Abstract
Objectives. The purpose of this research was to characterize the use of simulation in initial paramedic education programs in order assist stakeholders’ efforts to target educational initiatives and resources. This group sought to provide a snapshot of what simulation resources programs have or have access to and how they are used; faculty perceptions about simulation; whether program characteristics, resources, or faculty training influence simulation use; and if simulation resources are uniform for patients of all ages. Methods. This was a cross-sectional census survey of paramedic programs that were accredited or had a Letter of Review from the Committee on Accreditation of Educational Programs for the EMS Professions at the time of the study. The data were analyzed using descriptive statistics and chi-square analyses. Results. Of the 638 surveys sent, 389 valid responses (61%) were analyzed. Paramedic programs reported they have or have access to a wide range of simulation resources (task trainers [100%], simple manikins [100%], intermediate manikins [99%], advanced/fully programmable manikins [91%], live simulated patients [83%], computer-based [71%], and virtual reality [19%]); however, they do not consistently use them, particularly advanced (71%), live simulated patients (66%), computer-based (games, scenarios) (31%), and virtual reality (4%). Simulation equipment (of any type) reportedly sits idle and unused in (31%) of programs. Lack of training was cited as the most common reason. Personnel support specific to simulation was available in 44% of programs. Programs reported using simulation to replace skills more frequently than to replace field or clinical hours. Simulation goals included assessment, critical thinking, and problem-solving most frequently, and patient and crew safety least often. Programs using advanced manikins report manufacturers as their primary means of training (87%) and that 19% of faculty had no training specific to those manikins. Many (78%) respondents felt they should use more simulation. Conclusions. Paramedic programs have and have access to diverse simulation resources; however, faculty training and other program resources appear to influence their use.
Key words: : paramedic, education, simulation, emergency medical services, manikin
Introduction
Simulation is an increasingly important strategy in healthcare education. The term simulation can be interpreted in a variety of ways, but in this context it is used to describe techniques that imitate prehospital patient situations and are “designed to demonstrate procedures, decision-making, and critical thinking.” 1
The increasing trend in simulation use in healthcare education can be attributed to its many benefits. Notably, simulation allows standardization and consistent replication of patient conditions, it can provide a solution for overcoming limitations of clinical opportunities (e.g., low-frequency encounters), and simulation provides an opportunity for students to develop their skills without subjecting actual patients to risk. 2 Evidence from several healthcare disciplines has shown that simulation can improve knowledge and skill performance. 3–6 One study found paramedic student error rates were reduced when simulation was used to instruct specific program components. 7 The advantages of simulation-based education can likely be attributed to the reality that traditional clinical learning experiences often rely on chance encounters. 8
While such evidence of learning enhancement provides sufficient justification to support the use of simulation in initial paramedic education, there is also a growing body of evidence that supports the use of simulation as a substitute for selected clinical experiences. Several studies have reported that replacing a portion of clinical requirements with simulation is equal to, or in some cases, more effective than an equivalent clinical experience. 9–12 This evidence is of critical importance for emergency medical services (EMS) education, given the documented challenges of achieving targeted clinical and field skills and assessments among paramedic students 13 and the limited number of opportunities to perform advanced airway management on live patients. 14,15 Consequently, it is important for EMS education stakeholders to consider if and when it is appropriate to substitute simulation for skills, clinical hours, or field hours in paramedic programs. However, the answers to these questions are confounded by the existing lack of knowledge regarding the availability and use of simulation equipment and resources among initial paramedic education programs.
Further complicating the matter of simulation use in initial paramedic education is the reality that effective instruction using technology requires that educators have adequate knowledge about content, pedagogy (methods of teaching and learning), when to select a particular method to teach specific content, and the technology being used. 16 In order to attain this knowledge, appropriate faculty training is an essential element to the development of an effective simulation program. 17 There is little evidence in the literature describing simulation resources, how simulation is used, faculty training, or faculty perceptions about simulation in initial paramedic programs.
The purpose of this research project was to characterize the use of simulation in initial paramedic education programs. We specifically set out to provide a snapshot of the simulation resources currently available to paramedic education programs and to describe how those resources are used. We further sought to describe relationships between resource availability and use, while accounting for program characteristics, faculty training, and the perceptions of paramedic program faculty. The answers to these questions will provide essential knowledge for EMS stakeholders who seek to target educational initiatives and should serve as a cornerstone from which to build the body of knowledge pertaining to simulation use in initial paramedic education.
Methods
This research project was developed by a subcommittee of the National Association of EMS Educators’ Research Committee, composed of members with expertise in EMS education and healthcare simulation. The research proposal was determined to be exempt by the institutional review board of the University of Missouri –St. Louis.
