A pilot program introducing HPV testing as part of a public sector screening program was successfully and effectively implemented in a low-resource setting.
Key Words: careHPV, human papillomavirus, cervical cancer, screening program, Latin America
Abstract
Objective
In a primary human papillomavirus (HPV) screening program, we compared the 6-month follow-up among colposcopy and noncolposcopy-based management strategies for screen-positive women.
Materials and Methods
Women aged 30 to 49 years were screened with HPV DNA tests using both self-collection and provider collection of samples. Women testing positive received either (1) colposcopy management (CM) consisting of colposcopy and management per local guidelines or (2) screen-and-treat (ST) management using visual inspection with acetic acid to determine cryotherapy eligibility, with eligible women undergoing immediate cryotherapy. One thousand women were recruited in each cohort. Of these, 368 (18.4%) of 2000 women were recruited using a more intensive outreach strategy. Demographics, HPV positivity, and treatment compliance were compared across recruitment and management strategies.
Results
More women in the ST cohort received treatment within 6 months compared with those in the CM cohort (117/119 [98.3%] vs 64/93 [68.8%]; p < .001). Women recruited through more intensive outreach were more likely to be HPV positive, lived in urban areas, were more educated, and had higher numbers of lifetime sexual partners and fewer children.
Conclusions
Women in the CM arm were less likely to complete care than women in the ST arm. Targeted outreach to underscreened women successfully identified women with higher prevalence of HPV and possibly higher disease burden.
Human papillomavirus (HPV) tests used for cervical cancer screening in higher-resource settings are not accessible to low-resource settings because of cost and lack of infrastructure. An HPV screening test has been developed specifically for lower-resource settings (careHPV Test; QIAGEN, Gaithersburg, MD). Clinical studies have shown that its sensitivity for cervical precancer and cancer approaches that the US Food and Drug Administration–approved Hybrid Capture 2 Test (QIAGEN) on which careHPV was based.1,2
This test has made it feasible to implement HPV screening programs in some lower-resource countries nationwide. However, the most effective strategy for implementation of HPV testing in a public sector program is unknown. High-resource settings generally used colposcopy management (CM) strategies for screen-positive women. However, CM strategies require significant infrastructure and trained personnel, both of which are lacking in the lower-cost settings. Therefore, the World Health Organization (WHO) has endorsed colposcopy referral or immediate treatment after a positive HPV test. A study of an HPV testing program in South Africa showed that providing immediate treatment and eliminating the colposcopy step were more clinically effective and less costly than a CM strategy.3
The Cervical Cancer Prevention in El Salvador (CAPE) program was launched in 2011 to identify best practices for incorporating HPV-based screening and management into its national cervical cancer prevention program. The CAPE program is a 3-phase, 30,000-woman demonstration program that assesses the feasibility and cost-effectiveness of a screening and treatment intervention using this HPV test. The CAPE program is administered by the Salvadoran Ministry of Health (MOH) with technical support provided by the nonprofit organization, Basic Health International.
Phase 1 objectives were to the following: (1) screen 2,000 women aged 30 to 49 years living in the Paracentral region of El Salvador; (2) compare HPV-positive women's compliance with 2 management strategies; (3) demonstrate increased participation of underscreened and unscreened women; and (4) determine patient preference for self-sampling or provider sampling.4 The results of objectives 1 and 2 are discussed in detail in this article. The results of 3 and 4 are discussed briefly here and in more detail in other publications.4,5 The primary objective of this descriptive manuscript is to compare colposcopy and non-CM strategies for HPV-positive women. The secondary objectives included program evaluation, including examination of self-sampling feasibility, reliability of pathology, and assessment of a more intensive recruitment strategy.
MATERIALS AND METHODS
The MOH initiated phase 1 of CAPE at 4 health units (San Pedro Perúlapan, San Rafael Cedros, Apastepeque, and San Sebastián) that provide primary preventive care in the Paracentral region of El Salvador. These health units were selected with the goal of contacting 2,500 women to meet the target of screening 2,000 women, assuming 80% follow-up. According to 2007 national census data, 11,046 women aged 30 to 49 were living in these health units' catchment areas. Women were excluded if they lived outside the catchment area, were known to be pregnant, had a hysterectomy, loop electrosurgical excision procedure (LEEP), or cryotherapy, or previously had cervical precancer or cancer. According to government census, the 4 health units served populations similar in age, poverty level, and education.
Community census records were used to identify women aged 30 to 49 years without recent cervical cancer screening. Health promoters contacted women with no record of recent screening and invited them to attend an educational session about HPV testing at their local clinic. The program was internally evaluated by the MOH at periodic intervals. Concerns were raised about the low number of underscreened women who were being recruited. Only 10.7% (167/1565) of women enrolled and screened with HPV testing had either never been screened or not been screened in the past 5 years.
