Abstract
To help maximize the real‐world applicability of available interventions in clinical and community healthcare practice, there has been greater emphasis over the past two decades on engaging local communities in health‐related research. While there have been numerous successful community–academic partnered collaborations, there continues to be a need to articulate the common barriers experienced during the evolution of these partnerships, and to provide a roadmap for best practices that engage healthcare providers, patients, families, caregivers, community leaders, healthcare systems, public agencies and academic medical centers. To this end, this paper presents a summary of a forum discussion from the 2014 Southern California Dissemination, Implementation and Improvement (DII) Science Symposium, sponsored by the University of California Los Angeles (UCLA) Clinical Translational Science Institute (CTSI), University of Southern California (USC) CTSI, and Kaiser Permanente. During this forum, a diverse group of individuals representing multiple constituencies identified four key barriers to success in community‐partnered participatory research (CPPR) and discussed consensus recommendations to enhance the development, implementation, and dissemination of community health‐related research. In addition, this group identified several ways in which the over 60 NIH funded Clinical and Translational Science Institutes across the country could engage communities and researchers to advance DII science.
Keywords: community‐partnered participatory research, community‐based participatory research, community engagement, translational research, implementation science
Introduction
Despite significant investments in research to assess healthcare service delivery and community health programs, little is known about how best to ensure that lessons learned from positive and negative health‐related research experiences are internalized to enhance the quality of health for individuals, families and communities. The need for more effective strategies to improve health outcomes has led to a greater increase in and resources for dissemination, implementation and improvement (DII) science to help optimize real‐world applicability of interventions used in clinical and community healthcare practice.1, 2, 3, 4 In addition, there has been more attention on the use of community‐academic partnered approaches that engage healthcare providers, patients, families, caregivers, community leaders, healthcare systems, public agencies and academic medical centers to further assist in creating a context of broader input and greater trust.
The integration of DII science and community‐partnered participatory research (CPPR) approaches would allow for the delivery of practical evidenced‐based interventions with, rather than on, key stakeholders, thereby increasing the likelihood of true uptake into everyday use. This is becoming more critical as the burden of healthcare is being driven by chronic diseases and social determinants of health, requiring solutions that extend beyond the walls of a health provider or even health systems. A CPPR approach to DII science would bring diverse and unique interdisciplinary insights and expertise at the outset of a project organized around common goals and collaborative work focused on enhancing patient outcomes.5 Therefore, this paper seeks to advocate for the use of CPPR practices in DII science, especially during the earlier phases of translational research; and to offer insight about barriers and possible solutions to CPPR success in a large, urban community.
Methods Used to Develop Recommendations for the Use of CPPR in DII Science
The work presented here was based on and guided by preliminary findings, community engagement efforts, and forum discussions presented at the 2014 Southern California DII Science Symposium, sponsored by the University of California Los Angeles (UCLA) Clinical Translational Science Institute (CTSI), University of Southern California (USC) CTSI, and Kaiser Permanente. The goal of the day‐long symposium was to accelerate the quantity and quality of DII Science programs and activities by (a) sharing knowledge and information regarding current DII Science‐related activity in the greater Los Angeles area, and (b) fostering networking opportunities and collaboration between experienced researchers, academics who are new to the field and community partners, to increase their participation in the CTSI DII initiative's mission, goals, strategies and operational plans.6 A diverse group of 129 participants included senior and junior researchers, research fellows, leaders of local healthcare delivery systems and public health agencies, and research partners in community‐based organizations in Los Angeles. Keynote speakers representing funding agencies, public and private delivery systems and medical associations delivered addresses on the importance and opportunities for implementation and improvement science research. Participants discussed the challenges to designing and executing implementation and improvement science research that meets the needs of stakeholders in health care, public health and in communities.