Participants
This was a cross-sectional census survey of 638 paramedic programs that were either accredited by the Commission on Accreditation of Allied Health Education Programs (CAAHEP) as recommended by the Committee on Accreditation of Educational Programs for the Emergency Medical Services Professions (CoAEMSP) or holding a letter of review (in the “becoming accredited” process) as of November 13, 2013. 18, 19
Instrument
The survey instrument was developed and revised using a consensus decision-making approach. 20 The National Council for State Boards of Nursing (NCSBN) simulation survey was used as a launching point to develop the research instrument. 21 The survey was piloted and author K. McKenna conducted cognitive interviews to probe respondents’ understanding of the questions with eight additional paramedic programs representing diverse geographic and program sponsorship types. The committee made final changes to the instrument based on data collected from these interviews.
The survey instrument consisted of 56 multiple-choice and open-ended questions that were divided into sections relating to simulation equipment, faculty training, simulation methodology, program characteristics and logistics, faculty perceptions about simulation use, and program demographics. Programs were first asked to identify simulation equipment they have or have access to, and, later, which equipment they used in the most recently graduated paramedic class. Simulation equipment was categorized as task trainers (e.g., IV arm; airway head); manikins-simple (e.g., CPR manikin); manikins-intermediate (e.g., with airway, IV, ECG); manikins-advanced (fully programmable); standardized/simulated live patients; computer-based (games, scenarios); and virtual reality (3D or complex computer-generated images or haptic [create kinesthetic or tactile perception]) simulation.
Procedures
The Dillman tailored design was used to develop and distribute the survey electronically by email using Qualtrics survey software with three electronic and one telephone reminder to nonresponders. 22 The survey was open from November 15, 2013 to December 19, 2013. Participation was voluntary, and the participants were instructed that they could leave the survey at any time. All participants who initiated the survey process were eligible to enter a prize drawing regardless of survey completion. Systems were in place to assure that no individually identifiable results would be disclosed.
Analysis
De-identified raw data were exported from Qualtrics survey software into SPSS (version 21) for statistical analysis. Incomplete responses and respondents who declined to consent were excluded. The data were coded in preparation for analysis, and descriptive statistics were conducted. We then examined the relationships between resource availability and use, faculty training, and the perceptions of paramedic program faculty using chi-square analysis (due to the categorical nature of most variables) in order to answer our research questions.
Results
The survey generated 389 valid responses (61% response rate). The program location was categorized using the Federal Emergency Management Agency (FEMA) regions to protect the confidentiality of individual programs. 23 We then compared the relative frequencies of program location for all programs against those that responded in order to explore the response distribution and determine representativeness for our sample (Figure 1).
Figure 1. .
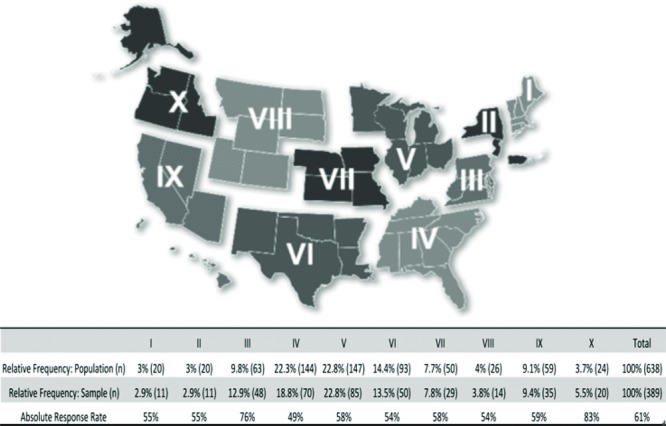
Relative frequency of paramedic program location and response rates by geographic (FEMA) regions.
Post-secondary institutions constituted the largest group of responses (75%), which consisted of two-year colleges (77%), four-year colleges or universities (13%), technical schools (9%), and other (1%). The remaining institutional sponsorship types included hospital, clinic, or medical center (12%), consortium (6%), governmental education or medical service (fire or EMS agency)(4%), and other (3%). One respondent did not know what type of institutional sponsorship his/her program had.
The majority of respondents (80%) classified their program's sponsoring institution as public, 14% as private: not-for-profit and 6% as private: for-profit. One-half of programs award an associate's degree, 48% a certificate-only, while only 2% award a bachelor's degree. Program length ranged from 3 to 45 months (M = 13.38, SD = 5.06). Total average annual student enrollment varied widely, but 65% of programs had between 11 and 35 students enrolled annually. Likewise, average individual class cohort size was between 11 and 35 students for 84% of programs.
We used chi-square analyses to explore potential relationships between each of the previously described program characteristics and our findings related to simulation equipment, resources, faculty training, and methods. No significant relationships were identified.
Simulation Resources
All program respondents have or have access to task trainers, and most (97%) use them (Table 1). Simple manikins were available to 100% of programs; however, only 92% reported using them. This was true for intermediate manikins as well, which are used by just 93% of programs despite our finding that 99% of all programs have or have access to them.