Recruitment was then changed to prioritizing identification of underscreened or unscreened women. Instead of using only community health records, these records were cross-referenced with local health unit Pap records to obtain the women's most current screening histories. This more intensive outreach strategy identified an additional 368 women eligible for screening with HPV testing. Among the 306 women for whom screening records were available, 147 (48%) were unscreened or underscreened. To increase participation, the clinic-based educational session was replaced with individual instruction at home for most women (96%) recruited with intensive outreach. Women were then offered an appointment for screening at a nearby clinic.
All participants provided self-collected and provider-collected specimens. The decision to include self-sampling was made by the MOH to assess the feasibility of using this modality in a larger screening program. However, the MOH decided only to use HPV results from provider-collected samples for clinical management decisions until self-collected sampling was approved.
Women who tested HPV positive on the provider-collected sample were managed with 1 of the following 2 strategies: (1) referral to colposcopy followed by treatment as needed (CM) or (2) screen-and-treat (ST) management using visual inspection with acetic acid to determine cryotherapy eligibility, with eligible women undergoing immediate treatment and ineligible women referred for colposcopy (ST). Human papillomavirus–negative women were instructed to rescreen in 5 years.
Follow-up strategies for HPV-positive women varied by health unit. Two health units followed a CM strategy and 2 health units followed an ST strategy. Treatment approaches were not randomized because CAPE was not designed as a research study but rather as a demonstration program. The research study design adhered to principles of implementation science and similar communities were chosen to have different interventions for treatment.
In the ST cohort, HPV-positive women were given a visual inspection with acetic acid examination by a physician-gynecologist at their follow-up visit. In accordance with recent WHO guidelines for treatment in regions where there is insufficient infrastructure for management, all eligible HPV-positive women received immediate cryotherapy even if no lesion was visualized.6 Contraindications to treatment included pregnancy, large cervical lesion, suspected cancer, and/or lesion extended into the endocervical canal.6 Referrals for colposcopy and further management were provided for women with any contraindications.
For HPV-positive women in the ST cohort eligible for cryotherapy, completion of follow-up was achieved if cryotherapy occurred within 6 months of screening. For women referred for colposcopy (i.e., in the CM cohort or in the ST cohort and not eligible for cryotherapy), follow-up was completed if 1 of 3 following outcomes occurred within 6 months of diagnosis: (1) normal colposcopic impression (no biopsy or endocervical curettage [ECC]); (2) normal biopsy and/or ECC; or (3) treatment based on biopsy or ECC results was completed. Following MOH guidelines, women with cervical intraepithelial neoplasia grade 1 (CIN 1) were treated with cryotherapy. Women with CIN grade 2 or 3 (CIN 2/3) received cryotherapy, LEEP, or a hysterectomy, as determined by the managing physician.
χ2 tests, Fisher exact tests, and 2 sample t tests were used to assess associations across recruitment periods and management strategies between demographic variables (age, education attainment, residential area, and number of children), sexual history (age at sexual initiation and number of lifetime sexual partners), time since last screening, HPV positivity, and follow-up compliance. Logistic regression was used to explore relationships between HPV positivity and demographic and screening characteristics, recruitment period, and management strategy. Variables with p values of less than .10 in unadjusted models were entered into the multivariate model using backwards elimination. The κ statistic and McNemar tests were used to compare agreement between provider- and self-collected sampling methods. The significance level was set at .05 and all statistical analyses were conducted using STATA Version 12 software (StataCorp LP, 2011, College Station, TX).
The University of Pittsburgh and the national ethical review board of El Salvador granted institutional review board approval to analyze the data.
RESULTS
Of the women invited to attend an educational session, 1,049 (74.3%) of 1,239 women in the CM cohort and 981 (79.2%) of 1,410 women in the ST cohort attended. Health promoters scheduled a screening appointment within 15 days of the session for the 958 (91.3%) of 1,049 women in the CM cohort and 938 (95.6%) of 981 women in the ST cohort eligible for screening. Fewer women in the CM cohort attended their screening appointment compared with women in the ST cohort (751/958 [78.4%] vs 881/938 [93.9%]; p < .001). Although the subjects were not randomized, the communities where the interventions were done were similar in size and women were similar in terms of important risk factors such as age at first intercourse and number of lifetime partners.
