Summary
Objective
Malalignment is associated with knee osteoarthritis (KOA), however, the optimal anatomic axis (AA) knee alignment measurement on a standard limb radiograph (SLR) is unknown. This study compares one-point (1P) and two-point (2P) AA methods using three knee joint centre locations and examines cross-sectional associations with symptomatic radiographic knee osteoarthritis (SRKOA), radiographic knee osteoarthritis (RKOA) and knee pain.
Methods
AA alignment was measured six different ways using the KneeMorf software on 1058 SLRs from 584 women in the Chingford Study. Cross-sectional associations with principal outcome SRKOA combined with greatest reproducibility determined the optimal 1P and 2P AA method. Appropriate varus/neutral/valgus alignment categories were established using logistic regression with generalised estimating equation models fitted with restricted cubic spline function.
Results
The tibial plateau centre displayed greatest reproducibility and associations with SRKOA. As mean 1P and 2P values differed by >2°, new alignment categories were generated for 1P: varus <178°, neutral 178–182°, valgus >182° and for 2P methods: varus <180°, neutral 180–185°, valgus >185°. Varus vs neutral alignment was associated with a near 2-fold increase in SRKOA and RKOA, and valgus vs neutral for RKOA using 2P method. Nonsignificant associations were seen for 1P method for SRKOA, RKOA and knee pain.
Conclusions
AA alignment was associated with SRKOA and the tibial plateau centre had the strongest association. Differences in AA alignment when 1P vs 2P methods were compared indicated bespoke alignment categories were necessary. Further replication and validation with mechanical axis alignment comparison is required.
Keywords: Anatomic axis, Knee alignment, Knee osteoarthritis, Radiography
Introduction
Knee osteoarthritis (KOA) is a major health burden with a 45% projected lifetime risk1, and accounts for the majority of total knee replacements (TKRs) leading to TKR rates trebling between 1991 and 20062. Its aetiology is multifactorial. Knee alignment is a known risk factor for KOA progression3, 4, 5, 6, 7, 8 with data on incidence being less clear3, 8, 9, 10. Malalignment either, varus or valgus influences load distribution across the knee joint, leading to subsequent degenerative changes11.
The gold standard alignment measurement is the mechanical axis (MA) measuring the hip–knee–ankle angle on a full limb radiograph (FLR)12, 13. Drawbacks with this are radiation exposure and specialist radiography equipment and expertise makes it costly. A proposed alternative alignment measurement, the anatomic axis (AA) method, is comparable to the MA method5, 14, 15, 16, 17, 18. The AA method measures the femoral–tibial angle on a standard limb radiograph (SLR) which unlike FLRs are typically obtained in clinical practice, thereby allowing alignment measurements in existing population cohort studies. Less radiation is received, making it safer and more cost-effective.
Consensus defining the optimal AA alignment method is not agreed19. Current literature contains variation in measurement technique using different knee joint centres (KJCs); tibial spine base mid-point8, tibial spine tips mid-point9, 16, 18, 20, 21, or unspecified centre of tibial spines14, 15, 22, 23.
In addition, the majority of AA alignment studies use a one-point (1P) AA method which measures the AA angle formed between the femoral anatomic axis (FAA) and the tibial anatomic axis (TAA) based on a single 1P KJC location. However, most MA alignment studies use a two-point (2P) method where the angle measured is formed by two separate axes: the femoral axis originating from the femoral head centre to the femoral intercondylar notch point, and the tibial axis originating from the KJC location to the ankle tibial plafond mid-point. More recent MA vs AA comparative alignment studies5, 17, 24 use a 2P AA vs a 2P MA method, but it is not clear if using a 1P or 2P AA method is optimum.
Previous work by McDaniel19 comparing performance metrics of AA methods using different KJCs against the gold standard MA method recommended standardising AA measurements using either tibial spine base mid-point or centre of tibia, and suggested comparing 1P and 2P methods in larger studies. Past studies examining alignment and KOA predominantly use radiographic knee osteoarthritis (RKOA) as their main clinical outcome which is limited as symptoms are not considered3, 4, 6, 7, 8, 9, 10, 25. This study uses symptomatic radiographic knee osteoarthritis (SRKOA) as the primary outcome which is relevant for both clinical diagnosis and for measuring the true KOA public health burden1, 26. We are not aware of alignment studies using pain as an outcome therefore knee pain, in addition to RKOA, are included as secondary outcomes. This cross-sectional AA alignment study has the following aims:
-
1)
To determine the optimal 1P and 2P AA method based on reproducibility and associations with clinical outcomes.
-
2)
To define appropriate varus, neutral and valgus alignment categories for the chosen method.
-
3)
To describe cross-sectional associations of the chosen method with SRKOA, RKOA and knee pain.
Method
Study population
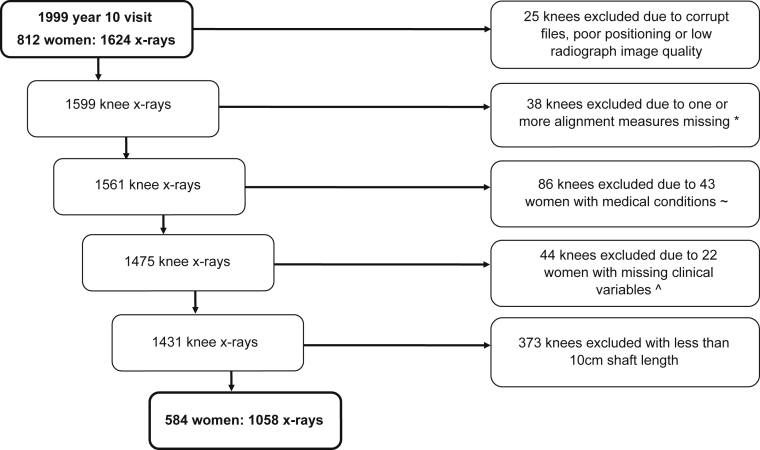
The Chingford Study is a prospective cohort study of osteoarthritis and osteoporosis comprising 1003 women aged 44–67 years at baseline derived from a general practice register in Chingford, whose demographic characteristics are similar to the UK population27. Women attending the year 10 (Y10) visit with accompanying knee SLRs and clinical variables were included in this study (Fig. 1)and their clinical characteristics are shown in Table 1.
Fig. 1.
Derivation of cross-sectional analysis sample of 1058 knees. *Total knee replacements (TKRs) and uni-condylar knee replacements (UKR) knees excluded as AA alignment measurements unobtainable with a prosthesis in situ (n = 8 knees). ∼Excluded medical conditions: rheumatoid arthritis, lupus, psoriatic arthritis, polymyalgia rheumatica, gout, fibromyalgia, Paget's disease, polio, Parkinson's disease, multiple sclerosis, stroke, cerebral palsy or chronic inflammatory demyelinating neuropathy. ˆMissing clinical variables: age, body mass index, or presence of knee injury.
Table I.
