Abstract
Purpose
Cubital tunnel syndrome is the second most common compression neuropathy in the upper extremity. A variety of procedures are used for treatment of cubital tunnel syndrome. There is a lack of consensus regarding the most appropriate procedure owing to similar rates of operative success and strong proponents for each technique. Our aim was to examine trends in and determinants of the use of different procedures for treatment of cubital tunnel syndrome.
Methods
We performed a retrospective cross-sectional analysis of the Healthcare Cost and Utilization Project Florida State Ambulatory Surgery Database for 2005 to 2012. We selected all patients who underwent in-situ decompression, transposition, or other surgical treatments for cubital tunnel syndrome. We tested trends in the use of these techniques and performed a multivariable analysis to examine associations between patient characteristics and surgeon case volume and the use of different techniques.
Results
Of the 26,164 patients who underwent surgery for cubital tunnel syndrome, 79.7% underwent in-situ decompression, 16.2% underwent transposition, and 4.1% underwent other surgical treatment. Over the study period, there was a statistically significant increase in the use of in-situ release and a decrease in the use of transposition. Females and patients treated by surgeons with a higher cubital tunnel surgery case volume underwent in-situ release at a statistically higher rate than other techniques.
Conclusions
In Florida, surgeon practice reflects the widespread adoption of in-situ release as the primary treatment for cubital tunnel syndrome and these numbers are increasing. Patient demographics and surgeon-level factors influence procedure selection.
Level of Evidence
III, Therapeutic
Keywords: cubital tunnel syndrome, surgeon volume, in-situ decompression, ulnar nerve transposition, medial epicondylectomy
Introduction
Ulnar nerve entrapment at the elbow is the second most common compression neuropathy in the upper extremity (1, 2). The incidence is estimated at 25 cases per 100,000 person-years (3, 4), affecting men twice as frequently as women (5). In many patients, the progressive disability resulting from ongoing pain, paresthesias, and muscle weakness (6-10) has a considerable economic impact. Juratli et al. (11) found that nearly half of all workers with ulnar neuropathy at the elbow were receiving disability benefits prior to their official diagnosis. Cubital tunnel syndrome, therefore, has important functional and financial implications for patients.
A variety of surgical approaches are used for the treatment of cubital tunnel syndrome. These include in-situ decompression, nerve transposition techniques, and other techniques such as medial epicondylectomy (2, 12, 13). There is disagreement in the literature regarding the most commonly used method of treatment for cubital tunnel syndrome (5, 14-16). Furthermore, recent literature has shown no difference in treatment effectiveness between in-situ decompression and transposition, although fewer complications have been reported after in-situ decompression (17-30). These findings underscore the challenges associated with selecting the most appropriate procedure for cubital tunnel syndrome treatment.
A survey by Hagemen et al. (31) demonstrated that surgeons in the U.S. rely on “what works in my hands”, “familiarity with treatment”, or “what my mentor taught me” when faced with inconclusive evidence. The choice of operative treatment continues to be largely based on the surgeon's preference and experience (32-34). In this study, we sought to evaluate trends in and associations with the use of different surgical techniques for management of cubital tunnel syndrome. We hypothesize that socio-demographic patient factors and surgeon case volume will be significantly associated with the use of specific surgical techniques for treatment of cubital tunnel syndrome.
Materials and Methods
Data Source
We performed a cross-sectional analysis of the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) Florida State Ambulatory Surgery Database (SASD) for the years 2005 to 2012. The database contains all-payer, discharge-level records for all ambulatory procedures occurring in emergency departments, hospital-based surgical units, and freestanding ambulatory surgery centers statewide. Although participating health organizations control the release of specific data, the database represents 100% of the records processed by AHRQ. Data are confirmed to be valid, internally consistent, and consistent with norms, when feasible. An independent contractor reviews all database statistics to ensure compatibility for closely related data elements, such as diagnosis and procedure codes (35).
