (n = 147) |
Mean (SD) = 13.5 (1.8) weeks GA |
CBCL 1½ -5 | Mean (SD) = 34 (1) months |
Elevated titers of TPOAbs in mothers were associated with externalizing problems in children (OR = 1.64), in particular with ADHD problems (OR = 1.77); maternal TSH was also associated with children’s externalizing problems (B = 0.18 per SD of TSH). |
|
Maternal iodine
deficiency |
Van Mil (2012) | Longitudinal; N = 1156 mother-child pairs (Generation R cohort) |
Urinary iodine |
Iodine:creatinine ratio < 10th percentile (48.6– 136.1 mg/g creatinine, n = 117) |
Median (range) = 13.2 (10.2 – 17.6) weeks GA |
BRIEF-P | 4 years | Low maternal urinary iodine was associated with deficits in inhibition, working memory and global executive functioning in the children. |
|
Multiple or
undefined thyroid dysfunction |
Andersen (2014a) | Retrospective; N = 857 014, all live-born singletons born between 1991 and 2004 in Denmark |
- | Hospital- diagnosed or treated hypothyroidism (N = 18 011) (information obtained from DNHR and DNPR) |
- | Diagnosis of ADHD or ASD (information obtained from DNHR and DPCR) |
3 years onwards | Maternal hypothyroidism diagnosed and treated after the birth of the child increased the risk of ASD (aHR 1.34); paternal thyroid dysfunction was not associated with an increased risk for any of these disorders. |
| Ghassabian (2011) | Longitudinal; N = 3736 mother-child pairs (Generation R cohort) |
TSH, fT4, T4 | - | Mean (SD) = 13.3 (1.7) weeks GA |
CBCL 1½ -5 | 1 ½ and 3 years | Maternal TSH levels were positively associated with combined externalizing scores at 1 ½ and 3 years (B = 0.22 per SD of TSH), particularly on attention deficit/hyperactivity (B = 0.08 per SD of TSH) and oppositional defiant subscales (B = 0.08 per SD of TSH); T4 and fT4 were not associated with an increased risk for behavioral problems. |
|
| Yau (2014) | Retrospective; N = 272 children born in Orange County, CA between 2000 and 2001 |
TSH | - | 15-19 weeks GA |
Diagnosis of ASD (n = 78, information obtained from medical records) or developmental delay (n = 45, defined as Mullen Scales of Early Learning and Vineland Adaptive Behavior Scales composite score <70) |
3 – 4 years | Maternal mid-pregnancy TSH levels were inversely associated with ASD risk in the child (aOR = 0.33) as well as risk of developmental delay (aOR = 0.09). |
|
Abbreviations. ADHD = Attention Deficit/ Hyperactivity Disorder, ASD = Autism Spectrum Disorders, BRIEF-P = Behavior Rating Inventory of Executive Function for Preschoolers, CBCL 1 ½ -5 = Child Behavior Checklist for Toddlers, CPRS-R:S = Conners’ Parent Rating Scale– Revised Short Form, DNHR = Danish National Hospital Register, DNPR = Danish National Prescription Registry, DPCR = Danish Psychiatric Central Register, DSM-IV = Diagnostic and Statistical Manual of Mental Disorders- Version IV, PDP = Pervasive Developmental Problems, SRS = Social Responsiveness Scale.
Maternal hypothyroidism and maternal hypothyroxinemia also have been related to development of ASD in their children (Roman et al., 2013, Andersen et al., 2014a). One study, however, reported an inverse association between mid-pregnancy TSH and ASD risk (Yau et al., 2015). The relationship between thyroid dysfunction and ASD may underlie alterations in the GABAergic systems, which is strongly influenced by prenatal THs and which has been implicated as a pathophysiological mechanism in ASD (Coghlan et al., 2012). Interestingly, neonates with low levels of BDNF are at increased risk of developing ASD later in life (Abdallah et al., 2013). BDNF regulates the maturation and function of GABAergic interneurons (Woo and Lu, 2006), and is itself regulated by TH (Koibuchi et al., 1999). BDNF also up-regulates KCC2 expression during development (Aguado et al., 2003), which controls the excitatory-inhibitory shift of GABAergic transmission (Sawano et al., 2013). A defect in this switch has been observed in two different animal models of autism (Tyzio et al., 2014).
The GABAergic system is also assumed to play a role in the etiology of schizophrenia (Gonzalez-Burgos et al., 2010). To date there are no studies on the association of maternal thyroid function during pregnancy and offspring schizophrenia risk, however, Andersen et al. (2014b) reported an increased risk for prescription of anxiolytics and antipsychotics in children of prenatally hypothyroid mothers.
2.4.4. Summary of human research
Maternal thyroid function during pregnancy is robustly associated with child neurodevelopment, as reflected by impaired cognitive and psychomotor functioning and increased risk for neurodevelopmental disorders such as ADHD and ASD. Preliminary evidence also suggests an influence of maternal TH deficiency on brain morphology (one limitation of these studies is that brain morphology was characterized in late childhood rather than at or soon after birth). The nature and size of the effect may depend, in part, on the timing of TH insufficiency. Low fT4 concentrations during early gestation may have the largest adverse effects, whereas the effects of high TSH levels do not seem to vary as a function of stage of gestation. The underlying mechanism of these differential effects are not clear and may possibly involve different etiological pathways. It also is likely that the autoimmune processes that produce common forms of hypothyroidism (OH and SCH; as indicated by the high titers of thyroid autoantibodies) may exert additional effects on pregnancy and fetal neurodevelopment over and beyond those of maternal thyroid dysfunction (Pop et al., 1995, Thangaratinam et al., 2011, Ghassabian et al., 2012). Isolated hypothyroxinemia, on the other hand, appears to be caused primarily by mildly or moderately insufficient iodine intake, which, as intrathyroidal iodine stores are progressively depleted over gestation (due to the increased demands from mother and fetus), may result in increased thyroidal T3 production at the expense of T4. T3 exerts sufficient negative feedback to the anterior pituitary to maintain TSH in the normal range, while at the same time fT4 levels decrease (Moleti et al., 2011). This decrease may be most harmful before the onset of fetal thyroid function.
We note that TH levels in maternal plasma do not provide a direct indicator of fetal TH status. While maternal and fetal circulating TH levels are correlated (Shields et al., 2011, Velasco et al., 2013), the relationship is likely influenced by fetal characteristics including genetic variants implicated in TH synthesis, action, transport and regulation (Medici et al., 2015). Additional studies are warranted to improve our understanding of the relationship between maternal and fetal thyroid function.
There are several knowledge gaps and questions that need to be addressed by future studies. These include the determination of the specific cognitive functions and the specific underlying changes in brain structure and function in children exposed to maternal thyroid dysfunction during gestation. A special focus should be placed on elucidating the impact of maternal hyperthyroidism, in order to make an informed decision about the advisability of L-T4 substitution therapy in cases of milder maternal TH deficiency (Andersen et al., 2014a, Yau et al., 2015).
Another important knowledge gap relates to the paucity of information about the interaction of the HPT axis with other endocrine systems and environmental conditions. The next part of this review addresses the effects of various gestational states and conditions that may interact with the maternal HPT axis and moderate the association of maternal thyroid dysfunction with child neurodevelopment.
3. Gestational states and conditions that may alter or interact with maternal thyroid function
The association of gestational states and conditions related to maternal stress and stress biology during pregnancy with child neurodevelopment is well established (Buss et al., 2004, O'Donnell et al., 2009, Buss et al., 2011, Buss et al., 2012b). Most studies of prenatal stress and brain development have focused on mechanisms primarily related to the hypothalamus-pituitary-adrenal (HPA) axis (Buss et al., 2012a). We propose here that it may be important to also consider the HPT axis when examining the effects of prenatal stress on fetal development for the following three reasons: (1) the HPT system itself is stress-sensitive; (2) the HPA and the HPT axes interact at multiple levels to regulate and counter-regulate one another; and (3) THs may program the regulation of the HPA axis during early development.
Accordingly, the following sections summarize the effects of stress on the HPT axis, describe HPAHPT interactions (see also Figure 1) after as well as during development, and discuss the relevance of these issues in the specific context of pregnancy and fetal brain development.
Figure 1.
Interactive relationship between hormones of the hypothalamic-pituitary-thyroid axis (HPT) and the hypothalamic-pituitary-adrenal (HPA) axis.
Depicted are the HPT and HPA axes and the regulatory circuits within the respective systems, as well as the effect of alterations on the level of the adrenal (red arrows) on HPT function and the thyroid (blue arrows) on HPA function. Solid lines represent positive associations, and dashed lines represent negative associations. Increased levels of cortisol have an inhibitory effect on the release of TSH from the pituitary and THs (T4 and T3) from the thyroid, as well as on the synthesis of the carrier protein TBG. Cortisol also promotes a switch within D1 activity towards a preferential inactivation of T4 into rT3, instead of an activation of T4 into T3. Increased availability of THs is associated with a general activation of the HPA axis on all levels and increased levels of the carrier protein CBG. However, THs also promote renal clearance and the metabolism of cortisol into its inactive form cortisone.
Abbreviations. 11β-HSD2 = 11β-hydroxysteroid dehydrogenase 2; ACTH = adrenocorticotropic hormone; CBG = cortisol-binding globulin; CRH = corticotropin-releasing hormone; D1 = deiodinase 1; rT3 = reverse T3; T3 = triiodothyronine; T4 = thyroxine; TBG = thyroxine-binding globulin; TRH = thyrotropin-releasing hormone; TSH = thyroid-stimulating hormone.
3.1. Stress
3.1.1. Acute Stress
The HPT axis is a stress-responsive system. Most research suggests that in rodents, circulating peripheral TH concentrations decrease in response to severe, uncontrollable stressors such as restraint stress or inescapable foot- or tailshocks (Langer et al., 1983, Bianco et al., 1987, Servatius et al., 2000, Helmreich et al., 2005, Helmreich et al., 2006, Helmreich and Tylee, 2011). These changes are likely due to a reduced secretion of these hormones by the thyroid gland (Helmreich and Tylee, 2011), but low T3 levels may also be the result of decreased activity of D1 in liver and kidney (Bianco et al., 1987). In contrast, T3 levels may be higher in the brain after stress (Baumgartner et al., 1998, Friedman et al., 1999), which may be due to an increase in D2 activity or increased expression of the TH-transporter transthyretin in the cerebro-spinal fluid (CSF) in response to acute stress (Baumgartner et al., 1998, Martinho et al., 2012). Instead of showing a compensatory increase, TSH and TRH appear to be decreased as well, which suggests a central downregulation (Bianco et al., 1987, Cizza et al., 1996, Helmreich and Tylee, 2011). Functionally, a stress-induced decrease in thyroid function may reflect a conservation of energy and resources by peripheral tissues in an unpredictable or threatening environment.
3.1.2. Chronic stress and depression
Chronic stress has been associated in most studies with decreased TH levels in mice (Cremaschi et al., 2000, Silberman et al., 2002). One study, however, found that in response to chronic mild stress TH levels were, instead, increased or unchanged, depending on the rat strain (Kioukia et al., 2000). It appears that a chronic central down-regulation of HPT activity may occur only in a subgroup of animals that have a greater sensitivity to stressful stimuli, perhaps due to a genetic predisposition, and that only these animals also exhibit accompanying behavioral or psychological changes (Kilburn-Watt et al., 2010). In human refugees, severe chronic psychological stress has been related to a general dampening of HPT activity, with reduced concentrations of TSH, T4, fT4, T3 and rT3 (Bauer et al., 1994). All of these subjects had been diagnosed with some form of psychological disease, most frequently affective disorders.
There is a clear link between thyroid function and affective or mood disorders. THs have been used since over half a century to accelerate or potentiate antidepressant treatments (Aronson et al., 1996, Baumgartner, 2000). The specific mechanisms and functional pathways for these effects are yet to be understood. While depressive symptoms (i.e., fatigue and psychomotor slowing) are frequent features in hypothyroidism (symptoms that are generally reversible with return to euthyroid status), only a fraction of patients with major depression show biomedical signs of thyroid dysfunction (Bauer et al., 2008, Hage and Azar, 2012). 25-30% of depressed patients show a blunted TSH response to TRH (Loosen, 1985). Together with reports of elevated TRH levels in depressed patients (Banki et al., 1988) these findings suggest a chronic TRH hypersecretion by the PVN leading to a downregulation of pituitary TRH receptors, which may be mediated by elevated levels of cortisol.
THs also interact with neurotransmitter systems involved in mood regulation, including the serotonergic and noradrenergic systems (Henley and Koehnle, 1997, Bauer et al., 2002). In addition, thyroid hormone receptors are abundant in many limbic structures, which are associated with the pathogenesis of affective disorders and stress regulation (e.g. amygdala and hippocampus) (Ruel et al., 1985). Interestingly, treatment of rodents with antidepressants results in an increase of T3 in the amygdala, an essential structure in emotion regulation (Prengel et al., 2000, Pinna et al., 2003). Tricyclic antidepressants and SSRIs have been shown to enhance the activity of D2, resulting in an increased conversion of T4 into active T3 in the brain (Baumgartner et al., 1994, Campos-Barros et al., 1994, Campos-Barros et al., 1995). This finding is consistent with the hypothesis that depression is related to brain hypothyroidism together with systemic euthyroidism (Jackson, 1998), perhaps secondary to a cortisol-related decrease in D2 activity (Hidal and Kaplan, 1988). On the other hand, acute stress has been shown to increase D2 activity, particularly in the brain (Baumgartner et al., 1998). It is possible that this D2 activation may be a transient effect that disappears or is reversed in response to chronic stress or chronically increased cortisol levels. Depression is, of course, a very heterogeneous condition, and it is possible that thyroid dysfunction may play a role in its pathogenesis in only a subgroup of individuals.
3.1.3. Traumatic stress
In contrast to other forms of acute and chronic stress, stress associated with traumatic exposures (e.g., PTSD, childhood abuse) has generally been associated with an activation of thyroid function and thyrotoxicosis. As summarized by Wang (2006), elevated T3 concentrations have been reported in several samples of combat veterans with PTSD, including World War II, Vietnam, Israeli and Croatian samples. Increased T3 and/or decreased TSH levels were also found in civilian trauma patients (Olff et al., 2006) and survivors of childhood sexual abuse (Friedman et al., 2005). However, some studies have found the reverse biomedical symptomatology. Haviland et al. (2006) report lower levels of T3 among sexually abused adolescent girls, and Sinai et al. (2014) observed a lower fT3/fT4 ratio in women with borderline personality disorder (BPD) exposed to interpersonal violence during childhood. The reasons for these observed differences may include comorbid depression, the sex of the individual, as well as type, timing and duration of trauma exposure.
Interestingly, PTSD patients often show decreased HPA activation, whereas acute or chronic stress and depression is generally associated with an increase in HPA activity (Miller et al., 2007). This suggests a close relationship and a certain antagonism between HPA and HPT axis.