A faculty member and a fellow who were selected based on their expertise and experience in the discussion topic moderated breakout sessions during the symposium. Rather than achieving consensus, these group sessions sought to describe both barriers and potential solutions. More information on the background, mission and goals of the symposium and CTSI DII initiative can be found in overview article.6 The Engaging the Community in DII research breakout session had 17 attendees whose expertise was in the following disciplines: health policy and management, public health, quality improvement, internal medicine, occupational science and occupational therapy, behavioral health sciences, education, community advocacy, neurodevelopmental sciences, nephrology, dietetics, and population sciences.
Institutions and organizations represented among the breakout session attendees were academic and research institutions (University of California Los Angeles, Charles R. Drew University, City of Hope, University of Southern California), health systems (U.S. Department of Veteran Affairs, Kaiser Permanente, Los Angeles County Department of Health Services) community organizations (Healthy African American Families, California Family Health Council), community clinics (ChapCare Medical Health Center), and foundation(s) (Robert Wood Johnson Foundation). The breakout session followed a semistructured question and answer format where session moderators asked open‐ended questions and encouraged attendees to brainstorm barriers and solutions.
Community‐Partnered Participatory Research
Community engagement has been recommended as a strategy for academic medical centers to partner more substantively with local communities, to eliminate health disparities and to improve health outcomes.1, 7, 8, 9, 10 In particular, many efforts focus on primary and secondary prevention to address the growing burden of chronic disease.7, 8, 9, 11, 12 The Institute of Medicine (IOM), American Association of Medical Colleges, and the Association of Schools of Public Health have cited community engagement as a core competency in medical and public health education in order to develop a new generation of clinicians and public health leaders practicing community and patient‐centered approaches to improve health. In response, academic medical centers have implemented community‐engaged programs to enhance the public health impact of scientific research8, 13, 14 and to improve access to high‐quality healthcare and public health interventions, particularly in low‐income, under‐resourced, and/or minority communities.13, 15, 16
Community‐partnered participatory research (CPRR) “emphasizes equal partnership for community and academic partners”7 during the identification of the health‐related concern to be studied, design and implementation of the research study itself, and planning for the flow of information. CPPR approaches acknowledge that methods need to be developed to deal with conflicts as they arise, and to evaluate the progress and impact of the research at various stages in the project.1, 7 The level of planning and community commitment at the outset of the research project works to insure a higher rate of buy‐in and potential success.1, 17
Dissemination, Implementation, and Improvement Science
The gap between knowledge and practice is a major focus of health services research.18, 19, 20 Dissemination, implementation and improvement (DII) sciences are now essential tools used among health services researchers and those who are interested in identifying the reasons for this knowledge translation gap and addressing complex systems issues related to patient care.18, 19, 20, 21, 22 Dissemination science is the study of communication strategies that are designed to increase awareness and understanding of innovative, effective policies and practices to facilitate their widespread adoption.6, 23, 24, 25 Implementation science is the systematic study of planned and active approaches to increase the uptake of effective practices.6, 23, 26, 27 Improvement science uses iterative quasi‐experimental and experimental learning methods to change processes and systems to achieve better outcomes with reliability at scale in healthcare and public health systems and services.6, 19, 28, 29, 30 The framework and methods used in each of these three sciences are not unrelated or mutually exclusive even though their focus might be different.
Barriers and Potential Solutions to Community Engagement in Health‐Related Research
During the Engaging the Community in DII research breakout session, four barriers to success in the utilization of CPPR approaches in the Los Angeles area emerged. Each barrier, detailed below, is followed by consensus recommendations based on group opinions, first‐hand knowledge, and research from the literature on CPPR and DII Science.
Barrier 1: Historically, communities of interest have had little influence over the “problems” to be studied in health‐related research
Health‐related research geared at assessing and addressing community‐based problems requires that researchers have an adequate understanding of the community needs. Despite multiple types of surveying efforts and needs assessment strategies, researchers seldom allow communities to define the problems they want solved. Notably, DII researchers’ traditional behavior tends to focus on the bench to bedside method to improve health, whereby research related to health interventions is developed in isolation of community input during the T1 and T2 phases, with the expectation that findings will be translated into community settings during the T3 and T4 phases. However, this approach to community‐based participatory research implies that researchers alone are the experts. Researchers often interact with communities by telling them what to do, rather than listening and learning what the community has to offer at the outset of a project. During this kind of academic driven “shared” interaction, the community is less likely to authentically engage in the process and thus, less prone to adopt or promote any recommendations that are the result of interactions that were never truly “shared” in the first place.