Whereas treatment trends were described using 2005-2012 data, patient and surgeon-level analyses were performed using data from 2010-2012 because they were the most recent data available that permitted consistently accurate assignation of patients to the surgeons who treated them. The database is publicly available and de-identified. As such, our study was exempt from human subject's regulation by the Institutional Review Board.
Cohort Selection
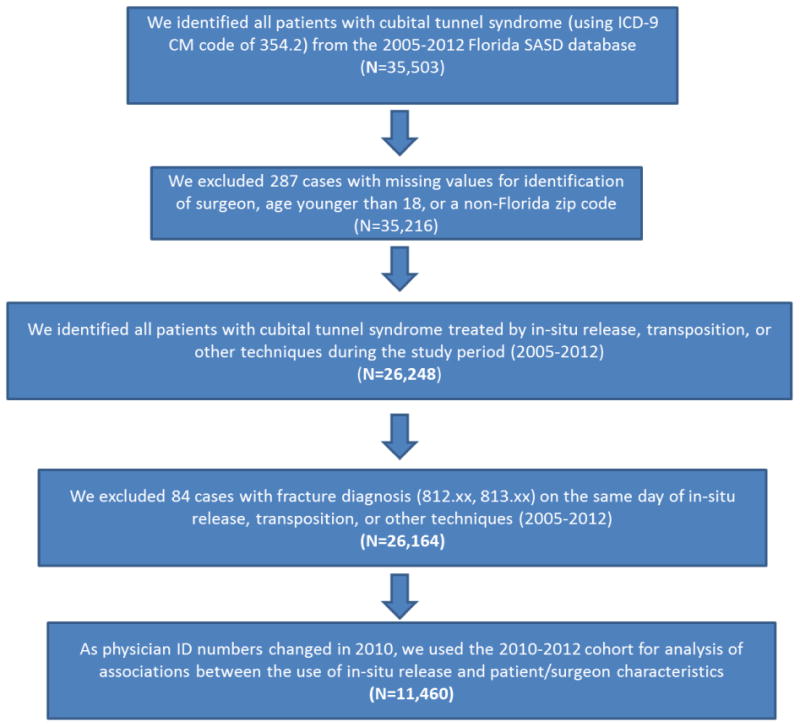
We included patients age 18 years and older who underwent surgical treatment for cubital tunnel syndrome and excluded patients with a non-Florida ZIP code, an unidentifiable treating surgeon, or a concomitant upper extremity fracture (ICD-9 codes 812.xx and 813.xx). We defined our study population using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9 CM) diagnostic code 354.2 (cubital tunnel syndrome). The current ICD coding system has different treatment codes for procedures used in the surgical treatment of compression of the ulnar nerve at the elbow. The codes 04.49 and 04.04 indicate simple decompression of the ulnar nerve at the elbow, code 04.60 indicates transposition of the ulnar nerve at the elbow, and code 04.79 indicates surgical treatment of cubital tunnel syndrome by other methods. These diagnosis and treatment codes were verified by 2 members of our research staff (JA, LZ). Patients without ICD-9 procedure codes were assumed to have not undergone surgery for cubital tunnel syndrome and were excluded from the analyses. Patients were assigned to one of 3 groups: in-situ release, transposition, and other treatment. Our final study cohort included 26,164 patients for the test of time trend of use for different procedures (2005-2012 cohort) and 11,460 patients (2010-2012 cohort) for the analysis of factors associated with procedure selection. The process of cohort creation is displayed in Figure 1.
Figure 1. The establishment of the study cohort.
Study Variables
Our primary outcome was the method of surgical treatment for cubital tunnel syndrome. Patient socio-demographic variables included age, sex, race (white, black, and other), household income, and location of patient residence. Household income was derived using patient ZIP code as a proxy and patient residence was sub-classified into large metropolitan, small metropolitan, micropolitan, and other as assigned by the HCUP SASD. Health-system-related variables, such as third-party payer (Medicare, Medicaid, Private, other) status were also included in the analysis. Surgeon factors included total volume and type of procedures used for treatment of cubital tunnel syndrome between 2010 and 2012.
