Abstract
Background
To anticipate the effects of ACOs on surgical care, we examined pre-enrollment utilization, outcomes, and costs of inpatient surgery among hospitals currently enrolled in Medicare ACOs versus non-enrolling facilities.
Methods
Using the Nationwide Inpatient Sample (2007-2011), we compared patient and hospital characteristics, distributions of surgical specialty care, and the most common inpatient surgeries performed between ACO-enrolling and non-enrolling hospitals prior to implementation of Medicare ACOs. We used multivariable regression to compare pre-enrollment inpatient mortality, length of stay (LOS), and costs.
Results
Hospitals now participating in Medicare ACO programs were more frequently non-profit (p<0.001), teaching institutions (p=0.01) that performed more specialty procedures (p<0.001). We observed no clinically meaningful pre-enrollment differences for inpatient mortality, prolonged LOS, or costs for procedures performed at ACO-enrolling versus non-enrolling hospitals.
Conclusions
Medicare ACO hospitals had pre-enrollment outcomes that were similar to non-participating facilities. Future studies will determine whether ACO participation yields differential changes in surgical quality or costs.
Keywords: surgery, quality improvement, costs, accountable care organizations, policy
Introduction
Established as part of the Affordable Care Act (ACA), Accountable Care Organization (ACO) programs for Medicare beneficiaries aim to improve quality of care and patient experience, and reduce health care costs. ACOs have rapidly increased in both size and number since the implementation of the ACA, such that in 2014 there were 338 Centers for Medicare and Medicaid Services (CMS) ACOs providing care to almost 5 million (>10%) Medicare beneficiaries.1 To date, the CMS ACO model appears to be moderately successful at lowering cost growth while meeting quality and patient experience benchmarks.2–4 Early ACOs have focused on primary care, and have directed attention towards improving care coordination and reducing over-utilization of health care services.2,5 Despite the fact that inpatient surgery accounts for a substantial proportion of healthcare costs, it has not been a focus of early ACOs, and none of the CMS quality benchmarks directly address surgical care.5
Accordingly, the extent to which ACOs might improve the quality and costs of inpatient surgical care is uncertain.6 It is possible that hospitals volunteering to participate in ACOs were already relatively high performers in regard to surgical care. In this scenario, the potential benefits of ACO participation may be limited, since there will be less room for improvement. Alternatively, early-adopting hospitals may have had high costs at baseline, and therefore may be more likely to reduce expenditures and qualify for shared savings. If this is true, then the ACO model may well prove to be effective at enhancing the cost-efficiency of hospital-based surgical care.
In this context, we investigated baseline (i.e., pre-ACA) differences in the utilization and outcomes of inpatient surgery between hospitals that are now formal participants in Medicare ACOs and those that are not. A better understanding of such baseline differences could help policymakers anticipate the potential impact of this model for the quality and cost of surgical care.
Methods
Identification of Patients and Surgical Procedures
We conducted a retrospective cohort study of patients undergoing common inpatient procedures in hospitals included in the Nationwide Inpatient Sample (NIS) from 2007 through 2011. The NIS database consists of standard hospital discharge abstracts from 46 states, approximating a 20 percent stratified sample of all hospitals in the US.7 We used data from the NIS to ascertain patient demographics (e.g., age, sex, race, and household income quartile), admission and discharge information (e.g., length of stay, admission type), hospital charges, and International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic and procedure codes.8
Surgical admissions were identified by the presence of a principal ICD-9-CM procedure code meeting NIS criteria for a major procedure performed in an operating room.7 We used Clinical Classification Software (CCS)9 available in the NIS to categorize diagnoses and procedures based on ICD-9-CM codes into clinically meaningful categories, as well as into 1 of 10 mutually exclusive groups of operations performed by distinct surgical specialties (e.g., general surgery, obstetrics/gynecology, urology).8
Identification of ACO Participant Hospitals
For this analysis, we included hospitals that ultimately enrolled in either the Pioneer or Medicare Shared Savings Program (MSSP) ACOs. We identified ACO-enrolling hospitals using a multi-step process. First, we used a publically available list from CMS to identify hospitals that were formal participants in the MSSP as of February 2014.10 Next, we confirmed that each of these facilities was an acute care hospital using the National Provider Identifier (NPI) database.11 To identify Pioneer ACO affiliated hospitals, we started with a published CMS list of Pioneer ACOs,12 and then visited each ACO's website to identify all affiliated hospitals. For both MSSP and Pioneer ACOs, we then identified each hospital by name in the American Hospital Association (AHA) Survey of Hospitals, and used the AHA identification number to link with the NIS. Throughout this manuscript, we refer to this collective group of hospitals as ACO-enrolling hospitals.
