Abstract
Objective
To assess how the effect of World Trade Center (WTC) exposure on physician-diagnosed chronic rhinosinusitis (CRS) in firefighters changed during the decade following the attack on 9/11 (11 September 2001 to 10 September 2011).
Methods
We examined temporal effects on the relation between WTC exposure and the incidence of physician diagnosed CRS in firefighters changed during the decade following the attack on 9/11 (11 September 2001 to 10 September 2011). Exposure was grouped by time of arrival at the WTC site as follows: (high) morning 11 September 2001 (n=1623); (moderate) afternoon 11 September 2001 or 12 September 2001 (n=7025); or (low) 13–24 September 2001 (n=1200). Piecewise exponential survival models were used to estimate incidences by exposure group, with change points in the relative incidences estimated by maximum likelihood.
Results
Incidences dramatically increased after 2007 due to a programmatic change that provided free medical treatment, but increases were similar in all exposure groups. For this reason, we observed no change point during the study period, meaning the relative incidence by exposure group (high vs moderate vs low) of CRS disease did not significantly change over the study period. The relative rate of developing CRS was 1.99 (95% CI=1.64 to 2.41) for high versus low exposure, and 1.52 (95% CI=1.28 to 1.80) for moderate versus low exposure during the 10-year follow-up period.
Conclusions
The risk of CRS in FDNY firefighters appears increased with WTC-exposure, and has not diminished by time since exposure.
Keywords: Chronic rhinosinusitis, Disease latency, World Trade Center disaster
What this paper adds.
It is unknown for how long new incident chronic rhinosinusitis is associated with exposure to the World Trade Center (WTC) disaster.
Latency of chronic rhinosinusitis to any occupational exposure has not previously been researched.
There is an association of new onset chronic rhinosinusitis for at least a decade after exposure to the WTC disaster site.
There is need for continued monitoring and treatment of worker with high levels of exposure to the WTC site.
Introduction
The 9/11 terrorist attacks on the World Trade Center (WTC) created a man-made disaster of devastating magnitude resulting in great volumes of dust and debris being released into the environment. It has been estimated that approximately 70% of the towers’ structural components were pulverised during the collapse, producing small and large inhalable particulates.1 Adverse short-term and medium-term respiratory effects of work at the WTC disaster site have been widely documented in Fire Department of the City of New York (FDNY) first responders and others.2 3 We first reported WTC cough syndrome, demonstrated that work-related exposures to the disaster site increased the odds of aerodigestive symptoms up to 9 years post-11 September 2001, and showed that the prevalence of physician-diagnosed lower respiratory conditions, both self-reported and FDNY-physician diagnosed, remained elevated 7–9 years after working at the site.4 5 However, while the association between WTC exposure and lower respiratory conditions has been well documented, fewer studies have focused on upper airway disturbance such as chronic rhinosinusitis,6 7 a condition that can interfere with the demanding level of physical activity required to perform firefighting duties and may also inhibit the use of respirators and other breathing equipment.
CRS is a relatively common disorder that affects about 12.1% of the adult population.8 Risk factors include allergies, exposure to airborne irritants, immune system disorders and viral infections. About one in five people with CRS report asthma, the most common comorbidity with CRS.9 A defining symptom of CRS is nasal congestion, which can affect one's ability to breathe. This could interfere with satisfactory performance of any occupation requiring strenuous physical activity or respiratory mask use. CRS has also been associated with lost work productivity and occupational absenteeism.10 11
In two previous studies we showed that new onset obstructive airways disease (OAD) was associated with WTC exposure for more than 5 years,12 and for the first post-9/11 decade.13 We used innovative statistical methods—parametric survival models with change points—to examine the relationship between WTC exposure and new onset OAD in each study. For the current study, we extend the use of this methodology to address a similar question in CRS incidence. The study goal is to estimate the duration of the response gradient between different levels of WTC exposure and the incidence of new onset CRS among WTC-exposed FDNY firefighters.
