Abstract
Purpose of the Study:
Stanford’s Chronic Disease Self-Management Program (CDSMP) has been proven to increase patients’ ability to manage distress. We describe how we replicated CDSMP in Asian and Pacific Islander (API) communities.
Design and Methods:
We used the “track changes” tool to deconstruct CDSMP into its various components (e.g., recruitment and staffing) and the “adaptation traffic light” to identify allowable modifications to the original program. We monitored local leaders’ fidelity of delivery of CDSMP and tracked participants’ attendance, satisfaction, and 6-month outcomes.
Results:
Between July 2007 and February 2010, 584 completed a CDSMP workshop. Baseline and 6-month data were available for 422 (72%), including 53 Caucasians, 177 Asians, and 194 Pacific Islanders. All 3 groups realized significant decreases in social and role activity limitations and significant increases in communication with physicians. Asians and Pacific Islanders also realized significant increases in self-rated health and time spent engaging in stretching/strengthening exercise. Asians also reported significant reductions in health distress and self-reported physician visits and increases in time spent in aerobic exercise, ability to cope with symptoms, and self-efficacy.
Implications:
Our experience suggests that CDSMP can be modified for increased cultural appropriateness for API communities while maintaining the key components responsible for behavior change.
Keywords: Health, Evidence-based practice, Asian and Pacific Rim older adults, Chronic illness
The United States is experiencing a substantial increase in the number of older adults, fueled by the aging of the baby boomers. The United States also is growing more diverse, and Asian and Pacific Islanders (APIs) are the third largest minority group (He, Sengupta, Velkoff, & DeBarros, 2005). In Hawaii, more than 75% of the aging population is API (Hawaii Executive Office on Aging, 2006; U.S. Census Bureau, 2010).
Although older Americans today are living longer and healthier lives than earlier generations, aging continues to be associated with chronic illness. Chronic conditions are associated with functional disabilities, poor quality of life for older adults, and economic stress for family caregivers, health care systems, and government (Agency for Healthcare Research Quality, 2009; Centers for Disease Control and Prevention & Merck Company Foundation, 2007; Grunfeld et al., 2004; He et al., 2005; Lam & Lauder, 2000; Sprangers et al., 2000; U.S. Census Bureau, 2006).
Although chronic illnesses are rarely cured completely, research consistently validates the benefits of a healthy lifestyle. Several health promotion programs have been proven, through controlled trials, to effectively increase fitness, increase self-management skills, and decrease health care costs (Altpeter, Bryant, Schneider, & Whitelaw, 2006). These programs are called evidence-based health promotion programs (U.S. Administration on Aging [AoA], 2010).
Dedicated to increasing access to health promotion programs among Hawaii seniors with chronic conditions, the Hawaii Healthy Aging Partnership (HHAP) was formed in 2003. This coalition of professionals from government offices for aging and public health, eldercare agencies, and the university secured federal grants to participate in the nationwide effort to improve elder health, replicating evidence-based health promotion programs. This nationwide effort included 16 states in 2006 and expanded to 46 states in 2010. HHAP replicates two evidence-based programs in Hawaii; Stanford’s Chronic Disease Self-Management Program (CDSMP) and EnhanceFitness Program (Tomioka et al., 2009). This article focuses on the adaptation of CDSMP in Hawaii.
CDSMP was developed at Stanford University to empower people with various chronic diseases to take control of their health (Lorig et al., 1999). CDSMP is based on self-efficacy theory, which posits that self-control is a key factor in health promotion and that individuals can “take control” of their health if helped to gain knowledge, skills, and confidence in their abilities to manage health challenges (Bandura, 1997). CDSMP aims to increase self-efficacy through six weekly, 2.5-hr sessions that promote mastery of new knowledge (e.g., about chronic disease) and skills (e.g., in health care communication and goal setting). Leaders model good self-management behaviors, and the group engages in problem-solving activities, support, and feedback sessions each week (Lorig & Holman, 2003). From this 6-week workshop, it is expected that participants feel better, have better control over their symptoms, and are better able to talk to their physicians (Lorig et al., 1999).
The literature includes reports of studies demonstrating CDSMP effectiveness in improving health behavior and status in many places and population and mixed results in terms of reducing health care utilization (Fu, Ding, McGowan, & Fu, 2006; Fu et al., 2003; Gitlin et al., 2008; Goeppinger, Armstrong, Schwartz, Ensley, & Brady, 2007; Griffiths et al., 2005; Kennedy et al., 2007; Lorig, Ritter, & Gonzalez, 2003; Lorig, Sobel, Ritter, Laurent, & Hobbs, 2001; Lorig, Ritter, et al., 2001; Lorig et al., 1999; Siu, Chan, Poon, Chui, & Chan, 2007; Swerissen et al., 2006). A study from the Netherlands reported no positive effects of CDSMP in elders (Elzen, Slaets, Snijders, & Steverink, 2007). These inconclusive findings suggest that translating evidence-based program from one community to another is challenging. Replicators must maintain fidelity to the intervention as designed, meaning that the intervention must be implemented as intended by the program developers (Dusenbury, Barnnigan, Falco, & Hansen, 2003, p. 237). Failing to maintain fidelity jeopardizes the effectiveness of the program.
However, a program developed in one community may not be attractive to or work well in another. Program acceptability and effectiveness may be influenced by differences in community context and culture. Thus, evidence-based programs must be tailored to fit a new community, and they must be evaluated to check that the key components responsible for behavior change are maintained and that the adapted intervention yields the expected benefits.
Hawaii has a multi-cultural population. About two thirds of residents are APIs, including Native Hawaiians (about 24% of the population), Japanese (22%), Filipinos (16%), and smaller proportions of Chinese, Koreans, Samoans, and others; Caucasians comprise only 21% of the state’s population (Hawaii’s Department of Health, 2009). API groups differ in significant ways from each other as well as from Caucasians. Although some are recent immigrants, many Asian elders in Hawaii are descendants from plantation laborers who arrived in Hawaii from China, Japan, Korea, and the Philippines a century ago. These Asian groups have higher life expectancies, lower prevalence of smoking and obesity, and higher participation in health screening than Caucasians in the state (Park, Braun, Horiuchi, Tottori, & Onaka, 2009). Native Hawaiians are the state’s indigenous people. Other Pacific Islanders have moved to Hawaii from U.S.-affiliated jurisdictions of American Samoa, Micronesia, and the Marshall Islands. Although most can communicate in English, many are unfamiliar with U.S. notions of appropriate health behaviors and expectations for compliance and communication (Tsark, the Cancer Council of the Pacific Islands, & Braun, 2007). Native Hawaiians and Pacific Islanders (NHPIs) have comparatively short life expectancies and low levels of education and income (Park et al., 2009).