Identification of Control Hospitals
We sought to identify a control group of hospitals that were not formal participants in an ACO, and that were also unlikely to be affiliated with a provider-based ACO (because ACOs are not required to have an affiliated hospital). To do this, we used publically available data to estimate the total number of lives covered by ACOs in each state.13 We then empirically defined states with fewer than 6% of lives covered by an ACO as having low ACO penetrance. Next, we classified all non-enrolling hospitals in these 38 low ACO penetrance states as controls (1,054 control hospitals). To ensure that none of the non-enrolling control hospitals were misclassified, we checked each control against the CMS published list of ACO participants. Throughout the manuscript, we refer to this group of facilities as non-enrolling hospitals.
Outcome Measures
We determined the 9 most common major procedures (based on CCS codes) performed during surgical admissions in ACO-enrolling and non-enrolling hospitals.9 For each of these procedures, we then compared inpatient mortality, prolonged length of stay (LOS), and costs between hospital groups. Inpatient mortality was analyzed only for procedures with mortality greater than 1%. Prolonged LOS was defined as a LOS greater than the 90th percentile for all patients undergoing that procedure.8 Costs associated with each surgical admission were calculated by converting the total admission charges to costs using a hospital specific cost to charge ratio provided by HCUP, and adjusting for the patient's primary admitting diagnosis.14
Statistical Analysis
First, we compared the characteristics of patients undergoing major inpatient procedures at ACO-enrolling and non-enrolling hospitals using chi squared, Wilcoxon rank sum, and t-tests, where appropriate. We used similar methods to examine differences in hospital-level characteristics.
We then compared the distributions of surgical specialty care and of the 9 most common inpatient surgeries according to ACO enrollment status. Next, we fit multivariable regression models to compare procedure-specific outcomes at ACO-enrolling and non-enrolling hospitals. In terms of outcome variables, inpatient mortality and prolonged LOS were treated as binary variables (logistic regression models), and generalized estimating equations were used to account for clustering of patient outcomes within hospitals. Total admission costs were log-transformed prior to analysis, in order to normalize their distribution. A mixed regression model was used to account for potential correlation of patient outcomes within hospitals. We controlled for a number of variables that may confound the relationship between ACO enrollment status and the measured outcomes, including age, gender, race, admission type (emergent/trauma, urgent, or elective), primary payer, median household income of patient's home zip code, number of Elixhauser comorbidities,15 region, hospital bed total, number of inpatient surgical cases, and hospital teaching status.
Results
We identified 273 and 151 hospitals enrolling in the MSSP and Pioneer ACO programs, respectively. Of these 424 ACO-enrolling hospitals, 225 linked to the NIS through the hospital's AHA ID. Table 1 describes the characteristics of patients treated at ACO-enrolling and non-enrolling hospitals. ACO-enrolling hospitals were larger, had greater surgical volume, and were more likely to be non-profit, teaching institutions located in the northwest and northeast (Table 2).
Table 1.