Methods
The study population consisted of male firefighters who were active (ie, not retired) on 11 September 2001 and arrived at the disaster site within the first 2 weeks after 11 September 2001 and consented to research (N=10 449). We excluded individuals with pre-9/11 CRS (N=458) because we were only interested in new onset disease. We also required members to have had at least one visit to an FDNY physician at any time during the study period (11 September 2001–10 September 2011) to exclude individuals who had no opportunity to report a medical condition (N=143) for a final study population of 9848. The study was approved by the institutional review board at Montefiore Medical Center, Bronx, New York, USA.
Demographic information including age and race was obtained from the FDNY employee database. The FDNY health programme, run by the FDNY Bureau of Health Services, has used an electronic medical record since 1996. FDNY physician diagnoses with dates and sinus CT scan results were obtained from this electronic medical record. Since October 2001, FDNY Bureau of Health Services also has collected data from self-administered health questionnaires completed during routine monitoring examinations conducted every 12–18 months. We used questionnaire information to categorise WTC exposure and smoking status.
The exposure measure was based on initial arrival time at the WTC site as follows: High (arrived morning of 11 September 2001); Moderate (arrived during the afternoon of 11 September 2001 or any time on 12 September 2001); Low (arrived any day between 13 September 2001 and 24 September 2001).2 4 5
An individual was assigned a rhinosinusitis diagnosis for this study if he had at least one post-9/11 diagnosis of either CRS or irritant chronic rhinitis in his FDNY medical record during the follow-up period. We defined the period of risk as from 11 September 2001 to the first of either a CRS diagnosis, retirement or the end of study on 10 September 2011. In accordance with the 2003 guidelines from the American Academy of Otolaryngology-Head and Neck Surgery multidisciplinary Rhinosinusitis Task Force, we required confirmation of CRS diagnosis with an abnormal result from a diagnostic test, either nasal laryngoscopy or sinus CT scan, during the study period.14
We used piecewise exponential survival models with change points to estimate relative rates of CRS across the three exposure groups during follow-up (11 September 2001 to 10 September 2011). Piecewise exponential survival models are similar to Cox regression models, but with baseline hazards that can change at a fixed number of time intervals rather than with every new event. Cox regression models cannot be used because they assume exposure–response relationships are time-invariant and the purpose of this research is to study how exposure–response relationships change with time. Piecewise exponential survival models are equivalent to Poisson regression models with separate intercepts for each time interval. Accordingly, we used software for Poisson regression models (SAS V.9.4, PROC GENMOD; SAS Institute, Cary, North Carolina, USA, http://www.sas.com) for the analyses. We allowed the baseline hazard to change every 3 months over the follow-up period; longer intervals would not have captured seasonal changes in incidence, while shorter intervals might have resulted in unstable estimates because of sparse data. In this fully parametric approach, HRs have true relative rate interpretations. The change points are the times that the relative rates change (increase or decrease) during the follow-up period; these change points are estimated from the data using maximum likelihood. A change point after which relative incidences did not differ significantly from one would show that the exposure–response relationship between WTC exposure and CRS was limited to the period prior to the change point. All models included the following covariates: age on 11 September 2001, retirement status, if applicable, as a time-dependent predictor, and self-reported smoking status (ever vs. never) as of the last completed questionnaire.
Results
There were 1867 confirmed cases of CRS by the end of the study period, yielding cumulative incidences in the high, medium, and low exposure groups of 23.5%, 19% and 12.4%, respectively, despite similar mean ages on 11 September 2001, smoking status and race/ethnicity (table 1). New diagnoses of CRS dramatically increased in all exposure groups starting 5 years post-9/11 and peaked between 7 and 10 years post-9/11 (figure 1). Nonetheless, likelihood ratio tests indicated that there was no evidence for any change point in relative rates between different levels of exposures (figure 2) during the first 10 years of follow-up (likelihood ratio test p=0.162).
Table 1.