Statistical Analysis
We used descriptive statistics to summarize trends in surgical management of cubital tunnel syndrome in the state of Florida from 2005 to 2012. We performed simple linear regressions using the rate of each type of procedure per year as the outcome and the calendar year as the key predictor. Using data from 2010 and 2012, we performed a univariate analysis to examine the association between patient/surgeon characteristics and the surgical technique. We then performed a hierarchical logistic regression analysis to examine the influence of patient characteristics on the choice of procedure for cubital tunnel syndrome with a binary dependent variable (in-situ release vs. transposition/other treatment). We assigned in-situ release as the reference group because it was the most commonly used technique. The selection of covariates (patient characteristics and surgeon volume/technique variety) in the multivariable model was based on results from the univariate analysis. To control for correlation among procedures performed by each surgeon, we included each surgeon as a random intercept of the model. Lastly, we calculated the intraclass correlation coefficient to ascertain the extent to which surgical treatment may be ascribed to clustering under a particular surgeon's care.
Results
Of the 2005-2012 study cohort (26,164 patients) who underwent surgery for cubital tunnel syndrome, 20,836 underwent in-situ decompression (79.7%), 4,247 underwent transposition (16.2%), and 1,081 underwent other surgical treatment (4.1%). Over the study period, there was a significant increase in the use of in-situ release and a decrease in the use of transposition techniques (Figure 2). For example, in 2005, the proportion of in-situ release among all techniques was 70%; this proportion increased by 26% over the study period. The proportion of transposition technique in 2005 was 27%; this proportion decreased 67% by 2012. On average, the proportion of in-situ release among other procedures increased 2.9% each year (95% CI [2.4%, 3.4%]) (p<0.001) and the proportion of transposition decreased 2.8% each year (95% CI [2.4%, 3.2%]) (p<0.001) (Table 1).
Figure 2. Trends in the use of each procedure type between 2005 and 2012.
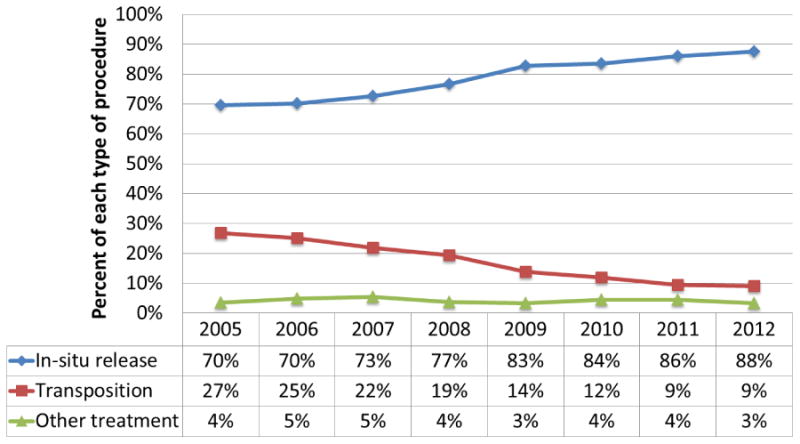
Table 1. Time trend of each type of cubital tunnel syndrome surgical treatment (2005-2012).
| Average change in percent each year¥ | P value | |
|---|---|---|
| In-situ release | 2.9 (2.4, 3.4) | <0.001 |
| Transposition | -2.8 (-2.4, -3.2) | <0.001 |
| Other treatment | -0.1 (-0.1, 0.3) | 0.52 |
The average change in the rate of each type of procedure was beta-coefficient calculated from a simple linear regression model.
Patient characteristics and procedure selection
For the 2010-2012 study cohort, socio-demographic and clinical characteristics of patients undergoing each procedure are presented in Table 2. No statistically significant association was found with regard to age, race, and median household income quartile on the selection of treatment techniques in univariate analysis. Women were slightly more likely than men to undergo in-situ release (p<0.001). Statistically significant differences were found with regard to patient locations and primary payers between the three procedure categories (Table 2).