Patient Characteristics (NIS 2007-2011)
| ACO-Enrolling Hospitals |
Non-Enrolling Hospitals |
||
|---|---|---|---|
| Characteristic | p-value | ||
| Admissions (No.) | 851,608 | 2,657,935 | |
| Age (yrs) | |||
| Median | 54 | 53 | <0.001 |
| Category, % | <0.001 | ||
| <50 | 42.9 | 45.6 | |
| 50-59 | 15.9 | 15.0 | |
| 60-69 | 17.3 | 16.4 | |
| 70-79 | 14.4 | 13.8 | |
| ≥80 | 9.5 | 9.2 | |
| Race (%) | <0.001 | ||
| White | 74.3 | 70.8 | |
| Black | 8.2 | 9.7 | |
| Hispanic | 11.3 | 13.1 | |
| Other | 6.2 | 6.4 | |
| Female (%) | 67.7 | 68.4 | <0.001 |
| Household Income (% in each quartile) | <0.001 | ||
| <$39,000 | 14 .3 | 22 .3 | |
| $39,000-47,999 | 22.2 | 23.4 | |
| $48,000-62,999 | 30.0 | 25.4 | |
| ≥$63,000 | 33.5 | 28.9 | |
| Admission Type (%) | <0.001 | ||
| Elective | 78 .6 | 80 .0 | |
| Trauma, emergent, urgent | 21.4 | 20.0 | |
| Comorbidity count (%) | <0.001 | ||
| 0 | 32.8 | 34.4 | |
| 1 | 23.2 | 23.0 | |
| ≥2 | 44.0 | 42.6 | |
| Primary Payer (%) | <0.001 | ||
| Medicare | 32.3 | 31.9 | |
| Medicaid | 11.8 | 14.8 | |
| Private, self-pay, or other | 55.9 | 53.3 |
Table 2.
Hospital Characteristics (NIS and AHA 2007-2011)
| Characteristic | ACO-Enrolling Hospitals | Non-Enrolling Hospitals | p-value |
|---|---|---|---|
| Hospitals (No.) | 225 | 1054 | |
| Median number of beds (med/surg) | 232 | 162 | <0.001 |
| Median number of Operating Rooms | 10 | 7 | <0.001 |
| Median number of inpatient surgical cases | 2842 | 1621.5 | <0.001 |
| Median number of total surgical cases | 7608 | 5332 | <0.001 |
| Hospitals (%) | |||
| ICU capabilities | 88.3 | 83.5 | 0.08 |
| Regional Trauma Center | 24.8 | 27.4 | 0.004 |
| Hospital Ownership (%) | <0.001 | ||
| Public | 5.3 | 15.2 | |
| Non-profit | 89.8 | 65.6 | |
| For profit | 4.9 | 19.2 | |