In addition to a paucity of true collaborations, researchers also need to do a better job of asking if their research procedures will be a burden to the community agency of interest, especially if data will be collected in new or unfamiliar way. Rather than requiring that research data collection methods occur in a specific way at the outset, researchers can begin by first asking, “What data is already being collected? What would this community and/or community agency(ies) like to know more about its data? Are there ways that data collection can be improved so that it is more relevant to this particular community and/or community agency(ies)?”
Potential Solution: Adopt a clear, consistent framework of CPPR that engages the community in all phases of the research pipeline
Figure 1 illustrates an adaptation of the translational steps in the research pipeline from humans to patients to practice based on Westfall.31 We advocate, whenever possible, the use of CPPR practices in all phases of the translational science pipeline to foster the future incorporation of research discoveries into day‐to‐day clinical practice. This model can inform bench and bedside research orientations, provide partnered answers to potential translational barriers, and ensure that research findings will disseminate and effectively translate into sustainable and generalizable clinical practice changes to better the health of communities. Using Jones and Wells7 as a guide, there are multiple CPPR activities that can begin in the T1 phase of research as preparatory activities in support of dissemination of future health‐related research findings. Specifically, we advocate for the development of community–academic partnerships before specific research questions are developed, so that community needs can be explored prior to the development of preclinical trials. This seamless integration of community involvement from T1 through to T4 stages could significantly assist DII efforts.
Figure 1.
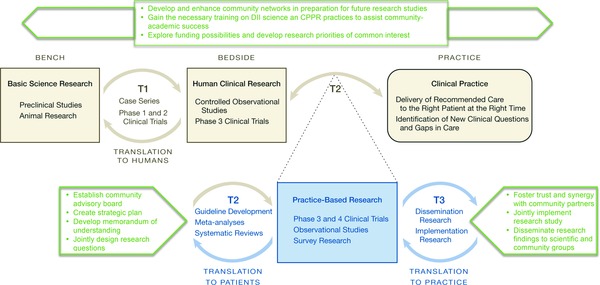
Incorporation of CPPR practices during all phases of the translational Science continuum. *Adapted from Westfall JM, Mold J, Fagnan L. Practice‐based research–“Blue Highways” on the NIH roadmap. JAMA. 2007; 294(4): 403–406.
Barrier 2: Often, during the development of research projects, key stakeholders are left out of the process
The Agency for Healthcare Research and Quality (AHRQ) defines stakeholders as “persons or groups who have a vested interest in a clinical decision and the evidence that supports that decision,” and further notes that “stakeholders may be patients, caregivers, clinicians, researchers, advocacy groups, professional societies, businesses, policymakers, or others. Each group has a unique and valuable perspective.”32 A core question often asked by community partners is “how do collaborators determine their partners?” Many within the community sector believe that the question does not get asked very well or very often during the development phases of community‐based intervention research projects and thus, key stakeholders who could make significant contributions are frequently omitted. Alternatively, while researchers may have the best of intentions to engage community stakeholders at the outset of a community‐based research intervention study, they may not have the necessary contacts or avenues to begin this dialogue, which is often specific to the research topic to be investigated (e.g., the need for community contacts vis‐a‐vis homelessness outreach). The DII forum in Los Angeles was an example of one such avenue, but formal gatherings, such as this, don't always exist, or may not be initiated on the same timetable as potential research studies to be initiated.