Table 2. Characteristics of the patient cohort by types of surgical procedures (2010-2012).
| In-Situ Release | Transposition | Other treatment | |
|---|---|---|---|
| Patient cohort | |||
| No. of patients | 9833 (86%) | 1161 (10%) | 466 (4%) |
| Age | |||
| Younger than 44 | 1753 (18%) | 236 (20%) | 91 (20%) |
| 45 to 54 | 2445 (25%) | 254 (22%) | 115 (25%) |
| 55 to 65 | 2757 (28%) | 341 (29%) | 112 (24%) |
| Greater than 65 | 2878 (29%) | 330 (28%) | 148 (32%) |
| Sex* | |||
| Male | 4730 (48%) | 627 (54%) | 258 (55%) |
| Female | 5097 (52%) | 533 (46%) | 208 (45%) |
| Missing | 6 (0%) | 1 (0%) | 0 (0%) |
| Race | |||
| White | 7614 (77%) | 994 (86%) | 305 (65%) |
| Black | 843 (9%) | 83 (7%) | 39 (8%) |
| Other | 1228 (12%) | 74 (6%) | 119 (26%) |
| Missing | 148 (2%) | 10 (1%) | 3 (1%) |
| Patient location* | |||
| Large metro | 4957 (50%) | 488 (42%) | 264 (57%) |
| Small metro | 4043 (41%) | 568 (49%) | 182 (39%) |
| Micro | 482 (5%) | 71 (6%) | 15 (3%) |
| Other | 351 (4%) | 34 (3%) | 5 (1%) |
| Median household income | |||
| Quartile 1 | 2342 (24%) | 248 (21%) | 93 (20%) |
| Quartile 2 | 2341 (24%) | 337 (29%) | 105 (23%) |
| Quartile 3 | 2585 (26%) | 307 (26%) | 148 (32%) |
| Quartile 4 | 2362 (24%) | 248 (21%) | 110 (24%) |
| Missing | 203 (2%) | 21 (2%) | 10 (2%) |
| Primary Payer* | |||
| Medicare | 3497 (36%) | 459 (40%) | 171 (37%) |
| Medicaid | 416 (4%) | 67 (6%) | 10 (2%) |
| Private | 4722 (48%) | 504 (43%) | 212 (45%) |
| Other | 1198 (12%) | 131 (11%) | 73 (16%) |
Large metro, 1 million residents or more; small metro, less than 1 million residents; micro, adjacent to large or small metro; Other, not metro or micro
P value <0.001, from Pearson's Chi-square test of independent distribution
Surgeon characteristics and procedure selection
In univariate analysis, both surgeon characteristics (case volume and number of types of procedure performed) were significantly associated with the procedure selected for treatment of cubital tunnel syndrome. Of the 713 surgeons who performed cubital tunnel release between 2010 and 2012, 63% performed only one technique (Table 3). Most of the surgeons (95%) performed one or two procedure types.
Table 3. Characteristics of the surgeon cohort (2010-2012).
| Surgeon characteristics | No. of Surgeons |
|---|---|
| No. of procedure types performed* | |
| One type | 448(63%) |
| Two types | 228(32%) |
| Three types | 37(5%) |
| Case volume* | |
| Quartile 1 (1 case) | 171(24%) |
| Quartile 2 (2-4 cases) | 219(31%) |
| Quartile 3 (5-11 cases) | 146(20%) |
| Quartile 4 (11-572 cases) | 177(25%) |
Multivariable analysis of factors associated with in-situ release
In multivariable analysis, males were less likely to undergo in-situ release than female patients (OR=0.81, 95%CI [0.70, 0.93]) (p=0.004). In addition, patients with private insurance were less likely to undergo in-situ release than Medicare beneficiaries (OR=0.65, 95% CI [0.45, 0.93]) (p=0.02) (Table 4). Patient location was not associated with the use of in-situ release.