3.2. HPA-HPT-Interactions
3.2.1. Effect of GC administration and adrenal dysfunction on HPT function
In humans, glucocorticoid (GC) administration decreases plasma TSH levels and attenuates the pituitary TSH response to TRH stimulation (Faglia et al., 1973, Banos et al., 1979, Ahlquist et al., 1989, Taylor et al., 1995). In addition, GCs enhance the negative feedback effect of T3 on TSH release (Ahlquist et al., 1989). The inhibitory actions of GCs on TSH release seem to involve an lipocortin 1 (LC1) dependent mechanism (Taylor et al., 1995), which is also an important factor in the anti-inflammatory effect of GCs (Perretti and D'Acquisto, 2009). GCs do not seem to affect the sensitivity of the thyroid to TSH stimulation (Vigneri et al., 1975, Banos et al., 1979). Nevertheless, increased levels of GCs lead to a reduction in T3 and a concomitant increase in rT3 concentrations in the blood, while T4 levels are either unaltered or slightly reduced (Duick et al., 1974, Chopra et al., 1975, Vigneri et al., 1975, Burr et al., 1976, Degroot and Hoye, 1976, Banos et al., 1979). A decrease in serum T3 is also observed in athyreotic patients on L-T4 substitution therapy (Duick et al., 1974, Chopra et al., 1975, Degroot and Hoye, 1976), which suggests that these changes are, at least in part, due to a GC induced shift in the metabolism of T4, whereby conversion of T4 to T3 is reduced in favor of a conversion of T4 to the inactive metabolite rT3. In addition, although GCs have been found to have a stimulatory effect on the NIS (that mediates the active iodide uptake in the thyroid gland (Unterholzner et al., 2006)), they probably inhibit the secretory activity of the thyroid (Chopra et al., 1975, Woltz et al., 1983). This may explain the decrease in serum T4 observed in some studies (Vigneri et al., 1975, Degroot and Hoye, 1976, Banos et al., 1979). An alternate explanation may be the tonic inhibitory effect of GCs on the synthesis of TBG, which is abolished by adrenalectomy (Banos et al., 1979, Emerson et al., 1993). Lower TBG binding of T4 would lead to an increase in the fT4 fraction, which, in turn, may enhance negative feedback but also increase renal clearance of T4. Administration of ACTH also reduces HPT activity, however the effect appears to be mediated by an increase in adrenal GC secretion (Brown-Grant, 1956, Banos et al., 1979).
To conclude, GCs generally inhibit thyroid function (see Figure 1). However, more recent evidence suggests that while this so in adult individuals, the effect may be in the reverse direction during embryonic or fetal development. In sheep, maternal or fetal administration of GCs in late pregnancy increases plasma T3 and rT3 but not T4 concentrations, which is probably due to an increase in renal and hepatic D1 activity and a decrease in renal and placental D3 activity (Thomas et al., 1978, Wu et al., 1978, Forhead et al., 2006, Forhead et al., 2007). In addition, prenatal GCs appeared to have a maturational effect on the fetal rat thyroid gland (Manojlovic-Stojanoski et al., 2014) and pituitary TSH-cells (Manojlović-Stojanoski et al., 2010). In contrast to the effect in the fetus, in the ewes (mothers) dexamethasone treatment reduced plasma concentrations of T3 and T4 and increased rT3 without any change in tissue deiodinase activity (Forhead et al., 2007). Since T3 has important maturational effects in the fetus, including on lung function, thermogenesis and gluconeogenesis, it has been suggested that these changes in T3 availability may mediate some of the effects of antenatal GC treatment (Forhead et al., 2007). In fact, administration of dexamethasone and T3 together to pregnant rats has been shown to have additive effects on phospholipid synthesis in the fetal lung (Gross et al., 1984).
The maturation-promoting effects of GCs on the HPT axis, which may strengthen the offspring’s chance of survival in uncertain times, come at the cost of decreased proliferation and a possibly permanently reduced thyroid size and number of pituitary TSH-cells (Manojlović-Stojanoski et al., 2010, Manojlovic-Stojanoski et al., 2014), which likely limits the future capacity of the thyroid gland. Maternal GCs have, indeed, been shown to have long-term effects on the function of their offspring’s HPT axis (Slone-Wilcoxon and Redei, 2004). High levels of maternal GCs may, therefore, promote premature maturation of the HPT axis and other tissues, partly mediated by elevated fetal T3 concentrations, with long-term implications for offspring thyroid function.
3.2.2. Effect of TH administration and thyroid dysfunction on HPA function
Conversely, administration of THs to rats produces hypertrophy of the adrenal gland and increases in corticotrophin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH) and GC secretion and/or production (Boler and Moore, 1982, Shi et al., 1994, Johnson et al., 2005, Johnson et al., 2013). The same phenomenon is seen in hyperthyroid patients (Felber et al., 1959, Hellman et al., 1961, Kenny et al., 1967), although there may be a decreased adrenocortical reserve in the chronic state, which results in a lower GC response to ACTH stimulation (Tsatsoulis et al., 2000, Johnson et al., 2005). The effect of TH on HPA activity may be partly mediated by an increased metabolic clearance of cortisol from the blood in the hyperthyroid state (Brown et al., 1958, Kenny et al., 1967), or the preferential metabolism of cortisol into its biologically inactive form, cortisone (indicated by increased urinary concentrations of the cortisone metabolite THE) (Hellman et al., 1961, Hoshiro et al., 2006). THs also induce CBG-binding of corticosterone in the rat (Fortier et al., 1970, Johnson et al., 2013). All of these alterations may lead to a decreased negative feedback on HPA axis activity and, consequently, HPA hyperactivity (see Figure 1).
The opposite phenomenon is seen in thyroidectomized or PTU-treated rats as well as in human patients with hypothyroidism. Absence of TH results in decreased adrenal weight (Kamilaris et al., 1991, Tohei, 2004), decreased production of CRH, ACTH and GCs (Hellman et al., 1961, Kenny et al., 1967, Fortier et al., 1970, Shi et al., 1994), a reduced adrenocortical response to ACTH (Kamilaris et al., 1991, Tohei, 2004), and a compensatory increase in the ACTH response to CRH (Kamilaris et al., 1991, Tohei, 2004). However, in the hypothyroid state there seems to be also a decreased clearance of cortisol (Brown et al., 1958, Kenny et al., 1967) and a relative increase of cortisol metabolites as compared to cortisone metabolites (THF/THE ratio) (Hellman et al., 1961, Hoshiro et al., 2006). The latter is also seen in patients with mineralocorticoid excess (AME), which is caused by the inability of the enzyme 11b-hydroxysteroid dehydrogenase type 2 (11β-HSD2) to inactivate cortisol to cortisone (Turpeinen et al., 2006). This suggests that TH may stimulate the activity of this enzyme, whereas a lack of TH impairs its function. Further indirect support for an influence of TH on the activity of 11β-HSD2 is provided by two studies that administered radioactively labeled cortisol and cortisone to investigate the reaction rates of the cortisol-cortisone-interconversion, which appears to be generally slower in hypothyroid subjects. Ichikawa et al. reported a shift towards an altered equilibrium between these steroids in favor of cortisol (Ichikawa et al., 1977), whereas Zumoff et al. showed that the reverse was true for hyperthyroid subjects (Zumoff et al., 1983). In line with these findings, Iranmanesh et al. (1990) observed significantly elevated concentrations of cortisol in hypothyroid men (the study obtained a blood sample every 20 minutes for a 24-hr period). The effect was due to the prolonged half-life of cortisol and was largely reversible with T4 treatment (Iranmanesh et al., 1990). Interestingly, absence of TH also reduces the GC response to stress (Fortier et al., 1970, Rodriguez et al., 2003).
In the developing rat, a stress hypo-responsive period occurs within the first two weeks after birth, during which time the basal function of the HPA axis and the HPA response to stress are markedly reduced. Neonatal hypothyroidism impairs the maturation of hypothalamic parvocellular CRF and AVP gene expression during this period (Dakine et al., 2000a) and delays the onset of mature ACTH and corticosterone responses to stress (Walker et al., 1989). On the other hand, perinatal T4 treatment induces an increase in CRH mRNA expression in the whole population of CRH synthesizing cells of the PVN (Dakine et al., 2000b), positively influences the development of the HPA diurnal rhythm (Lengvari et al., 1977), and accelerates a mature adrenocortical response to stress (Poland et al., 1979, Walker et al., 1989). Perinatal THs also influence GR concentrations in the adult hippocampus, which are important for the regulation of the HPA response to stress and enhance GC negative feedback sensitivity. Administration of T4 or T3 to neonatal rat pups increases GR levels whereas PTU-treatment decreases hippocampal GR concentrations (Meaney et al., 1987). Furthermore, the sustained effect of early environmental factors, such as handling and maternal care, on the development of HPA axis regulation, appear to be dependent on stimulation-induced T3 release or an increased conversion of T4 to T3, which, in turn, increases serotonergic activity and NGFI-A levels in the hippocampus (Meaney et al., 2000, Hellstrom et al., 2012). Thus, high levels of THs may accelerate HPA axis maturation, whereas a lack of THs may delay HPA axis maturation. Based on these observations it appears that HPT dysregulation in early life may permanently program the HPA axis, with important consequences for the susceptibility to stress-related disease. In contrast to the developmental trajectory of the rodent HPA axis, the human HPA axis is quite mature by the time of birth, so these same effects of high or low TH concentrations on HPA maturation may occur in humans during the prenatal (as opposed to postnatal) period of development.
3.2.3. Functional interaction of thyroid and adrenal hormones
A well-characterized functional interaction between THs and GCs has been documented for the stimulation of growth hormone (GH) synthesis in the pituitary. While GCs alone seem to have a small or no effect on GH production in vitro, they appear to potentiate the action of T3 (Martial et al., 1977, Samuels et al., 1977). This synergistic effect appears to be dependent on the simultaneous presence of both GR and TR in the cell nucleus and requires GR binding to DNA (Leers et al., 1994). THs and GCs also cooperate in the induction of cAMP-induced synthesis of hepatic phosphoenolpyruvate carboxykinase (PEPck), a rate-limiting enzyme in gluconeogenesis (Hoppner et al., 1986). So, although there appears to be a certain antagonism of THs and GCs with respect to their effect on the respective other axis, the hormones seem to have synergistic actions on other target tissues. Thus, a balance in the activity of both axes may be of critical importance for the bodily homeostasis.
3.3. Relevance in pregnancy
In the human fetus, GCs and THs in adequate levels may have a synergistic effect on fetal tissue maturation, which is reflected in the co-occurrence of the T3 and cortisol surges at term and further rise through labor. Both hormones have important functions in preparing the fetus for extrauterine life but may also permanently affect the development of the CNS if an imbalance occurs during intrauterine development. Maternal stress and/or chronically increased cortisol concentrations most likely reduce maternal circulating THs. At the same time, administration of GCs to the mother may increase fetal T3 levels, although, to date, this effect has only been examined in late pregnancy in sheep (Wu et al., 1978, Forhead et al., 2006, Forhead et al., 2007). Administration of GCs a couple of weeks or days before birth may prepone the timing of the naturally occurring surge in cortisol and T3 that is observed in sheep and humans. This effect appears to be mediated by an increased fetal D1 activity, a decreased placental D3 activity, as well as a premature maturation of the thyroid gland (Forhead et al., 2006, Manojlovic-Stojanoski et al., 2014). It is conceivable that part of the programming effects of prenatal stress or glucocorticoid administration in cases of imminent preterm birth on the function of various tissues (Cottrell and Seckl, 2009) may be mediated by a premature switch from proliferation to differentiation and the resultant reduction in cell numbers as a result of an untimely excess of T3 levels. However, it is important to note that the fetal thyroid only becomes functional around mid-gestation, and fetal D1 activity is very low relative to D3 activity during most of gestation (Darras et al., 1999), so that the effect of GCs on fetal T3 concentrations in early or mid gestation may in fact be very different from the effects seen at term. Furthermore, the vast majority of brain T3 is not derived from circulation but from local conversion of T4 to T3 by D2 (Crantz et al., 1982). Chronically elevated GCs or chronic stress may lead to less T4 in the fetal circulation, secondary to a decrease of T4 concentrations in the maternal compartment, and thus to lower concentrations of T3 in the fetal brain.
Both low T3 and high GCs adversely impact fetal brain development. It is not only possible but probable that their combined effect on the developing brain is either additive or multiplicative in nature. Brain areas likely to be particularly impacted include the developing hippocampus, which is highly sensitive to both hormones (Gould et al., 1991). The hippocampus is an important structure for cognitive processes such as memory and learning, and it also is involved in stress and emotion regulation.
In addition, low maternal thyroid function may decrease cortisol clearance from blood and reduce metabolism into inactive cortisone, potentially by impairing 11β-HSD2 activity. 11β-HSD2 is also highly expressed in the placenta, presumably to limit placental transfer of maternal GC to the fetal compartment. It is plausible that placental metabolism of cortisol may also be impaired by a lack of TH, thereby causing greater and/or premature exposure of cortisol in the fetus, however this has not yet been studied. Thus, in these ways, some of the effects of high maternal GCs on fetal brain development may be modulated by maternal thyroid status.
4. Summary and conclusion
THs affect multiple maturational processes of the central nervous system, and these effects are already apparent very early in the developmental process. During this time, even small or subtle alterations in brain structure or function can become progressively and substantially magnified during subsequent developmental periods to produce long-lasting or permanent deficits, which are largely irreversible by postnatal T4 treatment. Because the fetus is dependent on maternal TH supply in the first half of gestation and continues to be partially dependent on maternal supply until the end of gestation, it is of significant clinical importance to determine the specific effects of maternal thyroid dysfunction on the development of the fetal brain. The overview of the existent literature provided here suggests that even more moderate forms of thyroid dysfunction such as maternal hypothyroxinemia, particularly in the beginning of pregnancy, may have a long-lasting influence on child cognitive development and on the risk of developing neurodevelopmental disorders. Furthermore, adverse conditions that the mother may experience during pregnancy, such as various forms of stress, also may negatively affect her thyroid function. The HPT axis is stress-sensitive and may itself be involved in the development of stress-regulatory systems in the brain. Thus, optimal levels of maternal THs may not only be relevant for child cognitive function but may also be involved in the fetal programming of stress-related phenotypes and diseases.
To date, information is lacking regarding the interactive effect of maternal prenatal adverse conditions, such as chronic stress, and maternal thyroid function on the development of the fetal brain. To elucidate the nature of this interaction and potential sensitive periods during fetal brain development, future research studies should include serial assessments of maternal thyroid function as well as her psychological state and HPA axis activity over the entire course of pregnancy. A better understanding of HPT-HPA interactions during gestation may eventually result in a more optimal management of maternal thyroid dysfunction, and this may also include aspects of stress management, in order to minimize the detrimental effect of TH deficiency on fetal neurodevelopment.
In addition, knowledge gaps exist regarding the (preceding) changes in brain structure and function that underlie cognitive impairments observed in the children of TH deficient mothers. Because the cognitive impairments due to severe maternal TH deficiency are known to be refractory to T4 substitution after birth, it is critical to elucidate the specific nature and timing of the putative effects of more moderate forms of maternal thyroid dysfunction, and to separate them from influences of the postnatal environment. Multi-modal magnetic resonance imaging assessments, performed shortly after birth to obtain a “baseline” measure of brain developmental status that is not confounded by postnatal influences, may shed more light about the specific neurodevelopmental consequences of prenatal TH deficiency. A focus on anatomy, structural and functional connectivity of the sensorimotor and fronto-limbic networks (including the hippocampus), as well as the default mode network (DMN), would be of interest and relevance given the role THs play in development of brain circuits in general, and because disrupted development of these specific circuits may underlie changes in cognition and psychomotor function as well as neurodevelopmental (e.g. autism, ADHD) and psychiatric (e.g. depression) conditions (Geuze et al., 2005, Woodward et al., 2006, Zhang and Raichle, 2010).
The majority of the existing studies, particularly in humans, have focused solely on the effects of maternal TH deficiency. Very little is known about the effects of maternal TH excess on fetal brain development and function. This aspect warrants more attention, since accelerated maturation may prove to be just as detrimental as delayed maturation. Another knowledge gap exists with respect to gene-environment interactions on brain developmental trajectories. Serum thyroid parameters exhibit substantial inter-individual variability, and the heritability of the HPT set-point has been estimated to be 40-60% (Medici et al., 2015). However, the impact of polymorphisms in TH pathway genes on offspring neurodevelopment has not yet been considered in the literature.