Unfamiliarity with the key stakeholders under study creates a continuous barrier between researchers and the community that can often lead to trust issues. Historic injustices during past academic research efforts have made many under‐resourced communities wary of so‐called “partnered” research efforts. In order to build the relationship and improve “community life,” community partners need to be confident that there are no stakeholders behind the scenes with hidden agendas.17
Potential Solution: Develop a transdisciplinary approach to solving community‐based “problems”
A transdisciplinary approach “aims to overcome the disconnection between knowledge production, on the one hand, and the demand for knowledge to contribute to the solution of societal problems, on the other hand. This is achieved through transdisciplinary approaches in which researchers from a wide range of disciplines work together with stakeholders.”33 A common question that should consistently be asked is “who is not at the table that should be.”34 A strategy that might assist with this includes the development (and maintenance) of a local/regional catalogue of key community contacts, ideally stratified by disease/sociological issue (e.g., HIV/AIDS, homelessness, substance use, autism, postincarceration community reengagement, etc.) so that at the conceptualization of a community‐based project, key stakeholders can be invited to participate. In addition, survivors of the health‐related concerns under study and caregivers assisting individuals living with both acute and chronic conditions have invaluable knowledge and insight into the life experiences of treating, curing, living with, and dying from the various health‐related problems impacting our society today.
Barrier 3: Cultural differences and health disparities often limit community engagement
A recent systematic review of barriers and facilitators to minority research participation among four racial/ethnic minority populations35 reveals several factors that limit their participation in health‐related research. One key barrier to minority participation centers on an overall lack of trust between minority communities and the researchers with whom they work.36, 37 Generally speaking, minority populations have the perception that any research in which they might participate will benefit Whites or the research institution, not the people of color.35 This mistrust is predicated on the fear of purposeful mistreatment and experimentation on the part of the researcher, a fear that is rooted in such historical facts as the Tuskegee study and the sterilization of Native American women;38 the more recent study on the genetics of aggressive behavior in exclusively African American children;38 and ongoing discriminatory healthcare experiences.38, 39
A second key barrier identified by the aforementioned systematic review centers around the idea of competing demands (inconvenience; cost of participation), which can limit participation of low resource communities. People in low socioeconomic communities often have limited money and time to commit to research projects that do not or cannot contribute to meeting their basic needs. Transportation is often challenging, and trying to get to another location to participate in a research study outside of everyday life activities can be daunting, especially without additional funds or support to get involved. In addition, the inability to take time off from work to participate in a research project offered at an inconvenient time (such as during traditional 9 to 5 work hours) makes it implausible for many individuals who are already struggling to meet everyday life commitments. It is critical that researchers know and truly understand the cultural and financial needs of individuals across the various racial, ethnic, and socioeconomic communities with which they interact. Finding effective solutions to assist communities in participating with research requires that researchers work together with community leaders to build trust and develop realistic, meaningful solutions.
Potential Solution: Acknowledge that health disparities and cultural differences exist, and put supports in place to minimize the effect of said differences
By working with communities at the outset of any research project to determine what potential barriers rooted in culture and socioeconomics may exist for a given project, plans can be generated in advance, in order to mitigate potential issues before they arise. For example, in addition to engagement of community partners throughout the research process, ethnically‐ and linguistically‐matched researchers and culturally‐appropriate educational materials and health messages may facilitate trust.40, 41 Offering jobsite or community‐based satellite research activities may also help to offset barriers to participation. It is imperative that researchers respect socioeconomic and cultural differences, not just with “lip‐service,” but also with thoughtful actions guided by the stakeholders of interest.5
Another solution is to work within the framework of community advisory boards37 or to consult and partner with community leaders and community‐based organizations to collaboratively design recruitment strategies and materials during research study development that are representative and consistent with the culture and values of the community.42 This is an important step as community members can help evaluate recruitment strategies and provide invaluable input to tailor those strategies in the planning stages of the study. Engaging community members ensures that recruitment materials, which constitute the first point of contact with the community of interest, demonstrate the level of inclusiveness of the community's needs and expectations in the study design process as well as the commitment of researchers to provide a partnered answer to health and social disparities experienced by community members.