The effectiveness of CDSMP has not yet been explored in APIs, and Hawaii is a good laboratory for testing translation of CDSMP with API populations. This article describes how we adapted CDSMP in Hawaii and then evaluated the adapted program to assure that key components of CDSMP were delivered with fidelity and that expected outcomes were achieved.
Design and Methods
Program Adaptation Tools
We used the Track Change Tool adapted by the National Council on Aging (NCOA, n.d.) from Peterson (2003) to deconstruct CDSMP into its components, for example, marketing, recruitment, staffing, training, scheduling, and evaluation. Adapters discussed how each component of the program was carried out in its original offering and then provide a detailed description about how each component would be implemented in our community.
We then used the “adaptation traffic light” to identify which components were modifiable (Centers for Disease Control and Prevention, Division of Reproductive Health & ETR Associates, n.d.). Red-light changes, such as substantially shortening the program and deleting activities, cannot be made. Green-light changes, such as creating a local name for the program, can be freely made. Yellow-light changes include adding sessions and translating the entire curriculum to another language—these changes may be possible but should be made with caution and in consultation with the original program developer. We used the traffic-light tool to judge each potential discrepancy between how the original program was offered and how we felt it could be offered in Hawaii and then discussed yellow-light changes with Stanford.
Fidelity Monitoring Measures
CDSMP is an evidence-based program. As such, the key components of the intervention should be delivered exactly as developed. Assuring fidelity starts with excellent training, and trainers from Stanford traveled to Hawaii to train our first two sets of CDSMP leaders. Most of our CDSMP leaders were employees of AoA-funded service providers, who recruited their existing clients to CDSMP. Ethnic concordance between participants and leaders was encouraged, but this was not required or even possible in groups that included older adult groups of different ethnicities.
Our evaluator monitored fidelity of intervention delivery using a 10-item assessment developed by the Stanford Patient Education Research Center (2006). The items, scored on a 4-point Likert scale (1 = poor to 4 = excellent), evaluate leader adherence to the Stanford Leader’s Manual, appropriate modeling of CDSMP activities and techniques, and compliance with leader protocols. Each 6-week workshop is monitored by a trained evaluator at least once. The findings are analyzed by descriptive statistic techniques.
Evaluation Measures
Demographic data (age, gender, marital status, education, chronic conditions, and insurance) were collected on all participants. In this study, the findings were analyzed by three ethnic groupings (Caucasian, Asians, and NHPIs). Caucasians are individuals who identified themselves as Caucasian only. Asians are individuals who identified themselves as Filipino or Japanese. NHPIs are individuals who identified themselves as Native Hawaiian or other Pacific Islander. Session attendance was tracked by CDSMP leaders.
The self-administered Health Outcome Survey, previously validated by Stanford Patient Education Research Center (2006), was used to collect baseline and the six-month follow-up data. This questionnaire assesses health status, health behaviors, self-efficacy, communication with physician, and health care utilization. Health Status items include self-rated health (0 = poor to 5 = excellent), health distress (0 = none of the time to 5 = all of the time), and level of symptoms (0 = none to 10 = severe). Health behavior items include minutes spent in exercise, frequency of using recommended coping styles to manage chronic conditions (0 = never to 5 = always), social/role activities limitations, and self-rated ability to bathe, dress, bend, get in/out of bed, lift a cup to mouth, turn faucets on/off, walk on flat ground, and get in/out of a car (0 = without any difficulties to 4 = unable to do). There were six items measuring self-efficacy (0 = not at all confident to 10 = totally confident). Communication with physicians’ items examined frequency of proactive strategies, such as listing questions, asking questions, and discussing personal problems (0 = never to 5 = always). Health care utilization items asked for number of physician and emergency room (ER) visitations, and hospitalizations within the past 6 months. The pre- and post-findings are analyzed by paired t test analysis.
Program Satisfaction
Program satisfaction was assessed immediately upon completion of the CDSMP 6-week workshop. Our 15-item satisfaction survey was adapted from an instrument developed for CDSMP (Stanford Patient Education Research Center, 2006). Participants were asked how they heard about the workshop, reasons for attending, satisfaction with the leader and workshop, and their perceived skills, knowledge, and confidence to use self-management tools. The satisfaction and confidence items were assessed on a 10-point Likert scale (1 = not at all to 10 = totally). The descriptive statistics were performed to analyze the program satisfaction.
Sample
Initially in Hawaii, CDSMP participants were recruited through AoA-funded providers. Others participants were recruited through word of mouth, health fairs, churches, and mass media (e.g., newspaper and local newsletters). Between July 2007 and February 2010, 741 individuals enrolled in CDSMP. Included in this analysis are 675 (91%) of the participants; 32 participants did not respond to demographic questions, and another 34 were excluded because they identified themselves as neither Caucasians nor APIs.
Of the 675 Caucasian, Asian, or NHPI participants with baseline data, attendance was recorded for 668 participants (Figure 1). Of those, 584 (87%; including 84% of Caucasians, 91% of Asians, and 86% of NHPIs) successfully completed the workshop (attended four or more of the six sessions). Reasons for not being able to complete the workshop included illness, needing to go to doctors’ appointments, conflict with other activities, family emergencies, and moving. The satisfaction survey, administered at the sixth CDSMP session, was completed by 492 (84%) participants. This survey was anonymous, so not linked to participant ethnicity. The 6-month follow-up questionnaire was completed by 422 participants (72%; including 44% of Caucasians, 65% of Asians, and 69% of NHPIs).
Figure 1.