Iodine deficiency continues to affect millions of people worldwide, and the problem is not restricted to developing countries (WHO/UNICEF/ICCIDD, 2007). Furthermore, hypothyroidism caused by autoimmune processes such as Hashimoto thyroiditis is one of the most frequent endocrine disorders, affecting primarily the female population (Vanderpump, 2011). The cognitive impairments in children produced by severe maternal TH deficiency during pregnancy are well-established and clearly evident. Of even greater public health relevance, however, could be the effects of the even more frequent, milder forms of maternal thyroid dysfunction, since their initial effects may be less pronounced und thus easily disregarded. Gaining a better understanding of the independent contribution of maternal thyroid function during pregnancy and its interaction with adverse prenatal conditions may inform screening and intervention and screening strategies at a time when the brain is still highly plastic.
Highlights.
Thyroid hormones (TH) are crucial for key maturational processes during early brain development.
Maternal TH deficiency during pregnancy may result in impaired offspring cognitive development.
Gestational conditions related to stress may modulate maternal thyroid function.
Acknowledgements
Supported, in part, by US PHS (NIH) grants R01 MH-091351 (to CB) und R01 HD-060628 (to PDW).
Abbreviations
- 11β-HSD2
11b-hydroxysteroid dehydrogenase type 2
- ACTH
adrenocorticotropic hormone
- ADHD
attention-deficit hyperactivity disorder
- ASD
autism spectrum disorder
- BDNF
brain-derived neurotrophic factor
- CNS
central nervous system
- CRH
corticotropin-releasing hormone
- D
deiodinase
- DG
dentate gyrus
- fT4
free thyroxine
- fT3
free triiodothyronine
- GABA
γ-aminobutyric acid
- GC
glucocorticoid
- hCG
human chorionic gonadotropin
- HPA
hypothalamic-pituitary-adrenal
- HPT
hypothalamic-pituitary-thyroid
- KCC2
K+/Cl− cotransporter
- LAT
L-amino acid transporter
- LTP
long-term potentiation
- MCT
monocarboxylate transporter
- MDI
mental development index
- MMI
methimazole
- NIS
sodium-iodide symporter
- OATP
organic anion transporting peptide
- OH
overt hypothyroidism
- PDI
psychomotor development index
- PTSD
post-traumatic stress disorder
- PTU
propylthiouracil
- PV
parvalbumin
- PVN
paraventricular nucleus
- RCT
randomized control trial
- rT3
reverse T3
- SCH
subclinical hypothyroidism
- T3
triiodothyronine
- T4
thyroxine
- TBG
thyroxine-binding globulin
- TH
thyroid hormone (T3 and T4)
- THT
transmembrane thyroid hormone-transporter
- TPO
thyroid peroxidase
- TR
thyroid hormone receptor
- TRH
thyrotropin-releasing hormone
- TSH
thyroid-stimulating hormone
- TTR
transthyretin
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abdallah MW, Mortensen EL, Greaves-Lord K, Larsen N, Bonefeld-Jorgensen EC, Norgaard-Pedersen B, Hougaard DM, Grove J. Neonatal levels of neurotrophic factors and risk of autism spectrum disorders. Acta psychiatrica Scandinavica. 2013;128:61–69. doi: 10.1111/acps.12020. [DOI] [PubMed] [Google Scholar]
- Abraham H, Vincze A, Jewgenow I, Veszpremi B, Kravjak A, Gomori E, Seress L. Myelination in the human hippocampal formation from midgestation to adulthood. International journal of developmental neuroscience : the official journal of the International Society for Developmental Neuroscience. 2010;28:401–410. doi: 10.1016/j.ijdevneu.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Aguado F, Carmona MA, Pozas E, Aguilo A, Martinez-Guijarro FJ, Alcantara S, Borrell V, Yuste R, Ibanez CF, Soriano E. BDNF regulates spontaneous correlated activity at early developmental stages by increasing synaptogenesis and expression of the K+/Cl− co-transporter KCC2. Development. 2003;130:1267–1280. doi: 10.1242/dev.00351. [DOI] [PubMed] [Google Scholar]
- Ahlquist JA, Franklyn JA, Ramsden DB, Sheppard MC. The influence of dexamethasone on serum thyrotrophin and thyrotrophin synthesis in the rat. Molecular and cellular endocrinology. 1989;64:55–61. doi: 10.1016/0303-7207(89)90064-6. [DOI] [PubMed] [Google Scholar]
- Ahmed OM, Abd El-Tawab SM, Ahmed RG. Effects of experimentally induced maternal hypothyroidism and hyperthyroidism on the development of rat offspring: I. The development of the thyroid hormones-neurotransmitters and adenosinergic system interactions. International journal of developmental neuroscience : the official journal of the International Society for Developmental Neuroscience. 2010;28:437–454. doi: 10.1016/j.ijdevneu.2010.06.007. [DOI] [PubMed] [Google Scholar]
- Ahmed RG. Hypothyroidism and brain developmental players. Thyroid research. 2015;8:2. doi: 10.1186/s13044-015-0013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Dolado M, Cuadrado A, Navarro-Yubero C, Sonderegger P, Furley AJ, Bernal J, Munoz A. Regulation of the L1 cell adhesion molecule by thyroid hormone in the developing brain. Molecular and cellular neurosciences. 2000;16:499–514. doi: 10.1006/mcne.2000.0879. [DOI] [PubMed] [Google Scholar]
- Alvarez-Dolado M, Figueroa A, Kozlov S, Sonderegger P, Furley AJ, Munoz A. Thyroid hormone regulates TAG-1 expression in the developing rat brain. The European journal of neuroscience. 2001;14:1209–1218. doi: 10.1046/j.0953-816x.2001.01745.x. [DOI] [PubMed] [Google Scholar]
- Alvarez-Dolado M, Gonzalez-Sancho JM, Bernal J, Munoz A. Developmental expression of the tenascin-C is altered by hypothyroidism in the rat brain. Neuroscience. 1998;84:309–322. doi: 10.1016/s0306-4522(97)00511-3. [DOI] [PubMed] [Google Scholar]
- Alvarez-Dolado M, Ruiz M, Del Rio JA, Alcantara S, Burgaya F, Sheldon M, Nakajima K, Bernal J, Howell BW, Curran T, Soriano E, Munoz A. Thyroid hormone regulates reelin and dab1 expression during brain development. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1999;19:6979–6993. doi: 10.1523/JNEUROSCI.19-16-06979.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen SL, Laurberg P, Wu CS, Olsen J. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a Danish nationwide cohort study. BJOG : an international journal of obstetrics and gynaecology. 2014a;121:1365–1374. doi: 10.1111/1471-0528.12681. [DOI] [PubMed] [Google Scholar]
- Andersen SL, Olsen J, Wu CS, Laurberg P. Psychiatric disease in late adolescence and young adulthood. Foetal programming by maternal hypothyroidism? Clinical endocrinology. 2014b;81:126–133. doi: 10.1111/cen.12415. [DOI] [PubMed] [Google Scholar]
- Aoki Y, Belin RM, Clickner R, Jeffries R, Phillips L, Mahaffey KR. Serum TSH and total T4 in the United States population and their association with participant characteristics: National Health and Nutrition Examination Survey (NHANES 1999-2002) Thyroid : official journal of the American Thyroid Association. 2007;17:1211–1223. doi: 10.1089/thy.2006.0235. [DOI] [PubMed] [Google Scholar]
- Aronson R, Offman HJ, Joffe RT, Naylor CD. Triiodothyronine augmentation in the treatment of refractory depression. A meta-analysis. Archives of general psychiatry. 1996;53:842–848. doi: 10.1001/archpsyc.1996.01830090090013. [DOI] [PubMed] [Google Scholar]
- Arturi F, Lacroix L, Presta I, Scarpelli D, Caillou B, Schlumberger M, Russo D, Bidart JM, Filetti S. Regulation by human chorionic gonadotropin of sodium/iodide symporter gene expression in the JAr human choriocarcinoma cell line. Endocrinology. 2002;143:2216–2220. doi: 10.1210/endo.143.6.8844. [DOI] [PubMed] [Google Scholar]
- Ausó E, Cases O, Fouquet C, Camacho M, García-Velasco J-V, Gaspar P, Berbel P. Protracted expression of serotonin transporter and altered thalamocortical projections in the barrelfield of hypothyroid rats. European Journal of Neuroscience. 2001;14:1968–1980. doi: 10.1046/j.0953-816x.2001.01815.x. [DOI] [PubMed] [Google Scholar]
- Auso E, Lavado-Autric R, Cuevas E, Del Rey FE, Morreale De Escobar G, Berbel P. A moderate and transient deficiency of maternal thyroid function at the beginning of fetal neocorticogenesis alters neuronal migration. Endocrinology. 2004;145:4037–4047. doi: 10.1210/en.2004-0274. [DOI] [PubMed] [Google Scholar]
- Axelstad M, Hansen PR, Boberg J, Bonnichsen M, Nellemann C, Lund SP, Hougaard KS, Hass U. Developmental neurotoxicity of propylthiouracil (PTU) in rats: relationship between transient hypothyroxinemia during development and long-lasting behavioural and functional changes. Toxicol Appl Pharmacol. 2008;232:1–13. doi: 10.1016/j.taap.2008.05.020. [DOI] [PubMed] [Google Scholar]
- Azizi F, Aminorroya A, Hedayati M, Rezvanian H, Amini M, Mirmiran P. Urinary iodine excretion in pregnant women residing in areas with adequate iodine intake. Public health nutrition. 2003;6:95–98. doi: 10.1079/PHN2002366. [DOI] [PubMed] [Google Scholar]
- Banki CM, Bissette G, Arato M, Nemeroff CB. Elevation of immunoreactive CSF TRH in depressed patients. The American journal of psychiatry. 1988;145:1526–1531. doi: 10.1176/ajp.145.12.1526. [DOI] [PubMed] [Google Scholar]
- Banos C, Tako J, Salamon F, Gyorgyi S, Czikkely R. Effect of ACTH-stimulated glucocorticoid hypersecretion on the serum concentrations of thyroxine-binding globulin, thyroxine, triiodothyronine, reverse triiodothyronine and on the TSH-response to TRH. Acta medica Academiae Scientiarum Hungaricae. 1979;36:381–394. [PubMed] [Google Scholar]
- Bansal R, You SH, Herzig CT, Zoeller RT. Maternal thyroid hormone increases HES expression in the fetal rat brain: an effect mimicked by exposure to a mixture of polychlorinated biphenyls (PCBs) Brain research Developmental brain research. 2005;156:13–22. doi: 10.1016/j.devbrainres.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Bath SC, Steer CD, Golding J, Emmett P, Rayman MP. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the Avon Longitudinal Study of Parents and Children (ALSPAC) Lancet. 2013;382:331–337. doi: 10.1016/S0140-6736(13)60436-5. [DOI] [PubMed] [Google Scholar]
- Bauer M, Goetz T, Glenn T, Whybrow PC. The thyroid-brain interaction in thyroid disorders and mood disorders. Journal of neuroendocrinology. 2008;20:1101–1114. doi: 10.1111/j.1365-2826.2008.01774.x. [DOI] [PubMed] [Google Scholar]
- Bauer M, Heinz A, Whybrow PC. Thyroid hormones, serotonin and mood: of synergy and significance in the adult brain. Mol Psychiatry. 2002;7:140–156. doi: 10.1038/sj.mp.4000963. [DOI] [PubMed] [Google Scholar]
- Bauer M, Priebe S, Kurten I, Graf KJ, Baumgartner A. Psychological and endocrine abnormalities in refugees from East Germany: Part I. Prolonged stress, psychopathology, and hypothalamic-pituitary-thyroid axis activity. Psychiatry research. 1994;51:61–73. doi: 10.1016/0165-1781(94)90047-7. [DOI] [PubMed] [Google Scholar]
- Baumgartner A. Thyroxine and the treatment of affective disorders: an overview of the results of basic and clinical research. The international journal of neuropsychopharmacology / official scientific journal of the Collegium Internationale Neuropsychopharmacologicum (CINP) 2000;3:149–165. doi: 10.1017/S1461145700001887. [DOI] [PubMed] [Google Scholar]
- Baumgartner A, Dubeyko M, Campos-Barros A, Eravci M, Meinhold H. Subchronic administration of fluoxetine to rats affects triiodothyronine production and deiodination in regions of the cortex and in the limbic forebrain. Brain research. 1994;635:68–74. doi: 10.1016/0006-8993(94)91424-9. [DOI] [PubMed] [Google Scholar]
- Baumgartner A, Hiedra L, Pinna G, Eravci M, Prengel H, Meinhold H. Rat Brain Type II 5′-Iodothyronine Deiodinase Activity Is Extremely Sensitive to Stress. Journal of Neurochemistry. 1998;71:817–826. doi: 10.1046/j.1471-4159.1998.71020817.x. [DOI] [PubMed] [Google Scholar]
- Ben-Ari Y. Excitatory actions of gaba during development: the nature of the nurture. Nat Rev Neurosci. 2002;3:728–739. doi: 10.1038/nrn920. [DOI] [PubMed] [Google Scholar]
- Ben-Ari Y, Gaiarsa J-L, Tyzio R, Khazipov R. GABA: A Pioneer Transmitter That Excites Immature Neurons and Generates Primitive Oscillations. Physiological Reviews. 2007;87:1215–1284. doi: 10.1152/physrev.00017.2006. [DOI] [PubMed] [Google Scholar]
- Beninger RJ. The role of dopamine in locomotor activity and learning. Brain research. 1983;287:173–196. doi: 10.1016/0165-0173(83)90038-3. [DOI] [PubMed] [Google Scholar]
- Berbel P, Auso E, Garcia-Velasco JV, Molina ML, Camacho M. Role of thyroid hormones in the maturation and organisation of rat barrel cortex. Neuroscience. 2001;107:383–394. doi: 10.1016/s0306-4522(01)00368-2. [DOI] [PubMed] [Google Scholar]
- Berbel P, Guadaño-Ferraz A, Angulo A, Cerezo JRn. Role of thyroid hormones in the maturation of interhemispheric connections in rats. Behavioural brain research. 1994;64:9–14. doi: 10.1016/0166-4328(94)90114-7. [DOI] [PubMed] [Google Scholar]
- Berbel P, Marco P, Cerezo J, DeFelipe J. Distribution of parvalbumin immunoreactivity in the neocortex of hypothyroid adult rats. Neuroscience letters. 1996;204:65–68. doi: 10.1016/0304-3940(96)12318-1. [DOI] [PubMed] [Google Scholar]
- Berbel P, Mestre JL, Santamaria A, Palazon I, Franco A, Graells M, Gonzalez-Torga A, de Escobar GM. Delayed neurobehavioral development in children born to pregnant women with mild hypothyroxinemia during the first month of gestation: the importance of early iodine supplementation. Thyroid : official journal of the American Thyroid Association. 2009;19:511–519. doi: 10.1089/thy.2008.0341. [DOI] [PubMed] [Google Scholar]
- Berbel P, Navarro D, Roman GC. An evo-devo approach to thyroid hormones in cerebral and cerebellar cortical development: etiological implications for autism. Frontiers in endocrinology. 2014;5:146. doi: 10.3389/fendo.2014.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernal J. The significance of thyroid hormone transporters in the brain. Endocrinology. 2005;146:1698–1700. doi: 10.1210/en.2005-0134. [DOI] [PubMed] [Google Scholar]
- Bernal J. Thyroid hormone receptors in brain development and function. Nature clinical practice Endocrinology & metabolism. 2007;3:249–259. doi: 10.1038/ncpendmet0424. [DOI] [PubMed] [Google Scholar]