Demographics of Fire Department of the City of New York cohort by exposure group
| Exposure group | High | Moderate | Low | Total |
|---|---|---|---|---|
| Arrival time | 9 September am | 9 September pm to 12 September | 9 September to 24 September | |
| N | 1623 (16.5%) | 7025 (71.3%) | 1200 (12.2%) | 9848 |
| Mean age as of 11 September 2001 (SD) | 40.2 (7.3) | 39.9 (7.4) | 41.2 (7.9) | 40.1 (7.4) |
| (Range) | (21.3, 62.1) | (21.4, 64.3) | (22.5, 63.8) | (21.3, 64.3) |
| # Caucasian (% of non-missing) | 1487 (91.7%) | 6643 (94.6) | 1113 (92.8%) | 9243 (93.9%) |
| # Current smokers as of 11 September 2014 (% of non-missing) | 93 (5.7%) | 372 (5.3%) | 82 (6.8%) | 547 (5.6%) |
| # Former smokers as of 11 September 2014 (% of non-missing) | 505 (31.1%) | 2229 (31.7%) | 397 (33.1%) | 3131 (31.8%) |
| # Retired after 11 September 2001 (%) | 873 (53.8%) | 3344 (47.6%) | 635 (52.9%) | 4852 (49.3%) |
| Mean follow-up (years) (SD) | 8.2 (2.6) | 8.5 (2.4) | 8.5 (2.4) | 8.4 (2.4) |
| Mean # of physical examinations per firefighter (SD) | 32.5 (22.3) | 32.5 (22.5) | 30.7 (23.4) | 32.3 (22.6) |
| (Range) | (1, 138) | (0, 154) | (1, 148) | (0, 154) |
| Total diagnosed rhinosinusitis | 382 (23.5%) | 1336 (19%) | 149 (12.4%) | 1867 (19%) |
Figure 1.

Incident rates of chronic rhinosinusitis (CRS) in Fire Department of the City of New York (FDNY) cohort by exposure group throughout study period (11 September 2001 to 10 September 2011). High exposure: arrived morning of 11 September 2001. Moderate exposure: arrived afternoon of 11 September 2001 or anytime 12 September 2001. Low exposure: arrived any day between 13 September 2001 and 24 September 2001.
Figure 2.
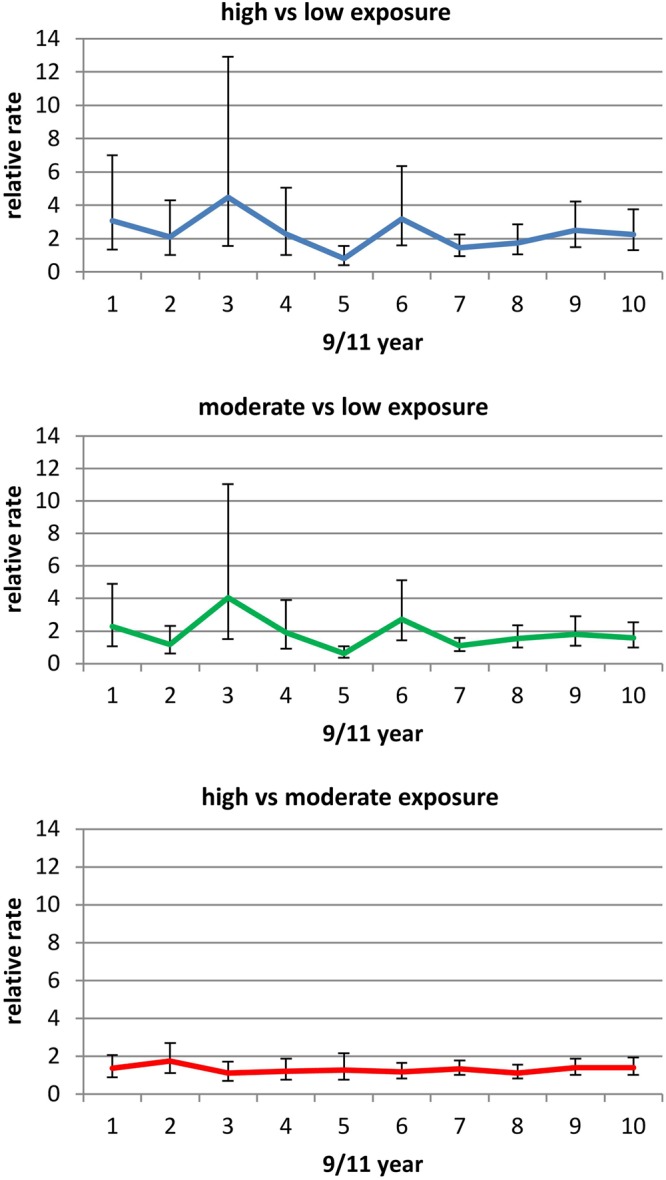
Relative rate of chronic rhinosinusitis (CRS) in Fire Department of the City of New York (FDNY) cohort throughout study period (11 September 2001 to 10 September 2011).