Table 1. .
Percentage of programs using specific task trainers
| Task trainer (simulators) used | n (%) |
|---|---|
| Airway manikins | 370 (100) |
| Intravenous arm | 365 (100) |
| Intraosseous | 362 (98) |
| ECG (3/4 lead) | 361 (98) |
| AED trainer | 341 (92) |
| Chest decompression | 336 (91) |
| Childbirth (pelvic delivery) | 325 (88) |
| Cricothyroid | 324 (87) |
| ECG (12 lead) | 309 (84) |
| Breath sound | 230 (62) |
| Heart sound | 151 (41) |
| Blood pressure | 145 (39) |
| Other | 27 (7) |
Trainers reported in the “other” category included central vascular access trainers (5), chest tube trainers, choking simulator, intramuscular or subcutaneous trainer (4), umbilical catheter (2) and others.
Advanced manikins were available to 91% of programs (76% have and 15% have access to), but only 71% of these programs indicated that they use them. This is a wider gap than in all other manikin types reported. A series of chi-square analyses showed that programs that reported “having access to” a given simulation resource use that resource less frequently than programs that reported “having” the same resource (Figure 2). There are further differences among the group who reported using advanced manikins, as it appears that the frequency of simulation with adult manikins is substantially greater (99%) than is simulation with child (43%), infant (46%), or neonate (18%) manikins.
Figure 2. .
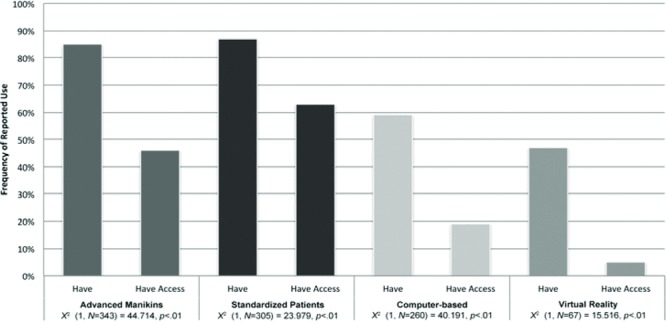
Comparison of simulation use based on availability of simulation resources.
Availability and use of simulation methods other than manikins was less frequent. Live simulated patients were accessible in 83% of programs, and 66% use them. Computer-based simulation was available to 71% of programs, but a much smaller percentage (31%) report they use it. Only 19% of all programs indicate access to virtual reality training and almost none of them (4%) use it.
Just under one-third of programs (31%) indicated they have simulation equipment that sits idle and unused. Most programs identified advanced manikins as the most expensive equipment sitting idle, but a simulation laboratory, a simulated ambulance, intermediate manikins, a simple manikin, task trainers, and four virtual reality simulation aids were also among the equipment reported as unused. Many of these respondents cited lack of training as the top reason equipment was not used, although a variety of other factors were identified (Table 2). The results of two chi-square analyses identified significant differences between the extent of reported faculty training and personnel resources with regard to the frequency with which simulation was used. We found that better faculty education resources χ2 (1, N = 377) = 50.112, p < 0.01 and personnel resources χ2 (1, N = 374) = 24.388, p < 0.01 were reported more frequently in programs in which equipment was not idle.
Table 2. .
Reasons simulation equipment sits idle and unused
| Resource | n (%) |
|---|---|
| Inadequate training | 31 (26) |
| Inadequate personnel | 23 (19) |
| Inadequate time | 17 (14) |
| Inadequate technical resources | 13 (11) |
| Other department will not allow | 3 (3) |
| No space to set up | 3 (3) |
| Other | 31 (26) |
Reasons for idle equipment in the “other” category included class scheduling or sequencing, staff resistance or lack of confidence, equipment that was broken or outdated, and others.
Among the programs that indicated they have or have access to advanced manikins, 81% reported their core faculty received training related to simulation specific to those manikins. These programs reported more training on manikin features, simulation operations, instructor roles, and debriefing than on programming and technological trouble-shooting. The least training was reported in the use of video (Table 3).
Table 3. .
Core faculty training on advanced (fully programmable) manikins
| Training type | None n (%) | Minimal n (%) | Some n (%) | A lot n (%) |
|---|---|---|---|---|
| Manikin features | 1 (<1) | 12 (5) | 130 (58) | 83 (37) |
| Simulator operations | 1 (<1) | 18 (8) | 123 (56) | 79 (36) |
| Instructor roles | 1 (<1) | 21 (9) | 138 (61) | 68 (30) |
| Debriefing | 6 (3) | 38 (17) | 126 (56) | 55 (24) |
| Programming | 13 (6) | 67 (30) | 114 (51) | 28 (13) |
| Technical trouble-shooting | 16 (7) | 77 (34) | 110 (49) | 23 (10) |
| Video use | 24 (11) | 74 (33) | 95 (43) | 30 (14) |
Faculty training by manufacturer representatives was the most frequent type of education and was reported by 87% of program respondents who indicated core faculty had advanced manikin training. Other fully programmable manikin simulation training included conference (37%); local or regional expert (33%); vendor workshops, such as Simulation User's Group Conference (SMUG) or Simulation User Network (SUN) (29%); other (8%); and certificate (4%). Of those who indicated other training, 13 said a peer or in-house expert provided training.