Table 4. Multivariable analysis of factors associated with the use of in-situ release for treatment of cubital tunnel syndrome (2010-2012).
| Patient and surgeon characteristics | Adjusted Odds Ratio ¥ | P value |
|---|---|---|
| Sex | ||
| Female | 1 | - |
| Male | 0.81 (0.70-0.93) | 0.004 |
| Patient location | ||
| Large metro | 1 | - |
| Small metro | 1.18 (0.69-2.01) | 0.55 |
| Micro | 1.06 (0.65-1.74) | 0.80 |
| Other | 1.12 (0.63-2.00) | 0.70 |
| Primary Payer | ||
| Medicare | 1 | - |
| Medicaid | 1.06 (0.90-1.24) | 0.50 |
| Private | 0.65 (0.45-0.93) | 0.02 |
| Other | 0.93 (0.74-1.18) | 0.55 |
| No. of procedure types performed by the surgeon between 2010 and 2012 | ||
| One type | 1 | |
| Two types | 0.13 (0.09-0.19) | <.0001 |
| Three types | 0.07 (0.04-0.14) | <.0001 |
| Surgeon case volume between 2010 and 2012† | ||
| Quartile 1 (1-21 case) | 1 | |
| Quartile 2 (22-61 cases) | 3.62 (2.25-5.82) | <.0001 |
| Quartile 3 (62-195 cases) | 20.83 (9.9-43.83) | <.0001 |
| Quartile 4 (195-572 cases) | 59.81 (16.37-218.56) | <.0001 |
Large metro, 1 million residents or more; small metro, less than 1 million residents; micro, adjacent to large or small metro; Other, not metro or micro
Adjusted odds ratios of undergoing in-situ release were calculated in hierarchical logistic models with a random effect of surgeons who treated the patient cohort, simultaneously adjusting for all patient factors.
Patients of surgeons in the highest category of case volume were substantially more likely to undergo in-situ release as compared to other techniques (OR=59.81, 95% CI [16.37, 218.56]) (p<0.001). Patients of surgeons who performed more than one type of procedure for cubital tunnel syndrome were less likely to undergo in-situ release (p<0.001) (Table 4). The intraclass correlation coefficient among surgeons in the sample was 0.67.
Discussion
In this cross-sectional study of recent patterns of treatment for cubital tunnel syndrome in the state of Florida, our results show that in-situ release is the most commonly used procedure, with a significant year over year increase in use over the study period. These findings are consistent with a study by Soltani et al. using the 1994, 1996, and 2006 National Survey of Ambulatory Surgery databases (5). They found that in-situ decompression replaced transposition as the technique most frequently performed for cubital tunnel syndrome in 2006. In their study, however, transposition techniques still comprised 38% of all surgical procedures used for treatment. We found that transposition encompassed only 16.2% of all procedures performed between 2005 and 2012. This discrepancy may be attributable to the more recent data collection period and our focus on only one state (Florida).
Of the variables assessed in this study, surgeon case volume was the factor most strongly associated with the use of a particular procedure. Specifically, we found that surgeons with the highest volume of cubital tunnel syndrome cases were significantly more likely to use in-situ release. One may surmise that surgeons with a high volume of cubital tunnel syndrome patients would be increasingly aware of the expanding role and established effectiveness of in-situ release. Further, a high intraclass correlation coefficient was found among encounters for the same surgeon. This indicates that the procedure a patient undergoes is highly dependent upon the treating surgeon. This finding was also noted in another Florida HCUP study evaluating patterns of treatment for thumb carpometacarpal arthritis (32). In both studies, effect sizes for surgeon-level characteristics greatly outweighed those for patient-level characteristics.
We also found that men were significantly less likely to undergo in-situ release as compared to transposition or other techniques. Richardson et al. (36) proposed that men may develop greater pressures over the ulnar nerve with hand usage as compared to females. This finding may partially explain the higher rates of transposition in men because greater pressure over the nerve is presumed to cause more profound neuropathy (37), thus theoretically providing the impetus to proceed with transposition or epicondylectomy.