The relative rate of developing CRS for the most highly exposed compared with the least exposed was 1.98 (95% CI 1.64 to 2.39) during the 10-year follow-up period. The increased relative rates of CRS in high versus moderate (1.31) and moderate versus low (1.52) exposure groups were also statistically significant throughout the decade post-9/11, p values all <0.0001.
Discussion
This is the first study to look at latency in diagnoses of CRS resulting from WTC exposure. We found that the effect of exposure to the WTC disaster on incident CRS diagnoses persisted for 10 years after initial exposure. Those with the highest exposure were twice as likely to develop CRS as the least exposed. We reported similar results in our previous study of OAD latency where new OAD diagnoses were associated with WTC exposure for at least 7 years.
While we believe that many new CRS diagnoses were associated with WTC exposure for 10 years post-9/11, our results need to be interpreted with caution. In 2007, programmatic changes allowed prescribed medications to be provided free for WTC-related conditions. This programme change was followed by substantial increases in the number of FDNY physician examinations and diagnoses of CRS in all three exposure groups. So while there was a change in the overall number of diagnoses at around 2007, the zero change point model shows that there was no change in the relative incidence of diagnoses in the moderate and high exposure groups when compared with the lowest exposure group. When interpreting the time interval between WTC exposure and reported disease onset as indicated by diagnosis date, we are unable to distinguish between the natural history of the disease and the effects of increased surveillance due to the FDNY programmatic change, but we note that the exposure gradient remained through the end of follow-up.
The main limitation of this study is our inability to access the medical records of non-FDNY physicians. The change point analysis is based on the time of first FDNY-reported CRS diagnoses and we are unable to speculate on how the change point would have differed if FDNY members first were diagnosed by non-FDNY physicians. We also believe there is a possibility that CRS was generally overlooked by both patients and physicians in the first few years after 9/11 due to more severe morbidity associated with OAD in the patient population.2 15 Again, the time of the incident CRS diagnosis could be a reflection of the urgency to diagnose and treat other diseases soon after 9/11.
Despite these limitations, this study has several strengths. We relied on medical records and not self-reported disease, the latter being more subject to bias and therefore less accurate. While many large epidemiological studies use self-reports to estimate the disease burden in populations, we had access to all participants’ FDNY medical records, which we mined for CRS diagnoses. We also used uniform and stringent diagnostic criteria, including a confirmatory abnormal sinus CT result or nasal laryngoscopy at any time during the follow-up period. There were low rates of loss to follow-up in this population, and finally, we used an exposure measure that has been validated in other studies.2 4 5
Detection and treatment of rhinosinusitis is important given its impact on quality of life16 and its potential to lead to worsening asthma,17 of particular clinical significance given the high incidence of asthma in this and other cohorts of WTC-exposed responders post-9/11.4 5 Unique to this population of first responders with physically demanding jobs, rhinosinusitis makes it difficult for firefighters to wear respirators, a requirement for the safe performance of their duties.
In conclusion, this research supports the association of new onset CRS long after exposure to the WTC disaster site. It also confirms the need for continued monitoring and treatment of this highly exposed cohort.