Clinical characteristics. Where AA = anatomic axis, BMI = body mass index, IQR = interquartile range, KJC = knee joint centre, K&L = Kellgren & Lawrence grade, n = number, RKOA = radiographic knee osteoarthritis, SD = standard deviation, SRKOA = symptomatic radiographic knee osteoarthritis, 1P = one-point, 2P = two-point
| Characteristic | Included Y10 cohort (n = 1058 knees) | Excluded Y10 cohort (n = 566 knees) | P value∗ |
|---|---|---|---|
| Age, median (IQR) years | 62 (57–67) | 63 (57–69) | 0.004 |
| BMI, median (IQR) kg/m2 | 26.2 (23.6–29.3) | 26.3 (23.4–29.7) | 0.69 |
| Knee injury, % | 16.5 | 15.9 | 0.78 |
| Knee pain ≥15 days, % | 13.4 | 15.4 | 0.28 |
| RKOA ≥2 K&L grade, % (n) | 27.9 | 27.9 (n = 544) | 0.98 |
| SRKOA, % (n) | 6.1 | 8.3 (n = 544) | 0.09 |
| Mean AA angle° (±SD) (n) | |||
| 1P KJC1 | 180.23 (3.70) | ||
| 1P KJC2 | 182.72 (3.40) | ||
| 1P KJC3 | 180.11 (2.93) | ||
| 2P KJC1 | 182.47 (2.78) | ||
| 2P KJC2 | 183.64 (2.66) | ||
| 2P KJC3 | 182.53 (2.51) | ||
Statistically significant P value is represented in bold.
P values compare age and BMI using Kruskal Wallis test; knee injury, knee pain, RKOA and SRKOA using chi-square test.
Imaging
Antero-posterior (AP) fully extended weight bearing bilateral knee SLRs were taken using a standardised protocol established at baseline and repeated for subsequent radiograph visits28. Plain film SLRs were digitally scanned at 600 pixels per inch (ppi) with a grey scale pixel depth of 16 bits allowing computerised alignment readings to be made.
All Y10 radiographs were graded (DJH) for Kellgren & Lawrence (K&L)29, 30, osteophytes and joint space narrowing (JSN) using the Chingford Atlas31. Radiographs were read individually, blinded to clinical information. Good intraobserver reproducibility was previously reported32.
Alignment measurement
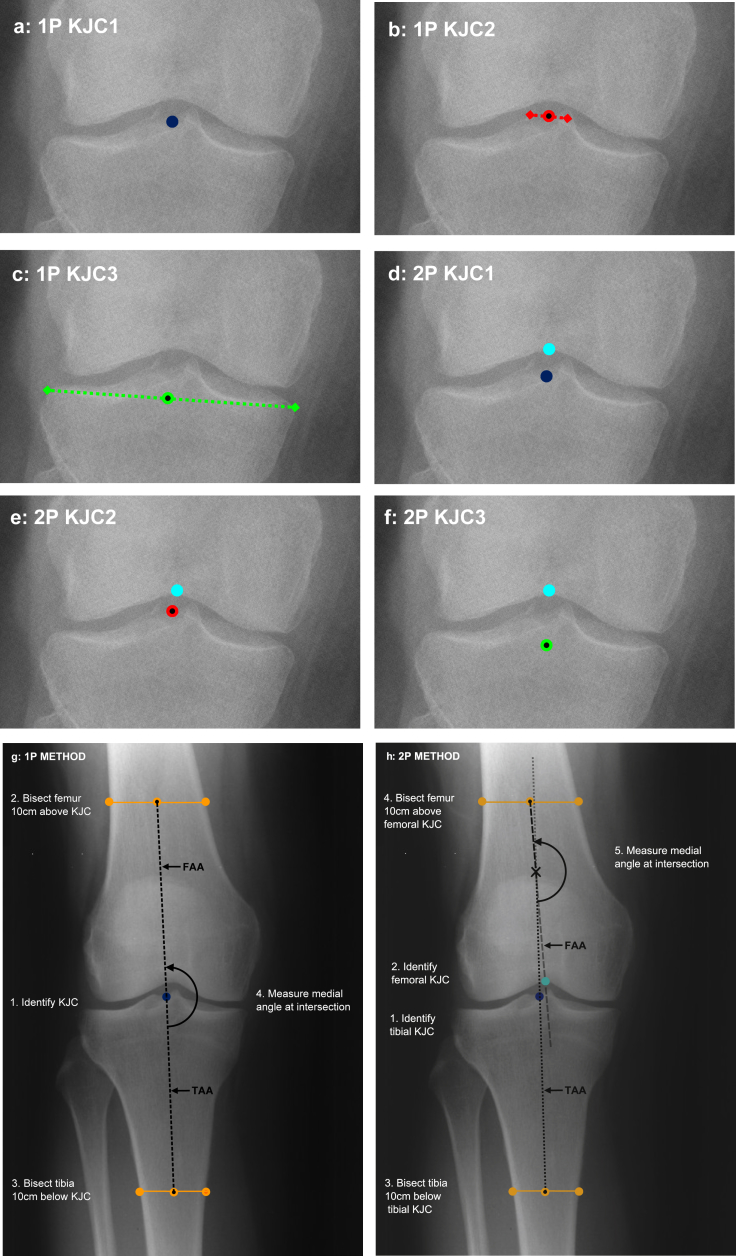
AA alignment was measured by manually placing points on each SLR image using the KneeMorf computer software33, 34. A total of six, three 1P [Fig. 2(a)–(c)] and three 2P [Fig. 2(d)–(f)] methods of measuring AA were tested using three tibial KJCs:
-
a)
tibial spine base mid-point (KJC1)
-
b)
tibial spine tips mid-point (KJC2)
-
c)
tibial plateau centre (KJC3)
Fig. 2.
One-point and two-point method knee joint centre locations. Where 1P = one-point; 2P = two-point; KJC = knee joint centre; KJC1 = tibial spine base mid-point; KJC2 = tibial spine tips mid-point; KJC3 = tibial plateau centre; FAA = femoral anatomic axis; TAA = tibial anatomic axis. (a) one-point method at tibial spine base mid-point; (b) one-point method at tibial spine tips mid-point; (c) one-point method at tibial plateau centre defined by line connecting lateral and medial margins of tibial plateau (excluding marginal osteophytes); (d) two-point method using femoral notch and tibial spine base mid-point; (e) two-point method using femoral notch and tibial spine tips mid-point; (f) two-point method using femoral notch and tibial plateau centre; (g) describing one-point method; (h) describing two-point method.
For the three 1P methods the AA angle is formed between the FAA and TAA based on each of the KJC locations above [Fig. 2(g)]. For the three 2P methods the AA angle is formed by two axes, the FAA originating from the femoral intercondylar notch point and the TAA originating from each of the KJC locations above [Fig. 2(h)].
The femoral shaft length guiding rule line was placed 10 cm above the KJC location and parallel to the femoral condyle tangent line; the tibial shaft length guiding rule was placed 10 cm below the KJC location and parallel to the tibial plateau tangent line. The end points for the femoral and tibial 10 cm shaft length guiding rule lines were always placed on the outer femoral and tibial bone shaft cortex20.
All Y10 SLRs were measured for alignment in 50 image batches by one reader (LMG). They were read individually, in a random order and blinded to clinical information. The intraclass correlation coefficients (ICCs) for intrareader reproducibility (Table II) for one set of 50 images (read twice 1 week apart) for all six AA measurements were high between 0.97 and 0.99. All the 95% limits of agreement (LoA) were similar although 1P KJC1 (−1.52, 2.78) and 2P KJC1 (−0.98, 1.67) were greatest.