Our study has several limitations due to the data source and the retrospective nature of the study. The quality of administrative datasets cannot be thoroughly confirmed and missing data remains an issue. For example, 24% of all patients in the Florida SASD database with a cubital tunnel syndrome diagnosis had no assigned ICD-9 procedure code. Although this cohort likely did not undergo surgical intervention for cubital tunnel syndrome, it is theoretically possible that the procedure code was not abstracted into the database. Importantly, secondary analysis found no clinically relevant differences in socio-demographics between this subgroup and patients with an ICD-9 procedure code. Further, no other surgeon-related variables, such as age, primary specialty, fellowship training, or years in practice, were available with the Florida SASD database. Because we are using data from only one state, our results may not be representative of treatment throughout the United States. Previous studies have shown geographical variation in the treatment of various hand conditions (38-40) and this may also be true of treatment of cubital tunnel syndrome. However, the trends we found regarding the increasing use of in-situ release are similar to those shown in other population-level studies on the treatment of cubital tunnel syndrome (5).
Because the Florida SASD surgeon identification number assignation changed between 2009 and 2010, we could only longitudinally track treatment choices by individual surgeon from either 2005 to 2009 or 2010 to 2012; we selected 2010 to 2012 because they were the most recent data. This narrow timeframe limited our ability to longitudinally analyze substantial changes in physician practice. Lastly, it is possible that some patients may have undergone revision ulnar nerve surgery with a different technique, which may account for some of the variation seen in treatment choices. Our data was cross-sectional with no longitudinal patient tracking and there is no diagnosis code for recurrent cubital tunnel syndrome to categorize this subset of patients. However, assuming a low rate of revision surgery, <7% as demonstrated by Goldfarb et al. (41) and the dominance of surgeon factors (ICC of 0.67), including revision surgery as another independent variable would not significantly change our study findings.
Contemporary healthcare mandates require increasing justification for resources. As a result, hand surgeons must support surgical decision-making with the best available evidence. Although much has been written about the established difficulty of influencing surgical practice with best-practice guidelines (42, 43), our analysis reveals the widespread adoption of in-situ release for treatment of cubital tunnel syndrome in Florida and these numbers are increasing. As with most procedures, however, patient demographics and surgeon-level factors influence procedure selection.
Acknowledgments
This project was supported by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
References
- 1.Palmer BA, Hughes TB. Cubital tunnel syndrome. J Hand Surg Am. 2010;35(1):153–163. doi: 10.1016/j.jhsa.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Waugh RP, Zlotolow DA. In situ decompression of the ulnar nerve at the cubital tunnel. Hand Clin. 2007;23(3):319–327. doi: 10.1016/j.hcl.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Mondelli M, Giannini F, Ballerini M, et al. Incidence of ulnar neuropathy at the elbow in the province of Siena (Italy) J Neurol Sci. 2005;234(1-2):5–10. doi: 10.1016/j.jns.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Zlowodzki M, Chan S, Bhandari M, et al. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007;89(12):2591–2598. doi: 10.2106/JBJS.G.00183. [DOI] [PubMed] [Google Scholar]
- 5.Soltani AM, Best MJ, Francis CS, et al. Trends in the surgical treatment of cubital tunnel syndrome: an analysis of the national survey of ambulatory surgery database. J Hand Surg Am. 2013;38(8):1551–1556. doi: 10.1016/j.jhsa.2013.04.044. [DOI] [PubMed] [Google Scholar]