Barrier 4: Dissemination of research findings seldom reach and/or are meaningful to the communities of study
A consistent complaint among community participants in academic research endeavors is that research findings are rarely meaningfully communicated back to those who participated, if communication about the findings occurs at all. In addition, participants often feel that the (eventual) cost of an intervention may be unreasonable for many in low socioeconomic communities. Thus, too many times, community participants feel that their time and efforts contribute to a research agenda that will not significantly or positively impact their own communities.
At the same time, researchers (or the academic partners) who participate in community‐based research must work diligently to keep‐up with academic expectations related to tenure and promotion, including the development of impactful publication records and the securing of research funding. Traditionally, the communication and dissemination needs of these two groups are so disparate and sometimes, even at odds. Researchers are likely to be chided by their peers for taking the time to develop jargon‐free dissemination materials for nonscientific audiences rather than focusing on developing manuscripts for scientific journals, and by their community partners who often perceive publishing in academic journals as irrelevant to their needs because the journals are difficult to access and/or understand for the lay community as they are written in an obscure, highly academically manner. Moreover, as noted above, the cost of many interventions is frequently too high for a large portion of underserved communities reinforcing the perception that the community is being used to generate findings for more affluent and/or nonminority communities.
Potential Solution: Commit to communicating research findings via multiple methods
It is essential that CPPR groups understand each other's needs, wants and priorities, and that they develop dissemination plans early on so that those involved in the project have a clear vision of the end product at the outset, and can contribute most advantageously to decisions regarding which information will be shared, at what time, and in a format that is relevant and of value to all partners and their constituents. A quick scan of the literature related to this topic yields a variety of successful ideas to communicate and disseminate research findings to satisfy both community and academic needs, such as:
Conduct community‐partnered research conferences43 using jargon‐free language at all phases of the project to educate researchers and the community about potential partnership opportunities, to kick off research activities, to educate community participants about research elements and scientific concepts, and finally, to disseminate findings in a user‐friendly way to assist with uptake.
Use traditional media outlets44 such as local cable television stations, online news forums, and mass circulation journals (Newsweek, Scientific American) to publicize research projects and their outcomes. Partnering with academic units based in communication sciences (journalism, or others) can provide for assistance in developing materials and enhance CPPR efforts.
Use a variety of social media outlets44 such as YouTube, Twitter, Facebook, Instagram, blogs, etc. to communicate findings in a community centered way. Develop a CPPR website or YouTube channel expressly devoted to disseminating research progress and findings along the way.
Develop community specific dissemination plans, such as write‐ups in church bulletins, fans printed with research information for use at churches and other community events, community agency newsletters, town hall meetings, radio and other formats.45, 46
To improve the accessibility of the interventions under study, the partnership should develop a plan early on to make sure there is adequate access of the intervention to the communities participating in the study and that the interventions are relevant. This may necessitate a commitment to vouchers or other strategies to constrain or mitigate the costs of potentially successful interventions for local community members and possibly those more broadly who might benefit from the intervention if such barriers are removed.
Conclusions and Consensus Recommendations for Clinical and Translational Science Programs
Through this community forum, we identified several tangible ways in which the over 60 NIH funded Clinical and Translational Science Institutes/Centers (CTSIs) across the country could engage communities and researchers to advance Dissemination, Implementation and Improvement (DII) science. These are summarized as follows:
Support ongoing forums to bring together communities and researchers for training in CPPR methods and capacity building to enhance the CPPR expertise of DII researchers across diverse communities within the United States.
Provide resources and/or join forces to sustain the efforts of existing, small CPPR working groups. Resources can take the form of consultation and technical assistance services to provide expertise in DII study design, study conduct and publication, and to increase the success of funding proposal responses to DII‐related funding announcements (e.g., NIH, the Patient‐Centered Outcomes Research Institute [PCORI], Center for Medicare and Medicaid Services [CMS], foundations, etc.).