Only 44% of programs reported the availability of personnel support (above regular faculty hours) to support simulation activities (Table 4).
Table 4. .
Simulation personnel resources availability
| Type of support | n (%) |
|---|---|
| Simulation lab support (programming, AV, set-up) | 89 (23) |
| Simulation lab operators (run the computers) | 80 (21) |
| Manikin maintenance | 78 (20) |
| Equipment manager | 75 (19) |
| Other | 18 (5) |
| None | 216 (56) |
Programs were divided on their opinions about their resource adequacy related to all types of simulation. Over half felt their physical facilities (71%), simulation equipment (59%), and personnel (55%) were adequate. However, less than half of the programs indicated that the faculty training (48%) and annual budget line were adequate (48%).
Simulation Methods
The most frequently reported purpose of simulation use among the paramedic programs that responded was skills instruction, with 89% of programs reporting they used it for that reason often or all of the time. Only 2% of programs indicated they never or rarely use simulation to teach skills.
Programs reported using simulation to substitute for skills required in clinical or field “All of the time,” “Often,” or “Sometimes” with greater frequency (43%) than they did to replace clinical hours (13%) or field internship hours (8%). Only 23% of programs said they “Never” use simulation to replace required field or clinical skills as compared to 66% who said they never substitute simulation for clinical and 77% of programs that do not substitute simulation for field internship hours.
Pediatric intubation is the most frequent skill required in clinical or field settings that is reportedly substituted with simulation, whereas medication administration and intravenous access are the least frequently substituted skills (Table 5).
Table 5. .
Frequency of simulation substitution for skills required during clinical or field
| Never n (%) | Rarely n (%) | Sometimes n (%) | Often n (%) | All of the time n (%) | Skill not required n (%) | |
|---|---|---|---|---|---|---|
| Pediatric intubation | 34 (12) | 31 (11) | 49 (17) | 90 (32) | 63 (22) | 17 (6) |
| Intraosseous insertion | 59 (21) | 39 (14) | 57 (20) | 77 (27) | 36 (13) | 16 (6) |
| Electrical therapy | 72 (25) | 45 (16) | 62 (22) | 66 (23) | 29 (10) | 10 (4) |
| Supraglottic airway | 72 (25) | 53 (19) | 62 (22) | 57 (20) | 32 (11) | 8 (3) |
| Childbirth | 91 (32) | 35 (13) | 61 (22) | 56 (20) | 27 (10) | 11 (4) |
| Adult intubation | 72 (25) | 65 (23) | 66 (23) | 60 (21) | 22 (8) | |
| Endotracheal suction | 94 (33) | 45 (16) | 70 (25) | 39 (14) | 19 (7) | 15 (5) |
| Patient assessment | 157 (56) | 53 (19) | 45 (16) | 16 (6) | 11 (4) | 1 (<1) |
| Intravenous access | 168 (59) | 53 (19) | 37 (13) | 16 (6) | 11 (4) | |
| Medication administration | 168 (59) | 52 (18) | 39 (14) | 16 (6) | 10 (4) |
Of 289 programs that indicated they replace skills required in clinical or field
Simulation was reportedly used “All of the time” or “Often” by 68% of programs for formative assessment such as quizzes or ungraded assignments. Only 49% of programs reported that simulation is used “All of the time” or “Often” for summative (high-stakes) assessment.
Simulation scenarios incorporated diverse goals in respondents’ programs, with patient assessment being the most frequent. The goal of patient safety (medical errors, lifting/moving) was reportedly used least often (Table 6).
Table 6. .