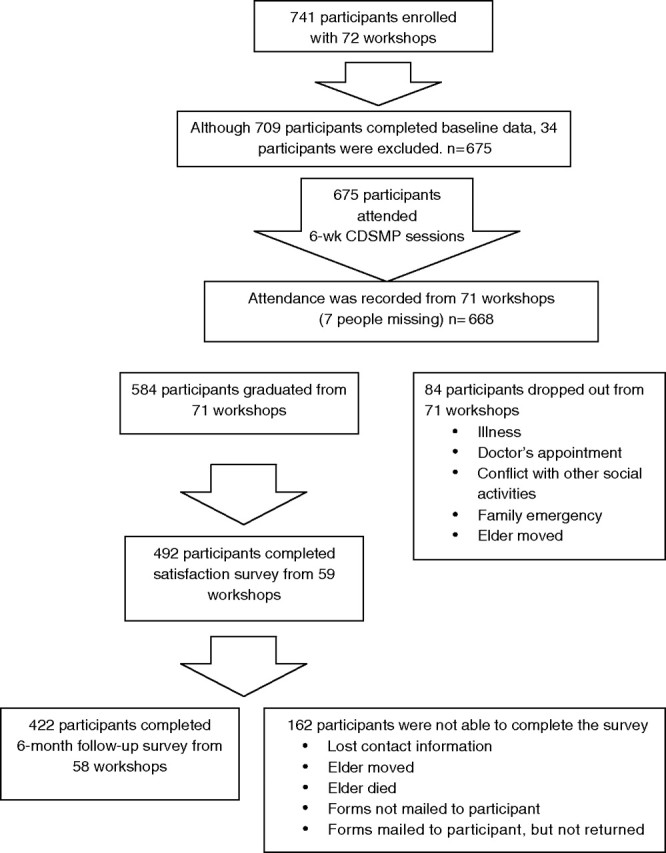
Program participants.
Results
Program Adaptations
From the CDSMP training and manual, it was clear that red-light changes would include shortening the program, using untrained leaders, and deleting or changing any self-management practices such as brainstorming, action planning, and the motivational approach.
Green-light changes (Table 1) included giving the program a local name, Ke Ola Pono (Hawaiian for health in balance), and adopting a bamboo logo (a commonly known Asian symbol of longevity). We also created a presentation to recruit participants to CDSMP. This allowed us to introduce CDSMP and its leaders, familiarize elders with new terms like “self-management,” and orient potential participants to program expectations. To the CDSMP sessions, we added an opening prayer for NHPI groups, as prayer normally is used by start NHPI gatherings (Braun, Tsark, Santos, Aitaoto, & Chong, 2006). We added a certificate of completion, especially motivational to Asian participants, who felt like they were “graduating from Stanford.” Most importantly, we trained CDSMP leaders from the communities within which we wanted to offer the program.
Table 1.
Hawaii Modifications to the Chronic Disease Self-Management Program (CDSMP)
| Modification | Light grading | Description |
| Giving the program a local name and bamboo logo | Green | Name was changed from CDSMP to Ke Ola Pono, which means “health in balance” in Hawaiian. Bamboo is a commonly known Asian symbol of longevity. Both were included in marketing materials. |
| Creating and delivering a recruitment presentation | Green | This presentation helped to familiarize elders with the concept of self-management, orient elders to program requirements and expectations, introduce leaders for the workshop, and create trust in discussing personal health issues. |
| Opening sessions with prayer | Green | Opening sessions with prayer is expected in some cultural groups, especially Native Hawaiians. |
| Providing healthy local food after each session | Green | Serving healthy food using local fresh fruits and vegetables has cultural meaning that promotes socialization. |
| Providing certificate for completion | Green | Leaders and officials signed the certificate, awarded at the end of the workshop. This activity increased motivation for program completion. |
| Adding “Session 0” to provide assistance to complete forms | Yellow | Group leaders provided one-on-one support to complete consent and registration forms and baseline questionnaires. This helped to overcome health literacy and vision barriers. |
| Adding 6-month reunion for graduates | Yellow | This activity provides opportunity to share successes and to collect 6-month follow-up data. |
| Adding opportunities to explain terms and clarify concepts using local examples | Yellow | Leaders reviewed content using their native language outside of class time so that program participants could learn English words related to self-management. Local examples were used to enhance understanding. |
| Training leaders to prepare the group members to be mindful of time limits and the need to hear from all participants | Yellow | Asking an elder to stop talking is not a familiar practice, especially when the leader is younger than the elder. Training leaders to prepare their groups for this enhanced acceptance of the program. |
Yellow-light changes were made in consultation with CDSMP developers (Table 1). Because we evaluated the program, we added a “Session 0” where we worked with elders one-on-one as they completed consent forms and baseline data questionnaires. This helped overcome health literacy and vision barriers experienced by some program participants. We also added a 6-month reunion for graduates so they could share their successes and at which we collected the 6-month follow-up data. Because we were offering CDSMP in Filipino and Samoan communities, we wanted to deliver CDSMP using the elders’ native language or Pidgin (Hawaiian English). Stanford advised us to deliver the intervention in Standard English but to add opportunities to explain terms and clarify concepts using local examples. Thus, leaders made special efforts to teach unfamiliar English words related to self-management (like fatigue and self-efficacy). Leaders also used native language to review program content during breaks and after each session.
Because some of the examples in the manual were not familiar to Hawaii seniors, local examples were used. For example, the manual likens the “action plan” to a roadmap, but few Hawaii residents are familiar with roadmaps. Instead, we compared the action plan to a call to a travel agent, who helps lay out where to go first and what to do next. During the healthy eating session, leaders used local foods as examples, such as rice, poi, papaya, and taro. Finally, local leaders were trained to set ground rules for sharing within the group. For example, before each session, leaders asked group members not to be offended if the leaders asked them to finish their comments and let another elder speak. Inclusion of this “pre-apology” was necessary because, in most API cultures, it is not customary for a younger person to tell an elder what to do.
Fidelity Monitoring
During the first 4 years, 14 trainings were provided to develop CDSMP trainers and leaders. Working in pairs, these leaders offered 72 workshops across six islands in the state. Workshops were held in senior centers, community centers, churches, senior housing, and service providers’ offices. Fidelity information was collected for 71 (99%) of all workshops by trained evaluators, who provided immediate feedback for improvement and filed a written report with the lead evaluator. Trained leaders who continue to score lower than 3 on any of the 10 evaluations items are asked to reattend training. To date, two leaders were so asked, and both dropped out of CDSMP. Summing fidelity findings across all leaders, the mean score was high (3.71 of 4), suggesting that leaders are leading their classes with a high degree of fidelity.