Table 1 presents demographic and screening characteristics of women screened, stratified by management cohort. Women in the CM cohort had less education (p = .003) and were more likely to have been screened within the past 3 years (74.0% vs 54.5%; p < .001) compared with women in the ST cohort. Among women contacted during more intensive outreach, those in the ST cohort had fewer children (p = .04), were less likely to have been screened within the past 3 years (57.2% vs 38.1%; p = .003), and were more likely to have urban residence (87.4% vs 16.9%; p < .001) compared with women in the CM cohort (data not in table).
TABLE 1.
Demographic and Screening Characteristics of Participants by Management Strategy Cohort
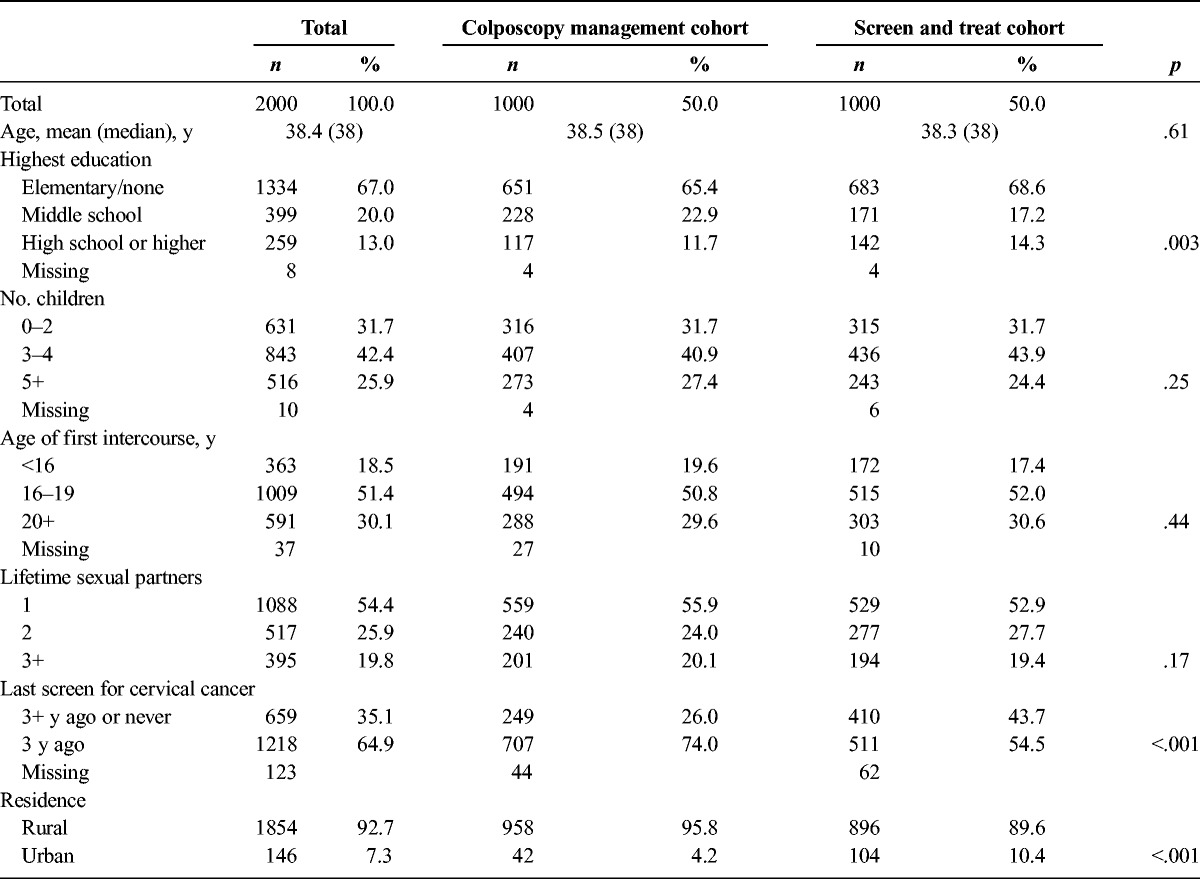
Table 2 presents results regarding screening outcomes, treatment, and compliance, stratified by management strategy. Human papillomavirus positivity did not differ significantly between CM and ST strategies (9.3% vs 11.9%, respectively; p = .06). In the CM cohort only, 6 (6.5%) of 93 women had a normal colposcopy examination or biopsy; in the ST cohort, colposcopy was only performed if women were not eligible for cryotherapy and all (8/8) had CIN 1 or worse biopsy.
TABLE 2.