Table II.
Intrareader Bland–Altman plot agreement parameters and ICCs. Where 1P = one-point, 2P = two-point, CI = confidence interval, ICC = intraclass coefficient, KJC = knee joint centre, LoA = limits of agreement, SD = standard deviation, SE = standard error (all units in degrees unless otherwise stated)
| n = 50 method | Mean diff. | SD of diff. | SE of mean diff. | 95% CI for mean diff. | 95% LoA | ICC | 95% CI | P value |
|---|---|---|---|---|---|---|---|---|
| 1P KJC1 | −0.63 | 1.10 | 0.15 | 0.31, 0.94 | −1.52, 2.78 | 0.97 | 0.95, 0.98 | <0.001 |
| 1P KJC2 | 0.11 | 0.77 | 0.11 | −0.11, 0.33 | −1.40, 1.63 | 0.99 | 0.98, 0.99 | <0.001 |
| 1P KJC3 | 0.11 | 0.67 | 0.09 | −0.08, 0.30 | −1.20, 1.42 | 0.99 | 0.98, 0.99 | <0.001 |
| 2P KJC1 | 0.35 | 0.68 | 0.10 | 0.16, 0.54 | −0.98, 1.67 | 0.98 | 0.97, 0.99 | <0.001 |
| 2P KJC2 | 0.10 | 0.54 | 0.08 | −0.06, 0.25 | −0.96, 1.16 | 0.99 | 0.98, 0.99 | <0.001 |
| 2P KJC3 | 0.09 | 0.56 | 0.08 | −0.06, 0.26 | −1.00, 1.20 | 0.99 | 0.98,0.99 | <0.001 |
Outcome variables
All outcomes were knee-based and decided a priori. The primary outcome variable was SRKOA as we considered this more clinically important to predict; RKOA and knee pain were secondary outcomes.
SRKOA was classified positive in K&L grade 2 or above knees reporting ≥15 days of knee pain in the previous month. All remaining knees were classified SRKOA negative.
RKOA was classified positive in K&L grade 2 or above knees. All remaining knees with K&L grades 0 and 1 were classified RKOA negative.
Knee pain was assessed using a modified National Health and Nutrition Examination Survey35 question in two parts for right and left knees: (1) “Have you had any knee pain in the last month?” and (2) “How many days of knee pain have you experienced in the last month?” Knee pain was classified positive if “yes” and “≥15 days”. All remaining knees were classified knee pain negative.
Clinical variables
Body weight, height and age data were collected as previously reported36. Body mass index (BMI) in kg/m2 was calculated and used as a continuous variable in analyses, as was age. For injury a knee specific question at Y10 was combined with person-level questions at years 1 and 2 to calculate a cumulative person-level knee injury by Y10 yes/no variable.
Statistical analyses
All analysis was completed using Stata version 13.0 (Stata Corp, College Station, Texas, USA). The clinical characteristics for included and excluded subjects were examined using Kruskal-Wallis tests and chi-square tests. Bland–Altman plots and ICCs for intrareader reproducibility were calculated. Pearson correlation coefficients were completed to determine the statistical significance of associations between each of the six AA alignment methods. Cross-sectional associations with clinical outcomes were compared using clustered t-tests to account for correlated knees that provide clustered data within women37. AA mean angle differences were considered clinically significant if greater than 1°38.
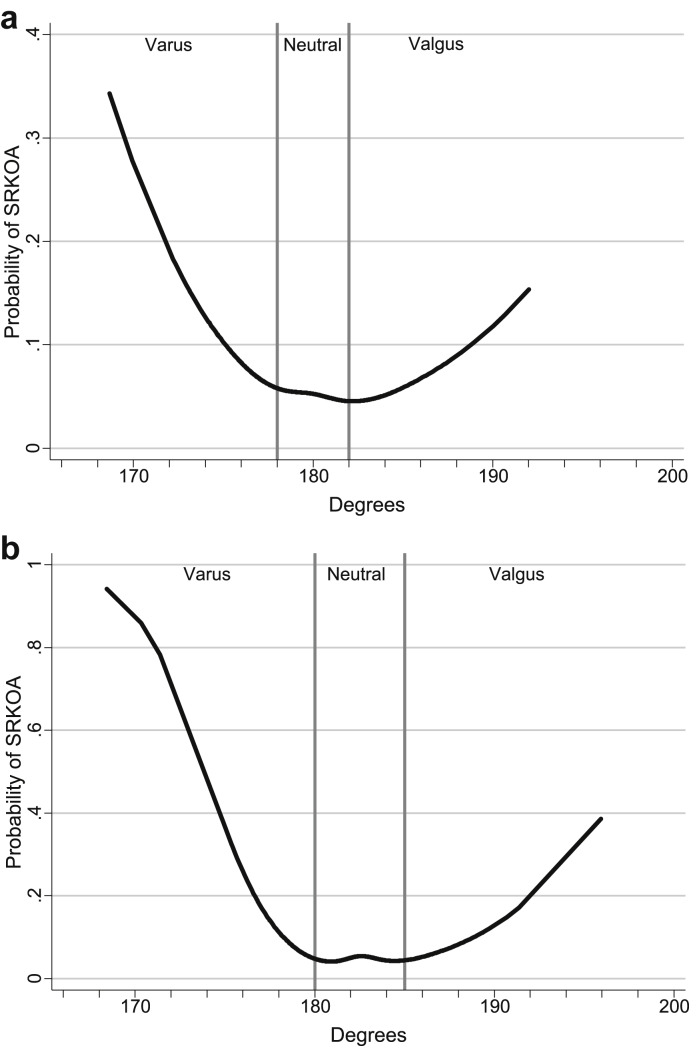
Logistic regression with generalized estimating equations (GEE) was used to account for correlation between both knees in one individual. Using SRKOA, similar steps to those followed by Heim39, were used to establish appropriate AA alignment category cut-off values:
-
1)
1P and 2P AA angles were plotted against SRKOA outcome using restricted cubic spline regression functions with five knots. Optimal cut-off values for varus/neutral/valgus knee alignment categories with SRKOA were assessed by visual inspection by three independent readers (NKA, LMG and MTS). A priori, the consensus for optimal alignment cut-off values was set where the probability of SRKOA outcome starts to decrease more rapidly for varus and increase more rapidly for valgus. The mean of the three values was calculated and rounded to the nearest degree to generate appropriate new varus/neutral/valgus categories for each method.
-
2)
Model fit using the original and new alignment categories was assessed using the Quasilikelihood under the Independence Criterion (QIC)40.
-
3)
Cross-sectional associations controlling for clinical variables (age, BMI and injury) were performed using neutral as the reference group.
GEE analyses were repeated for RKOA and knee pain outcomes, and sensitivity analyses were completed for SRKOA and knee pain outcomes. SRKOA positive knees were compared to RKOA negative (K&L grades 0 or 1) and knee pain negative (no pain in the preceding month); and knee pain positive knees were compared to knee pain negative knees. A further sensitivity analysis examined associations between medial and lateral JSN for RKOA risk in varus and valgus knees respectively.
Results
Study population
A total of 1058 knees from 584 women were included in this study (Fig. 1). Table I shows clinical characteristics for included and excluded women attending the Y10 visit. Although included women were slightly younger this difference was not clinically significant and all other characteristics were similar.