Evaluation Findings
Of the 675 participants included in this analysis (Table 2), most were female (86%) and 82% were APIs (including Filipino, Japanese, and NHPIs). The mean age of participants was 71.9 years, but Asian participants were significantly older (74.1 years). About 15% of participants reported English language limitations. Program participants reported a variety of chronic diseases, such as diabetes, heart diseases, hypertension, lung disease, arthritis, and osteoporosis. Almost all of the participants had health insurance.
Table 2.
Participants’ Demographic Characteristics
| Characteristics | Total (n = 675), n (%) | Caucasians (n = 120), n (%) | Asians (n = 273), n (%) | NHPIs (n = 282), n (%) |
| Age, years | M: 71.92, range: 25–95 | M: 69.27, range: 48–91 | M: 74.08, range: 25–95 | M: 70.97, range: 25–94 |
| <60 | 57 (8.6) | 18 (15.4) | 18 (6.8) | 21 (7.5) |
| 60–74 | 332 (50.1) | 64 (54.7) | 110 (41.4) | 158 (56.4) |
| 75+ | 274 (41.3) | 35 (29.9) | 138 (51.9) | 101 (36.1) |
| Missing | 12 | 3 | 7 | 2 |
| Gender | ||||
| Male | 97 (14.4) | 26 (21.7) | 34 (12.5) | 37 (13.1) |
| Female | 557 (85.6) | 94 (78.3) | 238 (87.5) | 245 (86.9) |
| Missing | 1 | 0 | 1 | 0 |
| Ethnicity | ||||
| Caucasian | 120 (17.8) | 120 (100) | — | — |
| Japanese | 113 (16.7) | — | 113 (41.4) | — |
| Filipino | 160 (23.7) | — | 160 (58.6) | — |
| Native Hawaiian | 264 (39.1) | — | — | 264 (93.6) |
| Pacific Islanders | 18 (2.7) | — | — | 18 (6.4) |
| Education | ||||
| Less than high school graduate | 156 (23.3) | 6 (5.0) | 83 (30.7) | 67 (23.9) |
| High school graduate | 239 (35.6) | 31 (25.8) | 83 (30.7) | 125 (44.3) |
| Some college/vocational school | 140 (20.8) | 34 (28.3) | 46 (17.0) | 60 (21.3) |
| Greater than college graduate | 137 (20.4) | 49 (40.8) | 58 (21.5) | 30 (10.6) |
| Missing | 3 | 0 | 3 | 0 |
| Marital Status | ||||
| Married | 231 (34.5) | 39 (33.1) | 102 (37.6) | 90 (32.1) |
| Divorced | 96 (14.3) | 38 (32.2) | 15 (5.5) | 43 (15.4) |
| Widowed | 287 (42.9) | 29 (24.6) | 126 (46.5) | 132 (47.1) |
| Other | 55 (8.2) | 12 (10.2) | 28 (10.3) | 15 (5.4) |
| Missing | 6 | 2 | 2 | 2 |
| Household size | M: 2.66, range: 1–16 | M: 1.77, range: 1–6 | M: 2.80, range: 1–15 | M: 2.90, range: 1–16 |
| Alone | 220 (32.8) | 56 (46.7) | 77 (28.6) | 87 (30.9) |
| Two | 220 (32.8) | 47 (39.2) | 83 (30.9) | 90 (31.9) |
| Greater than two people | 231 (34.4) | 17 (14.2) | 109 (40.5) | 105 (37.2) |
| Missing | 4 | 0 | 4 | 0 |
| Have English limitation | 101 (15.1) | 3 (2.5) | 80 (29.6) | 18 (6.4) |
| Missing | 5 | 1 | 3 | 1 |
| Chronic conditions | ||||
| Diabetes | 225 (33.4) | 30 (25.0) | 64 (23.6) | 131 (46.5) |
| Heart diseases | 162 (24.1) | 34 (28.3) | 49 (18.1) | 79 (28.0) |
| Hypertension | 378 (56.2) | 56 (46.7) | 157 (57.9) | 165 (58.5) |
| Lung disease | 105 (15.6) | 20 (16.7) | 31 (11.5) | 54 (19.1) |
| Arthritis | 308 (45.8) | 68 (56.7) | 113 (49.1) | 107 (37.9) |
| Osteoporosis | 119 (17.7) | 21 (17.5) | 69 (25.6) | 29 (10.3) |
| Health insurance | ||||
| None | 27 (4.0) | 3 (2.5) | 19 (7.0) | 5 (1.8) |
| Medicare | 477 (70.9) | 76 (63.3) | 188 (69.4) | 213 (75.5) |
| Medicaid | 143 (21.2) | 20 (16.7) | 51 (18.8) | 72 (25.5) |
| Private insurance | 351 (52.2) | 66 (55.0) | 133 (49.1) | 152 (53.9) |
| Veterans Affairs Benefits Insurance | 32 (4.8) | 10 (8.3) | 12 (4.4) | 10 (3.5) |
Attendance was recorded from 668 (99%) participants. Asians attended significantly more sessions (M = 5.11) than did NHPIs (M = 4.86) and Caucasians (M = 4.79), as determined by one-way analysis of variance (F = 3.04, p = .048) and post hoc tests (p = .042, p = .039). Our 6-month post-test retention rate was 72%. Participants were lost to follow-up because some leaders were unable to organize a reunion, some contact information was lost or inaccurate (impeding ability to collect follow-up data by phone or mail), and 23 participants died or relocated prior to follow-up. However, 422 participants completed both the baseline and 6-month questionnaires.
As shown in Table 3, all CDSMP participants showed significant improvements in social and role activity limitations (Caucasians t = 2.44, p = .018; Asians t = 6.63, p < .001; and NHPIs t = 2.14, p = .034) and significant increases in communication with physicians (Caucasians t = −2.73, p = .009; Asians t = −5.18, p < .001; and NHPIs t = −2.14, p = .017). Asians and NHPIs also realized significant increases in self-rated health (Asians t = 7.67, p < .001 and NHPIs t = 3.48, p < .001) and time spent engaging in stretching/strengthening exercise (Asians t = −5.70, p < .001 and NHPIs t = −2.78, p = .006). Caucasians and Asians showed significant reduction of physical limitations (Caucasians t = 2.63, p = .011 and Asians t = 4.05, p < .001), whereas NHPIs did not.
Table 3.