Screening and Management Outcomes by Management Strategy Cohort and Recruitment Period
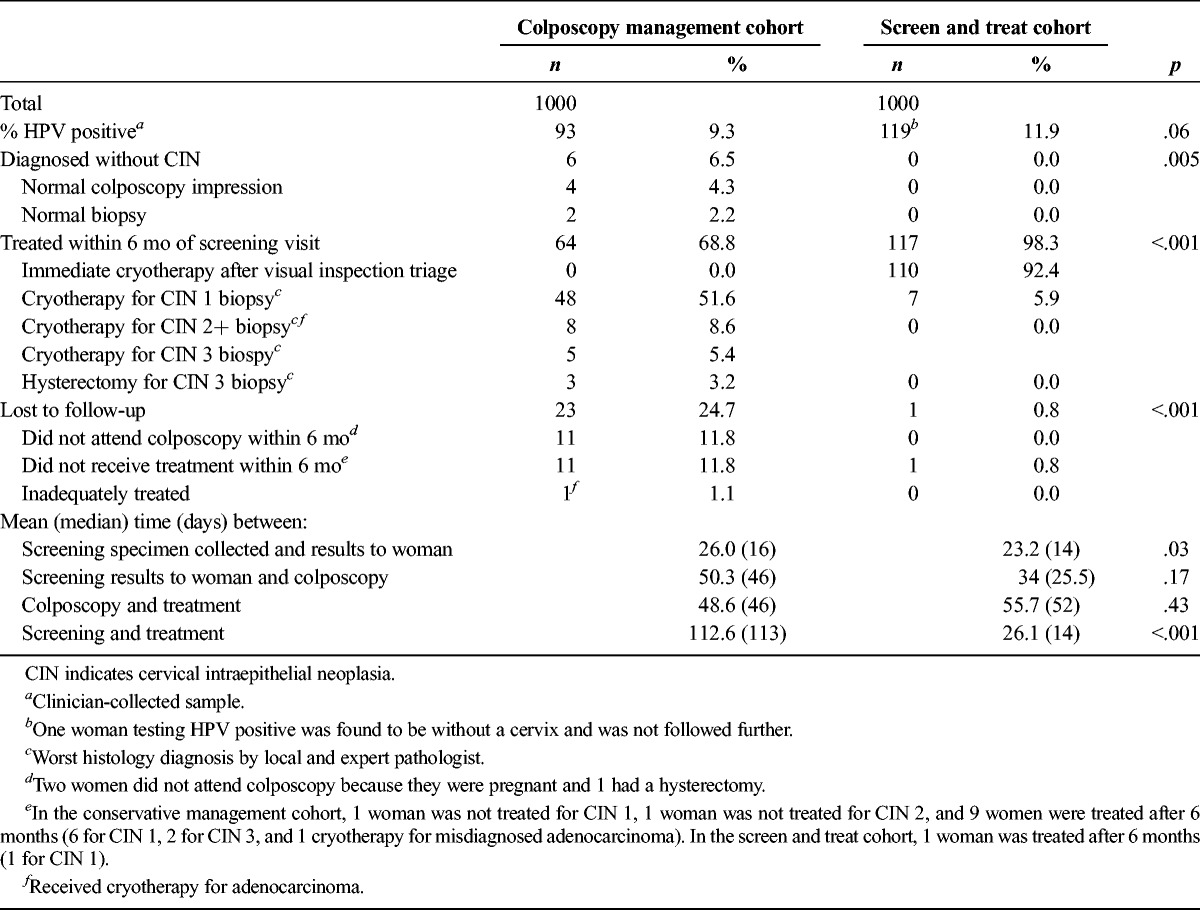
More women in the CM cohort did not attend colposcopy or receive adequate treatment within 6 months of screening compared with women in the ST cohort (23/93 [24.7%] vs 1/119 [1.0%], respectively; p < .001). Therefore, more women in the ST cohort received treatment within 6 months compared with those in the CM cohort (117/119 [98.3%] vs 64/93 [68.8%], respectively; p < .001).
The time in days between screening and treatment was shorter for the ST group than for the CM group during standard recruitment. The mean and median wait time between screening and treatment for CM was 112 and 114 days for CM compared with 26 and 14 days for ST (p < .001).
There was high percentage of women in the CM group given cryotherapy because of the high prevalence of CIN 1 diagnosed by the local pathologist, cryotherapy being the standard treatment in El Salvador for a CIN 1 biopsy result. Women with CIN 1 in the CM cohort, as diagnosed by the local pathologist, received the same treatment as those in the ST cohort after the intervening colposcopy.