Choosing optimal 1P and 2P method
All six alternative AA methods were highly correlated with each other and were statistically significant at P < 0.001 (Supplementary Table 1). All 1P methods were correlated with each other r = 0.84–0.91. The 2P methods were more strongly correlated r = 0.93–0.96; 1P vs 2P correlations were weaker, r = 0.77–0.91. Table III calculates cross-sectional associations using clustered t-tests between each AA method and clinical outcomes. The mean AA angles at all three KJCs using a 2P method are all greater (i.e., more valgus) than the same 1P method angles across all three outcomes. None of the three 1P KJCs were significantly different, although KJC3 showed the greatest mean difference (0.63°) in knees with and without SRKOA. For the 2P method KJC3 had the greatest mean difference (1.02°) being statistically (P = 0.01) and clinically significantly associated with SRKOA. In addition both 1P and 2P KJC3 displayed excellent intrareader reproducibility with ICCs at 0.99 (95% confidence interval or CI 0.98, 0.99), least mean differences and narrow 95% LoA of (−1.20, 1.42) for 1P and (−1.00, 1.20) for 2P KJC3 (Table II); and similarly for interreader reproducibility (50 images read once by two readers) with ICCs at 0.98 (95% CI 0.97, 0.99), least mean differences and narrow 95% LoA of (−1.49, 1.36) for 1P and (−1.49, 1.10) for 2P KJC3 (Supplementary Table 2). As the more consistently reliable measure, KJC3, the tibial plateau centre, was chosen for further alignment analyses.
Table III.
Clustered t-test cross-sectional associations with clinical outcomes. Where 1P = one-point, 2P = two-point, CI = confidence interval, KJC = knee joint centre, K&L = Kellgren & Lawrence grade, RKOA = radiographic knee osteoarthritis, SRKOA = symptomatic radiographic knee osteoarthritis, SD = standard deviation. All values shown are in degrees unless otherwise stated
| n = 1058 method | Knee pain (≥15 days) |
RKOA (≥2 K&L) |
SRKOA (≥2 K&L & ≥15 days) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| −(n = 916) Mean (±SD) (95% CI) | +(n = 142) Mean (±SD) (95% CI) | P value | −(n = 763) Mean (±SD) (95% CI) | +(n = 295) Mean (±SD) (95% CI) | P value | (n = 994) Mean (±SD) (95% CI) | +(n = 64) Mean (±SD) (95% CI) | P value | |
| 1P KJC1 | 180.18 (4.62) (179.88, 180.48) | 180.55 (4.57) (179.78, 181.31) | 0.38 | 180.07 (4.60) (179.75, 180.40) | 180.65 (4.62) (180.12, 181.18) | 0.07 | 180.23 (4.61) (179.94, 180.52) | 180.26 (4.61) (179.10, 181.42) | 0.96 |
| 1P KJC2 | 182.68 (4.28) (182.40, 182.95) | 182.97 (4.24) (182.26, 183.67) | 0.45 | 182.57 (4.27) (182.27, 182.87) | 183.09 (4.28) (182.60, 183.59) | 0.07 | 182.73 (4.28) (182.47, 183.00) | 182.46 (4.27) (181.39, 183.54) | 0.63 |
| 1P KJC3 | 180.11 (3.63) (179.87, 180.34) | 180.12 (3.59) (179.52, 180.72) | 0.98 | 180.07 (3.62) (179.81, 180.32) | 180.23 (3.63) (179.81, 180.64) | 0.52 | 180.15 (3.62) (179.92, 180.37) | 179.52 (3.61) (178.61, 180.43) | 0.18 |
| 2P KJC1 | 182.47 (3.52) (182.24, 182.70) | 182.44 (3.49) (181.86, 183.03) | 0.94 | 182.43 (3.52) (182.18, 182.68) | 182.57 (3.53) (182.16, 182.97) | 0.55 | 182.50 (3.51) (182.28, 182.72) | 181.88 (3.51) (181.00, 182.77) | 0.17 |
| 2P KJC2 | 183.65 (3.39) (183.43, 183.87) | 183.60 (3.35) (183.04, 184.15) | 0.87 | 183.61 (3.38) (183.37, 183.85) | 183.72 (3.39) (183.33, 184.11) | 0.62 | 183.68 (3.37) (183.48, 183.89) | 182.94 (3.36) (182.10, 183.79) | 0.09 |
| 2P KJC3 | 182.56 (3.17) (182.35, 182.76) | 182.34 (3.13) (181.82, 182.87) | 0.45 | 182.55 (3.16) (182.33, 182.78) | 182.46 (3.17) (182.10, 182.83) | 0.67 | 182.59 (3.15) (182.39, 182.79) | 181.57 (3.14) (180.78, 182.37) | 0.01 |
Statistically significant P value is represented in bold.
Choosing optimal alignment categories
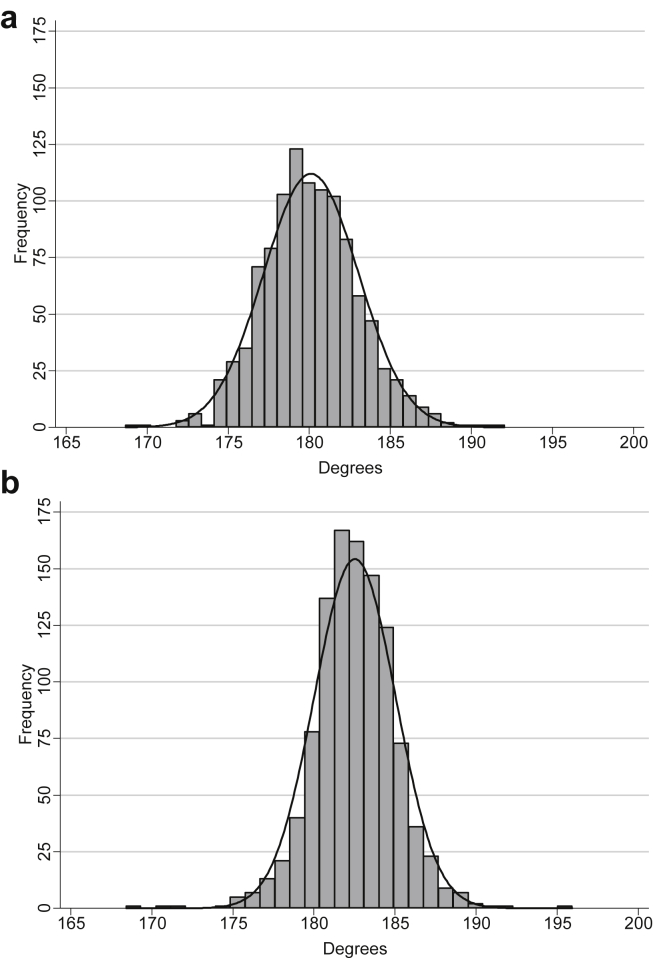
Fig. 3 shows histograms for chosen 1P and 2P KJC3 methods. Although both are normally distributed, the 2P method shows less variation (2P SD ± 2.51° vs 1P SD ± 2.93°) and displays a greater mean value of approximately 2°, compared to the 1P method indicating differences between 1P and 2P methods. The varus (<178°), neutral (178–182°) and valgus (>182°) alignment categories adopted from Colebatch16 (who studied AA vs MA alignment in a female healthy population with AP FLRs images) applied to the 1P method would be inappropriate for the 2P method. A nonlinear relationship between AA alignment and SRKOA for both methods was shown and new alignment cut-off values were defined using cubic spline regression curves (Fig. 4). Based on visual inspection the new alignment categories generated for 1P method were varus <178°, neutral 178–182° and valgus >182° and for the 2P method were varus <180°, neutral 180–185° and valgus >185°.