| Teaching Hospital (%) | 33.8 | 25.4 | 0.01 |
| Critical Access Hospital (%) | 8.4 | 12.7 | 0.07 |
| Rural location (%) | 22.2 | 33.3 | 0.001 |
| Region | <0.001 | ||
| Northeast | 29.3 | 24.3 | |
| Northwest | 29.8 | 12.5 | |
| South | 13.3 | 31.5 | |
| West | 27.6 | 31.7 |
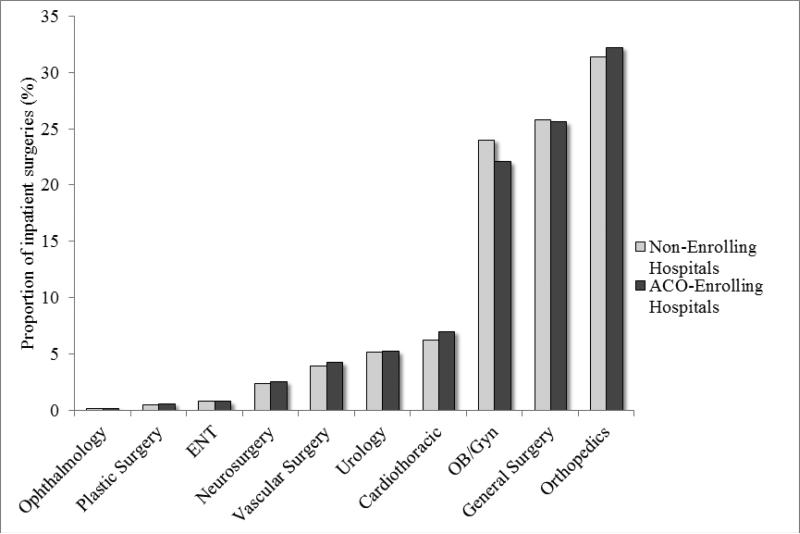
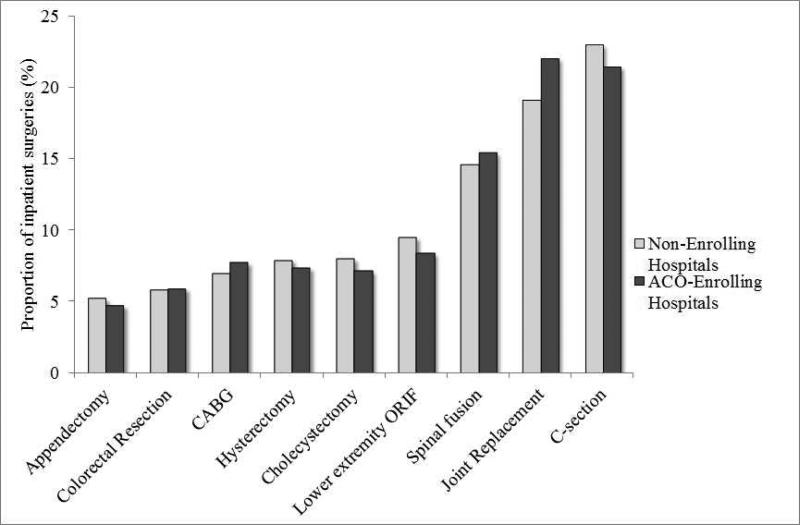
The distribution of cases according to surgical specialty, and the 9 most common inpatient surgical procedures differed by ACO enrollment status (p<0.001 for each, Figure 1, Figure 2). Overall, ACO-enrolling hospitals performed a greater proportion of surgical specialty procedures, and relatively fewer obstetric/gynecologic and general surgical procedures.
Figure 1.
The proportion of the most common inpatient surgical procedures performed in ACO-enrolling and non-enrolling hospitals (p<0.001).
Figure 2.
The proportion of all major surgical procedures in ACO-enrolling and non-enrolling hospitals by surgical specialty service (p<0.001).
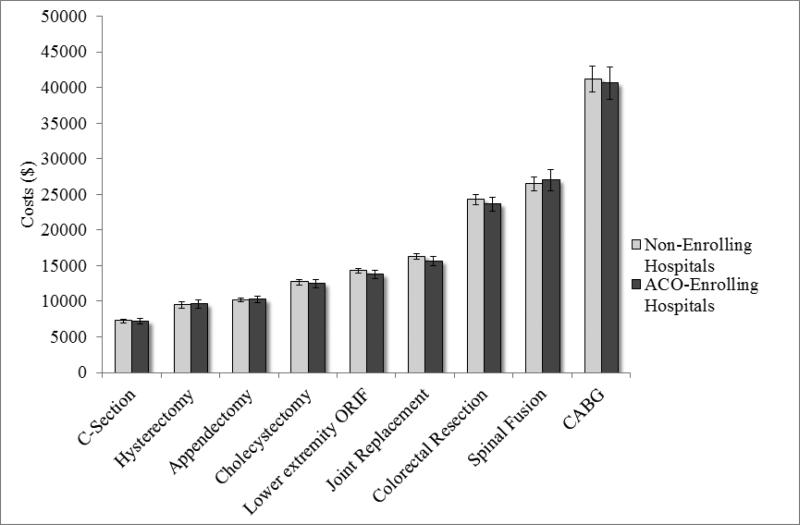
Among the procedures with greater than 1% inpatient mortality overall (lower extremity open reduction and internal fixation (ORIF), cholecystectomy, colorectal resection, coronary artery bypass graft (CABG)), the adjusted likelihood of inpatient mortality was similar for ACO-enrolling and non-enrolling hospitals (Table 3). The adjusted likelihood of a prolonged LOS was also similar for ACO-enrolling and non-enrolling hospitals for 8 of the 9 most commonly performed procedures; patients undergoing colorectal resection at ACO-enrolling hospitals were more likely to have a prolonged length of stay (Table 4). In addition, there were no differences in the cost of surgical admissions between ACO-enrolling and non-enrolling hospitals (Figure 3).