Simulation goal frequency
| Never n (%) | Rarely n (%) | Sometimes n (%) | Often n (%) | All of the time n (%) | |
|---|---|---|---|---|---|
| Patient assessment | 1 (<1) | 1 (<1) | 26 (7) | 130 (35) | 215 (58) |
| Critical thinking | 1 (<1) | 4 (1) | 24 (6) | 149 (40) | 195 (52) |
| Clinical decision-making | 1 (<1) | 5 (1) | 32 (9) | 153 (41) | 183 (49) |
| Problem-solving | 1 (<1) | 4 (1) | 34 (9) | 152 (41) | 182 (49) |
| Team leader | 1 (<1) | 6 (2) | 33 (9) | 152 (41) | 179 (48) |
| Team member | 2 (1) | 6 (2) | 41 (11) | 145 (39) | 176 (48) |
| Communication | 3 (1) | 10 (3) | 57 (15) | 138 (37) | 165 (44) |
| Crew safety | 10 (3) | 29 (8) | 70 (19) | 101 (27) | 162 (44) |
| Patient safety (medical errors, lifting/moving) | 10 (3) | 38 (10) | 86 (23) | 122 (33) | 115 (31) |
Over three-fourths (78%) of paramedic program respondents felt they should use more simulation in their programs. No program indicated that less simulation should be used. A chi-square analysis demonstrated a significant relationship between wanting to use more simulation and the perceived adequacy of faculty education (χ 2 (1, N = 371) = 9.665, p < 0.01). Programs that indicated a desire to use more simulation less frequently reported a perceived adequacy of personnel (χ 2(1, N = 367) = 14.512, p < 0.01) and more frequently reported that they have no personnel support (above regular faculty) dedicated to simulation-related activities (χ 2(1, N = 374) = 9.154, p < 0.01).
The top barriers to advanced simulation specified by those who would like to use more advanced simulation in their programs were faculty training, staff resources, and money to purchase equipment (Table 7).
Table 7. .
Barriers to advanced simulation use
| Barrier | n (%) |
|---|---|
| Training –facilitating simulation | 195 (67) |
| Training –writing scenarios | 193 (67) |
| Time to write scenarios | 177 (61) |
| Staff to run simulation | 174 (60) |
| Money to purchase resources | 169 (58) |
| Training –debriefing simulation | 136 (47) |
| Money to schedule time | 81 (28) |
| Difficult to schedule resources | 77 (27) |
In programs reporting they should use more simulation (n = 290)
Discussion
The results of this study indicate that most accredited paramedic programs have or have access to diverse simulation resources. While 91% of programs reported having or having access to advanced, fully programmable manikins, only 71% use them. Programs that actually have advanced manikins were more likely to use them than those who only reported having access to those same resources. Program respondents were substantially less likely to use advanced neonate, infant and pediatric as compared to adult simulation manikins. While the 2009 National EMS Education Standards do not specify the number of hours to be devoted to infant and child topics during a paramedic program, the National Registry of EMTs cognitive examination test blueprint indicates that 15% of each clinical area (airway, medical, cardiac, and trauma) relate to infants and children. 24,25 In a review of paramedic clinical records, Brazelton et al. found that paramedic students only saw an average of 24.6 ± 16.6 pediatric patients during clinical and only 5.6 ± 4.6 children while in their field internship. 26 Additionally, Kokx et al. reported that most pediatric patients encountered during paramedic clinical and field experiences were school-age and older. 27 They recommended that educators identify strategies to increase paramedic student exposure to children. Without appropriate age-related simulation resources, it is unlikely paramedic programs will be able to increase student exposure to a variety of critical situations in young patients.
A large number of programs have equipment, in many cases very expensive manikins and other resources, that sits unused. This study makes it clear that merely having or having access to the equipment does not guarantee it will be used. This is especially true when programs share resources, which significantly reduces their use of them.
These results also point out that a lack of paramedic program faculty training related to simulation is an area of weakness and impacts the likelihood that simulation equipment will be used. This is particularly true with advanced simulation technology. Despite the evidence that faculty preparation is an essential element of a successful simulation program, Waxman and Miller noted that in some healthcare programs, simulation programs were able to start up with equipment purchased using grant funds, yet “minimal attention has been paid to faculty development.” 28 It is unrealistic to think that faculty would develop expertise in simulation without appropriate education and mentoring, yet Jeffries points out that in nursing programs simulation equipment is purchased with the tacit understanding that faculty will adopt the technology, when in fact they are not prepared to do so. 29 Aside from mastering the mechanical operation of advanced simulation manikins, effective facilitation when using advanced simulation requires a shift from the teacher as “dispenser of information” to that of a moderator. 28 The difficulty in making that shift was illustrated in respondent comments indicating that their staff was “resistant to” or “not comfortable” using simulation.
More than one-half of programs reported no personnel resources to support simulation above regular faculty hours. This resource deficit was significantly related to less use of simulation resources and the desire by programs to use simulation more often.