Fig. 3.
Histograms of chosen (a) 1P KJC3 and (b) 2P KJC3 methods.
Fig. 4.
| Fig. 4a | Fig. 4b |
| 1P KJC3 | 2P KJC3 |
| Reader 1 (NKA): 178.0–182.5° | Reader 1 (NKA): 180.5–184.5° |
| Reader 2 (LMG): 177.5–182.5° | Reader 2 (LMG): 180.5–185.5° |
| Reader 3 (MTS): 178.0–182.0° | Reader 3 (MTS): 180.0–185.5° |
| Mean: 177.8–182.3° | Mean: 180.3–185.0° |
| Rounded to: 178.0–182.0° | Rounded to: 180.0–185.0° |
Model fit with original and new alignment categories
Table IV shows the new alignment categories for 2P KJC3 classified a greater number of knees as neutral (n = 778) with a closer varus (n = 134) and valgus (n = 146) split than the previous alignment categories which classified the majority of knees as valgus (n = 613). The new categories provided slightly lower odds ratios with tighter 95% CIs for mainly varus knees for all three outcomes than the original categories. The QIC values suggest there is little difference for SRKOA outcome but for RKOA the new categories show a better fit with lower QIC values. The reverse is true when it comes to knee pain with slightly lower QIC values seen for original categories compared to new categories.
Table IV.
Cross-sectional GEE association with clinical outcomes by alignment classification for chosen methods. Where 1P = one-point, 2P = two-point, KJC = knee joint centre, KJC3 = tibial plateau centre, K&L = Kellgren & Lawrence grade, QIC = quasi-likelihood under the independence model criterion, RKOA = radiographic knee osteoarthritis, SD = standard deviation, SRKOA = symptomatic radiographic knee osteoarthritis. *Adjusted for Y10 age, BMI and knee injury. ˆUses original 2P categories
| Method (n = 1058 knees) | Knee pain (≥15 days) |
RKOA (≥2 K&L) |
SRKOA (≥2 K&L & ≥15 days) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| −(n = 916) |
+(n = 142) |
QIC | −(n = 763) |
+(n = 295) |
QIC | −(n = 994) |
+(n = 64) |
QIC | ||
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |||||
| 1P KJC3 | Neutral 178–182° (n = 555) | n = 488 | n = 67 |
1248 1240* |
n = 414 | n = 141 |
1869 1636* |
n = 529 | n = 26 |
776 735* |
| Reference | 1.0 (−) | – | 1.0 (−) | – | 1.0 (−) | – | ||||
| Varus <178° (n = 245) | n = 213 | n = 32 | n = 172 | n = 73 | n = 225 | n = 20 | ||||
| Unadjusted | 0.99 (0.70, 1.39) | 0.95 | 1.08 (0.79, 1.48) | 0.62 | 1.59 (0.96, 2.63) | 0.07 | ||||
| Adjusted* | 0.98 (0.70, 1.37) | 0.90 | 1.13 (0.79, 1.61) | 0.49 | 1.57 (0.97, 2.54) | 0.07 | ||||
| Valgus >182° (n = 258) | n = 215 | n = 43 | n = 177 | n = 81 | n = 240 | n = 18 | ||||
| Unadjusted | 1.19 (0.87, 1.63) | 0.26 | 1.01 (0.74, 1.38) | 0.93 | 1.17 (0.69, 1.98) | 0.56 | ||||
| Adjusted* | 1.14 (0.84, 1.56) | 0.39 | 0.88 (0.63, 1.25) | 0.48 | 1.04 (0.64, 1.71) | 0.86 | ||||
| 2P KJC3 | Neutral 180–185° (n = 778) | n = 682 | n = 96 |
1248 1241* |
n = 602 | n = 176 |
1822 1612* |
n = 746 | n = 32 |
758 723* |
| Reference | 1.0 (−) | – | 1.0 (−) | – | 1.0 (−) | – | ||||
| Varus <180° (n = 134) | n = 113 | n = 21 | n = 78 | n = 56 | n = 116 | n = 18 | ||||
| Unadjusted | 0.98 (0.64, 1.48) | 0.92 | 1.82 (1.26, 2.64) | 0.002 | 2.24 (1.28, 3.95) | 0.005 | ||||
| Adjusted* | 0.92 (0.62, 1.39) | 0.70 | 1.81 (1.20, 2.73) | 0.005 | 1.86 (1.10, 3.15) | 0.02 | ||||
| Valgus >185° (n = 146) | n = 121 | n = 25 | n = 83 | n = 63 | n = 132 | n = 14 | ||||
| Unadjusted | 1.21 (0.82, 1.77) | 0.33 | 2.01 (1.26, 2.64) | <0.001 | 1.40 (0.74, 2.64) | 0.30 | ||||
| Adjusted* | 1.14 (0.78, 1.66) | 0.49 | 1.79 (1.20, 2.66) | 0.004 | 1.15 (0.64, 2.08) | 0.64 | ||||
| Original 2P KJC3ˆ | Neutral 178–182° (n = 408) | n = 360 | n = 48 |
1243 1236* |
n = 294 | n = 114 |
1849 1624* |
n = 386 | n = 22 |
758 724* |
| Reference | 1.0 (−) | – | 1.0 (−) | – | 1.0 (−) | – | ||||
| Varus <178° (n = 37) | n = 27 | n = 10 | n = 16 | n = 21 | n = 27 | n = 10 | ||||
| Unadjusted | 2.40 (1.21, 4.79) | 0.01 | 2.12 (1.07, 4.20) | 0.03 | 4.86 (2.09, 11.28) | <0.001 | ||||
| Adjusted* | 2.03 (1.03, 4.02) | 0.04 | 1.96 (0.91, 4.19) | 0.08 | 3.25 (1.43, 7.37) | 0.005 | ||||
| Valgus >182° (n = 613) | n = 529 | n = 84 | n = 453 | n = 160 | n = 581 | n = 32 | ||||
| Unadjusted | 1.25 (0.92, 1.70) | 0.15 | 0.83 (0.63, 1.09) | 0.17 | 1.09 (0.66, 1.80) | 0.74 | ||||
| Adjusted* | 1.25 (0.92, 1.70) | 0.15 | 0.78 (0.58, 1.06) | 0.12 | 1.08 (0.67, 1.76) | 0.74 | ||||
AA alignment and clinical outcomes
Varus vs neutral alignment knees had significantly higher odds of SRKOA using the 2P method and this association remained significant when adjusted (Table IV). A similar, but nonsignificant trend was seen for the 1P method. Valgus compared with neutral alignment was not significantly associated with SRKOA using either the 2P or 1P KJC3 method.