Table 3.
Inpatient Procedural Mortality (NIS 2007-2011)
| Mortality |
|
|---|---|
| Procedure | Adjusted ACO-Enrolling OR (95% CI) |
| Lower extremity ORIF | 0.91 (0.80-1.02) |
| Cholecystectomy | 1.05 (0.92-1.19) |
| Colorectal Resection | 1.03 (0.94-1.13) |
| CABG | 0.98 (0.86-1.11) |
* Adjusted for age, gender, race, admission type, payer, income, comorbidities, region, hospital bed total, number of inpatient surgical cases, and hospital teaching status.
Mortality calculated for procedures with >1% overall mortality.
Referent group are non-enrolling hospitals.
Table 4.
Inpatient Procedural Prolonged LOS (NIS 2007-2011)
| Prolonged LOS |
|
|---|---|
| Procedure | Adjusted ACO-Enrolling OR (95% CI) |
| C-section | 1.18 (0.94-1.49) |
| Spinal fusion | 1.02 (0.87-1.19) |
| Hysterectomy | 1.07 (0.90-1.27) |
| Joint Replacement | 0.86 (0.73-1.02) |
| Lower extremity ORIF | 0.99 (0.85-1.14) |
| Cholecystectomy | 0.93 (0.82-1.06) |
| Colorectal Resection | 1.12 (1.02-1.24) |
| Appendectomy | 1.00 (0.92-1.08) |
| CABG | 1.18 (0.97-1.45) |
* Adjusted for age, gender (where appropriate), race, admission type, payer, income, comorbidities, region, hospital bed total, number of inpatient surgical cases, and hospital teaching status.
Referent group are non-enrolling hospitals.
Figure 3.
Adjusted costs (with 95% CI) of the 9 most common major inpatient surgical procedures in ACO-enrolling and non-enrolling hospitals (p>0.05).
Discussion
Prior to implementation of the ACA, there were no substantive differences in the utilization and outcomes of inpatient surgery between hospitals that now differ with respect to ACO participation. We specifically found no clinically meaningful differences in inpatient mortality, prolonged LOS, or hospital costs between these two groups. Collectively, these findings suggest that, prior to implementation of the ACA, hospitals that have been early adopters of the ACO model had characteristics and performance that were very similar to those that have chosen not to participate.
There are several potential explanations for these findings. First, given the focus of ACO's on primary care,2,5 it is possible that hospital administrators did not emphasize the role of surgical care when deciding to volunteer for an ACO program. At least one empirical study has demonstrated that for patients treated in Integrated Delivery Systems versus Non-Integrated Delivery Systems, a comparison of healthcare structures arguably most synonymous to ACOs, quality improvements and savings in the outpatient setting might not extend to inpatient surgery.16 Therefore, any baseline differences between ACO-enrolling and non-enrolling hospitals in other areas of care, possibly affecting the decision to become an ACO, may not manifest as concurrent differences in surgical care and outcomes. Second, hospitals’ decision to participate in ACOs may not be associated with obvious opportunities for improving clinical care and instead may be more related to strategic decisions around referrals, market share, and other non-clinical factors. In this scenario, it is not surprising that baseline performance would be relatively similar for hospitals that now differ by ACO status. Third, it is possible that hospitals with average performance on metrics of surgical quality and costs were more likely to volunteer for ACO programs. High performing hospitals may envision a harder time achieving the additional improvements needed to reach benchmarks for shared savings. Conversely, lower performing hospitals may not have been confident in their ability to improve. Ultimately, the decision to volunteer for an ACO program is likely driven by factors and incentives that have little relationship to current performance with delivery of inpatient surgical care.