Footnotes
Funding: This research was supported by the National Institute for Occupational Safety and Health, grant #1U01 OH010711-01: “For how long is WTC Exposure associated with Chronic Rhinosinusitis?” (PI: CBH).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Institutional Review Board of Albert Einstein College of Medicine and Montefiore Medical Center.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lioy PJ, Weisel CP, Millette JR, et al. . Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environ Health Perspect 2002;110:703–14. 10.1289/ehp.02110703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aldrich TK, Gustave J, Hall CB, et al. . Lung function in rescue workers at the World Trade Center after 7 years. N Engl J Med 2010;362:1263–72. 10.1056/NEJMoa0910087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farfel M, DiGrande L, Brackbill R, et al. . An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J Urban Health 2008;85:880–909. 10.1007/s11524-008-9317-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weakley J, Webber MP, Gustave J, et al. . Trends in respiratory diagnoses and symptoms of firefighters exposed to the World Trade Center disaster: 2005–2010. Prev Med 2011;53:364–9. 10.1016/j.ypmed.2011.09.001 [DOI] [PubMed] [Google Scholar]
- 5.Webber MP, Glaser MS, Weakley J, et al. . Physician-diagnosed respiratory conditions and mental health symptoms 7–9 years following the World Trade Center disaster. Am J Ind Med 2011;54:661–71. 10.1002/ajim.20993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin S, Reibman J, Bowers JA, et al. . Upper respiratory symptoms and other health effects among residents living near the World Trade Center site after September 11, 2001. Am J Epidemiol 2005;162:499–507. 10.1093/aje/kwi233 [DOI] [PubMed] [Google Scholar]
- 7.Reibman J, Liu M, Cheng Q, et al. . Characteristics of a residential and working community with diverse exposure to World Trade Center dust, gas, and fumes. J Occup Environ Med 2009;51:534–41. 10.1097/JOM.0b013e3181a0365b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Summary Health Statistics for US Adults: National Health Interview Survey, table 3,4 2015. http://www.cdc.gov/nchs/data/series/sr_10/sr10_260.pdf
- 9.Hamilos DL. Patient information: Chronic rhinosinusitis (Beyond the Basics) 2015.
- 10.Blanc PD, Trupin L, Eisner M, et al. . The work impact of asthma and rhinitis: findings from a population-based survey. J Clin Epidemiol 2001;54:610–18. 10.1016/S0895-4356(00)00349-8 [DOI] [PubMed] [Google Scholar]
- 11.Stankiewicz J, Tami T, Truitt T, et al. . Impact of chronic rhinosinusitis on work productivity through one-year follow-up after balloon dilation of the ethmoid infundibulum. Int Forum Allergy Rhinol 2011;1:38–45. 10.1002/alr.20008 [DOI] [PubMed] [Google Scholar]
- 12.Glaser MS, Webber MP, Zeig-Owens R, et al. . Estimating the time interval between exposure to the World Trade Center disaster and incident diagnoses of obstructive airway disease. Am J Epidemiol 2014;180:272–9. 10.1093/aje/kwu137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall CB, Liu X, Zeig-Owens R, et al. . The duration of an exposure response gradient between incident obstructive airways disease and work at the World Trade Center site: 2001–2011. PLoS Curr 2015;7 10.1371/currents.dis.8a93e7682624698558a76a1fa8c5893f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benninger MS, Ferguson BJ, Hadley JA, et al. . Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg 2003;129(3 Suppl):S1–32. 10.1016/S0194-5998(03)01397-4 [DOI] [PubMed] [Google Scholar]
- 15.Prezant DJ. World Trade Center cough syndrome and its treatment. Lung 2008;186(Suppl 1):S94–102. 10.1007/s00408-007-9051-9 [DOI] [PubMed] [Google Scholar]
- 16.Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngol Head Neck Surg 1995;113:104–9. 10.1016/S0194-5998(95)70152-4 [DOI] [PubMed] [Google Scholar]
- 17.Rachelefsky GS, Spector SL. Sinusitis and asthma. J Asthma 1990;27:1–3. 10.3109/02770909009073287 [DOI] [PubMed] [Google Scholar]