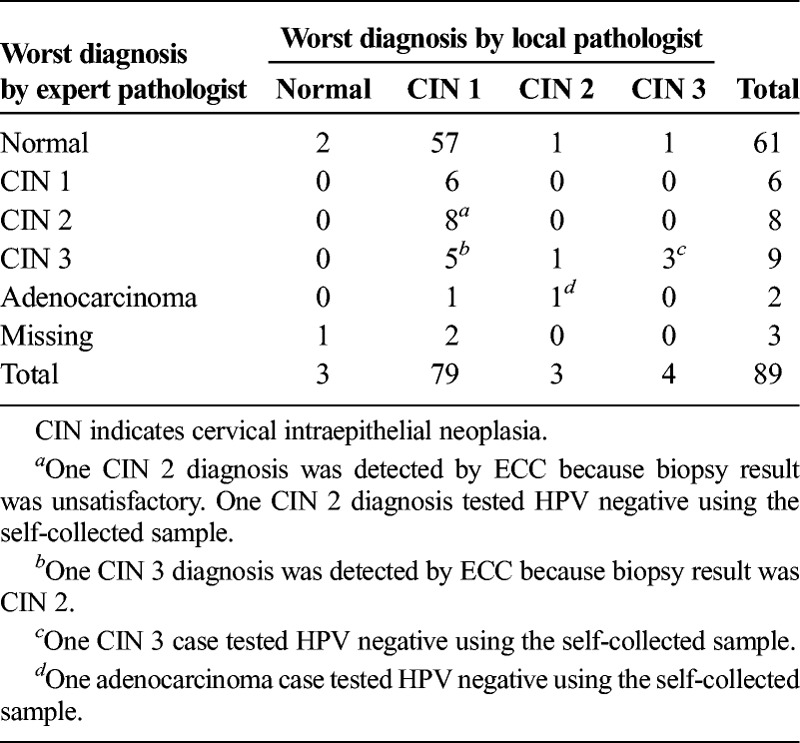
During phase 1, 89 women had colposcopy with biopsy. Local pathologists made the initial diagnosis of all specimens, and the treatment course was based on the primary pathologist's diagnosis. Preliminary data indicated an unusually high rate of CIN 1 and an unusually low rate of CIN 2 or worse. An expert gynecologic pathologist conducted quality assurance on 86 biopsy specimens (3 specimens were unavailable for review, see Table 3). The expert pathologist diagnosed fewer cases of CIN 1 than did the local pathologist (6 vs 79; p < .001) and more cases of CIN 2 or more severe (19 vs 7; p < .001).
TABLE 3.
Worst Histopathology Result of Biopsy by Local and Expert Pathologists
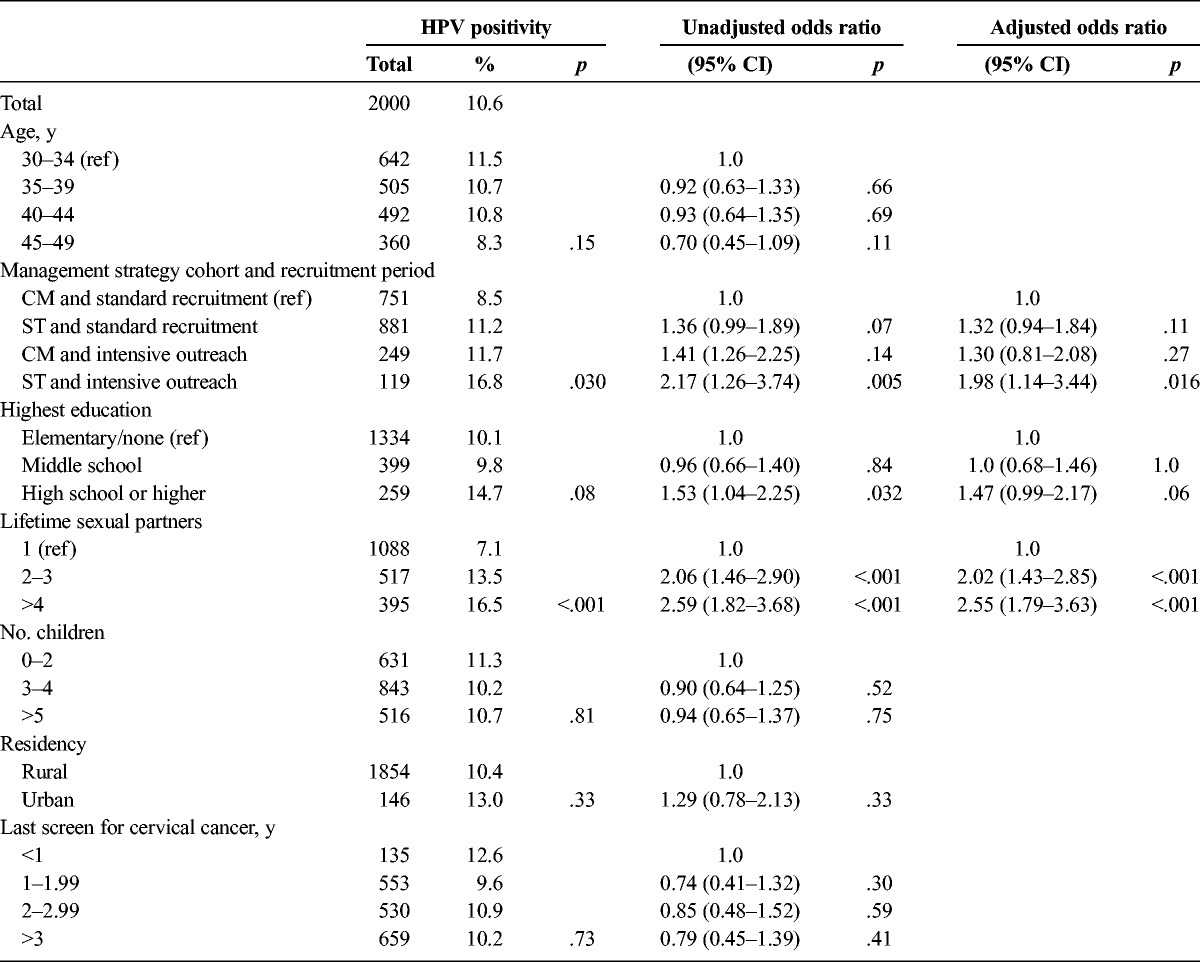
In the univariate analysis (see Table 4), testing HPV positive was associated with education (reference group, women with elementary education/none; odds ratio [OR], 1.5 for women with high school education or higher; p = .03); recruitment strategy and management cohort (reference group, women in the CM cohort and standard recruitment group; OR, 2.2 for women in the ST cohort and more intensive outreach; p = .005); and number of lifetime sexual partners (reference group, women with 1 lifetime partner; OR, 2.1 for women with 2–3 lifetime partners; p < .001; and OR, 2.6 for women with more than 4 lifetime partners; p < .001).