- 6.Arle JE, Zager EL. Surgical treatment of common entrapment neuropathies in the upper limbs. Muscle Nerve. 2000;23(8):1160–1174. doi: 10.1002/1097-4598(200008)23:8<1160::aid-mus2>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 7.Mackinnon SE, Novak CB. Compression Neuropathies. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green's Operative Hand Surgery. 6. New York: Churchill-Livingstone; 2010. pp. 1392–1437. [Google Scholar]
- 8.Keiner D, Gaab MR, Schroeder HW, et al. Comparison of the long-term results of anterior transposition of the ulnar nerve or simple decompression in the treatment of cubital tunnel syndrome--a prospective study. Acta Neurochir (Wien) 2009;151(4):311–315. doi: 10.1007/s00701-009-0218-4. [DOI] [PubMed] [Google Scholar]
- 9.Blair WF. Upper extremity ulnar compressive neuropathy: surgical technique and return to work status. Tech Hand Up Extrem Surg. 1997;1(2):132–138. doi: 10.1097/00130911-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Song JW, Waljee JF, Burns PB, et al. An outcome study for ulnar neuropathy at the elbow: a multicenter study by the surgery for ulnar nerve (SUN) study group. Neurosurgery. 2013;72(6):971–981. doi: 10.1227/NEU.0b013e31828ca327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Juratli SM, Nayan M, Fulton-Kehoe D, et al. A population-based study of ulnar neuropathy at the elbow in Washington State workers' compensation. Am J Ind Med. 2010;53(12):1242–1251. doi: 10.1002/ajim.20866. [DOI] [PubMed] [Google Scholar]
- 12.Bartels RH, Menovsky T, Van Overbeeke JJ, et al. Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg. 1998;89(5):722–727. doi: 10.3171/jns.1998.89.5.0722. [DOI] [PubMed] [Google Scholar]
- 13.Heithoff SJ. Cubital tunnel syndrome does not require transposition of the ulnar nerve. J Hand Surg Am. 1999;24(5):898–805. doi: 10.1053/jhsu.1999.0898. [DOI] [PubMed] [Google Scholar]
- 14.Novak CB, Mackinnon SE. Selection of operative procedures for cubital tunnel syndrome. Hand (N Y) 2009;4(1):50–54. doi: 10.1007/s11552-008-9133-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henry M. Modified intramuscular transposition of the ulnar nerve. J Hand Surg Am. 2006;31(9):1535–1542. doi: 10.1016/j.jhsa.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 16.Catalano LW, 3rd, Barron OA. Anterior subcutaneous transposition of the ulnar nerve. Hand Clin. 2007;23(3):339–344. doi: 10.1016/j.hcl.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Bartels RH, Termeer EH, van der Wilt GJ, et al. Simple decompression or anterior subcutaneous transposition for ulnar neuropathy at the elbow: a cost-minimization analysis--Part 2. Neurosurgery. 2005;56(3):531–536. doi: 10.1227/01.NEU.0000154132.40212.6E. [DOI] [PubMed] [Google Scholar]
- 18.Bartels RH, Verhagen WI, van der Wilt GJ, et al. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: part 1. Neurosurgery. 2005;56(2):522–530. doi: 10.1227/01.neu.0000154131.01167.03. [DOI] [PubMed] [Google Scholar]
- 19.Gervasio O, Gambardella G, Zaccone C, et al. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56(1):108–117. doi: 10.1227/01.neu.0000145854.38234.81. [DOI] [PubMed] [Google Scholar]
- 20.Adkinson JM, Chung KC. Minimal-incision in-situ ulnar nerve decompression at the elbow. Hand Clin. 2014;30(1):63–70. doi: 10.1016/j.hcl.2013.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nabhan A, Ahlhelm F, Kelm J, et al. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 2005;30(5):521–524. doi: 10.1016/j.jhsb.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Foster RJ, Edshage S. Factors related to the outcome of surgically managed compressive ulnar neuropathy at the elbow level. J Hand Surg Am. 1981;6(2):181–192. doi: 10.1016/s0363-5023(81)80173-6. [DOI] [PubMed] [Google Scholar]
- 23.Biggs M, Curtis JA. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery. 2006;58(2):296–304. doi: 10.1227/01.NEU.0000194847.04143.A1. [DOI] [PubMed] [Google Scholar]