When considering the many reasons to use simulation in initial paramedic education, our finding that patient and crew safety were the least-frequently reported simulation goals is a potential cause for concern. Simulation scenarios are an ideal strategy to rehearse skills essential for patient safety by permitting practice of high-risk, low-frequency skills or situations. They also allow the learner to develop routines and practice safety behaviors, such as “safety checks, interruptions, stressors, adverse events, and handoffs.” 30 Because of these features, safety should be a key goal of interdisciplinary simulation. 31 It may be that safety is being addressed indirectly, because some of the more commonly reported goals in this study (e.g., teamwork and decision-making) are the core components of safety programs, such as Crew Resource Management. The use of such programs has been shown to improve these skills in a simulated prehospital setting, which may result in improved patient and crew safety by addressing deficiencies that could otherwise lead to medical errors. 32 As such, it may be that more of this disparity resides in how the goals are framed rather than being a matter of goal priority. Nonetheless, both U.S. and Canadian safety reports emphasize the need to integrate a culture of safety within each component of EMS education, chiefly by improving clinical decision-making skills and by instilling the knowledge of how safe patient care is influenced by individual and system factors. 33,34 To ensure students incorporate safety principles within their practice, both patient and crew safety goals should be explicitly integrated within simulation scenarios.
Many respondents felt they should use more simulation, which is consistent with Hayden's findings in nursing programs. 35 We identified faculty training, equipment, and personnel as factors significantly associated with underuse of simulation. A lack of personnel resources was also noted to be a barrier to simulation in nursing programs. 35
Presently simulation is substituted for skills required in clinical (hospital) or field rotations much more frequently than it is for hours of clinical or field (ambulance) rotations. In 2010 Hayden reported that nursing programs substituted simulation for clinical hours 69% of the time. 35 Recent evidence suggests that substituting simulation for some of the clinical experience results in equivalent or at least not worse outcomes than for clinical. 9–12 Despite this, there is no clear guidance in EMS related to when it is appropriate to substitute simulation for clinical or field experience.
This study leaves many unanswered questions related to the use of simulation in paramedic programs. As a result of a gap in the literature, we relied heavily on findings of simulation research from other healthcare fields; however, consideration should be given to the unique attributes of EMS and the associated challenges of simulating such a dynamic environment. These differences pose a concern when attempting to translate the findings of nonspecific healthcare simulation research and likely indicate a need to develop a body of knowledge specific to the use of simulation in EMS education.
Limitations
The population of paramedic programs chosen for this research included only accredited paramedic programs (or those formally in the process of becoming accredited). National paramedic program accreditation is a component of the EMS system infrastructure identified in the EMS Education Agenda for the Future. 36 All programs using the NREMT cognitive examination (NREMT-C) as a credentialing test for licensure or certification were required to have national accreditation by January 1, 2013 to be eligible to test. 37 Presently, 44 states use the NREMT-C as a prerequisite for paramedic licensure.38Therefore, nonaccredited programs in the six states not using the NREMT-C were not included.
The comparative data for the FEMA regions was measured on February 19, 2014, approximately 3 months after the survey data was gathered. Given the frequent changes in the number of programs with CoAEMSP letter of review or accreditation, there may have been a different number of CoAEMSP programs at the time of the survey. Although the recruitment email was sent to the program director of each paramedic program, there is no way to assure that the program director alone completed the survey. Additionally, the results may be influenced by nonresponse bias. The questions related to frequency with which skills and hours were substituted did not specify a particular time period. Therefore, detailed characteristics about program directors’ substitutions practices are unknown.
Data were gathered from the program director viewpoint and do not explore individual faculty or student perspectives. Future research should explore which types of education and mentorship assure smooth and effective adoption of effective simulation that promotes paramedic student learning.
Conclusion
These results suggest that simulation in accredited paramedic programs mirrors the proverbial three-legged stool. To ensure simulation is used effectively, programs must have the appropriate equipment, faculty training, and resources. If any of these elements is missing, the stool topples and programs are less likely to use simulation. Administrators must recognize that to maximize the use of simulation within their program, they must view simulation as a fully integrated strategy within their education system. This research provides data for accredited paramedic program personnel to present to administrators to justify requests for faculty education and personnel resources to maximize the use of their simulation equipment.
It is incumbent on program directors to ensure that their faculty has adequate initial and ongoing simulation education, mentors to assist with adoption of new technologies, and sufficient personnel resources and equipment (representing patients of all ages) to promote the most effective use of simulation. Regional and national simulation work groups should be developed to allow faculty to collaborate on simulation best practices within accredited paramedic programs. While there are standardized resources to train nursing faculty on how to use simulation, and generic simulation instruction competencies for healthcare, no specific framework exists specifically geared to guide simulation best practices in the unique prehospital environment. The EMS community should collaborate to provide that framework so that the three-legged stool of simulation will stand firmly on a solid pedagogical foundation to serve as an essential tool for paramedic student learning.
Declaration of Interest
Laerdal Medical Corporation, a corporate sponsor of NAEMSE, provided financial support for this research. K. McKenna and J. Todaro serve on the NAEMSE board of directors and J. Freel is the executive director. Funds were used to support committee meetings and expenses related to the study. The study was conducted independently of the funders.