Varus vs neutral alignment was associated with an almost two-fold increase in RKOA odds for the 2P method, but to a lesser extent than SRKOA. Valgus vs neutral alignment was significantly associated with RKOA for the 2P method, the greatest 2P valgus association across all three outcomes.
For the 1P method, varus vs neutral alignment demonstrated greater association with RKOA than valgus vs neutral alignment but neither were significantly associated.
In comparison, greater associations were present for valgus vs neutral knees than varus vs neutral knees for knee pain, although neither 2P nor 1P associations were statistically significant.
Sensitivity analyses
The association between AA alignment and SRKOA did not change substantially in the unadjusted 1P or 2P KJC3 sensitivity analysis, although full adjustment was not possible due to reduced power. In the adjusted sensitivity analysis for knee pain, the greater, but statistically nonsignificant associations for valgus knees were maintained (Supplementary Table 3).
The increase in the odds of RKOA for varus and valgus knees compared to neutral was explored further in Supplementary Table 4, which shows the significant associations with RKOA using the 2P method may partly be explained by the associations between medial JSN for varus knees and lateral JSN for valgus knees.
Discussion
This study shows AA alignment is associated with SRKOA and RKOA but not knee pain alone, with the tibial plateau knee centre having the strongest association. Differences in AA alignment when 1P vs 2P methods were compared indicated the requirement for bespoke alignment categories for each method. This is one of the first studies to extensively compare 1P and 2P AA alignment methods and has identified the tibial plateau centre as the optimal location based on reproducibility and association with clinically important variables. This is consistent with McDaniel19 who compared AA alignment metrics using different KJCs against the gold standard MA alignment method. Although posterior–anterior view SLRs in fixed flexion with a positioning frame were used he recommended standardising AA measurements using either tibial spine base mid-point (KJC1) or tibial plateau centre (KJC3) and suggested comparing 1P and 2P methods in larger studies.
Our results show an approximate 2° difference in AA alignment angles measured using a 1P compared to a 2P method (Fig. 3). There are often difficulties identifying the tibial spine base (KJC1) and tips mid-point (KJC2) due to indistinct tibial spines and/or tibial spine osteophytes. Although KJC3 requires exclusion of marginal tibial osteophytes on the tibial plateau, if present these are easy to exclude compared to osteophytes located on or around the tibial spines. Although this study does not explain the mechanism of these differences, to our knowledge there are no other studies examining this, which highlights the importance of using bespoke cut-points according to the methodology chosen.
Previous comparative AA vs MA alignment studies have used AA alignment as a continuous measurement in their analyses, with angles less than 180° considered varus and angles greater than 180° valgus14, 17, 18, 19. However, when using association with clinical outcomes, our preferred method of choice, to define category cut-points, a U-shaped relationship between AA alignment and SRKOA was observed therefore bespoke AA alignment categories were required. Some AA alignment studies using alignment categories in their analyses8, 20, 21, 41 have applied a valgus offset angle to the varus <178.5°, neutral 178.5–180° and valgus >180° categories described in Moreland's42 seminal paper examining MA alignment in 25 healthy males aged 30. This was not deemed applicable to this AA alignment all female elderly cohort. We therefore used a technique developed by Heim43, to determine new appropriate alignment categories for varus/neutral/valgus knees for both 1P and 2P methods based on the association with SRKOA (Fig. 4). For the 1P method the alignment categories remained the same, as those used in Colebatch's study16: varus <178°, neutral 178–182° and valgus >182°. For the 2P method the new suggested alignment categories were varus <180°, neutral 180–185° and valgus >185° as lower QIC values in Table IV indicated these were a better fit for SRKOA and RKOA outcomes.
Varus knees compared to neutral knees were associated with a significant increase in the odds of SRKOA for the 2P method, with a similar but nonsignificant association for the 1P method. Valgus knees vs neutral knees were not significantly associated with an increase in the odds of SRKOA using either the 2P or 1P method. For RKOA, the 2P method showed significantly higher odds for varus and valgus knees compared to neutral knees. A similar but nonsignificant association was seen for the 1P method.
These associations with RKOA may partly be explained by the relationship between medial JSN for varus knees and lateral JSN for valgus knees as shown in the sensitivity analysis (Supplementary Table 4). These results agree with Teichtahl25 who reported cross-sectional varus and valgus AA alignment (measured as continuous variables) being associated with higher likelihood of respective medial and lateral compartment specific JSN in a KOA cohort. The load transmitted through a neutrally aligned knee is distributed unequally between medial and lateral compartments12, 44, 45, with up to 70% going through the medial compartment46. This disproportionate transmission to the medial compartment in a normally aligned knee was first reported by Morrison in 197047. Knee alignment therefore influences the medial to lateral compartment load distribution, with any shift from neutral alignment of the hip, knee and ankle affecting load distribution at the knee joint11. With just 4–6° of varus alignment, the load through the medial compartment can be increased by up to 90%12. Valgus alignment is associated with an increase in lateral compartment loading48 however, greater load is taken through the medial compartment until a more severe valgus deformity is present44, 45, which may explain the nonsignificant association between valgus vs neutral knees and SRKOA. These increases in compartment loading are thought to increase stress on articular cartilage and surrounding knee joint structures, leading to subsequent degenerative KOA changes.
There were greater associations for knee pain outcome for valgus vs neutral knees compared to varus vs neutral knees. These associations were maintained in the adjusted sensitivity analysis, although neither the 2P or 1P associations were statistically significant. The reasons why knee pain should behave differently to RKOA and SRKOA outcomes are not clear and further studies in this area are required. It could be related to the multidimensional aspects of pain and that more than just OA knee pain was being measured here although women with inflammatory, neurological and fibromyalgia type conditions were excluded. Or it may be due to knee pain originating from knee soft tissue structures such as ligaments, menisci and/or possibly due to patella–femoral joint involvement which was not assessed in this study as skyline radiographs were not available.
Strengths and limitations
This study has a number of strengths. It uniquely compared six alternative AA alignment measures using three different KJCs. It is one of the first studies to compare 1P vs 2P method alignment. This has been carried out using a large sample of over 1000 knees from 584 women representative of a normal, predominantly Caucasian, female population27, 49. Cross-sectional associations have been assessed with SRKOA, RKOA and knee pain outcomes which is not only novel, but also clinically relevant as the discordant relationship between RKOA and reported knee pain is well known26. A further strength of this study is the use of KneeMorf computer software allowing AA alignment measurements to be collected digitally rather than manually.
There are some potential limitations to this study. Due to the original cohort study design, the results are restricted to middle-aged predominantly Caucasian women and therefore cannot be extrapolated to men. Importantly this cross-sectional data is taken from a longitudinal cohort study with losses to follow-up from deaths, withdrawal due to illness and/or disability leading to a possibly healthier cohort attending follow-up visits. However there were no clinically significant differences between included and excluded subjects in this study. We adjusted for the most important potential confounding factors of age, BMI and knee injury which are consistent with the alignment literature. However, residual confounding may exist due to the remaining effects of measured confounders, in addition to those possibly unmeasured or unknown.
When the Chingford study started in 1989, the standard view for knee SLR was antero-posterior, weight-bearing in full knee extension. Due to underestimation of JSN in fully extended views, current practice now prefers semiflexed views50. To accurately evaluate change over time, long-term cohort studies often continue using the same radiographic protocol established at baseline, and therefore these results cannot be generalised to semiflexed knee radiographs.