- 24.Caliandro P, La Torre G, Padua R, et al. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2011(7):CD006839. doi: 10.1002/14651858.CD006839.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Macadam SA, Gandhi R, Bezuhly M, et al. Simple decompression versus anterior subcutaneous and submuscular transposition of the ulnar nerve for cubital tunnel syndrome: a meta-analysis. J Hand Surg Am. 2008;33(8):1314, e1–12. doi: 10.1016/j.jhsa.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Ruchelsman DE, Lee SK, Posner MA. Failed surgery for ulnar nerve compression at the elbow. Hand Clin. 2007;23(3):359–371. doi: 10.1016/j.hcl.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Posner MA. Compression ulnar neuropathies at the elbow: II. treatment. J Am Acad Orthop Surg. 1998;6(5):289–297. doi: 10.5435/00124635-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Burns PB, Kim HM, Gaston RG, et al. Predictors of functional outcomes after simple decompression for ulnar neuropathy at the elbow: a multicenter study by the SUN study group. Arch Phys Med Rehabil. 2014;95(4):680–685. doi: 10.1016/j.apmr.2013.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Malay S, SUN Study Group. Chung KC. The minimal clinically important difference after simple decompression for ulnar neuropathy at the elbow. J Hand Surg Am. 2013;38(4):652–659. doi: 10.1016/j.jhsa.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giladi AM, Gaston RG, Haase SC, et al. Trend of recovery after simple decompression for treatment of ulnar neuropathy at the elbow. Plast Reconstr Surg. 2013;131(4):563e–573e. doi: 10.1097/PRS.0b013e318282764f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hageman MG, Guitton TG, Ring D, Science of Variation Group How surgeons make decisions when the evidence is inconclusive. J Hand Surg Am. 2013;38(6):1202–1208. doi: 10.1016/j.jhsa.2013.02.032. [DOI] [PubMed] [Google Scholar]
- 32.Aliu O, Davis MM, DeMonner S, et al. The influence of evidence in the surgical treatment of thumb basilar joint arthritis. Plast Reconstr Surg. 2013;131(4):816–828. doi: 10.1097/PRS.0b013e3182818d08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kitto S, Petrovic A, Gruen RL, et al. Evidence-based medicine training and implementation in surgery: The role of surgical cultures. J Eval Clin Pract. 2011;17(4):819–826. doi: 10.1111/j.1365-2753.2010.01526.x. [DOI] [PubMed] [Google Scholar]
- 34.Chung KC. Treatment of ulnar nerve compression at the elbow. J Hand Surg Am. 2008;33(9):1625–1627. doi: 10.1016/j.jhsa.2008.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: Apr, 2015. [April 10, 2015]. http://www.ahrq.gov/research/data/hcup/index.html. [PubMed] [Google Scholar]
- 36.Birkmeyer JD, Reames BN, McCulloch P, et al. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121–1129. doi: 10.1016/S0140-6736(13)61215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richardson JK, Green DF, Jamieson SC, et al. Gender, body mass and age as risk factors for ulnar mononeuropathy at the elbow. Muscle Nerve. 2001;24(4):551–554. doi: 10.1002/mus.1039. [DOI] [PubMed] [Google Scholar]
- 38.Szabo RM, Kwak C. Natural history and conservative management of cubital tunnel syndrome. Hand Clin. 2007;23(3):311–318. doi: 10.1016/j.hcl.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 39.Matlock DD, Groeneveld PW, Sidney S, et al. Geographic variation in cardiovascular procedure use among Medicare fee-for-service vs Medicare Advantage beneficiaries. JAMA. 2013;310(2):155–162. doi: 10.1001/jama.2013.7837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meakins JL. Evidence-based surgery. Surg Clin North Am. 2006 Feb;86(1):1–16. vii. doi: 10.1016/j.suc.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 41.Howes N, Chagla L, Thorpe M, et al. Surgical practice is evidence-based. Br J Surg. 1997;84(9):1220–1223. [PubMed] [Google Scholar]
- 42.Grilli R, Lomas J. Evaluating the message: The relationship between compliance rate and the subject of a practice guideline. Med Care. 1994;32:202–213. doi: 10.1097/00005650-199403000-00002. [DOI] [PubMed] [Google Scholar]
- 43.Kingston R, Barry M, Tierney S, et al. Treatment of surgical patients is evidence-based. Eur J Surg. 2001;167(5):324–330. doi: 10.1080/110241501750215168. [DOI] [PubMed] [Google Scholar]