Provide resources and training to the CPPR community on various research methodologies of clinical translational science. Often, in CPPR, it is not always best practice to engage in traditional blinded, randomized, clinical trial methodologies when advancing health care. Many quality improvement methods arise from thoughtful analysis of existing clinical and research databases and the use of practical trials that cover a range of study designs including “pragmatic” and “adaptive” trial designs that are more specific for advancing care rather than testing causal research hypotheses.47
Host an annual CPPR focused get‐together where community partners can present the everyday challenges that they would like help studying, so that the research community can say, “Here's what I have to offer”; and then brokerage can occur. The CTSIs can be integral in facilitating these relationships as they often already have community and academic partnerships in‐place to assist in initiating the dialog. The priorities need to center around the integration of the public agenda, the community agenda, and the science agenda, and the CTSIs are uniquely positioned to facilitate this effort.
Develop a CTSI specific funding mechanism to support the time needed for both academicians and community leaders to cultivate the necessary relationships to develop relevant CPPR projects.
Develop and maintain an easily accessible online directory of individuals across all academic units involved in CPPR, organized by area of expertise rather than discipline. This directory could support the interdisciplinary collaborations needed to build CPPR projects designed to meet society's complex health needs.
In conclusion, the implementation of the solutions and strategies described here, in addition to other related strategies, will advance CPPR and enhance DII science as an effective approach to help optimize the inculcation of evidence into clinical and community healthcare practice.
Conflict of Interest
The manuscript authors declare that they have no conflict of interests, financial or other to declare.
Previous Presentations
The work is based on preliminary findings, stakeholder engagement efforts, and forum discussions presented at the 2014 Southern California Regional Dissemination, Implementation and Improvement Science Symposium sponsored, in part, by the National Institutes of Health/National Center for Advancing Translational Sciences through UCLA CTSI Grant Number UL1TR000124, the Southern California CTSI Grant Number UL1TR000130, and Kaiser Permanente Southern California.
Acknowledgments
The research described was supported, in part, by the National Institutes of Health/National Center for Advancing Translational Sciences through UCLA CTSI Grant Number UL1TR000124, the Southern California CTSI Grant Number UL1TR000130, and Kaiser Permanente Southern California. Work on the manuscript was also supported by the National Institutes of Health/National Center for Research Resources/National Center for Advancing Translational Sciences Grant Number KL2TR000131 (SB); and National Institutes of Health Grant Numbers 2P20MD000182 (KN), 3P30AG021684 (KN). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Community Engagement Workgroup: Lenore Arab, Araceli Espinoza, Eddy Palacios, and Shari Randolph
References
- 1. Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community‐based research: assessing partnership approaches to improve public health. Ann Rev Pub Health. 1998; 19: 173–202. [DOI] [PubMed] [Google Scholar]
- 2. Petersen R, Hunkins JA, Riegel LD, Smith L. Forging new partnerships to build healthier communities for a healthier state. North Carol Med J. 2012; 73(4): 270–273. [PubMed] [Google Scholar]
- 3. Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, Sirett E, Wong G, Cargo M, Herbert CP, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q. 2012; 90(2): 311–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wallerstein NB, Duran B. Using community‐based participatory research to address health disparities. Health Promo Pract. 2006; 7(3): 312–323. [DOI] [PubMed] [Google Scholar]
- 5. Woolf SH, Purnell JQ, Simon SM, Zimmerman EB, Camberos GJ, Haley A, Fields RP. Translating evidence into population health improvement: strategies and barriers. Ann Rev Publ Health. 2015; 36: 463–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Inkelas M, Brown AF, Vassar SD, Sankaré IC, Martinez AB, Kubicek K, Kuo T, Mahajan A, Gould M, Mittman BS. Accelerating dissemination implementation and improvement science in CTSAs through regional partnerships. Clin Transl Sci. 2015; In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jones L, Wells K. Strategies for academic and clinician engagement in community‐participatory partnered research. JAMA. 2007; 297(4): 407–410. [DOI] [PubMed] [Google Scholar]