- Bianco AC, Nunes MT, Hell NS, Maciel RMB. The Role of Glucocorticoids in the Stress-Induced Reduction of Extrathyroidal 3,5,3′-Triiodothyronine Generation in Rats. Endocrinology. 1987;120:1033–1038. doi: 10.1210/endo-120-3-1033. [DOI] [PubMed] [Google Scholar]
- Boler RK, Moore NA. Depression of Adrenocortical Function by Pharmacologic Doses of Thyroxine in Intact and Unilaterally Adrenalectomized Rats. Hormone Research in Paediatrics. 1982;16:209–218. doi: 10.1159/000179504. [DOI] [PubMed] [Google Scholar]
- Bourgeois JP. Synaptogenesis, heterochrony and epigenesis in the mammalian neocortex. Acta paediatrica. 1997;422:27–33. doi: 10.1111/j.1651-2227.1997.tb18340.x. [DOI] [PubMed] [Google Scholar]
- Braunstein GD. Endocrine Changes in Pregnancy. In: Melmed S, et al., editors. Williams Textbook of Endocrinology. 12th ed Saunders (Elsevier); Philadelphia, PA: 2011. [Google Scholar]
- Brent GA. The Debate over Thyroid-Function Screening in Pregnancy. New England Journal of Medicine. 2012;366:562–563. doi: 10.1056/NEJMe1112591. [DOI] [PubMed] [Google Scholar]
- Brosvic GM, Taylor JN, Dihoff RE. Influences of early thyroid hormone manipulations: Delays in pup motor and exploratory behavior are evident in adult operant performance. Physiology & behavior. 2002;75:697–715. doi: 10.1016/s0031-9384(02)00668-6. [DOI] [PubMed] [Google Scholar]
- Brown-Grant K. The effect of ACTH and adrenal steroids on thyroid activity, with observations on the adrenal-thyroid relationship. The Journal of physiology. 1956;131:58–69. doi: 10.1113/jphysiol.1956.sp005444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown H, Englert E, Jr., Wallach S. Metabolism of free and conjugated 17-hydroxycorticosteroids in subjects with thyroid disease. The Journal of clinical endocrinology and metabolism. 1958;18:167–179. doi: 10.1210/jcem-18-2-167. [DOI] [PubMed] [Google Scholar]
- Buchholz DR. More similar than you think: Frog metamorphosis as a model of human perinatal endocrinology. Developmental biology. 2015 doi: 10.1016/j.ydbio.2015.02.018. [DOI] [PubMed] [Google Scholar]
- Burr WA, Ramsden DB, Griffiths RS, Black EG, Hoffenberg R, Meinhold H, Wenzel KW. Effect of a single dose of dexamethasone on serum concentrations of thyroid hormones. Lancet. 1976;2:58–61. doi: 10.1016/s0140-6736(76)92283-2. [DOI] [PubMed] [Google Scholar]
- Burrow GN, Fisher DA, Larsen PR. Maternal and fetal thyroid function. The New England journal of medicine. 1994;331:1072–1078. doi: 10.1056/NEJM199410203311608. [DOI] [PubMed] [Google Scholar]
- Buss C, Davis EP, Hobel CJ, Sandman CA. Maternal pregnancy-specific anxiety is associated with child executive function at 6-9 years age. Stress. 2011;14:665–676. doi: 10.3109/10253890.2011.623250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss C, Davis EP, Shahbaba B, Pruessner JC, Head K, Sandman CA. Maternal cortisol over the course of pregnancy and subsequent child amygdala and hippocampus volumes and affective problems. Proceedings of the National Academy of Sciences of the United States of America. 2012a;109:E1312–1319. doi: 10.1073/pnas.1201295109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss C, Entringer S, Swanson JM, Wadhwa PD. The Role of Stress in Brain Development: The Gestational Environment's Long-Term Effects on the Brain. Cerebrum : the Dana forum on brain science. 2012b;2012:4. [PMC free article] [PubMed] [Google Scholar]
- Buss C, Wolf OT, Witt J, Hellhammer DH. Autobiographic memory impairment following acute cortisol administration. Psychoneuroendocrinology. 2004;29:1093–1096. doi: 10.1016/j.psyneuen.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Caldwell KL, Makhmudov A, Ely E, Jones RL, Wang RY. Iodine status of the U.S. population, National Health and Nutrition Examination Survey, 2005-2006 and 2007-2008. Thyroid : official journal of the American Thyroid Association. 2011;21:419–427. doi: 10.1089/thy.2010.0077. [DOI] [PubMed] [Google Scholar]
- Calvo RM, Jauniaux E, Gulbis B, Asuncion M, Gervy C, Contempre B, Morreale de Escobar G. Fetal tissues are exposed to biologically relevant free thyroxine concentrations during early phases of development. The Journal of clinical endocrinology and metabolism. 2002;87:1768–1777. doi: 10.1210/jcem.87.4.8434. [DOI] [PubMed] [Google Scholar]
- Campos-Barros A, Meinhold H, Köhler R, Müller F, Eravci M, Baumgartner A. The effects of desipramine on thyroid hormone concentrations in rat brain. Naunyn-Schmiedeberg's Arch Pharmacol. 1995;351:469–474. doi: 10.1007/BF00171037. [DOI] [PubMed] [Google Scholar]
- Campos-Barros A, Meinhold H, Stula M, Muller F, Kohler R, Eravci M, Putzien O, Baumgartner A. The influence of desipramine on thyroid hormone metabolism in rat brain. The Journal of pharmacology and experimental therapeutics. 1994;268:1143–1152. [PubMed] [Google Scholar]
- Chan S, Kachilele S, McCabe CJ, Tannahill LA, Boelaert K, Gittoes NJ, Visser TJ, Franklyn JA, Kilby MD. Early expression of thyroid hormone deiodinases and receptors in human fetal cerebral cortex. Brain research Developmental brain research. 2002;138:109–116. doi: 10.1016/s0165-3806(02)00459-5. [DOI] [PubMed] [Google Scholar]
- Chan SY, Franklyn JA, Pemberton HN, Bulmer JN, Visser TJ, McCabe CJ, Kilby MD. Monocarboxylate transporter 8 expression in the human placenta: the effects of severe intrauterine growth restriction. The Journal of endocrinology. 2006;189:465–471. doi: 10.1677/joe.1.06582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Zhou Z, Zhong M, Zhang Y, Li M, Zhang L, Qu M, Yang J, Wang Y, Yu Z. Thyroid Hormone Promotes Neuronal Differentiation of Embryonic Neural Stem Cells by Inhibiting STAT3 Signaling Through TRalpha1. Stem cells and development. 2012 doi: 10.1089/scd.2012.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng SY, Leonard JL, Davis PJ. Molecular aspects of thyroid hormone actions. Endocrine reviews. 2010;31:139–170. doi: 10.1210/er.2009-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevrier J, Harley KG, Kogut K, Holland N, Johnson C, Eskenazi B. Maternal Thyroid Function during the Second Half of Pregnancy and Child Neurodevelopment at 6, 12, 24, and 60 Months of Age. Journal of thyroid research. 2011;2011:426427. doi: 10.4061/2011/426427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra IJ, Williams DE, Orgiazzi J, Solomon DH. Opposite Effects of Dexamethasone on Serum Concentrations of 3, 3′,5′-Triiodothyronine (Reverse T3) and 3,3′,5′-Triiodothyronine (T3) The Journal of Clinical Endocrinology & Metabolism. 1975;41:911–920. doi: 10.1210/jcem-41-5-911. [DOI] [PubMed] [Google Scholar]
- Cizza G, Brady LS, Esclapes M, Blackman MR, Gold PW, Chrousos GP. Age and Gender Influence Basal and Stress-Modulated Hypothalamic-Pituitary-Thyroidal Function in Fischer 344/N Rats. Neuroendocrinology. 1996;64:440–448. doi: 10.1159/000127150. [DOI] [PubMed] [Google Scholar]
- Coghlan S, Horder J, Inkster B, Mendez MA, Murphy DG, Nutt DJ. GABA system dysfunction in autism and related disorders: From synapse to symptoms. Neuroscience & Biobehavioral Reviews. 2012;36:2044–2055. doi: 10.1016/j.neubiorev.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contempre B, Jauniaux E, Calvo R, Jurkovic D, Campbell S, de Escobar GM. Detection of thyroid hormones in human embryonic cavities during the first trimester of pregnancy. The Journal of clinical endocrinology and metabolism. 1993;77:1719–1722. doi: 10.1210/jcem.77.6.8263162. [DOI] [PubMed] [Google Scholar]
- Costeira MJ, Oliveira P, Santos NC, Ares S, Saenz-Rico B, de Escobar GM, Palha JA. Psychomotor development of children from an iodine-deficient region. The Journal of pediatrics. 2011;159:447–453. doi: 10.1016/j.jpeds.2011.02.034. [DOI] [PubMed] [Google Scholar]
- Cottrell EC, Seckl JR. Prenatal stress, glucocorticoids and the programming of adult disease. Frontiers in behavioral neuroscience. 2009;3:19. doi: 10.3389/neuro.08.019.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council on Environmental Health. Rogan WJ, Paulson JA, Baum C, Brock-Utne AC, Brumberg HL, Campbell CC, Lanphear BP, Lowry JA, Osterhoudt KC, Sandel MT, Spanier A, Trasande L. Iodine deficiency, pollutant chemicals, and the thyroid: new information on an old problem. Pediatrics. 2014;133:1163–1166. doi: 10.1542/peds.2014-0900. [DOI] [PubMed] [Google Scholar]
- Craig WY, Allan WC, Kloza EM, Pulkkinen AJ, Waisbren S, Spratt DI, Palomaki GE, Neveux LM, Haddow JE. Mid-gestational maternal free thyroxine concentration and offspring neurocognitive development at age two years. The Journal of clinical endocrinology and metabolism. 2012;97:E22–28. doi: 10.1210/jc.2011-1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crantz FR, Silva JE, Larsen PR. An Analysis of the Sources and Quantity of 3,5,3′-Triiodothyronine Specifically Bound to Nuclear Receptors in Rat Cerebral Cortex and Cerebellum. Endocrinology. 1982;110:367–375. doi: 10.1210/endo-110-2-367. [DOI] [PubMed] [Google Scholar]
- Cremaschi GA, Gorelik G, Klecha AJ, Lysionek AE, Genaro AM. Chronic stress influences the immune system through the thyroid axis. Life Sciences. 2000;67:3171–3179. doi: 10.1016/s0024-3205(00)00909-7. [DOI] [PubMed] [Google Scholar]
- Cuevas E, Auso E, Telefont M, Morreale de Escobar G, Sotelo C, Berbel P. Transient maternal hypothyroxinemia at onset of corticogenesis alters tangential migration of medial ganglionic eminence-derived neurons. The European journal of neuroscience. 2005;22:541–551. doi: 10.1111/j.1460-9568.2005.04243.x. [DOI] [PubMed] [Google Scholar]
- Curling TB. Two Cases of absence of the Thyroid body, and symmetrical swellings of fat tissue at the sides of the neck, connected with defective cerebral development. Medico-chirurgical transactions. 1850;33:303–306. doi: 10.1177/095952875003300123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakine N, Oliver C, Grino M. Effects of experimental hypothyroidism on the development of the hypothalamo-pituitary-adrenal axis in the rat. Life Sci. 2000a;67:2827–2844. doi: 10.1016/s0024-3205(00)00869-9. [DOI] [PubMed] [Google Scholar]
- Dakine N, Oliver C, Grino M. Thyroxine modulates corticotropin-releasing factor but not arginine vasopressin gene expression in the hypothalamic paraventricular nucleus of the developing Rat. Journal of neuroendocrinology. 2000b;12:774–783. doi: 10.1046/j.1365-2826.2000.00520.x. [DOI] [PubMed] [Google Scholar]
- Darbra S, Garau A, Balada F, Sala J, Marfg-Carbonell MA. Perinatal hypothyroidism effects on neuromotor competence, novelty-directed exploratory and anxiety-related behaviour and learning in rats. Behavioural brain research. 2003;143:209–215. doi: 10.1016/s0166-4328(03)00041-x. [DOI] [PubMed] [Google Scholar]
- Darras VM, Houbrechts AM, Van Herck SLJ. Intracellular thyroid hormone metabolism as a local regulator of nuclear thyroid hormone receptor-mediated impact on vertebrate development. Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms. 2015;1849:130–141. doi: 10.1016/j.bbagrm.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Darras VM, Hume R, Visser TJ. Regulation of thyroid hormone metabolism during fetal development. Molecular and cellular endocrinology. 1999;151:37–47. doi: 10.1016/s0303-7207(99)00088-x. [DOI] [PubMed] [Google Scholar]
- de Escobar GM, Ares S, Berbel P, Obregon MJ, del Rey FE. The changing role of maternal thyroid hormone in fetal brain development. Seminars in perinatology. 2008;32:380–386. doi: 10.1053/j.semperi.2008.09.002. [DOI] [PubMed] [Google Scholar]
- de Escobar GM, Obregon MJ, del Rey FE. Maternal thyroid hormones early in pregnancy and fetal brain development. Best practice & research Clinical endocrinology & metabolism. 2004;18:225–248. doi: 10.1016/j.beem.2004.03.012. [DOI] [PubMed] [Google Scholar]
- Degroot LJ, Hoye K. Dexamethasone suppression of serum T3 and T4. The Journal of clinical endocrinology and metabolism. 1976;42:976–978. doi: 10.1210/jcem-42-5-976. [DOI] [PubMed] [Google Scholar]
- Dentice M, Marsili A, Zavacki A, Larsen PR, Salvatore D. The deiodinases and the control of intracellular thyroid hormone signaling during cellular differentiation. Biochimica et Biophysica Acta (BBA) - General Subjects. 2013;1830:3937–3945. doi: 10.1016/j.bbagen.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong J, Liu W, Wang Y, Xi Q, Chen J. Hypothyroidism following developmental iodine deficiency reduces hippocampal neurogranin, CaMK II and calmodulin and elevates calcineurin in lactational rats. International Journal of Developmental Neuroscience. 2010;28:589–596. doi: 10.1016/j.ijdevneu.2010.07.230. [DOI] [PubMed] [Google Scholar]
- Dowling AL, Martz GU, Leonard JL, Zoeller RT. Acute changes in maternal thyroid hormone induce rapid and transient changes in gene expression in fetal rat brain. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2000;20:2255–2265. doi: 10.1523/JNEUROSCI.20-06-02255.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling AL, Zoeller RT. Thyroid hormone of maternal origin regulates the expression of RC3/neurogranin mRNA in the fetal rat brain. Brain research Molecular brain research. 2000;82:126–132. doi: 10.1016/s0169-328x(00)00190-x. [DOI] [PubMed] [Google Scholar]
- Duick DS, Warren DW, Nicoloff JT, Otis CL, Croxson MS. Effect of single dose dexamethasone on the concentration of serum triiodothyronine in man. The Journal of clinical endocrinology and metabolism. 1974;39:1151–1154. doi: 10.1210/jcem-39-6-1151. [DOI] [PubMed] [Google Scholar]
- Elder DA, Karayal AF, D'Ercole AJ, Calikoglu AS. Effects of hypothyroidism on insulin-like growth factor-I expression during brain development in mice. Neuroscience letters. 2000;293:99–102. doi: 10.1016/s0304-3940(00)01508-1. [DOI] [PubMed] [Google Scholar]