Our study has several limitations. First, we cannot confirm that facilities classified as non-enrolling hospitals didn't interact with physicians or other providers that eventually enrolled in an ACO. In an effort to exclude such hospitals that may see an “ACO effect” from ACO-enrolling providers in the same community or region, we used only hospitals from states with low ACO penetrance (<6% of lives covered by an ACO) as our controls. Second, due to state-specific privacy laws preventing hospital identification in the NIS, certain states could not be included in this analysis. However, our study did include ACO-enrolling and non-enrolling hospitals from all major geographic regions of the country.
Third, it is possible that there were unmeasured differences in patient characteristics and disease severity not completely accounted for by variables available in the administrative data. Nonetheless, our multivariable models did include a relatively broad range of patient and hospital characteristics that differed between the hospital groups. Finally, when examining costs we used charges converted to costs rather than actual payments. Even so, our approach is similar to previous studies8,17,18 and represents an established method for estimating costs based on NIS data.19
These limitations notwithstanding, our findings have potential implications for both policymakers and ACO leaders. For policymakers, our finding that surgical care prior to the ACA was similar at hospitals that now differ with respect to ACO participation indicates that adoption of this model, at least for hospitals, is probably not driven by specific opportunities to quickly improve the quality and cost-efficiency of surgical care (and thereby achieve shared savings). In addition, understanding whether changes from this baseline—with respect to population-level utilization, quality, and/or costs of surgical care—occur after ACO implementation will likely be an important determinant of further dissemination of this model. Moreover, if ACO policies drive improvements in surgical quality and costs, the care processes and infrastructure that led to such changes may be replicable in hospitals that are not currently participating.
For ACO leaders, the fact that their baseline performance in surgery was similar to their non-enrolling peers suggests that there may be opportunities to apply quality and care-coordination activities in other areas of care to inpatient surgery. Such an effort could impact quality and ultimately costs of surgical care.
Moving forward, studies that specifically compare long-term quality and cost outcomes for beneficiaries treated in ACOs and those who were not will further clarify the implications of this model for surgical care. Ultimately the magnitude of any improvements, in addition to effects of ACOs on patient satisfaction and surgical utilization, will inform the broader impact of ACOs for surgery, as well as the potential enthusiasm for greater dissemination of the model.
Summary.
To anticipate the effects of ACOs on surgical care, we examined pre-enrollment utilization, outcomes, and costs of inpatient surgery among hospitals currently enrolled in Medicare ACOs, versus non-enrolling facilities, prior to the implementation of the Affordable Care Act. Across the nine most common inpatient surgeries, we observed no clinically meaningful differences for inpatient mortality, prolonged length of stay, or costs among hospital groups. Collectively, these findings suggest that hospitals that now participate in ACOs had similar baseline performance to those not participating. The ability of ACO-enrolling hospitals to differentially improve quality and cost beyond these baseline measures will inform the impact of this model for surgical care.
Acknowledgments
Funding:
This work was supported by the University of Michigan Clinical & Translational Science Award [UL1TR000433 to SRH]; the National Institute of Diabetes and Digestive and Kidney Disease [T32 F025681 to LAH]; and the National Cancer Institute [1-RO1-CA-174768 to DCM].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest:
Scott Hawken: none
Lindsey A. Herrel: Paid consultant for ArborMetrix
Chandy Ellimoottil: none
Zachary A. Montgomery: none
Zaojun Ye: none
David C. Miller: Paid consultant for ArborMetrix. Contract support of Michigan Urologic Surgery
Collaborative and Michigan Value Collaborative.