- 8. Institute of Medicine . The CTSA Program at NIH: Opportunities for Advancing Clinical and Translational Research. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 9. Gelmon SB, Seifer SD, Kauper‐Brown J, Mikkelsen M. Building Capacity for Community Engagement: Institutional Self‐Assessment. Seattle, WA: Community‐Campus Partnerships for Health; 2005. [Google Scholar]
- 10. Aguilar‐Gaxiola S, Ahmed S, Franco Z, Kissack A, Gabriel D, Hurd T, Ziegahn L, Bates NJ, Calhoun K, Carter‐Edwards L, et al. Towards a unified taxonomy of health indicators: academic health centers and communities working together to improve population health. Acad Med. 2014; 89(4): 564–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ackermann RT. Bridging the why and the how of clinical‐community integration. Am J Prev Med. 2013; 45(4): 526–529. [DOI] [PubMed] [Google Scholar]
- 12. National Research Council . Living Well with Chronic Illness: A Call for Public Health Action. Washington, DC: The National Academies Press; 2012. [Google Scholar]
- 13. Hood NE, Brewer T, Jackson R, Wewers ME. Survey of community engagement in NIH‐funded research. Clin Transl Sci. 2010; 3(1): 19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fournier AM. Service learning in a homeless clinic. J Gen Inter Med. 1999; 14(4): 258–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Michener JL, Yaggy S, Lyn M, Warburton S, Champagne M, Black M, Cuffe M, Califf R, Gilliss C, Williams RS, et al. Improving the health of the community: Duke's experience with community engagement. Acad Med. 2008; 83(4): 408–413. [DOI] [PubMed] [Google Scholar]
- 16. Agency for Toxic Substances and Disease Registry . CTSA Community Engagement Key Function Committee Task Force on the Principals of Community Engagement (Second Edition). Atlanta, Georgia: Agency for Toxic Substances & Disease Registry; 2011. [Google Scholar]
- 17. Jones L, Wells K, Norris K, Meade B, Koegel P. The vision, valley, and victory of community engagement. Ethnic Dis. 2009; 19(4 Suppl 6): S6–3–7. [PMC free article] [PubMed] [Google Scholar]
- 18. Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Admin Pol Mental Health. 2009; 36(1): 24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marshall M, Pronovost P, Dixon‐Woods M. Promotion of improvement as a science. Lancet 2013; 381(9864): 419–421. [DOI] [PubMed] [Google Scholar]
- 20. Kuo T, Gase LN, Inkelas M. Dissemination, implementation and improvement science research in population health: opportunities for public health and CTSAs. Clin Transl Sci. 2015. Aug 3; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moen RD, Nolan TW, Provost LP. Quality Improvement through Planned Experimentation. 3rd edn New York, NY, USA: McGraw‐Hill; 1991. [Google Scholar]
- 22. Holzer J, Kass N. Community engagement strategies in the original and renewal applications for CTSA grant funding. Clin Transl Sci. 2014; 7(1): 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schillinger D. An Introduction to Effectiveness, Dissemination and Implementation Research. San Francisco, CA, USA: University of California San Francisco; 2010. [Google Scholar]
- 24. Rabin BA, Brownson RC, Haire‐Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. J Pub Health Manage Pract. 2008; 14(2): 117–123. [DOI] [PubMed] [Google Scholar]
- 25. Training Institute for Dissemination and Implementation Research in Health. http://conferences.thehillgroup.com/OBSSRinstitutes/TIDIRH2013. Accessed June 29, 2015.
- 26. Peters DH, Adam T, Alonge O, Agyepong IA, Tran N. Implementation research: what it is and how to do it. Br J Sports Med. 2014; 48: 731–736. [DOI] [PubMed] [Google Scholar]
- 27. Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004; 82(4): 581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Langley GJ, Nolan KM, Norman CL, Provost LP, Nolan TW. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. New York, NY: Wiley Desktop Editions; 2009. [Google Scholar]
- 29. Margolis P, Provost LP, Schoettker PJ, Britto MT. Quality improvement, clinical research, and quality improvement research–opportunities for integration. Pediatr Clin North Am. 2009; 56(4): 831–841. [DOI] [PubMed] [Google Scholar]
- 30. Perla RJ, Provost LP, Parry GJ. Seven propositions of the science of improvement: exploring foundations. Qual Manage Health Care. 2013; 22(3): 170–186. [DOI] [PubMed] [Google Scholar]
- 31. Westfall JM, Mold J, Fagnan L. Practice‐based research–“Blue Highways“ on the NIH roadmap. JAMA. 2007; 297(4): 403–406. [DOI] [PubMed] [Google Scholar]
- 32. Agency for Healthcare Research and Quality . The Effective Health Care Program Stakeholder Guide. 2014; http://www.ahrq.gov/research/findings/evidence‐based‐reports/stakeholderguide/chapter3.html. Accessed December 15, 2014.