- Emerson CH, Seiler CM, Alex S, Fang SL, Mori Y, DeVito WJ. Gene expression and serum thyroxine-binding globulin are regulated by adrenal status and corticosterone in the rat. Endocrinology. 1993;133:1192–1196. doi: 10.1210/endo.133.3.8365361. [DOI] [PubMed] [Google Scholar]
- Faglia G, Ferrari C, Beck-Peccoz P, Spada A, Travaglini P, Ambrosi B. Reduced plasma thyrotropin response to thyrotropin releasing hormone after dexamethasone administration in normal subjects. Hormone and metabolic research = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 1973;5:289–292. doi: 10.1055/s-0028-1093930. [DOI] [PubMed] [Google Scholar]
- Farsetti A, Desvergne B, Hallenbeck P, Robbins J, Nikodem VM. Characterization of myelin basic protein thyroid hormone response element and its function in the context of native and heterologous promoter. The Journal of biological chemistry. 1992;267:15784–15788. [PubMed] [Google Scholar]
- Felber JP, Reddy WJ, Selenkow HA, Thorn GW. Adrenocortical response to the 48-hour ACTH test in myxedema and hyperthyroidism. The Journal of clinical endocrinology and metabolism. 1959;19:895–906. doi: 10.1210/jcem-19-8-895. [DOI] [PubMed] [Google Scholar]
- Ferraz AGo, del Rey FE, de Escobar GM, Innocenti GM, Berbel P. The development of the anterior commissure in normal and hypothyroid rats. Developmental Brain Research. 1994;81:293–308. doi: 10.1016/0165-3806(94)90315-8. [DOI] [PubMed] [Google Scholar]
- Finken MJ, van Eijsden M, Loomans EM, Vrijkotte TG, Rotteveel J. Maternal hypothyroxinemia in early pregnancy predicts reduced performance in reaction time tests in 5- to 6-year-old offspring. The Journal of clinical endocrinology and metabolism. 2013;98:1417–1426. doi: 10.1210/jc.2012-3389. [DOI] [PubMed] [Google Scholar]
- Forhead AJ, Curtis K, Kaptein E, Visser TJ, Fowden AL. Developmental Control of Iodothyronine Deiodinases by Cortisol in the Ovine Fetus and Placenta Near Term. Endocrinology. 2006;147:5988–5994. doi: 10.1210/en.2006-0712. [DOI] [PubMed] [Google Scholar]
- Forhead AJ, Jellyman JK, Gardner DS, Giussani DA, Kaptein E, Visser TJ, Fowden AL. Differential Effects of Maternal Dexamethasone Treatment on Circulating Thyroid Hormone Concentrations and Tissue Deiodinase Activity in the Pregnant Ewe and Fetus. Endocrinology. 2007;148:800–805. doi: 10.1210/en.2006-1194. [DOI] [PubMed] [Google Scholar]
- Fortier C, Delgado A, Ducommun P, Ducommun S, Dupont A, Jobin M, Kraicer J, MacIntosh-Hardt B, Marceau H, Mialhe P, Mialhe-Voloss C, Rerup C, Van Rees GP. Functional interrelationships between the adenohypophysis, thyroid, adrenal cortex and gonads. Canadian Medical Association journal. 1970;103:864–874. [PMC free article] [PubMed] [Google Scholar]
- Friedman MJ, Wang S, Jalowiec JE, McHugo GJ, McDonagh-Coyle A. Thyroid hormone alterations among women with posttraumatic stress disorder due to childhood sexual abuse. Biol Psychiatry. 2005;57:1186–1192. doi: 10.1016/j.biopsych.2005.01.019. [DOI] [PubMed] [Google Scholar]
- Friedman Y, Bacchus R, Raymond R, Joffe RT, Nobrega JN. Acute stress increases thyroid hormone levels in rat brain. Biological Psychiatry. 1999;45:234–237. doi: 10.1016/s0006-3223(98)00054-7. [DOI] [PubMed] [Google Scholar]
- Friesema EC, Grueters A, Biebermann H, Krude H, von Moers A, Reeser M, Barrett TG, Mancilla EE, Svensson J, Kester MH, Kuiper GG, Balkassmi S, Uitterlinden AG, Koehrle J, Rodien P, Halestrap AP, Visser TJ. Association between mutations in a thyroid hormone transporter and severe X-linked psychomotor retardation. Lancet. 2004;364:1435–1437. doi: 10.1016/S0140-6736(04)17226-7. [DOI] [PubMed] [Google Scholar]
- Geuze E, Vermetten E, Bremner JD. MR-based in vivo hippocampal volumetrics: 2. Findings in neuropsychiatric disorders. Mol Psychiatry. 2005;10:160–184. doi: 10.1038/sj.mp.4001579. [DOI] [PubMed] [Google Scholar]
- Ghassabian A, Bongers-Schokking JJ, de Rijke YB, van Mil N, Jaddoe VW, de Muinck Keizer-Schrama SM, Hooijkaas H, Hofman A, Visser W, Roman GC, Visser TJ, Verhulst FC, Tiemeier H. Maternal thyroid autoimmunity during pregnancy and the risk of attention deficit/hyperactivity problems in children: the Generation R Study. Thyroid : official journal of the American Thyroid Association. 2012;22:178–186. doi: 10.1089/thy.2011.0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghassabian A, Bongers-Schokking JJ, Henrichs J, Jaddoe VWV, Visser TJ, Visser W, de Muinck Keizer-Schrama SMPF, Hooijkaas H, Steegers EAP, Hofman A, Verhulst FC, van der Ende J, De Rijke YB, Tiemeier H. Maternal Thyroid Function During Pregnancy and Behavioral Problems in the Offspring: The Generation R Study. Pediatric research. 2011;69:454–459. doi: 10.1203/PDR.0b013e3182125b0c. [DOI] [PubMed] [Google Scholar]
- Ghassabian A, El Marroun H, Peeters RP, Jaddoe VW, Hofman A, Verhulst FC, Tiemeier H, White T. Downstream effects of maternal hypothyroxinemia in early pregnancy: nonverbal IQ and brain morphology in school-age children. The Journal of clinical endocrinology and metabolism. 2014a;99:2383–2390. doi: 10.1210/jc.2013-4281. [DOI] [PubMed] [Google Scholar]
- Ghassabian A, Steenweg-de Graaff J, Peeters RP, Ross HA, Jaddoe VW, Hofman A, Verhulst FC, White T, Tiemeier H. Maternal urinary iodine concentration in pregnancy and children's cognition: results from a population-based birth cohort in an iodine-sufficient area. BMJ open. 2014b;4:e005520. doi: 10.1136/bmjopen-2014-005520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert ME, Paczkowski C. Propylthiouracil (PTU)-induced hypothyroidism in the developing rat impairs synaptic transmission and plasticity in the dentate gyrus of the adult hippocampus. Developmental Brain Research. 2003;145:19–29. doi: 10.1016/s0165-3806(03)00191-3. [DOI] [PubMed] [Google Scholar]
- Gilbert ME, Ramos RL, McCloskey DP, Goodman JH. Subcortical band heterotopia in rat offspring following maternal hypothyroxinaemia: structural and functional characteristics. Journal of neuroendocrinology. 2014;26:528–541. doi: 10.1111/jne.12169. [DOI] [PubMed] [Google Scholar]
- Gilbert ME, Rovet J, Chen Z, Koibuchi N. Developmental thyroid hormone disruption: prevalence, environmental contaminants and neurodevelopmental consequences. Neurotoxicology. 2012;33:842–852. doi: 10.1016/j.neuro.2011.11.005. [DOI] [PubMed] [Google Scholar]
- Gilbert ME, Sui L. Dose-dependent reductions in spatial learning and synaptic function in the dentate gyrus of adult rats following developmental thyroid hormone insufficiency. Brain research. 2006;1069:10–22. doi: 10.1016/j.brainres.2005.10.049. [DOI] [PubMed] [Google Scholar]
- Gilbert ME, Sui L, Walker MJ, Anderson W, Thomas S, Smoller SN, Schon JP, Phani S, Goodman JH. Thyroid hormone insufficiency during brain development reduces parvalbumin immunoreactivity and inhibitory function in the hippocampus. Endocrinology. 2007;148:92–102. doi: 10.1210/en.2006-0164. [DOI] [PubMed] [Google Scholar]
- Glinoer D. The Regulation of Thyroid Function in Pregnancy: Pathways of Endocrine Adaptation from Physiology to Pathology. Endocrine reviews. 1997;18:404–433. doi: 10.1210/edrv.18.3.0300. [DOI] [PubMed] [Google Scholar]
- Glinoer D. The importance of iodine nutrition during pregnancy. Public health nutrition. 2007;10:1542–1546. doi: 10.1017/S1368980007360886. [DOI] [PubMed] [Google Scholar]
- Goldey ES, Kehn LS, Rehnberg GL, Crofton KM. Effects of Developmental Hypothyroidism on Auditory and Motor Function in the Rat. Toxicology and Applied Pharmacology. 1995;135:67–76. doi: 10.1006/taap.1995.1209. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Burgos G, Hashimoto T, Lewis DA. Alterations of cortical GABA neurons and network oscillations in schizophrenia. Current psychiatry reports. 2010;12:335–344. doi: 10.1007/s11920-010-0124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman JH, Gilbert ME. Modest thyroid hormone insufficiency during development induces a cellular malformation in the corpus callosum: a model of cortical dysplasia. Endocrinology. 2007;148:2593–2597. doi: 10.1210/en.2006-1276. [DOI] [PubMed] [Google Scholar]
- Gould E, Woolley CS, McEwen BS. The hippocampal formation: morphological changes induced by thyroid, gonadal and adrenal hormones. Psychoneuroendocrinology. 1991;16:67–84. doi: 10.1016/0306-4530(91)90071-z. [DOI] [PubMed] [Google Scholar]
- Grau G, Aguayo A, Vela A, Aniel-Quiroga A, Espada M, Miranda G, Martinez-Indart L, Martul P, Castaño L, Rica I. Normal intellectual development in children born from women with hypothyroxinemia during their pregnancy. Journal of Trace Elements in Medicine and Biology. 2015;31:18–24. doi: 10.1016/j.jtemb.2015.02.004. [DOI] [PubMed] [Google Scholar]
- Gross I, Dynia DW, Wilson CM, Ingleson LD, Gewolb IH, Rooney SA. Glucocorticoid-thyroid hormone interactions in fetal rat lung. Pediatric research. 1984;18:191–196. doi: 10.1203/00006450-198402000-00017. [DOI] [PubMed] [Google Scholar]
- Guadano-Ferraz A, Benavides-Piccione R, Venero C, Lancha C, Vennstrom B, Sandi C, DeFelipe J, Bernal J. Lack of thyroid hormone receptor [alpha]1 is associated with selective alterations in behavior and hippocampal circuits. Mol Psychiatry. 2003;8:30–38. doi: 10.1038/sj.mp.4001196. [DOI] [PubMed] [Google Scholar]
- Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, O'Heir CE, Mitchell ML, Hermos RJ, Waisbren SE, Faix JD, Klein RZ. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. The New England journal of medicine. 1999;341:549–555. doi: 10.1056/NEJM199908193410801. [DOI] [PubMed] [Google Scholar]
- Hage MP, Azar ST. The Link between Thyroid Function and Depression. Journal of thyroid research. 2012;2012:590648. doi: 10.1155/2012/590648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartoft-Nielsen ML, Boas M, Bliddal S, Rasmussen AK, Main K, Feldt-Rasmussen U. Do Thyroid Disrupting Chemicals Influence Foetal Development during Pregnancy? Journal of thyroid research. 2011;2011:342189. doi: 10.4061/2011/342189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasegawa M, Wada H. Developmental hypothyroidism disrupts visual signal detection performance in rats. Physiology & behavior. 2013;112-113:90–95. doi: 10.1016/j.physbeh.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Hashimoto K, Curty FH, Borges PP, Lee CE, Abel ED, Elmquist JK, Cohen RN, Wondisford FE. An unliganded thyroid hormone receptor causes severe neurological dysfunction. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:3998–4003. doi: 10.1073/pnas.051454698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser P, Zametkin AJ, Martinez P, Vitiello B, Matochik JA, Mixson JA, Weintraub BD. Attention Deficit-Hyperactivity Disorder in People with Generalized Resistance to Thyroid Hormone. New England Journal of Medicine. 1993;328:997–1001. doi: 10.1056/NEJM199304083281403. [DOI] [PubMed] [Google Scholar]
- Haviland MG, Sonne JL, Anderson DL, Nelson JC, Sheridan-Matney C, Nichols JG, Carlton EI, Murdoch WG. Thyroid hormone levels and psychological symptoms in sexually abused adolescent girls. Child abuse & neglect. 2006;30:589–598. doi: 10.1016/j.chiabu.2005.11.011. [DOI] [PubMed] [Google Scholar]
- Hellman L, Bradlow HL, Zumoff B, Gallagher TF. The influence of thyroid hormone on hydrocortisone production and metabolism. The Journal of clinical endocrinology and metabolism. 1961;21:1231–1247. doi: 10.1210/jcem-21-10-1231. [DOI] [PubMed] [Google Scholar]
- Hellstrom IC, Dhir SK, Diorio JC, Meaney MJ. Maternal licking regulates hippocampal glucocorticoid receptor transcription through a thyroid hormone–serotonin–NGFI-A signalling cascade. Philosophical Transactions of the Royal Society B: Biological Sciences. 2012;367:2495–2510. doi: 10.1098/rstb.2012.0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmreich DL, Crouch M, Dorr NP, Parfitt DB. Peripheral triiodothyronine (T3) levels during escapable and inescapable footshock. Physiology & behavior. 2006;87:114–119. doi: 10.1016/j.physbeh.2005.09.010. [DOI] [PubMed] [Google Scholar]
- Helmreich DL, Parfitt DB, Lu XY, Akil H, Watson SJ. Relation between the hypothalamic-pituitary-thyroid (HPT) axis and the hypothalamic-pituitary-adrenal (HPA) axis during repeated stress. Neuroendocrinology. 2005;81:183–192. doi: 10.1159/000087001. [DOI] [PubMed] [Google Scholar]
- Helmreich DL, Tylee D. Thyroid hormone regulation by stress and behavioral differences in adult male rats. Hormones and Behavior. 2011;60:284–291. doi: 10.1016/j.yhbeh.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henley WN, Koehnle TJ. Thyroid hormones and the treatment of depression: An examination of basic hormonal actions in the mature mammalian brain. Synapse. 1997;27:36–44. doi: 10.1002/(SICI)1098-2396(199709)27:1<36::AID-SYN4>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Henrichs J, Bongers-Schokking JJ, Schenk JJ, Ghassabian A, Schmidt HG, Visser TJ, Hooijkaas H, de Muinck Keizer-Schrama SM, Hofman A, Jaddoe VV, Visser W, Steegers EA, Verhulst FC, de Rijke YB, Tiemeier H. Maternal thyroid function during early pregnancy and cognitive functioning in early childhood: the generation R study. The Journal of clinical endocrinology and metabolism. 2010;95:4227–4234. doi: 10.1210/jc.2010-0415. [DOI] [PubMed] [Google Scholar]
- Heuer H, Maier MK, Iden S, Mittag J, Friesema EC, Visser TJ, Bauer K. The monocarboxylate transporter 8 linked to human psychomotor retardation is highly expressed in thyroid hormone-sensitive neuron populations. Endocrinology. 2005;146:1701–1706. doi: 10.1210/en.2004-1179. [DOI] [PubMed] [Google Scholar]
- Heyland A, Moroz LL. Cross-kingdom hormonal signaling: an insight from thyroid hormone functions in marine larvae. The Journal of experimental biology. 2005;208:4355–4361. doi: 10.1242/jeb.01877. [DOI] [PubMed] [Google Scholar]
- Hidal JT, Kaplan MM. Inhibition of thyroxine 5′-deiodination type II in cultured human placental cells by cortisol, insulin, 3′, 5′-cyclic adenosine monophosphate, and butyrate. Metabolism: clinical and experimental. 1988;37:664–668. doi: 10.1016/0026-0495(88)90087-x. [DOI] [PubMed] [Google Scholar]