References
- 1.Barnes AJ, Unruh L, Chukmaitov A, Van Ginneken E. Accountable care organizations in the USA: Types, developments and Challenges. Health Policy (New York) 2014;118(1):1–7. doi: 10.1016/j.healthpol.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 2.Berkowitz S a, Pahira JJ. Accountable Care Organization Readiness and Academic Medical Centers. Acad Med. 2014;89(9):1–6. doi: 10.1097/ACM.0000000000000365. [DOI] [PubMed] [Google Scholar]
- 3. [October 20, 2014];Medicare ACOs Continue to Succeed in Improving Care, Lowering Cost Growth. 2014 http://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2014-Fact-sheets-items/2014-09-16.html.
- 4.McWilliams JM, Landon BE, Chernew ME, Zaslavsky AM. Changes in Patients’ Experiences in Medicare Accountable Care Organizations. NEJM. 2014;371(18):1715–1724. doi: 10.1056/NEJMsa1406552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dupree JM, Patel K, Singer SJ, et al. Attention to surgeons and surgical care is largely missing from early medicare accountable care organizations. Health Aff. 2014;33:972–979. doi: 10.1377/hlthaff.2013.1300. [DOI] [PubMed] [Google Scholar]
- 6.Stain SC, Hoyt DB, Hunter JG, Joyce G, Hiatt JR. American Surgery and the Affordable Care Act. JAMA Surg. 2014;149(9):984–985. doi: 10.1001/jamasurg.2014.1343. [DOI] [PubMed] [Google Scholar]
- 7.HCUP NIS Database Documentation [November 1, 2014];Healthc Cost Util Proj. 2014 www.hcup us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.
- 8.Gadzinski AJ, Dimick JB, Ye Z, Miller DC. Utilization and outcomes of inpatient surgical care at critical access hospitals in the United States. JAMA Surg. 2013;148(7):589–596. doi: 10.1001/jamasurg.2013.1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clinical Classifications Software for ICD-9-CM [November 1, 2014];Healthc Cost Util Proj. 2014 www.hcup us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 10.Shared Savings Program ACOs - ACO Participatns Data Page. Centers Medicare Medicaid Serv; 2014. [June 1, 2014]. https://data.cms.gov/ACO/Medicare-Shared-Savings-Program-Accountable-Care-O/ay8x-m5k6. [Google Scholar]
- 11.NPI Regsitry Natl Plan Provid Enumer Syst. 2014 https://nppes.cms.hhs.gov/NPPESRegistry/NPIRegistryHome.do.
- 12.Medicare Pioneer ACO Model Performance Year 1 and Performance Year 2 Financial Results. Centers Medicare Medicaid Serv; 2014. [October 1, 2014]. http://innovation.cms.gov/Files/x/PioneerACO-Fncl-PY1PY2.pdf. [Google Scholar]
- 13.Petersen M, Gardner P, Tu T MD. Growth and Dispersion of Accountable Care Organizations: June 2014 Update. 2014 http://leavittpartners.com/2014/06/growth-dispersion-accountable-care-organizations-june-2014-update/
- 14.Cost-to-charge ratio files. [November 1, 2014];Healthc Cost Util Proj. 2014 http://www.hcup us.ahrq.gov/db/state/costtocharge.jsp.
- 15.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Miller DC, Ye Z, Gust C, Birkmeyer JD. Anticipating the effects of accountable care organizations for inpatient surgery. JAMA Surg. 2013;148(6):549–554. doi: 10.1001/jamasurg.2013.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sachs T, Pomposelli F, Hamdan A, Wyers M, Schemerhorn M. Trends in the national outcomes and costs for claudication and limb threatening ischemia: Angioplasty vs bypass graft. J Vasc Surg. 2011;54(4):1021–1031. doi: 10.1016/j.jvs.2011.03.281. [DOI] [PubMed] [Google Scholar]
- 18.Yu HY, Hevelone ND, Lipsitz SR, Kowalczyk KJ, Hu JC. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol. 2012;187(April):1392–1399. doi: 10.1016/j.juro.2011.11.089. [DOI] [PubMed] [Google Scholar]
- 19.Sun Y, Friedman B. Tools for more accurate inpatient cost estimates with HCUP databases. [November 1, 2014];Healthc Cost Util Proj. 2009 http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.