The lack of FLRs for MA alignment measurement is a limitation. Recent studies have demonstrated strong correlation (r = 0.75–0.88) in KOA populations between MA alignment on FLRs and AA alignment on SLRs14, 15, 18. Alignment measurements on SLRs do not capture the distal tibial or proximal femoral anatomy. The femoral shaft part used to determine AA alignment does not include the femoral neck that protrudes medially from the upper femoral shaft which is used in determining MA alignment, therefore use of a valgus offset correction angle (approximately 4.0°) is suggested to account for the AA and MA alignment difference14, 15, 18. A recent study by Colebatch16, comparing fully extended AP SLRs with FLRs (r = 0.81) in a female healthy population, found no need to apply an offset correction angle in terms of mean alignment or those classified as valgus. This difference could result from studying a healthy all female population in comparison to studies by Kraus18, Hinman14 and Issa15 who used mixed gender RKOA populations, and/or from using a fully extended knee position compared to fixed-flexion18 or semiflexed15 radiographic views. As the Chingford study is a female only cohort containing a mix of healthy and KOA participants with fully extended SLR images an offset correction has not been used and rather than trying to reproduce MA alignment we have specifically defined alignment categories according to clinically relevant variables.
Conclusion
This study has uniquely compared AA alignment using 1P and 2P measurements at three different KJC landmarks and against clinical outcomes and reproducibility has identified KJC3, the tibial plateau centre, as the optimal KJC for future alignment analyses in this cohort. Based on cross-sectional associations with SRKOA, this study has identified appropriate varus/neutral/valgus alignment categories for use with 1P and 2P methods. The overall results suggest differences in AA alignment when 1P vs 2P methods are compared. This requires replicating in other cohorts and further validation with comparison to MA alignment could then determine whether a 1P or 2P AA method is preferable.
Acknowledgements
We would like to thank all of the participants in the Chingford Women's Study and Maxine Daniels for their time and dedication, and Arthritis Research UK for their funding contributions.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.joca.2015.11.009.
Author contributions
-
1)
Conception and design of the study, or acquisition of data, or analysis and interpretation of data: LG, MS, SD, KL, DH, TS, DH, NA.
-
2)
Drafting the article or revising it critically for important intellectual content: LG, MS, SD, KL, DH, TS, CC, ED, DH, NA.
-
3)
Final approval of the version to be submitted: LG, MS, SD, KL, DH, TS, CC, ED, DH, NA.
Competing interest statement
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf and declare that (1) LG, MS-S, SD, KL, DH, TS, ED, and DJH have no conflicts of interest to declare; (2) CC reports personal fees from Servier, personal fees from Amgen, personal fees from Eli Lilly, personal fees from Merck, personal fees from Medtronic, personal fees from Novartis, outside the submitted work; (3) NKA reports personal fees from Flexion (PharmaNet), personal fees from Lily, personal fees from Merck, personal fees from Q-Med, personal fees from Roche, personal fees from Smith & Nephew, grants from Novartis, grants from Pfizer, grants from Schering Plough, grants from Servier, personal fees from Amgen, personal fees from GSK, personal fees from NICOX, personal fees from Smith and Nephew, outside the submitted work.
Role of the funding source
Funding provided by Arthritis Research UK.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Murphy L., Schwartz T.A., Helmick C.G., Renner J.B., Tudor G., Koch G. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59(9):1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Culliford D.J., Maskell J., Beard D.J., Murray D.W., Price A.J., Arden N.K. Temporal trends in hip and knee replacement in the United Kingdom: 1991 to 2006. J Bone Joint Surg. 2010;92(1):130–135. doi: 10.1302/0301-620X.92B1.22654. [DOI] [PubMed] [Google Scholar]
- 3.Sharma L., Song J., Dunlop D., Felson D., Lewis C.E., Segal N. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69(11):1940–1945. doi: 10.1136/ard.2010.129742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma L., Song J., Felson D.T., Cahue S., Shamiyeh E., Dunlop D.D. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 5.Felson D.T., Cooke T.D., Niu J., Goggins J., Choi J., Yu J. Can anatomic alignment measured from a knee radiograph substitute for mechanical alignment from full limb films? Osteoarthritis Cartilage. 2009;17(11):1448–1452. doi: 10.1016/j.joca.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Felson D.T., Goggins J., Niu J., Zhang Y., Hunter D.J. The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum. 2004;50(12):3904–3909. doi: 10.1002/art.20726. [DOI] [PubMed] [Google Scholar]
- 7.Felson D.T., McLaughlin S., Goggins J., LaValley M.P., Gale M.E., Totterman S. Bone marrow edema and its relation to progression of knee osteoarthritis. Ann Intern Med. 2003;139(5 Pt 1):330–336. doi: 10.7326/0003-4819-139-5_part_1-200309020-00008. [DOI] [PubMed] [Google Scholar]
- 8.Brouwer G.M., van Tol A.W., Bergink A.P., Belo J.N., Bernsen R.M., Reijman M. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56(4):1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- 9.Hunter D.J., Niu J., Felson D.T., Harvey W.F., Gross K.D., McCree P. Knee alignment does not predict incident osteoarthritis: the Framingham osteoarthritis study. Arthritis Rheum. 2007;56(4):1212–1218. doi: 10.1002/art.22508. [DOI] [PubMed] [Google Scholar]
- 10.Felson D.T., Niu J., Gross K.D., Englund M., Sharma L., Cooke T.D. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the multicenter osteoarthritis study and the osteoarthritis initiative. Arthritis Rheum. 2013;65(2):355–362. doi: 10.1002/art.37726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tetsworth K., Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25(3):367–377. [PubMed] [Google Scholar]
- 12.Hsu R.W., Himeno S., Coventry M.B., Chao E.Y. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 13.Cooke T.D., Sled E.A. Optimizing limb position for measuring knee anatomical axis alignment from standing knee radiographs. J Rheumatol. 2009;36(3):472–477. doi: 10.3899/jrheum.080732. [DOI] [PubMed] [Google Scholar]
- 14.Hinman R.S., May R.L., Crossley K.M. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum. 2006;55(2):306–313. doi: 10.1002/art.21836. [DOI] [PubMed] [Google Scholar]
- 15.Issa S.N., Dunlop D., Chang A., Song J., Prasad P.V., Guermazi A. Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis Rheum. 2007;57(3):398–406. doi: 10.1002/art.22618. [DOI] [PubMed] [Google Scholar]
- 16.Colebatch A.N., Hart D.J., Zhai G., Williams F.M., Spector T.D., Arden N.K. Effective measurement of knee alignment using AP knee radiographs. Knee. 2009;16(1):42–45. doi: 10.1016/j.knee.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Chang C.B., Choi J.Y., Koh I.J., Seo E.S., Seong S.C., Kim T.K. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis Cartilage. 2010;18(4):530–538. doi: 10.1016/j.joca.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Kraus V.B., Vail T.P., Worrell T., McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum. 2005;52(6):1730–1735. doi: 10.1002/art.21100. [DOI] [PubMed] [Google Scholar]