- Hoerder-Suabedissen A, Molnar Z. Development, evolution and pathology of neocortical subplate neurons. Nat Rev Neurosci. 2015;16:133–146. doi: 10.1038/nrn3915. [DOI] [PubMed] [Google Scholar]
- Hoppner W, Sussmuth W, O'Brien C, Seitz HJ. Cooperative effect of thyroid and glucocorticoid hormones on the induction of hepatic phosphoenolpyruvate carboxykinase in vivo and in cultured hepatocytes. European journal of biochemistry / FEBS. 1986;159:399–405. doi: 10.1111/j.1432-1033.1986.tb09882.x. [DOI] [PubMed] [Google Scholar]
- Hoshiro M, Ohno Y, Masaki H, Iwase H, Aoki N. Comprehensive study of urinary cortisol metabolites in hyperthyroid and hypothyroid patients. Clinical endocrinology. 2006;64:37–45. doi: 10.1111/j.1365-2265.2005.02412.x. [DOI] [PubMed] [Google Scholar]
- Ibarrola N, Rodriguez-Pena A. Hypothyroidism coordinately and transiently affects myelin protein gene expression in most rat brain regions during postnatal development. Brain research. 1997;752:285–293. doi: 10.1016/s0006-8993(96)01480-1. [DOI] [PubMed] [Google Scholar]
- Ichikawa Y, Yoshida K, Kawagoe M, Saito E, Abe Y, Arikawa K, Homma M. Altered equilibrium between cortisol and cortisone in plasma in thyroid dysfunction and inflammatory diseases. Metabolism: clinical and experimental. 1977;26:989–997. doi: 10.1016/0026-0495(77)90016-6. [DOI] [PubMed] [Google Scholar]
- Iglesias T, Caubin J, Stunnenberg HG, Zaballos A, Bernal J, Munoz A. Thyroid hormone-dependent transcriptional repression of neural cell adhesion molecule during brain maturation. The EMBO journal. 1996;15:4307–4316. [PMC free article] [PubMed] [Google Scholar]
- Iranmanesh A, Lizarralde G, Johnson ML, Veldhuis JD. Dynamics of 24-hour endogenous cortisol secretion and clearance in primary hypothyroidism assessed before and after partial thyroid hormone replacement. The Journal of clinical endocrinology and metabolism. 1990;70:155–161. doi: 10.1210/jcem-70-1-155. [DOI] [PubMed] [Google Scholar]
- Jackson IM. The thyroid axis and depression. Thyroid : official journal of the American Thyroid Association. 1998;8:951–956. doi: 10.1089/thy.1998.8.951. [DOI] [PubMed] [Google Scholar]
- Jahagirdar V, Zoeller TR, Tighe DP, Wagner CK. Maternal hypothyroidism decreases progesterone receptor expression in the cortical subplate of fetal rat brain. Journal of neuroendocrinology. 2012 doi: 10.1111/j.1365-2826.2012.02318.x. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Calogero AE, Konstandi M, Kamilaris TC, La Vignera S, Chrousos GP. Effects of experimentally induced hyperthyroidism on central hypothalamic-pituitary-adrenal axis function in rats: in vitro and in situ studies. Pituitary. 2013;16:275–286. doi: 10.1007/s11102-012-0417-5. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Kamilaris TC, Calogero AE, Gold PW, Chrousos GP. Experimentally-induced hyperthyroidism is associated with activation of the rat hypothalamic-pituitary-adrenal axis. European journal of endocrinology / European Federation of Endocrine Societies. 2005;153:177–185. doi: 10.1530/eje.1.01923. [DOI] [PubMed] [Google Scholar]
- Julvez J, Alvarez-Pedrerol M, Rebagliato M, Murcia M, Forns J, Garcia-Esteban R, Lertxundi N, Espada M, Tardon A, Riano Galan I, Sunyer J. Thyroxine levels during pregnancy in healthy women and early child neurodevelopment. Epidemiology. 2013;24:150–157. doi: 10.1097/EDE.0b013e318276ccd3. [DOI] [PubMed] [Google Scholar]
- Kamilaris TC, DeBold CR, Johnson EO, Mamalaki E, Listwak SJ, Calogero AE, Kalogeras KT, Gold PW, Orth DN. Effects of short and long duration hypothyroidism and hyperthyroidism on the plasma adrenocorticotropin and corticosterone responses to ovine corticotropin-releasing hormone in rats. Endocrinology. 1991;128:2567–2576. doi: 10.1210/endo-128-5-2567. [DOI] [PubMed] [Google Scholar]
- Kanold PO, Luhmann HJ. The subplate and early cortical circuits. Annual review of neuroscience. 2010;33:23–48. doi: 10.1146/annurev-neuro-060909-153244. [DOI] [PubMed] [Google Scholar]
- Kenny FM, Iturzaeta N, Preeyasombat C, Taylor FH, Migeon CJ. Cortisol production rate. VII. Hypothyroidism and hyperthyroidism in infants and children. The Journal of clinical endocrinology and metabolism. 1967;27:1616–1622. doi: 10.1210/jcem-27-11-1616. [DOI] [PubMed] [Google Scholar]
- Kester MH, Martinez de Mena R, Obregon MJ, Marinkovic D, Howatson A, Visser TJ, Hume R, Morreale de Escobar G. Iodothyronine levels in the human developing brain: major regulatory roles of iodothyronine deiodinases in different areas. The Journal of clinical endocrinology and metabolism. 2004;89:3117–3128. doi: 10.1210/jc.2003-031832. [DOI] [PubMed] [Google Scholar]
- Kilburn-Watt E, Banati RB, Keay KA. Altered Thyroid Hormones and Behavioural Change in a Sub-Population of Rats Following Chronic Constriction Injury. Journal of neuroendocrinology. 2010;22:960–970. doi: 10.1111/j.1365-2826.2010.02038.x. [DOI] [PubMed] [Google Scholar]
- Kim B. Thyroid hormone as a determinant of energy expenditure and the basal metabolic rate. Thyroid : official journal of the American Thyroid Association. 2008;18:141–144. doi: 10.1089/thy.2007.0266. [DOI] [PubMed] [Google Scholar]
- Kioukia N, Bekris S, Antoniou K, Papadopoulou-Daifoti Z, Christofidis I. Effects of chronic mild stress (CMS) on thyroid hormone function in two rat strains. Psychoneuroendocrinology. 2000;25:247–257. doi: 10.1016/s0306-4530(99)00051-7. [DOI] [PubMed] [Google Scholar]
- Klein RZ, Sargent JD, Larsen PR, Waisbren SE, Haddow JE, Mitchell ML. Relation of severity of maternal hypothyroidism to cognitive development of offspring. Journal of medical screening. 2001;8:18–20. doi: 10.1136/jms.8.1.18. [DOI] [PubMed] [Google Scholar]
- Klieverik LP, Coomans CP, Endert E, Sauerwein HP, Havekes LM, Voshol PJ, Rensen PCN, Romijn JA, Kalsbeek A, Fliers E. Thyroid Hormone Effects on Whole-Body Energy Homeostasis and Tissue-Specific Fatty Acid Uptake in Vivo. Endocrinology. 2009;150:5639–5648. doi: 10.1210/en.2009-0297. [DOI] [PubMed] [Google Scholar]
- Koibuchi N, Fukuda H, Chin WW. Promoter-specific regulation of the brain-derived neurotropic factor gene by thyroid hormone in the developing rat cerebellum. Endocrinology. 1999;140:3955–3961. doi: 10.1210/endo.140.9.6997. [DOI] [PubMed] [Google Scholar]
- Kooistra L, Crawford S, van Baar AL, Brouwers EP, Pop VJ. Neonatal effects of maternal hypothyroxinemia during early pregnancy. Pediatrics. 2006;117:161–167. doi: 10.1542/peds.2005-0227. [DOI] [PubMed] [Google Scholar]
- Korevaar TIM, Medici M, Rijke YBd, Visser W, Keizer-Schrama SMPFdM, Jaddoe VWV, Hofman A, Ross HA, Visser WE, Hooijkaas H, Steegers EAP, Tiemeier H, Bongers-Schokking JJ, Visser TJ, Peeters RP. Ethnic Differences in Maternal Thyroid Parameters during Pregnancy: The Generation R Study. The Journal of Clinical Endocrinology & Metabolism. 2013;98:3678–3686. doi: 10.1210/jc.2013-2005. [DOI] [PubMed] [Google Scholar]
- Kriegstein AR, Noctor SC. Patterns of neuronal migration in the embryonic cortex. Trends in neurosciences. 2004;27:392–399. doi: 10.1016/j.tins.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Kunz S, Spirig M, Ginsburg C, Buchstaller A, Berger P, Lanz R, Rader C, Vogt L, Kunz B, Sonderegger P. Neurite fasciculation mediated by complexes of axonin-1 and Ng cell adhesion molecule. The Journal of cell biology. 1998;143:1673–1690. doi: 10.1083/jcb.143.6.1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurian MA, Jungbluth H. Genetic disorders of thyroid metabolism and brain development. Developmental Medicine & Child Neurology. 2014;56:627–634. doi: 10.1111/dmcn.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer P, Foldes O, Kvetnansky R, Culman J, Torda T, El Daher F. Pituitary-thyroid function during acute immobilization stress in rats. Experimental and clinical endocrinology. 1983;82:51–60. doi: 10.1055/s-0029-1210255. [DOI] [PubMed] [Google Scholar]
- Lazarus JH. Iodine Status in Europe in 2014. European Thyroid Journal. 2014;3:3–6. doi: 10.1159/000358873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus JH, Bestwick JP, Channon S, Paradice R, Maina A, Rees R, Chiusano E, John R, Guaraldo V, George LM, Perona M, Dall'Amico D, Parkes AB, Joomun M, Wald NJ. Antenatal thyroid screening and childhood cognitive function. The New England journal of medicine. 2012;366:493–501. doi: 10.1056/NEJMoa1106104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leers J, Steiner C, Renkawitz R, Muller M. A thyroid hormone receptor-dependent glucocorticoid induction. Molecular endocrinology. 1994;8:440–447. doi: 10.1210/mend.8.4.8052265. [DOI] [PubMed] [Google Scholar]
- Lengvari I, Branch BJ, Taylor AN. The effect of perinatal thyroxine treatment on the development of the plasma corticosterone diurnal rhythm. Neuroendocrinology. 1977;24:65–73. doi: 10.1159/000122697. [DOI] [PubMed] [Google Scholar]
- Leung AM, Pearce EN, Braverman LE. Sufficient iodine intake during pregnancy: just do it. Thyroid : official journal of the American Thyroid Association. 2013;23:7–8. doi: 10.1089/thy.2012.0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Shan Z, Teng W, Yu X, Li Y, Fan C, Teng X, Guo R, Wang H, Li J, Chen Y, Wang W, Chawinga M, Zhang L, Yang L, Zhao Y, Hua T. Abnormalities of maternal thyroid function during pregnancy affect neuropsychological development of their children at 25-30 months. Clinical endocrinology. 2010;72:825–829. doi: 10.1111/j.1365-2265.2009.03743.x. [DOI] [PubMed] [Google Scholar]
- Lindholm D, Castren E, Tsoulfas P, Kolbeck R, Berzaghi Mda P, Leingartner A, Heisenberg CP, Tessarollo L, Parada LF, Thoenen H. Neurotrophin-3 induced by tri-iodothyronine in cerebellar granule cells promotes Purkinje cell differentiation. The Journal of cell biology. 1993;122:443–450. doi: 10.1083/jcb.122.2.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C-r, Miao J, Zhang Y-l, Liu Y-m, Yu B-g. Effects of Hypothyroidism on Expression of CRMP2B and ARPC5 during Development of the Rat Frontal Cortex. International Journal of Biological Sciences. 2013;9:209–218. doi: 10.7150/ijbs.5646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loosen PT. The TRH-induced TSH response in psychiatric patients: a possible neuroendocrine marker. Psychoneuroendocrinology. 1985;10:237–260. doi: 10.1016/0306-4530(85)90002-2. [DOI] [PubMed] [Google Scholar]
- Lopez-Espindola D, Morales-Bastos C, Grijota-Martinez C, Liao XH, Lev D, Sugo E, Verge CF, Refetoff S, Bernal J, Guadano-Ferraz A. Mutations of the thyroid hormone transporter MCT8 cause prenatal brain damage and persistent hypomyelination. The Journal of clinical endocrinology and metabolism. 2014;99:E2799–2804. doi: 10.1210/jc.2014-2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loubiere LS, Vasilopoulou E, Glazier JD, Taylor PM, Franklyn JA, Kilby MD, Chan SY. Expression and function of thyroid hormone transporters in the microvillous plasma membrane of human term placental syncytiotrophoblast. Endocrinology. 2012;153:6126–6135. doi: 10.1210/en.2012-1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhmann HJ, Kilb W, Hanganu-Opatz IL. Subplate cells: amplifiers of neuronal activity in the developing cerebral cortex. Frontiers in neuroanatomy. 2009;3:19. doi: 10.3389/neuro.05.019.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manojlović-Stojanoski M, Nestorović N, Ristić N, Trifunović S, Filipović B, Šošić-Jurjević B, Sekulić M. Unbiased stereological estimation of the rat fetal pituitary volume and of the total number and volume of TSH cells after maternal dexamethasone application. Microscopy Research and Technique. 2010;73:1077–1085. doi: 10.1002/jemt.20842. [DOI] [PubMed] [Google Scholar]
- Manojlovic-Stojanoski MN, Filipovic BR, Nestorovic NM, Sosic-Jurjevic BT, Ristic NM, Trifunovic SL, Milosevic V. Morpho-functional characteristics of rat fetal thyroid gland are affected by prenatal dexamethasone exposure. Steroids. 2014;84:22–29. doi: 10.1016/j.steroids.2014.03.006. [DOI] [PubMed] [Google Scholar]
- Manzano J, Cuadrado M, Morte B, Bernal J. Influence of thyroid hormone and thyroid hormone receptors in the generation of cerebellar gamma-aminobutyric acid-ergic interneurons from precursor cells. Endocrinology. 2007;148:5746–5751. doi: 10.1210/en.2007-0567. [DOI] [PubMed] [Google Scholar]
- Martial JA, Seeburg PH, Guenzi D, Goodman HM, Baxter JD. Regulation of growth hormone gene expression: synergistic effects of thyroid and glucocorticoid hormones. Proceedings of the National Academy of Sciences of the United States of America. 1977;74:4293–4295. doi: 10.1073/pnas.74.10.4293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinho A, Gonçalves I, Costa M, Santos CR. Stress and Glucocorticoids Increase Transthyretin Expression in Rat Choroid Plexus via Mineralocorticoid and Glucocorticoid Receptors. J Mol Neurosci. 2012;48:1–13. doi: 10.1007/s12031-012-9715-7. [DOI] [PubMed] [Google Scholar]
- McCarrison R. Observations on Endemic Cretinism in the Chitral and Gilgit Valleys. Proceedings of the Royal Society of Medicine. 1909;2:1–36. doi: 10.1177/003591570900200601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod DSA, McIntyre HD. Subclinical hypothyroidism and related biochemical entities in pregnancy: implications and management. Obstetric Medicine. 2010;3:139–144. doi: 10.1258/om.2010.100023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meaney MJ, Aitken DH, Sapolsky RM. Thyroid hormones influence the development of hippocampal glucocorticoid receptors in the rat: a mechanism for the effects of postnatal handling on the development of the adrenocortical stress response. Neuroendocrinology. 1987;45:278–283. doi: 10.1159/000124741. [DOI] [PubMed] [Google Scholar]