Summary of Participants’ Health Outcome Results (Total: N = 424, Caucasians: n = 53, Asians: n = 177, and Native Hawaiians and Pacific Islanders [NHPIs]: n = 194)
| Item | Mean |
t | df | Significance | ||
| Baseline (SD) | 6 month (SD) | Change (SD) | ||||
| Self-rated health (1–5, higher score indicates poorer health) | ||||||
| Caucasians | 3.02 (0.99) | 2.91 (1.02) | 0.11 (0.93) | 0.88 | 52 | .381 |
| Asians | 3.09 (0.79) | 2.49 (0.90) | 0.60 (1.03) | 7.67 | 175 | .001 |
| NHPIs | 2.96 (0.80) | 2.76 (0.79) | 0.21 (0.81) | 3.48 | 189 | .001 |
| Health distress (0–5, higher score indicates more distress) | ||||||
| Caucasians | 1.94 (1.24) | 1.56 (1.05) | 0.38 (0.91) | 0.88 | 50 | .005 |
| Asians | 2.05 (1.21) | 1.16 (0.85) | 0.89 (1.29) | 9.15 | 173 | .001 |
| NHPIs | 1.71 (1.36) | 1.55 (1.30) | 0.15 (1.12) | 1.85 | 188 | .066 |
| Symptoms (0–10, higher score indicates more severe symptoms) | ||||||
| Fatigue | ||||||
| Caucasians | 4.65 (2.75) | 3.49 (2.43) | 1.16 (1.91) | 4.32 | 50 | .001 |
| Asians | 3.80 (2.75) | 2.47 (1.90) | 1.33 (2.92) | 6.01 | 174 | .001 |
| NHPIs | 3.56 (2.71) | 3.21 (2.74) | 0.35 (2.56) | 1.89 | 190 | .060 |
| Shortness of breath | ||||||
| Caucasians | 2.57 (2.77) | 2.25 (2.70) | 0.32 (2.16) | 1.08 | 52 | .284 |
| Asians | 2.79 (2.95) | 1.38 (1.80) | 1.41 (2.83) | 6.61 | 175 | .001 |
| NHPIs | 2.67 (2.97) | 2.42 (2.81) | 0.25 (2.69) | 1.28 | 192 | .201 |
| Pain | ||||||
| Caucasians | 3.91 (2.94) | 3.49 (2.73) | 0.42 (2.61) | 1.15 | 52 | .254 |
| Asians | 4.23 (3.08) | 2.36 (2.27) | 1.86 (3.44) | 7.18 | 175 | .001 |
| NHPIs | 3.17 (2.89) | 3.10 (3.01) | 0.01 (2.67) | 0.35 | 191 | .726 |
| Exercise behaviors (minutes per week) | ||||||
| Stretching/strengthening | ||||||
| Caucasians | 39.91 (53.11) | 46.13 (52.61) | −6.23 (49.26) | −0.92 | 52 | .362 |
| Asians | 51.77 (57.05) | 86.14 (67.90) | −34.37 (79.78) | −5.70 | 174 | .001 |
| NHPIs | 52.46 (61.29) | 65.89 (61.44) | −13.43 (66.69) | −2.78 | 190 | .006 |
| Aerobic exercise | ||||||
| Caucasians | 88.02 (100.97) | 101.32 (89.95) | −13.30 (88.58) | −1.09 | 52 | .279 |
| Asians | 102.75 (98.34) | 174.88 (138.77) | −72.14 (135.40) | −7.01 | 172 | .001 |
| NHPIs | 124.49 (117.93) | 142.22 (125.65) | −17.73 (134.59) | −1.80 | 186 | .073 |
| Coping with symptoms (0–5, higher score indicates greater use of skills) | ||||||
| Caucasians | 1.27 (0.99) | 1.57 (1.05) | −0.30 (1.01) | −2.14 | 51 | .037 |
| Asians | 1.46 (0.99) | 2.53 (1.38) | −1.07 (1.54) | −8.80 | 159 | .001 |
| NHPIs | 1.77 (1.19) | 1.84 (1.15) | −0.07 (1.15) | −0.86 | 178 | .394 |
| Social/role activities limitations (0–4, higher score indicates greater limitations) | ||||||
| Caucasians | 1.44 (1.09) | 1.14 (0.97) | 0.29 (0.87) | 2.44 | 51 | .018 |
| Asians | 1.22 (1.18) | 0.62 (0.73) | 0.60 (1.20) | 6.63 | 173 | .001 |
| NHPIs | 0.90 (1.13) | 0.74 (1.06) | 0.16 (1.00) | 2.14 | 186 | .034 |
| Self-rated physical abilities (0–4, higher score indicates greater difficulties) | ||||||
| Caucasians | 0.32 (0.38) | 0.20 (0.27) | 0.12 (0.31) | 2.63 | 48 | .011 |
| Asians | 0.31 (0.44) | 0.17 (0.28) | 0.14 (0.44) | 4.05 | 173 | .001 |
| NHPIs | 0.12 (0.27) | 0.17 (0.38) | −0.05 (0.35) | −2.05 | 189 | .042 |
| Self-efficacy (1–10, higher sore indicates higher self-efficacy) | ||||||
| Caucasians | 6.04 (2.53) | 7.27 (2.39) | −0.87 (2.27) | −2.63 | 46 | .012 |
| Asians | 7.21 (2.32) | 8.56 (1.87) | −1.35 (2.88) | −5.82 | 153 | .001 |
| NHPIs | 7.40 (2.57) | 7.83 (2.58) | −0.43 (3.06) | −1.82 | 167 | .070 |
| Communication with physicians (0–5, higher score indicates better communication with physicians) | ||||||
| Caucasians | 2.32 (1.12) | 2.66 (1.10) | −0.34 (0.90) | −2.73 | 51 | .009 |
| Asians | 1.60 (1.02) | 2.06 (1.17) | −0.46 (1.16) | −5.18 | 174 | .001 |
| NHPIs | 1.90 (1.23) | 2.10 (1.24) | −0.20 (1.14) | −2.41 | 191 | .017 |
| Health care utilization | ||||||
| Physician visit | ||||||
| Caucasians | 5.20 (10.65) | 4.27 (5.16) | 0.92 (8.18) | 0.81 | 50 | .425 |
| Asians | 2.89 (2.79) | 1.99 (1.77) | 0.90 (2.63) | 4.52 | 175 | .001 |
| NHPIs | 3.12 (3.22) | 3.11 (3.61) | 0.01 (3.68) | 0.02 | 186 | .984 |
| ER visit | ||||||
| Caucasians | 0.15 (0.46) | 0.35 (1.30) | −0.19 (1.40) | −0.99 | 51 | .327 |
| Asians | 0.18 (0.48) | 0.12 (0.37) | 0.06 (0.54) | 1.55 | 175 | .124 |
| NHPIs | 0.34 (0.78) | 0.36 (0.98) | −0.02 (1.12) | −0.26 | 191 | .796 |
| Hospitalization | ||||||
| Caucasians | 0.10 (0.36) | 0.10 (0.30) | 0.00 (0.49) | 0.00 | 51 | 1.000 |
| Asians | 0.11 (0.53) | 0.06 (0.24) | 0.05 (0.57) | 1.05 | 176 | .295 |
| NHPIs | 0.20 (0.50) | 0.18 (0.75) | 0.02 (0.78) | 0.37 | 191 | .711 |
| Hospital days | ||||||
| Caucasians | 0.60 (3.03) | 0.31 (1.31) | 0.29 (3.36) | 0.62 | 51 | .538 |
| Asians | 0.33 (0.27) | 0.14 (0.64) | 0.19 (2.78) | 0.92 | 176 | .360 |
| NHPIs | 0.49 (1.98) | 0.34 (1.35) | 0.16 (2.29) | 0.95 | 191 | .346 |
Additionally, Asians reported significant reductions in health distress (t = 9.15, p < .001), fatigue (t = 6.01, p < .001), shortness of breath (t = 6.61, p < .001), pain (t = 7.18, p < .001), and self-reported physician visits (t = 4.52, p = .001). Finding also showed significant increases in time spent in aerobic exercise (t = −7.01, p < .001), ability to cope with symptoms (t = −8.80, p < .001), and self-efficacy (t = −5.82, p < .001).