TABLE 4.
HPV Positivity Given Demographic and Personal Risk Factors
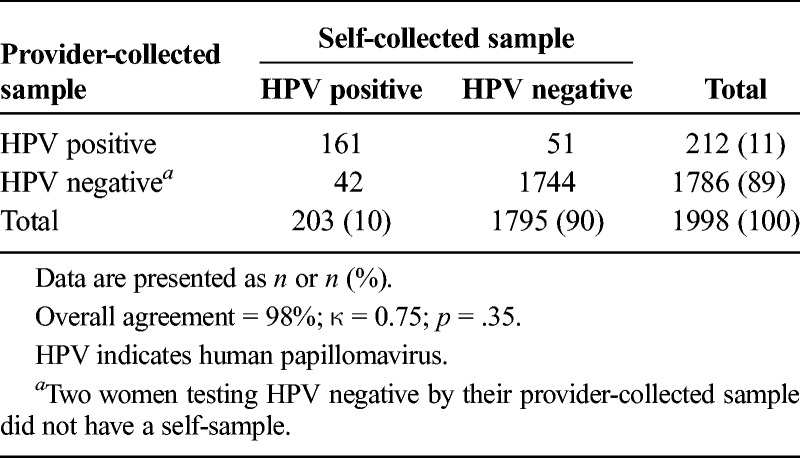
Overall agreement between self-collected and provider-collected HPV samples was 98% with a κ value of 0.75 (p = .4; see Table 5). Among 1,998 samples tested for HPV, 42 (2.1%) tested positive on self-collection and negative on provider collection and 5 (2.6%) tested negative on self-collection and positive on provider collection. Nineteen women with CIN 2 or more severe diagnoses tested positive for HPV on provider collection; of these, 16 (84.2%) tested positive on self-collection.
TABLE 5.
HPV Positivity by Self- Versus Provider-Collected Sampling
DISCUSSION
Although both the CM and ST strategies were successful in managing the care of women who tested HPV positive, the ST cohort led to a significantly higher number of women who completed treatment at 6 months (98.3% vs 68.8%). Although it may seem obvious that an immediate treatment would yield a greater number of managed cases, the extent of this effect was higher than expected particularly because this was a highly controlled, MOH-driven project.