- Meaney MJ, Diorio J, Francis D, Weaver S, Yau J, Chapman K, Seckl JR. Postnatal handling increases the expression of cAMP-inducible transcription factors in the rat hippocampus: the effects of thyroid hormones and serotonin. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2000;20:3926–3935. doi: 10.1523/JNEUROSCI.20-10-03926.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medici M, Visser WE, Visser TJ, Peeters RP. Genetic determination of the hypothalamic-pituitary-thyroid axis: where do we stand? Endocrine reviews. 2015;36:214–244. doi: 10.1210/er.2014-1081. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological bulletin. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Modesto T, Tiemeier H, Peeters RP, Jaddoe VW, Hofman A, Verhulst FC, Ghassabian A. Maternal Mild Thyroid Hormone Insufficiency in Early Pregnancy and Attention-Deficit/Hyperactivity Disorder Symptoms in Children. JAMA pediatrics. 2015 doi: 10.1001/jamapediatrics.2015.0498. [DOI] [PubMed] [Google Scholar]
- Mohan V, Sinha RA, Pathak A, Rastogi L, Kumar P, Pal A, Godbole MM. Maternal thyroid hormone deficiency affects the fetal neocorticogenesis by reducing the proliferating pool, rate of neurogenesis and indirect neurogenesis. Experimental neurology. 2012;237:477–488. doi: 10.1016/j.expneurol.2012.07.019. [DOI] [PubMed] [Google Scholar]
- Moleti M, Trimarchi F, Vermiglio F. Doubts and Concerns about Isolated Maternal Hypothyroxinemia. Journal of thyroid research. 2011;2011:463029. doi: 10.4061/2011/463029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moleti M, Trimarchi F, Vermiglio F. Thyroid physiology in pregnancy. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2014;20:589–596. doi: 10.4158/EP13341.RA. [DOI] [PubMed] [Google Scholar]
- Morte B, Diez D, Auso E, Belinchon MM, Gil-Ibanez P, Grijota-Martinez C, Navarro D, de Escobar GM, Berbel P, Bernal J. Thyroid hormone regulation of gene expression in the developing rat fetal cerebral cortex: prominent role of the Ca2+/calmodulin-dependent protein kinase IV pathway. Endocrinology. 2010;151:810–820. doi: 10.1210/en.2009-0958. [DOI] [PubMed] [Google Scholar]
- Murcia M, Rebagliato M, Iniguez C, Lopez-Espinosa MJ, Estarlich M, Plaza B, Barona-Vilar C, Espada M, Vioque J, Ballester F. Effect of iodine supplementation during pregnancy on infant neurodevelopment at 1 year of age. American journal of epidemiology. 2011;173:804–812. doi: 10.1093/aje/kwq424. [DOI] [PubMed] [Google Scholar]
- Nagy Z, Westerberg H, Klingberg T. Maturation of white matter is associated with the development of cognitive functions during childhood. Journal of cognitive neuroscience. 2004;16:1227–1233. doi: 10.1162/0898929041920441. [DOI] [PubMed] [Google Scholar]
- Navarro D, Alvarado M, Morte B, Berbel D, Sesma J, Pacheco P, Morreale de Escobar G, Bernal J, Berbel P. Late maternal hypothyroidism alters the expression of Camk4 in neocortical subplate neurons: a comparison with Nurr1 labeling. Cereb Cortex. 2014;24:2694–2706. doi: 10.1093/cercor/bht129. [DOI] [PubMed] [Google Scholar]
- Negishi T, Kawasaki K, Sekiguchi S, Ishii Y, Kyuwa S, Kuroda Y, Yoshikawa Y. Attention-deficit and hyperactive neurobehavioural characteristics induced by perinatal hypothyroidism in rats. Behavioural brain research. 2005;159:323–331. doi: 10.1016/j.bbr.2004.11.012. [DOI] [PubMed] [Google Scholar]
- O'Donnell K, O'Connor TG, Glover V. Prenatal stress and neurodevelopment of the child: focus on the HPA axis and role of the placenta. Developmental neuroscience. 2009;31:285–292. doi: 10.1159/000216539. [DOI] [PubMed] [Google Scholar]
- Oken E, Braverman LE, Platek D, Mitchell ML, Lee SL, Pearce EN. Neonatal thyroxine, maternal thyroid function, and child cognition. The Journal of clinical endocrinology and metabolism. 2009;94:497–503. doi: 10.1210/jc.2008-0936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M, Guzelcan Y, de Vries GJ, Assies J, Gersons BP. HPA- and HPT-axis alterations in chronic posttraumatic stress disorder. Psychoneuroendocrinology. 2006;31:1220–1230. doi: 10.1016/j.psyneuen.2006.09.003. [DOI] [PubMed] [Google Scholar]
- Opazo MC, Gianini A, Pancetti F, Azkcona G, Alarcon L, Lizana R, Noches V, Gonzalez PA, Marassi MP, Mora S, Rosenthal D, Eugenin E, Naranjo D, Bueno SM, Kalergis AM, Riedel CA. Maternal hypothyroxinemia impairs spatial learning and synaptic nature and function in the offspring. Endocrinology. 2008;149:5097–5106. doi: 10.1210/en.2008-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakkila F, Mannisto T, Pouta A, Hartikainen AL, Ruokonen A, Surcel HM, Bloigu A, Vaarasmaki M, Jarvelin MR, Moilanen I, Suvanto E. The impact of gestational thyroid hormone concentrations on ADHD symptoms of the child. The Journal of clinical endocrinology and metabolism. 2014;99:E1–8. doi: 10.1210/jc.2013-2943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel J, Landers K, Li H, Mortimer RH, Richard K. Thyroid hormones and fetal neurological development. The Journal of endocrinology. 2011;209:1–8. doi: 10.1530/JOE-10-0444. [DOI] [PubMed] [Google Scholar]
- Pathak A, Sinha RA, Mohan V, Mitra K, Godbole MM. Maternal thyroid hormone before the onset of fetal thyroid function regulates reelin and downstream signaling cascade affecting neocortical neuronal migration. Cereb Cortex. 2011;21:11–21. doi: 10.1093/cercor/bhq052. [DOI] [PubMed] [Google Scholar]
- Perretti M, D'Acquisto F. Annexin A1 and glucocorticoids as effectors of the resolution of inflammation. Nat Rev Immunol. 2009;9:62–70. doi: 10.1038/nri2470. [DOI] [PubMed] [Google Scholar]
- Pharoah PO, Connolly KJ, Ekins RP, Harding AG. Maternal thyroid hormone levels in pregnancy and the subsequent cognitive and motor performance of the children. Clinical endocrinology. 1984;21:265–270. doi: 10.1111/j.1365-2265.1984.tb03468.x. [DOI] [PubMed] [Google Scholar]
- Pinna G, Broedel O, Eravci M, Stoltenburg-Didinger G, Plueckhan H, Fuxius S, Meinhold H, Baumgartner A. Thyroid hormones in the rat amygdala as common targets for antidepressant drugs, mood stabilizers, and sleep deprivation. Biol Psychiatry. 2003;54:1049–1059. doi: 10.1016/s0006-3223(03)00414-1. [DOI] [PubMed] [Google Scholar]
- Pizzagalli F, Hagenbuch B, Stieger B, Klenk U, Folkers G, Meier PJ. Identification of a novel human organic anion transporting polypeptide as a high affinity thyroxine transporter. Molecular endocrinology. 2002;16:2283–2296. doi: 10.1210/me.2001-0309. [DOI] [PubMed] [Google Scholar]
- Poland RE, Weichsel ME, Jr., Rubin RT. Postnatal maturation patterns of serum corticosterone and growth hormone in rats: effect of chronic thyroxine administration. Hormone and metabolic research = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 1979;11:222–227. doi: 10.1055/s-0028-1092713. [DOI] [PubMed] [Google Scholar]
- Pop VJ, Brouwers EP, Vader HL, Vulsma T, van Baar AL, de Vijlder JJ. Maternal hypothyroxinaemia during early pregnancy and subsequent child development: a 3-year follow-up study. Clinical endocrinology. 2003;59:282–288. doi: 10.1046/j.1365-2265.2003.01822.x. [DOI] [PubMed] [Google Scholar]
- Pop VJ, de Vries E, van Baar AL, Waelkens JJ, de Rooy HA, Horsten M, Donkers MM, Komproe IH, van Son MM, Vader HL. Maternal thyroid peroxidase antibodies during pregnancy: a marker of impaired child development? The Journal of Clinical Endocrinology & Metabolism. 1995;80:3561–3566. doi: 10.1210/jcem.80.12.8530599. [DOI] [PubMed] [Google Scholar]
- Pop VJ, Kuijpens JL, van Baar AL, Verkerk G, van Son MM, de Vijlder JJ, Vulsma T, Wiersinga WM, Drexhage HA, Vader HL. Low maternal free thyroxine concentrations during early pregnancy are associated with impaired psychomotor development in infancy. Clinical endocrinology. 1999;50:149–155. doi: 10.1046/j.1365-2265.1999.00639.x. [DOI] [PubMed] [Google Scholar]
- Prengel H, Brodel O, Hiedra L, Pinna G, Eravci M, Meinhold H, Baumgartner A. Effects of tranylcypromine on thyroid hormone metabolism and concentrations in rat brain. Neuropharmacology. 2000;39:99–109. doi: 10.1016/s0028-3908(99)00077-5. [DOI] [PubMed] [Google Scholar]
- Qiu R, Wang J, Tsark W, Lu Q. Essential role of PDZ-RGS3 in the maintenance of neural progenitor cells. Stem cells (Dayton, Ohio) 2010;28:1602–1610. doi: 10.1002/stem.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quignodon L, Legrand C, Allioli N, Guadaño-Ferraz A, Bernal J, Samarut J, Flamant F. Thyroid hormone signaling is highly heterogeneous during pre- and postnatal brain development. Journal of Molecular Endocrinology. 2004;33:467–476. doi: 10.1677/jme.1.01570. [DOI] [PubMed] [Google Scholar]
- Rakic P. Evolution of the neocortex: a perspective from developmental biology. Nat Rev Neurosci. 2009;10:724–735. doi: 10.1038/nrn2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakic P, Caviness VS., Jr Cortical development: View from neurological mutants two decades later. Neuron. 1995;14:1101–1104. doi: 10.1016/0896-6273(95)90258-9. [DOI] [PubMed] [Google Scholar]
- Rami A, Patel AJ, Rabié A. Thyroid hormone and development of the rat hippocampus: Morphological alterations in granule and pyramidal cells. Neuroscience. 1986;19:1217–1226. doi: 10.1016/0306-4522(86)90135-1. [DOI] [PubMed] [Google Scholar]
- Reid RE, Kim E-M, Page D, O'Mara SM, O'Hare E. Thyroxine replacement in an animal model of congenital hypothyroidism. Physiology & behavior. 2007;91:299–303. doi: 10.1016/j.physbeh.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Robichaux MA, Cowan CW. Signaling Mechanisms of Axon Guidance and Early Synaptogenesis. In: Andersen SL, Pine DS, editors. The Neurobiology of Childhood. Springer; Berlin: 2014. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Pena A. Oligodendrocyte development and thyroid hormone. Journal of neurobiology. 1999;40:497–512. doi: 10.1002/(sici)1097-4695(19990915)40:4<497::aid-neu7>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Pena A, Ibarrola N, Iniguez MA, Munoz A, Bernal J. Neonatal hypothyroidism affects the timely expression of myelin-associated glycoprotein in the rat brain. The Journal of clinical investigation. 1993;91:812–818. doi: 10.1172/JCI116301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez T, Albuquerque-Araujo WI, Reis LC, Antunes-Rodrigues J, Ramalho MJ. Hypothyroidism attenuates stress-induced prolactin and corticosterone release in septic rats. Experimental physiology. 2003;88:755–760. doi: 10.1113/eph8802621. [DOI] [PubMed] [Google Scholar]
- Roman GC, Ghassabian A, Bongers-Schokking JJ, Jaddoe VW, Hofman A, de Rijke YB, Verhulst FC, Tiemeier H. Association of gestational maternal hypothyroxinemia and increased autism risk. Annals of neurology. 2013;74:733–742. doi: 10.1002/ana.23976. [DOI] [PubMed] [Google Scholar]
- Ruel J, Faure R, Dussault JH. Regional distribution of nuclear T3 receptors in rat brain and evidence for preferential localization in neurons. Journal of endocrinological investigation. 1985;8:343–348. doi: 10.1007/BF03348511. [DOI] [PubMed] [Google Scholar]
- Ruiz-Marcos A, Sanchez-Toscano F, Obregon MJ, Del Rey FE, De Escobar GM. Thyroxine treatment and recovery of hypothyroidism-induced pyramidal cell damage. Brain research. 1982;239:559–574. doi: 10.1016/0006-8993(82)90530-3. [DOI] [PubMed] [Google Scholar]
- Samadi A, Skocic J, Rovet JF. Children born to women treated for hypothyroidism during pregnancy show abnormal corpus callosum development. Thyroid : official journal of the American Thyroid Association. 2015;25:494–502. doi: 10.1089/thy.2014.0548. [DOI] [PubMed] [Google Scholar]
- Samuels HH, Horwitz ZD, Stanley F, Casanova J, Shapiro LE. Thyroid hormone controls glucocorticoid action in cultured GH1 cells. Nature. 1977;268:254–257. doi: 10.1038/268254a0. [DOI] [PubMed] [Google Scholar]
- Santiago P, Velasco I, Muela JA, Sanchez B, Martinez J, Rodriguez A, Berrio M, Gutierrez-Repiso C, Carreira M, Moreno A, Garcia-Fuentes E, Soriguer F. Infant neurocognitive development is independent of the use of iodised salt or iodine supplements given during pregnancy. The British journal of nutrition. 2013;110:831–839. doi: 10.1017/S0007114512005880. [DOI] [PubMed] [Google Scholar]
- Sawano E, Takahashi M, Negishi T, Tashiro T. Thyroid hormone-dependent development of the GABAergic pre- and post-synaptic components in the rat hippocampus. International journal of developmental neuroscience : the official journal of the International Society for Developmental Neuroscience. 2013;31:751–761. doi: 10.1016/j.ijdevneu.2013.09.007. [DOI] [PubMed] [Google Scholar]
- Servatius RJ, Natelson BH, Moldow R, Pogach L, Brennan FX, Ottenweller JE. Persistent Neuroendocrine Changes in Multiple Hormonal Axes after a Single or Repeated Stressor Exposures. Stress. 2000;3:263–274. doi: 10.3109/10253890009001132. [DOI] [PubMed] [Google Scholar]
- Shi ZX, Levy A, Lightman SL. Thyroid hormone-mediated regulation of corticotropin-releasing hormone messenger ribonucleic acid in the rat. Endocrinology. 1994;134:1577–1580. doi: 10.1210/endo.134.3.8119200. [DOI] [PubMed] [Google Scholar]
- Shields BM, Knight BA, Hill A, Hattersley AT, Vaidya B. Fetal Thyroid Hormone Level at Birth Is Associated with Fetal Growth. The Journal of clinical endocrinology and metabolism. 2011;96:E934–E938. doi: 10.1210/jc.2010-2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimokawa N, Yousefi B, Morioka S, Yamaguchi S, Ohsawa A, Hayashi H, Azuma A, Mizuno H, Kasagi M, Masuda H, Jingu H, Furudate SI, Haijima A, Takatsuru Y, Iwasaki T, Umezu M, Koibuchi N. Altered cerebellum development and dopamine distribution in a rat genetic model with congenital hypothyroidism. Journal of neuroendocrinology. 2014;26:164–175. doi: 10.1111/jne.12135. [DOI] [PubMed] [Google Scholar]
- Siesser WB, Zhao J, Miller LR, Cheng SY, McDonald MP. Transgenic mice expressing a human mutant beta1 thyroid receptor are hyperactive, impulsive, and inattentive. Genes, brain, and behavior. 2006;5:282–297. doi: 10.1111/j.1601-183X.2005.00161.x. [DOI] [PubMed] [Google Scholar]