References
- Jeffries PR. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs Educ Perspect. 2005;26:96–103. [PubMed] [Google Scholar]
- Rodgers DL. High-fidelity patient simulation: a descriptive white paper report. Healthcare Simul Strategies. 2007;10:68–77. [Google Scholar]
- Simon EL, Lecat PJ, Haller NA, Williams C J, Martin SW, Carney JA, Pakiela JA. Improved auscultation skills in paramedic students using a modified stethoscope. J Emerg Med. 2012;43:1091–7. doi: 10.1016/j.jemermed.2012.01.048. [DOI] [PubMed] [Google Scholar]
- Cook, D. A., Hatala, R., Brydges, R., Zendejas, B., Szosteck, J. H., Wang, A. T., Erwin, P. J., Hamstra, S. J. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. 2011;306:978–988. doi: 10.1001/jama.2011.1234. JAMA. [DOI] [PubMed] [Google Scholar]
- Dickison P. D. The Ohio State University; Columbus, Ohio: Using computer-based clinical simulations to improve student score on the paramedic national credentialing examination. Thesis. Retrieved from etd.ohiolink.edu/ 2010. [Google Scholar]
- Gordon D. L., Issenberg S. B., Gordon M. S., LaCombe D., McGaghie W. C., Petrusa E. R. Stroke training of prehospital providers: an example of simulation-enhanced blended learning and evaluation. Med Teacher. 2005:114–21. doi: 10.1080/01421590400029756. [DOI] [PubMed] [Google Scholar]
- Wyatt A., Fallows B., Archer F. Do clinical simulations using a human patient simulator in the education of paramedics in trauma care reduce error rates in preclinical performance. Prehosp Emerg Care. 2004;8:435–6. [Google Scholar]
- Motola I., Devine L. A., Chung H. S., Sullivan J. E., Issenberg S. B. Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Med Teacher. 2013;35:e1511–e1530. doi: 10.3109/0142159X.2013.818632. [DOI] [PubMed] [Google Scholar]
- Hayden J. K., Smiley R. A., Alexander M., Kardong-Edgren S., Jeffries M. R. The NCSBN National Simulation Study: a longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. J Nurs Regul. 2014;5(2):S1–S64. [Google Scholar]
- Watson K., Wright A., Morris N., McMeeken J., Rivett D., Blackstock F., Jones A., Haines T., O'Connor V., Watson G., Peterson R., Jull G. Can simulation replace part of clinical time? Two parallel randomised controlled trials. Med Educ. 2012;46:657–67. doi: 10.1111/j.1365-2923.2012.04295.x. [DOI] [PubMed] [Google Scholar]
- McGaghie W. C., Issenberg S. B., Cohen E. R., Barsuk J. H., Wayne D., B. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86:706–11. doi: 10.1097/ACM.0b013e318217e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall R. E., Plant J. R., Bands C. J., Wall A. R., Kang J., Hall C. A. Human patient simulation is effective for teaching paramedic students endotracheal intubation. Acad Emerg Med. 2005;12:850–5. doi: 10.1197/j.aem.2005.04.007. [DOI] [PubMed] [Google Scholar]
- Salzman J. G., Page D. I., Kaye K., Stethman N. Paramedic student adherence to the National Standard Curriculum recommendations. Prehosp Emerg Care. 2007;11:448–52. doi: 10.1080/10903120701536701. [DOI] [PubMed] [Google Scholar]
- Westergard B. C., Peterson B. K., Salzman J. G., Anderson R., Buldra M., Burnett A. M. Longitudinal and regional trends in paramedic student exposure to advanced airway placement: 2001–2011. Prehosp Emerg Care. 2013;17:379–85. doi: 10.3109/10903127.2013.764949. [DOI] [PubMed] [Google Scholar]
- Johnston B., Seitz S. R., Wang H. E. Limited opportunities for paramedic student endotracheal intubation training in the operating room. Acad Emerg Med. 2006;13:1051–5. doi: 10.1197/j.aem.2006.06.031. [DOI] [PubMed] [Google Scholar]
- Mishra P., Koehler M. Technological pedagogical content knowledge: a framework for teacher knowledge. Teachers College Rec. 2006;108:1017–94. [Google Scholar]
- Waxman K. T., Miller MA. Faculty development to implement simulations: strategies and possibilities. Clinical Simulations in Nursing Education: Advanced Concepts, Trends, and Opportunities. In: Jeffries PR, editor. Philadelphia, PA: Wolters Kluwer, Lippincott, Williams & Wilkins; 2014. [Google Scholar]
- Commission on Accreditation of Allied Health Education Programs. What is CAAHEP. 2014 www.caahep.org : CAAHEP. [Google Scholar]
- Committee on Accreditation of Educational Programs for the Emergency Medical Service Professions. CoAEMSP. 2014 www.coaemsp.org; CoAEMSP. [Google Scholar]