Although the ST strategy does introduce the risk of overtreatment, the CM strategy poses a risk of undertreatment because of increased likelihood of noncompliance with 1 or more of the multiple visits needed to complete the management protocol. We believe that the benefits of the ST approach far outweigh the risk of overtreatment because the adverse effects of cryotherapy are minimal, particularly in the age group targeted for screening in low- and middle-income countries where cervical cancer rates are extremely high. There is even some evidence that a cryotherapy procedure is protective against future HPV infection and precancer.7–10 For this reason, the WHO recommendations for cervical cancer screening in low-resource settings include HPV screening, followed by immediate triage and treatment.11 Furthermore, the CM strategy would likely result in an equal number of cryotherapy treatments as the ST strategy because MOH guidelines dictate cryotherapy for women diagnosed with CIN 1 on biopsy a common finding for women screening HPV positive. In this pilot, 80% of women who completed follow-up in the CM arm had cryotherapy, compared with 100% in the ST cohort.
Outreach and educational sessions were critical factors associated with participation. Although 3 quarters of women contacted during standard recruitment, 2,030 (76.1%) of 2,515 women attended a group educational session and more than 1,632 (86%) of 1,896 women eligible for screening subsequently completed screening.
The outreach strategies of the MOH health promoters were essential to increasing participation at every step of phase 1. Health promoters may have more invested in outcomes, because they are employees of the agency administering CAPE; this motivation likely contributed to almost 90% compliance with colposcopy appointments among women in the CM cohort, higher than the 70% to 80% compliance observed in previous literature. Without the frequent communication and encouragement provided to participants by the health promoters, the number of women who were screened and completed treatment would likely be considerably lower.12–16
We were pleased to find that this project improved the colposcopy referral system in the Paracentral region. Before this program, women had to return to the clinic after receiving an abnormal Pap or HPV positive result to schedule the colposcopy appointment. After phase 1 of CAPE was implemented, the colposcopy appointment was scheduled as soon as women received the abnormal result. Eliminating the additional visit has considerably improved follow-up.
Additional unscreened and underscreened women were successfully identified and treated once health promoters initiated more intensive outreach by using local health unit Pap records to update screening histories in community census records. Women identified through more intensive outreach had profiles associated with greater risk of HPV and cervical cancer; they were more likely to have 4 or more lifetime sexual partners, and almost half had not been screened in the previous 3 years. It is difficult to draw conclusions about the implications of higher HPV prevalence in this population because they differ from those identified through standard recruitment. The more intensive outreach strategy of providing individual instruction in women's homes increased participation and encouraged follow-up. The results of more intensive outreach during phase 1 indicate that it will be necessary to employ this recruitment strategy as CAPE expands.
Our study showed that self-sampling was almost as effective as provider sampling at detecting HPV. A separate study conducted in a subset of 518 women found that almost 40% of women preferred self-sampling to provider sampling, and more than 60% of women accepted self-sampling.4 Most women with high-grade lesions identified by provider-collected samples were also identified as HPV positive by self-collected samples. Ideally, to ensure optimal sensitivity, all samples would be collected by providers when using careHPV. However, this is not feasible in many low-resource settings. Providing a self-sampling option can greatly increase the number of women screened and treated and may help decrease overall cervical cancer mortality.5
One of this program's most important findings is that pathology diagnosis is challenging even in a highly regulated national program. The local pathologist diagnosed only 7 (36.8%) of 19 high-grade lesions identified by the expert pathologist upon secondary review. Even if all women underwent colposcopy, inaccurate pathology diagnosis may limit the effectiveness of a colposcopy-based strategy to provide appropriate care, because the success of that approach is dependent on pathology diagnosis. Although the MOH encourages LEEP or hysterectomy for patients with CIN 3, only 3 of 9 patients with CIN 3 received a diagnosis of CIN 2/3 by the local pathologist; the other 6 received cryotherapy (rather than LEEP) for the presumed diagnosis of CIN 1. In addition, the total percentage of women treated in the CM cohort was no different than in the ST cohort because of the overdiagnosis of CIN 1 by the local pathologist. These findings underscore the need to direct more resources toward pathology training to improve pathology diagnosis.
Phase 1 of CAPE was the first government-led implementation of an HPV-based cervical cancer screening program using this HPV test. Cervical Cancer Prevention in El Salvador is a real-time demonstration program that will ultimately screen 30,000 women. The main weakness of this project is that women were not randomized to a management strategy (CM or ST), because CAPE was not designed as a research study. The 2 treatment cohorts, however, were similar enough to conclude that the findings provide valuable insights into how these strategies might perform in a larger context. We found that ST strategy consistent with recent WHO recommendations was successfully and effectively implemented by the Salvadoran MOH.
In conclusion, using the ST management strategy led to a greater likelihood of successful management of HPV-positive women than the CM strategy. The self-sampling strategy was feasible, and active recruitment leads to a higher enrollment of HPV-positive women. There are limitations to local pathology programs and efforts should be made to strengthen these systems because some clinical decisions will be made on the basis of pathologic diagnosis.