Program Satisfaction
Most of the 492 participants completing satisfaction surveys heard about CDSMP through AoA-funded providers (65%) or their Area Agency on Aging (9%). They attended the program because they had chronic conditions (74%), wanted to learn self-management (67%), and/or lived with and/or cared for someone with chronic conditions (23%). Other reasons included desire to socialize, help others, prepare for future, and become a CDSMP leader. Participants were very satisfied with the program and leaders (M = 9.77), willing to use the skills they learned from the workshop (M = 9.46), and confident that they could continue to use CDSMP skills to manage their chronic conditions (M = 8.97) and to live independently (M = 9.13).
Implications
Our study demonstrated that CDSMP works well in Hawaii’s API groups with minor changes to the program’s appearance and presentation. We adapted CDSMP for APIs by changing its name, training leaders of the same ethnicity as the elders, and supplementing sessions with activities appropriate and appealing to the local culture. These included prayer for NHPI, a graduation ceremony, one-on-one data collection, local examples, and in-language or Pidgin explanations. High participation, completion, and satisfaction suggest that these modifications enhanced acceptability of the program in Hawaii.
Other researchers have reported on how they have adapted evidence-based programs, including Gitlin and colleagues (2008), who adapted CDSMP for an African American population. We were greatly assisted in our work by the Tracking Changes Tool (NCOA, n.d.), which helped us to deconstruct CDSMP and plan its replication. The adaptation traffic light helped identify the components that could be modified (Centers for Disease Control and Prevention, Division of Reproductive Health & ETR Associates, n.d.). We encourage other communities to use these tools. We also believe that the Aging Network would benefit from guidelines on allowable and unallowable modifications for CDSMP and a compilation of examples of how CDSMP has been adapted for different ethnic groups.
Finding from fidelity monitoring evaluation suggested that leaders from a variety of backgrounds (lay, professional, male, female, Native Hawaiian, Filipino, Caucasian, and Japanese) can lead CDSMP workshops without jeopardizing the program content. Bigger issues for Hawaii were maintaining a pool of trained leaders willing to offer CDSMP. Many of the leaders trained in Hawaii were AoA-funded service providers who sometimes had difficulty finding time to lead the workshops. We lost leaders who changed jobs and/or relocated to the Continental United States. The departure of key program champions required us to step up efforts to train new leaders and nurture more champions for CDSMP. A few leaders had difficulty following the Hawaii evaluation plan and needed refresher sessions on the protocols.
On the other hand, some leaders embraced the program and demonstrated amazing commitment. For example, the coordinator of CDSMP on Maui, who was trained as a leader in 2007, lost 100 pounds by applying CDSMP skills in her own life. Some service providers added CDSMP to staff members’ job descriptions and assured they had time to lead several workshops each year. As other investigators have found, developing strategies to reduce turnover and maintain champions are critical components of program sustainability (Scheirer, 2005).
As previously mentioned, Hawaii has been 1 of the 46 states participating in a nationwide effort to replicate evidenced-based health promotion programs for seniors. This allowed us to compare our data with other programs. Although we were disappointed with our program completion rate of 87%, this compares with 75% of 8,908 participants in 16 states in 2009 (NCOA, 2009) and 74% of 24,606 participants in 45 states in 2011 (NCOA, 2011). We credit our high retention rates to the green- and yellow-light adaptations we made to CDSMP
Although pre- and post-assessments were not required by this initiative, Hawaii was one of several states that collected 6-month follow-up data from participants. Our evaluation findings suggested that the CDSMP modifications did not jeopardize program effectiveness. Six months after the program, many of the API participants, especially Asians, reported improvements in health, coping, exercise behaviors, self-efficacy, and health communication, along with decreases in bothersome symptoms (e.g., fatigue and pain), limitations, and visits to the doctor’s office. Our 6-month findings are similar to those of the original Stanford study (Lorig et al., 1999) as well as others (Fu et al., 2006, 2003; Gitlin et al., 2008; Goeppinger et al., 2007; Griffiths et al., 2005; Kennedy et al., 2007; Lorig et al., 2003; Lorig, Ritter, et al., 2001; Siu et al., 2007; Swerissen et al., 2006).
Interestingly, Asian participants attended more sessions and improved in more measures than did Caucasian or NHPI participants. We examined if perhaps they had fewer chronic diseases coming into CDSMP. In fact, Asians reported the lowest prevalence of heart and lung diseases of the three groups (Table 2). However, Asians also were significantly older than Caucasian and NHPI participants, and 58% reported having hypertension (compared with 47% of Caucasians), 49% reported having arthritis (compared with 38% of NHPIs), and 26% reported having osteoporosis (compared with 10% of NHPIs and 18% of Caucasians).