- 19.McDaniel G., Mitchell K.L., Charles C., Kraus V.B. A comparison of five approaches to measurement of anatomic knee alignment from radiographs. Osteoarthritis Cartilage. 2010;18(2):273–277. doi: 10.1016/j.joca.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong A.K., Inglis D., Beattie K.A., Doan A., Ioannidis G., Obeid J. Reproducibility of computer-assisted joint alignment measurement in OA knee radiographs. Osteoarthritis Cartilage. 2009;17(5):579–585. doi: 10.1016/j.joca.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhai G., Ding C., Cicuttini F., Jones G. A longitudinal study of the association between knee alignment and change in cartilage volume and chondral defects in a largely non-osteoarthritic population. J Rheumatol. 2007;34(1):181–186. [PubMed] [Google Scholar]
- 22.Felson D.T., Nevitt M.C., Zhang Y., Aliabadi P., Baumer B., Gale D. High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis Rheum. 2002;46(5):1217–1222. doi: 10.1002/art.10293. [DOI] [PubMed] [Google Scholar]
- 23.Teichtahl A.J., vies-Tuck M.L., Wluka A.E., Jones G., Cicuttini F.M. Change in knee angle influences the rate of medial tibial cartilage volume loss in knee osteoarthritis. Osteoarthritis Cartilage. 2009;17(1):8–11. doi: 10.1016/j.joca.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 24.Sheehy L., Felson D., Zhang Y., Niu J., Lam Y.M., Segal N. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthritis Cartilage. 2011;19(1):58–64. doi: 10.1016/j.joca.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teichtahl A.J., Cicuttini F.M., Janakiramanan N., Davis S.R., Wluka A.E. Static knee alignment and its association with radiographic knee osteoarthritis. Osteoarthritis Cartilage. 2006;14(9):958–962. doi: 10.1016/j.joca.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 26.Bedson J., Croft P.R. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. doi: 10.1186/1471-2474-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hart D.J., Spector T.D. The relationship of obesity, fat distribution and osteoarthritis in women in the general population: the Chingford Study. J Rheumatol. 1993;20(2):331–335. [PubMed] [Google Scholar]
- 28.Hart D.J., Doyle D.V., Spector T.D. Incidence and risk factors for radiographic knee osteoarthritis in middle-aged women: the Chingford Study. Arthritis Rheum. 1999;42(1):17–24. doi: 10.1002/1529-0131(199901)42:1<17::AID-ANR2>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 29.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kellgren J.H., Lawrence J.S., Bier F. Genetic factors in generalized osteo-arthrosis. Ann Rheum Dis. 1963;22:237–255. doi: 10.1136/ard.22.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burnett S., Hart D.J., Cooper C., Spector T.D. Springer-Verlag; London: 1994. A Radiographic Atlas of Osteoarthritis; pp. 1–45. [Google Scholar]
- 32.Spector T.D., Hart D.J., Byrne J., Harris P.A., Dacre J.E., Doyle D.V. Definition of osteoarthritis of the knee for epidemiological studies. Ann Rheum Dis. 1993;52(11):790–794. doi: 10.1136/ard.52.11.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leyland K.M., Hunter D., Judge A., Bottomley N., Hart D., Gill R. Bezier curver for measuring joint space on knee radiographs—reproducibility and validity (conference abstract) Osteoarthritis Cartilage. 2011;19(S1):S180–S181. [Google Scholar]
- 34.Leyland K.M., Kiran A., Judge A., Hunter D., Hart D., Javaid K. Joint space narrowing over 5 years predicts future knee replacements up to 15 years later (conference abstract) Rheumatol Oxf. 2013;52(Suppl 1):i152. [Google Scholar]
- 35.Davis M.A., Ettinger W.H., Neuhaus J.M., Mallon K.P. Knee osteoarthritis and physical functioning: evidence from the NHANES I Epidemiologic Followup Study. J Rheumatol. 1991;18(4):591–598. [PubMed] [Google Scholar]
- 36.Goulston L.M., Kiran A., Javaid M.K., Soni A., White K.M., Hart D.J. Does obesity predict knee pain over fourteen years in women, independently of radiographic changes? Arthritis Care Res Hob. 2011;63(10):1398–1406. doi: 10.1002/acr.20546. [DOI] [PubMed] [Google Scholar]
- 37.Donner A., Klar N. Arnold; London: 2000. Design and Analysis of Cluster Randomization Trials in Health Research. [Google Scholar]
- 38.Cicuttini F., Wluka A., Hankin J., Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatol Oxf. 2004;43(3):321–324. doi: 10.1093/rheumatology/keh017. [DOI] [PubMed] [Google Scholar]
- 39.Heim N., Snijder M.B., Heymans M.W., Deeg D.J., Seidell J.C., Visser M. Optimal cutoff values for high-risk waist circumference in older adults based on related health outcomes. Am J Epidemiol. 2011;174(4):479–489. doi: 10.1093/aje/kwr093. [DOI] [PubMed] [Google Scholar]
- 40.Pan W. Akaike's information criterion in generalized estimating equations. Biometrics. 2001;57(1):120–125. doi: 10.1111/j.0006-341x.2001.00120.x. [DOI] [PubMed] [Google Scholar]
- 41.Mazzuca S.A., Brandt K.D., Chakr R., Lane K.A. Varus malalignment negates the structure-modifying benefits of doxycycline in obese women with knee osteoarthritis. Osteoarthritis Cartilage. 2010;18(8):1008–1011. doi: 10.1016/j.joca.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moreland J.R., Bassett L.W., Hanker G.J. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745–749. [PubMed] [Google Scholar]
- 43.Edwards M.H., van der Pas S., Denkinger M.D., Parsons C., Jameson K.A., Schaap L. Relationships between physical performance and knee and hip osteoarthritis: findings from the European Project on Osteoarthritis (EPOSA) Age Ageing. 2014;43(6):806–813. doi: 10.1093/ageing/afu068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harrington I.J. Static and dynamic loading patterns in knee joints with deformities. J Bone Joint Surg Am. 1983;65(2):247–259. doi: 10.2106/00004623-198365020-00016. [DOI] [PubMed] [Google Scholar]
- 45.Johnson F., Leitl S., Waugh W. The distribution of load across the knee. A comparison of static and dynamic measurements. J Bone Joint Surg Br. 1980;62(3):346–349. doi: 10.1302/0301-620X.62B3.7410467. [DOI] [PubMed] [Google Scholar]
- 46.Schipplein O.D., Andriacchi T.P. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 47.Morrison J.B. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970;3(1):51–61. doi: 10.1016/0021-9290(70)90050-3. [DOI] [PubMed] [Google Scholar]
- 48.Bruns J., Volkmer M., Luessenhop S. Pressure distribution at the knee joint. Influence of varus and valgus deviation without and with ligament dissection. Arch Orthop Trauma Surg. 1993;113(1):12–19. doi: 10.1007/BF00440588. [DOI] [PubMed] [Google Scholar]
- 49.Hart D.J., Mootoosamy I., Doyle D.V., Spector T.D. The relationship between osteoarthritis and osteoporosis in the general population: the Chingford Study. Ann Rheum Dis. 1994;53(3):158–162. doi: 10.1136/ard.53.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Buckland W. Radiographic assessment of osteoarthritis: comparison between existing methodologies. Osteoarthritis Cartilage. 1999;7(4):430–433. doi: 10.1053/joca.1998.0234. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.