Footnotes
The authors have declared they have no conflicts of interest.
The study was supported by Einhorn Family Charitable Trust.
The facts and opinions hereby published in this study are solely the personal statements and observations of the respective authors. The data gathered and conclusions manifested are a result of independent work with no conflicts of interest stated. Authors are responsible for all contents including accuracy of the facts, statements, citing resources, etc. The authors of this article certify that the work is original and not published or submitted for publication elsewhere.
The University of Pittsburgh and the national ethical review board of El Salvador granted institutional review board approval for this study.
REFERENCES
- 1. YL Qiao, Sellors JW, Eder PS, et al. A new HPV-DNA test for cervical-cancer screening in developing regions: a cross-sectional study of clinical accuracy in rural China. Lancet Oncol 2008; 9: 929– 36. [DOI] [PubMed] [Google Scholar]
- 2. Zhao FH, Jeronimo J, Qiao YL, et al. An evaluation of novel, lower-cost molecular screening tests for human papillomavirus in rural China. Cancer Prev Res (Phila) 2013; 6: 938– 48. [DOI] [PubMed] [Google Scholar]
- 3. Goldie SJ, Kuhn L, Denny L, et al. Policy analysis of cervical cancer screening strategies in low-resource settings: clinical benefits and cost-effectiveness. JAMA 2001; 285: 3107– 15. [DOI] [PubMed] [Google Scholar]
- 4. Rosenbaum AJ, Gage JC, Alfaro KM, et al. Acceptability of self-collected versus provider-collected sampling for HPV DNA testing among women in rural El Salvador. Int J Gynecol Obstet 2014; 126: 156– 60. [DOI] [PubMed] [Google Scholar]
- 5. Campos NG, Maza M, Alfaro K, et al. The comparative and cost-effectiveness of HPV-based cervical cancer screening algorithms in El Salvador. Int J Cancer 2015; 137: 893– 902. [DOI] [PubMed] [Google Scholar]
- 6. WHO Guidelines: Use of Cryotherapy for Cervical Intraepithelial Neoplasia. Geneva: World Health Organization; 2011. Available at: http://www.ncbi.nlm.nih.gov/books/NBK138476. Accessed December 1, 2015. [PubMed] [Google Scholar]
- 7. Jacob M, Broekhuizen FF, Castro W, et al. Experience using cryotherapy for treatment of cervical precancerous lesions in low-resource settings. Int J Gynecol Obstet 2015; 89: S13– 20. [DOI] [PubMed] [Google Scholar]
- 8. Chirenje ZM, Rusakaniko S, Akino V, et al. A randomised clinical trial of loop electrosurgical excision procedure (LEEP) versus cryotherapy in the treatment of cervical intraepithelial neoplasia. J Obstet Gynecol 2001; 21: 617– 21. [DOI] [PubMed] [Google Scholar]
- 9. McClung EC, Blumenthal PD. Efficacy, safety, acceptability and affordability of cryotherapy: a review of current literature. Minerva Ginecol 2012; 64: 149– 71. [PubMed] [Google Scholar]
- 10. Follen Mitchell M, Tortolero-Luna G, Cook E, et al. A randomized clinical trial of cryotherapy, laser vaporization, and loop electrosurgical excision for treatment of squamous intraepithelial lesions of the cervix. Obstet Gynecol 1998; 92: 737– 44. [PubMed] [Google Scholar]
- 11. WHO WHO Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 12. Everett T, Bryant A, Griffin MF, et al. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database Syst Rev 2011: CD002834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Spadea T, Bellini S, Kunst A, et al. The impact of interventions to improve attendance in female cancer screening among lower socioeconomic groups: a review. Prev Med 2010; 50: 159– 64. [DOI] [PubMed] [Google Scholar]
- 14. White K, Garces IC, Bandura L, et al. Design and evaluation of a theory-based, culturally relevant outreach model for breast and cervical cancer screening for Latina immigrants. Ethn Dis 2012; 22: 274– 80. [PMC free article] [PubMed] [Google Scholar]
- 15. Pirzadeh A, Mazaheri MA. The effect of education on women's practice based on the health belief model about Pap smear test. Int J Prev Med 2012; 3: 585– 90. [PMC free article] [PubMed] [Google Scholar]
- 16. Agurto I, Arrossi S, White S, et al. Involving the community in cervical cancer prevention programs. Int J Gynaecol Obstet 2005; 89(suppl 2): S38– 45. [DOI] [PubMed] [Google Scholar]