- 33. Hirsch Hadorn G, Hoffman‐Riem H, Biber‐Klemm S, Grossenbacher‐Mansuy W, Joye D, Pohl C, Wiesmann U, Zemp E. Handbook of Transdisciplinary Research. Bern, Switzerland: 2007. [Google Scholar]
- 34. Bluthenthal RN, Jones L, Fackler‐Lowrie N, Ellison M, Booker T, Jones F, McDaniel S, Moini M, Williams KR, Klap R, et al. Witness for wellness: preliminary findings from a community‐academic participatory research mental health initiative. Ethnic Dis. 2006; 16(1 Suppl 1): S18–S34. [PubMed] [Google Scholar]
- 35. George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Pub Health. 2014; 104(2): e16–e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Pub Health. 2007; 97(7): 1283–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Corbie‐Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Inter Med. 2002; 162(21): 2458–2463. [DOI] [PubMed] [Google Scholar]
- 38. Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underser. 2010; 21(3): 879–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Jacobs EA, Mendenhall E, McAlearney AS, Rolle I, Whitaker EE, Warnecke R, Ferrans CE. An exploratory study of how trust in health care institutions varies across African American, Hispanic and white populations. Commun Med. 2011; 8(1): 89–98. [DOI] [PubMed] [Google Scholar]
- 40. Shattell MM, Hamilton D, Starr SS, Jenkins CJ, Hinderliter NA. Mental health service needs of a Latino population: a community‐based participatory research project. Issu Mental Health Nurs. 2008; 29(4): 351–370. [DOI] [PubMed] [Google Scholar]
- 41. Carroll JK, Yancey AK, Spring B, Figueroa‐Moseley C, Mohr DC, Mustian KM, Sprod LK, Purnell JQ, Fiscella K. What are successful recruitment and retention strategies for underserved populations? Examining physical activity interventions in primary care and community settings. Transl Behav Med. 2011; 1(2): 234–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. De las Nueces D, Hacker K, DiGirolamo A, Hicks LS. A systematic review of community‐based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Serv Res. 2012; 47(3 Pt 2): 1363–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Khodyakov D, Pulido E, Ramos A, Dixon E. Community‐partnered research conference model: the experience of community partners in care study. Progr Comm Health Partnersh. 2014; 8(1): 83–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ammerman A, Harris JR, Brownson RC, Tovar‐Aguilar JA, Committee PRCS. CDC's Prevention Research Centers Program: translating research into action with communities. J Prim Prev. 2011; 32(3–4): 131–134. [DOI] [PubMed] [Google Scholar]
- 45. Jones L, Lu MC, Lucas‐Wright A, Dillon‐Brown N, Broussard M, Wright K, Maidenberg M, Norris K, Ferré C. One hundred intentional acts of kindness toward a pregnant woman: building reproductive social capital in Los Angeles. Ethnic Dis. 2010; 20(1 Suppl 2): S2–36–40. [PMC free article] [PubMed] [Google Scholar]
- 46. Sankaré IC, Bross R, Brown AF, Del Pino HE, Jones LF, Morris DM, Porter C, Lucas‐Wright A, Vargas R, Forge N, et al. Strategies to build trust and recruit African American and Latino community residents for health research: a cohort study. Clin Trans Sci. 2015. Jun 21; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Schwartz D, Lellouch J. Explanatory and pragmatic attitudes in therapeutical trials. J Chron Dis. 1967; 20(8): 637–648. [DOI] [PubMed] [Google Scholar]