As noted earlier, Asians in Hawaii tend to be more compliant with health screenings than other ethnic groups. A cross-ethnic analysis of surveillance data from older adults in Hawaii suggested that Japanese and Filipino elders were more likely to participate in annual health checks than Caucasian and Native Hawaiian elders (Braun, Mokuau, & Browne, 2010). It may be that the Asian participants were more willing than the other groups to fully embrace CDSMP and put into practice the knowledge and skills gained from the workshops. Future research could employ multivariate analysis to discern the relative impact of age, preexisting disease, and attendance on self-reported improvements of CDSMP participants.
Efforts to embed evidence-based programs across a state’s Aging Network were time consuming (Tomioka et al., 2009). The HHAP was established to help prepare the Aging Network for this task. Established in 2003, the partnerships spent its first few years building capacity among its government and service-provider members. For example, members were not familiar with concepts like “evidence-based programming,” “research translation,” and “fidelity.” Training was provided to partnership members to increase their skills in assessment, planning, grant writing, adaptation, and evaluation. Training included hands-on operationalization of concepts presented through lecture. Attention to capacity building at the agency level can facilitate program implementation and sustainability (Scheirer, 2005).
As always in community-based research, our research had limitations. Participant data were self-reported and may have been compromised by inability to remember the past correctly (especially the exact timing of a physician or ER visit) and desire to please program providers (Groves et al., 2004; Ritter, Stewart, Kaymaz, Sobel, & Block, 2001). Although a standard evaluation procedure was established, not all sites followed it exactly. We used several methods to collect data from elders, from helping them complete surveys at baseline and reunions, to collecting data by mail and phone when reunions were not possible. We lost seniors over time, although sponsoring a reunion was very helpful in collecting 6-month follow-up data. Finally, we did not have a control or comparison group for this study. CDSMP is an evidence-based program, suggesting that replicators should not have to conduct their own randomized control trials to prove the program’s efficacy if intermediate outcomes (such as self-reported health) are positive.
It required tremendous effort to build provider capacity, to identify and translate evidence-based programs, and to implement new programs statewide. However, based on our study findings, we concluded that CDSMP is modifiable to API communities and that, in its modified form, it is effective in increasing chronic disease self-management skills.
Funding
Funding to replicate Enhance Fitness and the Chronic Disease Self-Management Program in Hawaii comes from the U.S. Administration on Aging, the National Council on Aging, and Atlantic Philanthropies (90AM3117/01, 90AM3117/04, and 90RA0009/01).
Acknowledgments
We acknowledge the HHAP, a coalition of the Executive Office on Aging, the Area Agencies on Aging, the Department of Health, the University of Hawaii, and service providers dedicated to expand health promotion options for older adults in Hawaii.
References
- Agency for Healthcare Research Quality. 2008 National Healthcare Disparities Report. Rockville, MD: U.S. Department of Health and Human Services; 2009. Retrieved from http://www.ahrq.gov/qual/nhdr08/nhdr08.pdf. [Google Scholar]
- Altpeter M, Bryant L, Schneider E, Whitelaw N. Evidence-based health practice: Knowing and using what works for older adults. Home Health Care Services Quarterly. 2006;25:1–11. doi: 10.1300/J027v25n01_01. doi: 10.1300/J027v25n01_01. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freeman; 1997. [Google Scholar]
- Braun KL, Mokuau N, Browne CV. Life expectancy, morbidity, and health practices of Native Hawaiian elders: A review of Hawaii surveillance data. Honolulu, HI: Myron B. Thompson School of Social Work; 2010. [Google Scholar]
- Braun KL, Tsark JU, Santos L, Aitaoto N, Chong C. Building Native Hawaiian capacity in cancer research and programming. Cancer. 2006;107(Suppl. 8):2082–2090. doi: 10.1002/cncr.22157. doi: 10.1002/cncr.22157. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention & Merck Company Foundation. The state of aging and health in America 2007. Whitehouse Station, NJ: The Merck Company Foundation; 2007. Retrieved from http://www.cdc.gov/aging/pdf/saha_2007.pdf. [Google Scholar]
- Centers for Disease Control and Prevention, Division of Reproductive Health & ETR Associates. Adaptation traffic light guide: Green, yellow and red light adaptations. Retrieved November 24, 2010, from www.actforyouth.net/documents/ETR%20Adaptation%20guide.pdf. [Google Scholar]
- Dusenbury L, Barnnigan R, Falco M, Hansen W. A review of research on fidelity of implementation: Implications for drug abuse prevention in school settings. Health Education Research. 2003;18:237–256. doi: 10.1093/her/18.2.237. PMID: 12729182. [DOI] [PubMed] [Google Scholar]
- Elzen H, Slaets JP, Snijders TA, Steverink N. Evaluation of the chronic disease self-management program (CDSMP) among chronically ill older people in the Netherlands. Social Science & Medicine. 2007;64:1832–1841. doi: 10.1016/j.socscimed.2007.02.008. doi:10.1016/j.socscimed.2007.02.00. [DOI] [PubMed] [Google Scholar]
- Fu D, Ding Y, McGowan P, Fu H. Evaluation of Chronic Disease Self Management Program (CDSMP) in Shanghai. Patient Education and Counseling. 2006;64:389–396. doi: 10.1016/j.pec.2005.05.002. doi:10.1016/j.socscimed.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Fu D, Fu H, McGowan P, Shen YE, Zhu L, Yang H, et al. Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: Randomized controlled trial. Bulletin of the World Health Organization. 2003;81:174–182. Retrieved from http://www.who.int/bulletin/volumes/81/3/en/Dongbo0303.pdf. [PMC free article] [PubMed] [Google Scholar]
- Gitlin LN, Chernett NL, Harris LF, Palmer D, Hopkins P, Dennis MP. Harvest health: Translation of the Chronic Disease Self-Management Program for older African Americans in a senior setting. The Gerontologist. 2008;48:698–705. doi: 10.1093/geront/48.5.698. PMID: 18981286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goeppinger J, Armstrong B, Schwartz T, Ensley D, Brady TJ. Self-management education for persons with arthritis: Managing comorbidity and eliminating health disparities. Arthritis Care & Research. 2007;57:1081–1088. doi: 10.1002/art.22896. doi: 10.1002/art.22896. [DOI] [PubMed] [Google Scholar]
- Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomized controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease. Journal of General Practice. 2005;55:831–837. PMCID: PMC1570787. [PMC free article] [PubMed] [Google Scholar]
- Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey methodology. Hoboken, NJ: Wiley; 2004. [Google Scholar]
- Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, et al. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. Canadian Medical Association Journal. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. doi:10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawaii’s Department of Health. Hawaii Health Survey 2008. 2009. Retrieved October 15, 2010, from http://hawaii.gov/health/statistics/vital-statistics/hhs/hhs_08/hhs08t11.pdf. [Google Scholar]
- Hawaii Executive Office on Aging. Profile of Hawaii's older adults and their caregivers: 2006. 2006. Retrieved June 3, 2010, from Reports on Elderly Issues and Family Caregiving: http://hawaii.gov/health/eoa/Docs/2006.pdf. [Google Scholar]
- He W, Sengupta M, Velkoff VA, DeBarros KA. 65+ in the United States: 2005—U.S. Census Bureau. Washington, DC: Government Printing Office; 2005. Retrieved from http://www.census.gov/prod/2006pubs/p23-209.pdf. [Google Scholar]
- Kennedy A, Reeves D, Bower P, Lee V, Middleton E, Richardson G, et al. The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: a pragmatic randomised controlled trial. Journal of Epidemiology and Community Health. 2007;61:254–261. doi: 10.1136/jech.2006.053538. doi:10.1136/jech.2006.053538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam CL, Lauder IJ. The impact of chronic diseases on the health-related quality of life (HRQOL) of Chinese patients in primary care. Family Practice. 2000;17:159–166. doi: 10.1093/fampra/17.2.159. doi: 10.1093/fampra/17.2.159. [DOI] [PubMed] [Google Scholar]
- Lorig K, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, Gonzalez VM. Hispanic chronic disease self-management: A randomized community-based outcome trial. Nursing Research. 2003;52:361–369. doi: 10.1097/00006199-200311000-00003. doi: 10.1097/00006199-200311000-00003. [DOI] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Stewart A, Sobel D, Brown BW, Bandura A, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39:1217–1223. doi: 10.1097/00005650-200111000-00008. PMID: 11606875. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinical Practice. 2001;4:256–262. PMID: 11769298. [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization. Medical Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- National Council on Aging. AoA Evidence-Based Programs. Washington, DC: Author; 2009. (Tech. Rep. 10/1/2006-7/31/2009, November 24th, 2009) [Google Scholar]
- National Council on Aging. CDSMP Weekly Update. Washington, DC: Author; 2011. (Tech. Rep. CDSMP Weekly Update, January 7th, 2011) [Google Scholar]
- National Council on Aging. Evidence-based: Healthy aging programming: Tools and checklists. Retrieved April 16, 2011 from http://www.ncoa.org/news-ncoa-publications/publications/cha_tools_checklists.pdf. [Google Scholar]
- Park CB, Braun KL, Horiuchi BY, Tottori C, Onaka AT. Longevity disparities in multiethnic Hawaii: An analysis of 2000 life tables. Public Health Reports. 2009;124:579–584. doi: 10.1177/003335490912400415. PMID: 19618795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson EW. Using cognitive behavioral strategies to reduce fear of falling: A matter of balance. Generations. 2003;26:53–59. Tool Retrieved January 15, 2011 from http://www.healthyagingprograms.org/content.asp?sectionid=66&ElementID=336. [Google Scholar]
- Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA. Self-reports of health care utilization compared to provider records. Journal of Clinical Epidemiology. 2001;54:136–141. doi: 10.1016/s0895-4356(00)00261-4. doi: 10.1016/S0895-4356(00)00261-4. [DOI] [PubMed] [Google Scholar]
- Scheirer MA. Is sustainability possible? A review and commentary on empirical studies of program sustainability. American Journal of Evaluation. 2005;26:320–347. doi: 10.1177/1098214005278752. [Google Scholar]
- Siu AM, Chan CC, Poon PK, Chui DY, Chan SC. Evaluation of the Chronic Disease Self-Management Program in a Chinese population. Patient Education and Counseling. 2007;65:42–50. doi: 10.1016/j.pec.2006.04.013. doi:10.1016/j.pec.2006.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprangers MA, De Regt EB, Andries F, Van Agt HM, Bijl RV, De Boer JB, et al. Which chronic conditions are associated with better or poorer quality of life? Journal of Clinical Epidemiology. 2000;53:895–907. doi: 10.1016/s0895-4356(00)00204-3. doi: 10.1016/S0895-4356(00)00204-3. [DOI] [PubMed] [Google Scholar]
- Stanford Patient Education Research Center. Stanford patient education research center. 2006. Retrieved June 24, 2006, from http://patienteducation.stanford.edu/ [Google Scholar]
- Swerissen H, Belfrage J, Weeks A, Jordan L, Walker C, Furler J, et al. Randomized control trial of a Self-Management Program for people with a chronic illness from Vietnamese, Chinese, Italian and Greek backgrounds. Patient Education and Counseling. 2006;64:360–368. doi: 10.1016/j.pec.2006.04.003. doi:10.1016/j.pec.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Tomioka M, Tom T, Higuchi P, Kidani S, Pendleton N, Yamashita B, et al. The Hawaii Healthy Aging Partnership: Partnership development—An investment for program success. Hawaii Journal of Public Health. 2009;2:20–31. Retrieved from http://hawaii.gov/health/hjph/Volumes/Volume2.1.pdf. [Google Scholar]
- Tsark J. Braun KL the Cancer Council of the Pacific Island. Reducing cancer health disparities in the US-associated Pacific. Journal of Public Health Management and Practice. 2007;13:49–58. doi: 10.1097/00124784-200701000-00009. PMID: 17149100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Administration on Aging. AoA evidence-based prevention program. Washington, DC: U.S. Department of Health and Human Services, Administration on Aging; 2010. [Google Scholar]
- U.S. Census Bureau. U.S. Census Bureau News: Dramatic changes in U.S. aging highlighted in new census. Washington, DC: U.S. Department of Commerce; 2006. [Google Scholar]
- U.S. Census Bureau. Hawaii. 2010. Retrieved June 23, 2010, from State & County QuickFacts: http://quickfacts.census.gov/qfd/states/15000.html. [Google Scholar]