- Silberman DM, Wald M, Genaro AMa. Effects of chronic mild stress on lymphocyte proliferative response. Participation of serum thyroid hormones and corticosterone. International Immunopharmacology. 2002;2:487–497. doi: 10.1016/s1567-5769(01)00190-4. [DOI] [PubMed] [Google Scholar]
- Sinai C, Hirvikoski T, Nordstrom AL, Nordstrom P, Nilsonne A, Wilczek A, Asberg M, Jokinen J. Hypothalamic pituitary thyroid axis and exposure to interpersonal violence in childhood among women with borderline personality disorder. European journal of psychotraumatology. 2014;5 doi: 10.3402/ejpt.v5.23911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slone-Wilcoxon J, Redei EE. Maternal-fetal glucocorticoid milieu programs hypothalamic-pituitary-thyroid function of adult offspring. Endocrinology. 2004;145:4068–4072. doi: 10.1210/en.2004-0473. [DOI] [PubMed] [Google Scholar]
- Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, Nixon A, Pearce EN, Soldin OP, Sullivan S, Wiersinga W. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid : official journal of the American Thyroid Association. 2011;21:1081–1125. doi: 10.1089/thy.2011.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenzel D, Wilsch-Brauninger M, Wong FK, Heuer H, Huttner WB. Integrin alphavbeta3 and thyroid hormones promote expansion of progenitors in embryonic neocortex. Development. 2014;141:795–806. doi: 10.1242/dev.101907. [DOI] [PubMed] [Google Scholar]
- Stiles J, Jernigan TL. The basics of brain development. Neuropsychology review. 2010;20:327–348. doi: 10.1007/s11065-010-9148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suarez-Rodriguez M, Azcona-San Julian C, Alzina de Aguilar V. Hypothyroxinemia during pregnancy: the effect on neurodevelopment in the child. International journal of developmental neuroscience : the official journal of the International Society for Developmental Neuroscience. 2012;30:435–438. doi: 10.1016/j.ijdevneu.2012.07.004. [DOI] [PubMed] [Google Scholar]
- Taylor AD, Flower RJ, Buckingham JC. Dexamethasone inhibits the release of TSH from the rat anterior pituitary gland in vitro by mechanisms dependent on de novo protein synthesis and lipocortin 1. The Journal of endocrinology. 1995;147:533–544. doi: 10.1677/joe.0.1470533. [DOI] [PubMed] [Google Scholar]
- Taylor PN, Okosieme OE, Dayan CM, Lazarus JH. Therapy of endocrine disease: Impact of iodine supplementation in mild-to-moderate iodine deficiency: systematic review and meta-analysis. European journal of endocrinology / European Federation of Endocrine Societies. 2014;170:R1–R15. doi: 10.1530/EJE-13-0651. [DOI] [PubMed] [Google Scholar]
- ten Donkelaar HJ, van der Vliet T. Overview of the Development of the Human Brain and Spinal Cord. In: ten Donkelaar HJ, et al., editors. Clinical Neuroembryology. Springer; Berlin: 2006. [Google Scholar]
- Thangaratinam S, Tan A, Knox E, Kilby MD, Franklyn J, Coomarasamy A. Association between thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of evidence. BMJ. 2011;342:d2616. doi: 10.1136/bmj.d2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas AL, Krane EJ, Nathanielsz PW. Changes in the fetal thyroid axis after induction of premature parturition by low dose continuous intravascular cortisol infusion to the fetal sheep at 130 days of gestation. Endocrinology. 1978;103:17–23. doi: 10.1210/endo-103-1-17. [DOI] [PubMed] [Google Scholar]
- Thorpe-Beeston JG, Nicolaides KH, Felton CV, Butler J, McGregor AM. Maturation of the secretion of thyroid hormone and thyroid-stimulating hormone in the fetus. The New England journal of medicine. 1991;324:532–536. doi: 10.1056/NEJM199102213240805. [DOI] [PubMed] [Google Scholar]
- Tohei A. Studies on the functional relationship between thyroid, adrenal and gonadal hormones. The Journal of reproduction and development. 2004;50:9–20. doi: 10.1262/jrd.50.9. [DOI] [PubMed] [Google Scholar]
- Travers CA, Guttikonda K, Norton CA, Lewis PR, Mollart LJ, Wiley V, Wilcken B, Eastman CJ, Boyages SC. Iodine status in pregnant women and their newborns: are our babies at risk of iodine deficiency? The Medical journal of Australia. 2006;184:617–620. doi: 10.5694/j.1326-5377.2006.tb00417.x. [DOI] [PubMed] [Google Scholar]
- Tsatsoulis A, Johnson E, Kalogera C, Seferiadis K, Tsolas O. The effect of thyrotoxicosis on adrenocortical reserve. European Journal of Endocrinology. 2000;142:231–235. doi: 10.1530/eje.0.1420231. [DOI] [PubMed] [Google Scholar]
- Turpeinen U, Markkanen H, Sane T, Hamalainen E. Determination of free tetrahydrocortisol and tetrahydrocortisone ratio in urine by liquid chromatography-tandem mass spectrometry. Scandinavian journal of clinical and laboratory investigation. 2006;66:147–159. doi: 10.1080/00365510500474504. [DOI] [PubMed] [Google Scholar]
- Tyzio R, Nardou R, Ferrari DC, Tsintsadze T, Shahrokhi A, Eftekhari S, Khalilov I, Tsintsadze V, Brouchoud C, Chazal G, Lemonnier E, Lozovaya N, Burnashev N, Ben-Ari Y. Oxytocin-mediated GABA inhibition during delivery attenuates autism pathogenesis in rodent offspring. Science. 2014;343:675–679. doi: 10.1126/science.1247190. [DOI] [PubMed] [Google Scholar]
- Unterholzner S, Willhauck MJ, Cengic N, Schutz M, Goke B, Morris JC, Spitzweg C. Dexamethasone stimulation of retinoic Acid-induced sodium iodide symporter expression and cytotoxicity of 131-I in breast cancer cells. The Journal of clinical endocrinology and metabolism. 2006;91:69–78. doi: 10.1210/jc.2005-0779. [DOI] [PubMed] [Google Scholar]
- van Mil NH, Tiemeier H, Bongers-Schokking JJ, Ghassabian A, Hofman A, Hooijkaas H, Jaddoe VW, de Muinck Keizer-Schrama SM, Steegers EA, Visser TJ, Visser W, Ross HA, Verhulst FC, de Rijke YB, Steegers-Theunissen RP. Low urinary iodine excretion during early pregnancy is associated with alterations in executive functioning in children. The Journal of nutrition. 2012;142:2167–2174. doi: 10.3945/jn.112.161950. [DOI] [PubMed] [Google Scholar]
- Vanderpump MPJ. The epidemiology of thyroid disease. British Medical Bulletin. 2011;99:39–51. doi: 10.1093/bmb/ldr030. [DOI] [PubMed] [Google Scholar]
- Velasco I, Carreira M, Santiago P, Muela JA, Garcia-Fuentes E, Sanchez-Munoz B, Garriga MJ, Gonzalez-Fernandez MC, Rodriguez A, Caballero FF, Machado A, Gonzalez-Romero S, Anarte MT, Soriguer F. Effect of iodine prophylaxis during pregnancy on neurocognitive development of children during the first two years of life. The Journal of clinical endocrinology and metabolism. 2009;94:3234–3241. doi: 10.1210/jc.2008-2652. [DOI] [PubMed] [Google Scholar]
- Velasco I, Martin J, Gallego M, Gutierrez-Repiso C, Santiago P, Lopez-Siguero JP, Mesa EG, Peral JH, Perez V, Garcia-Fuentes E, Soriguer F. Maternal-fetal thyroid function at the time of birth and its relation with iodine intake. Thyroid : official journal of the American Thyroid Association. 2013;23:1619–1626. doi: 10.1089/thy.2013.0035. [DOI] [PubMed] [Google Scholar]
- Vermiglio F, Lo Presti VP, Moleti M, Sidoti M, Tortorella G, Scaffidi G, Castagna MG, Mattina F, Violi MA, Crisa A, Artemisia A, Trimarchi F. Attention deficit and hyperactivity disorders in the offspring of mothers exposed to mild-moderate iodine deficiency: a possible novel iodine deficiency disorder in developed countries. The Journal of clinical endocrinology and metabolism. 2004;89:6054–6060. doi: 10.1210/jc.2004-0571. [DOI] [PubMed] [Google Scholar]
- Vigneri R, Pezzino V, Filetti S, Squatrito S, Galbiati A, Polosa P. Effect of dexamethasone on thyroid hormone response to TSH. Metabolism: clinical and experimental. 1975;24:1209–1213. doi: 10.1016/0026-0495(75)90059-1. [DOI] [PubMed] [Google Scholar]
- Visser WE, Friesema EC, Jansen J, Visser TJ. Thyroid hormone transport in and out of cells. Trends in endocrinology and metabolism: TEM. 2008;19:50–56. doi: 10.1016/j.tem.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Vulsma T, Gons MH, de Vijlder JJ. Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. The New England journal of medicine. 1989;321:13–16. doi: 10.1056/NEJM198907063210103. [DOI] [PubMed] [Google Scholar]
- Walker CD, Sizonenko PC, Aubert ML. Modulation of the neonatal pituitary and adrenocortical responses to stress by thyroid hormones in the rat: effects of hypothyroidism and hyperthyroidism. Neuroendocrinology. 1989;50:265–273. doi: 10.1159/000125232. [DOI] [PubMed] [Google Scholar]
- Wallis K, Sjogren M, van Hogerlinden M, Silberberg G, Fisahn A, Nordstrom K, Larsson L, Westerblad H, Morreale de Escobar G, Shupliakov O, Vennstrom B. Locomotor deficiencies and aberrant development of subtype-specific GABAergic interneurons caused by an unliganded thyroid hormone receptor alpha1. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2008;28:1904–1915. doi: 10.1523/JNEUROSCI.5163-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P, Gao J, Zhao S, Guo Y, Wang Z, Qi F. Maternal Thyroxine Levels During Pregnancy and Outcomes of Cognitive Development in Children. Molecular neurobiology. 2015 doi: 10.1007/s12035-015-9189-z. [DOI] [PubMed] [Google Scholar]
- Wang S. Traumatic stress and thyroid function. Child abuse & neglect. 2006;30:585–588. doi: 10.1016/j.chiabu.2005.11.012. [DOI] [PubMed] [Google Scholar]
- Wang Y, Wang Y, Dong J, Wei W, Song B, Min H, Yu Y, Lei X, Zhao M, Teng W, Chen J. Developmental hypothyroxinemia and hypothyroidism reduce proliferation of cerebellar granule neuron precursors in rat offspring by downregulation of the sonic hedgehog signaling pathway. Molecular neurobiology. 2014;49:1143–1152. doi: 10.1007/s12035-013-8587-3. [DOI] [PubMed] [Google Scholar]
- Wang Y, Wei W, Wang Y, Dong J, Song B, Min H, Teng W, Chen J. Neurotoxicity of developmental hypothyroxinemia and hypothyroidism in rats: Impairments of long-term potentiation are mediated by phosphatidylinositol 3-kinase signaling pathway. Toxicology and Applied Pharmacology. 2013;271:257–265. doi: 10.1016/j.taap.2013.04.034. [DOI] [PubMed] [Google Scholar]
- Wang Y, Zhong J, Xu H, Wei W, Dong J, Yu F, Wang Y, Gong J, Shan Z, Teng W, Chen J. Perinatal Iodine Deficiency and Hypothyroidism Increase Cell Apoptosis and Alter Doublecortin and Reelin Protein Expressions in Rat Cerebellum. Archives of Medical Research. 2012;43:255–264. doi: 10.1016/j.arcmed.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Westerholz S, de Lima AD, Voigt T. Regulation of early spontaneous network activity and GABAergic neurons development by thyroid hormone. Neuroscience. 2010;168:573–589. doi: 10.1016/j.neuroscience.2010.03.039. [DOI] [PubMed] [Google Scholar]
- WHO/UNICEF/ICCIDD . Assessment of iodine deficiency disorders and monitoring their elimination. 3rd ed World Health Organization; 2007. [Google Scholar]
- Williams F, Watson J, Ogston S, Hume R, Willatts P, Visser T. Mild maternal thyroid dysfunction at delivery of infants born </=34 weeks and neurodevelopmental outcome at 5.5 years. The Journal of clinical endocrinology and metabolism. 2012;97:1977–1985. doi: 10.1210/jc.2011-2451. [DOI] [PubMed] [Google Scholar]
- Williams GR. Neurodevelopmental and neurophysiological actions of thyroid hormone. Journal of neuroendocrinology. 2008;20:784–794. doi: 10.1111/j.1365-2826.2008.01733.x. [DOI] [PubMed] [Google Scholar]
- Willoughby KA, McAndrews MP, Rovet JF. Accuracy of episodic autobiographical memory in children with early thyroid hormone deficiency using a staged event. Developmental cognitive neuroscience. 2014a;9:1–11. doi: 10.1016/j.dcn.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby KA, McAndrews MP, Rovet JF. Effects of maternal hypothyroidism on offspring hippocampus and memory. Thyroid : official journal of the American Thyroid Association. 2014b;24:576–584. doi: 10.1089/thy.2013.0215. [DOI] [PubMed] [Google Scholar]
- Woltz HH, Thompson FN, Kemppainen RJ, Munnell JF, Lorenz MD. Effect of prednisone on thyroid gland morphology and plasma thyroxine and triiodothyronine concentrations in the dog. American journal of veterinary research. 1983;44:2000–2003. [PubMed] [Google Scholar]
- Woo NH, Lu B. Regulation of cortical interneurons by neurotrophins: from development to cognitive disorders. The Neuroscientist : a review journal bringing neurobiology, neurology and psychiatry. 2006;12:43–56. doi: 10.1177/1073858405284360. [DOI] [PubMed] [Google Scholar]
- Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE. Neonatal MRI to Predict Neurodevelopmental Outcomes in Preterm Infants. New England Journal of Medicine. 2006;355:685–694. doi: 10.1056/NEJMoa053792. [DOI] [PubMed] [Google Scholar]
- Wu S-Y, Klein AH, Chopra IJ, Fisher DA. Alterations in Tissue Thyroxine-5′-Monodeiodinating Activity in Perinatal Period. Endocrinology. 1978;103:235–239. doi: 10.1210/endo-103-1-235. [DOI] [PubMed] [Google Scholar]
- Yau VM, Lutsky M, Yoshida CK, Lasley B, Kharrazi M, Windham G, Gee N, Croen LA. Prenatal and neonatal thyroid stimulating hormone levels and autism spectrum disorders. Journal of autism and developmental disorders. 2015;45:719–730. doi: 10.1007/s10803-014-2227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang D, Raichle ME. Disease and the brain's dark energy. Nature reviews Neurology. 2010;6:15–28. doi: 10.1038/nrneurol.2009.198. [DOI] [PubMed] [Google Scholar]
- Zhang HM, Su Q, Luo M. Thyroid hormone regulates the expression of SNAP-25 during rat brain development. Molecular and cellular biochemistry. 2008;307:169–175. doi: 10.1007/s11010-007-9596-1. [DOI] [PubMed] [Google Scholar]
- Zoeller RT. Transplacental thyroxine and fetal brain development. The Journal of clinical investigation. 2003;111:954–957. doi: 10.1172/JCI18236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zumoff B, Bradlow HL, Levin J, Fukushima DK. Influence of thyroid function on the in vivo cortisol in equilibrium cortisone equilibrium in man. Journal of steroid biochemistry. 1983;18:437–440. doi: 10.1016/0022-4731(83)90062-6. [DOI] [PubMed] [Google Scholar]