- Dyer J. R. G., Johansson A., Helbing D., Couzin I., D., Krause J. Leadership, consensus decision making and collective behavior in humans. Philos Trans R Soc. 2009;364:781–9. doi: 10.1098/rstb.2008.0233. 1098/rstb.2008.0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chicago, IL: 2010. National Council of State Boards of Nursing. Simulation Use in Prelicensure Nursing Programs. [Google Scholar]
- Dillman D. A., Smyth J., D., Christian L. M. 3rd ed. Hoboken, NJ: Wiley; 2007. Internet, Mail and Mixed-mode Surveys: The Tailored Design Method. [Google Scholar]
- Federal Emergency Management Agency. Regional Operations. Retrieved 8/30/14 from www.fema.gov/regional-operations . [Google Scholar]
- Washington: Department of Transportation; 2009. U.S. Department of Transportation, National Highway Traffic Safety Administration. National EMS Education Standards. (DOT HS 811 077A) Retrieved from www.ems.gov/pdf/811077a.pdf . [Google Scholar]
- Columbus, OH: National Registry of EMTs; National Registry of EMTs. 2009 National EMS Practice Analysis. [Google Scholar]
- Brazelton T., Wewerka S. S., Burnett A. M., Carhart E., Danielson L., Tritt P., Kokx G., Studnek J. R. Washington, DC: 2013. Hide or go seek: Do more pediatric encounters make better paramedics? Paper presented at the National Association of EMS Educators Annual Symposium. [Google Scholar]
- Kokx G., Wewerka S. S., Brazelton T. B., Romero G. A., Hanson K., Holyoke L., Syverson S. Orlando, FL: 2012. Childlike wonder: the current state of paramedic student pediatric clinical education. Paper presented at the National Association of EMS Educators. [Google Scholar]
- Waxman K. T., Miller M., A. Faculty development to implement simulations: strategies and possibilities. Clinical Simulations in Nursing Education: Advanced Concepts, Trends, and Opportunities. In: Jeffries PR, editor. Philadelphia, PA: Wolters Kluwer, Lippincott, Williams & Wilkins; 2014. 9, 12. [Google Scholar]
- Jeffries P. R. Getting in STEP with simulations. Nurs Educ Perspect. 2008;29:70–3. doi: 10.1097/00024776-200803000-00006. [DOI] [PubMed] [Google Scholar]
- Reising D. L., Hensel D. Clinical simulations focused on patient safety. Clinical Simulations in Nursing Education: Advanced Concepts, Trends, and Opportunities. In: Jeffries PR, editor. Philadelphia, PA: Wolters Kluwer, Lippincott, Williams & Wilkins; 2014. [Google Scholar]
- Palaganas J. C., Mancini M. E. Interprofessional education using clinical simulations. Clinical Simulations in Nursing Education: Advanced Concepts, Trends, and Opportunities. In: Jeffries PR, editor. Philadelphia, PA: Wolters Kluwer, Lippincott, Williams & Wilkins; 2014. pp. 58–70. [Google Scholar]
- Carhart E. Available from ProQuest Dissertations and Theses database; 2012. Effects of Crew Resource Management Training on Medical Errors in a Simulated Prehospital Environment. Thesis. (UMI No. 3534980) [Google Scholar]
- Bigham B. L., Bull E., Morrison M., Burgess R., Maher J., Brooks, Morrison L. J. Pan-Canadian Patient Safety in EMS Advisory Group. Patient safety in emergency medical services: executive summary and recommendations from the Niagra Summit. Can J Emerg Med. 2011;13:13–8. doi: 10.2310/8000.2011.100232. [DOI] [PubMed] [Google Scholar]
- Strategy for a National EMS Culture of Safety; 2013. National Highway Traffic Safety Administration, Health Resources and Services Administration EMS for Children, & American College of Emergency Physicians. [Google Scholar]
- Hayden J. Use of simulation in nursing education: national survey results. J Nurs Regul. 2010;1:52–57. [Google Scholar]
- Washington, DC: U.S. Department of Health and Human Services; 2000. U.S. Department of Transportation, National Highway Traffic Safety Administration. Emergency Medical Services Education Agenda for the Future: A Systems Approach. (DOT HS 809 042) Retrieved from www.nhtsa.gov/people/injury/ems/FinalEducationAgenda. pdf . [Google Scholar]
- National Registry of EMTs. Paramedic accreditation implementation policy. 2012 Retrieved 8/30/2014, from www.nremt.org/nremt/about/search.asp#1 ,CAAHEP. [Google Scholar]
- National Registry of EMTs. State reciprocity. 2014 Retrieved 8/30/14 from www.nremt.org/nremt/about/stateReciprocity Map.asp . [Google Scholar]


