Abstract
Generalized anxiety disorder (GAD) is a chronic and disabling disorder which is characterized by worrisome mentation about future outcomes. Because the evocative stimuli in GAD are largely internally derived, the feared outcomes contained in worry episodes can be invoked – and responded to – regardless of external context. We hypothesized that individuals with GAD would be entrained to internally-regulated, fixed patterns of anxiety on a day-to-day basis and that successful therapeutic intervention would serve to mitigate this entrainment. Thus, the present study examined the constructs of flexibility and rigidity as they apply to the daily fluctuation of anxious symptoms in individuals with GAD. We aimed to demonstrate that an apparently variable system can be conceptualized as rigid when the variability maps onto stable and predictable periodic oscillations. Sixty-nine individuals completed cognitive-behavioral treatment for GAD. Average age was 36.62 years (SD = 11.56), and participants were mostly Caucasian (89.5%) and female (68.4%). Daily-diary data indicating level of anxiety on a 0 to 100-point scale and collected four times per day were subjected to spectral analysis in order to determine the spectral power attributable to daily oscillations – which was related to the degree of rigidity in daily anxiety. Diurnal rigidity decreased throughout therapy and the degree to which rigidity was reduced significantly predicted reliable change at post-treatment. Thus, symptom rigidity can be conceptualized as stable periodic fluctuation and is discernible from other metrics of volatility in repeated measures data. Moreover, diurnal rigidity is significantly reduced during treatment, facilitating flexible responding to environmental demands.
Keywords: generalized anxiety disorder, rigidity, flexibility, instability, variability, dynamics
Flexibility, rigidity, and stability are popular constructs that have been employed across various psychological research domains, including psychotherapy (Newman & Fisher, 2013), psychophysiology (Fisher & Woodward, 2014; Hoehn-Saric, McLeod, Funderburk, & Kowalski, 2004), personality (Wright, Pincus, & Lenzenweger, 2012), and emotion regulation (Gruber, Kogan, Quoidbach, & Mauss, 2013). Yet, inconsistencies remain in the operationalization and quantitation of these constructs, and it is not always clear where the distinctions lie between instability and flexibility, or stability and rigidity. However they are quantified, these constructs are inherently dynamic, going beyond between-subjects differences in level to focus on within-subject regulatory processes (Fisher, 2015). Flexibility, stability, and rigidity relate to the behavior of systems – cognitive, emotional, and so forth – where these systems need not be dynamical in the formal sense (Vallacher & Nowak, 2002), but are related nevertheless to the organization and coherence of phenomena over time. Here, dynamic systems theory provides a valuable heuristic for considering stability and variability within psychopathology and psychotherapy.
Dynamic systems theory is a transdisciplinary theory concerned with the behavior of complex systems over time. Central to this theory is the concept of self-organization, the organization of patterns of relatedness between system components as they vary in time (Ashby, 1962). A system that is self-organized is predictable: a sufficient understanding of the structure of the system – the quantitative relationships between the variables from one moment to another – allows one to predict subsequent behavior of the system (Ashby, 1947b). Human systems become self-organized in response to internal and environmental demands (Ashby, 1947a). For instance, an individual may experience random fluctuations in bodily arousal. By chance, these fluctuations may periodically crest during periods of social interaction. If the individual attributes the (otherwise random) bodily arousal to the social environment, a positive feedback loop may occur, strengthening the previously random co-occurrence into a coherent and predictable system of apprehension and arousal.
Thus, cognition, affect, and behavior can become organized into patterns of relatedness that are discernible from moment-to-moment and predictive of subsequent cognition, affect, and behavior. Within these systems an inherent tension exists between stability and variability – between promoting continuity in patterns of relatedness and allowing variation. Stability allows the system to maintain coherence and structure, but may leave the system rigid and inadaptable if too deeply entrenched. Conversely, variability facilitates flexible responding to environmental demands, but may threaten systemic integrity. In the present study, we aim to demonstrate that systems that are variable (and potentially interpretable as either unstable or flexible) can nevertheless be quite rigid and inflexible. Here we examine the variability in daily anxiety in individuals with generalized anxiety disorder (GAD) before and during the course of psychotherapy. By utilizing spectral analysis (described below) we aim to demonstrate that patterns of anxious symptoms can be rigid in their adherence to stable, periodic fluctuations (i.e. oscillations), and that psychotherapy can lessen the presence and rigidity of these patterns over time.
Rigidity as stable periodic fluctuation
One way that the amount of rigidity in daily symptoms can be quantified is by assessing the degree to which the observed variability in symptom level adheres to fixed, periodic waveforms. Symptoms that vary habitually from day to day – that is, rising and falling at regular intervals – will form a sinusoidal pattern over time. Spectral analysis is a method for identifying the presence and influence of such periodic patterns in time series data. Moreover, spectral analysis assesses the contribution a given pattern makes to the overall variation in the data – this is known as spectral power (see Results for additional details). Users of linear regression may liken spectral power to the R2 statistic, which reflects the proportion of variance in a dependent variable accounted for by a given model. Spectral analysis assesses how closely-fixed data are to each wave form – in the same way that an ordinary least squares regression tests how closely data points fall to a best-fit line. The more closely the data points adhere to a given wave form, the more power in that frequency of variation1.
Consistent with prior research in this domain (Fisher, Newman, & Molenaar, 2011), we were interested in the spectral power located at daily frequencies of once-per-day and higher – that is, daily and intra-daily variation. Greater power in this range indicates that the observed data points are falling very close to waveforms with daily or intra-daily frequency. Of paramount importance: whereas these data are varying relatively rapidly, they are exhibiting variability that is (roughly) uniform day in and day out, making the patterns rigid and highly predictable. Conversely, when the power is reduced in this frequency range, this indicates that the data are adhering less and less strictly to these daily and intra-daily waveforms (the data points fit less well to these daily oscillations and thus are less rigidly patterned day-to-day).
Spectral analysis thus provides a potentially unique angle on clinical phenomena, one that may help clarify the roles of symptom variation and persistence in psychiatric disorders. Specific to GAD, the current Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (DSM-5; American Psychiatric Association, 2013) requires “excessive anxiety and worry…occurring more days than not,” that the “individual finds…difficult to control” (p. 222). Researchers and clinicians interested in better-understanding the excessiveness, consistency, or controllability of worry and anxiety in GAD may employ an intensive repeated measure paradigm for observing in situ variation in daily anxiety. One might reasonably hypothesize that chronic, excessive, and uncontrollable anxiety would be reflected in measurements that are elevated and largely invariant; and that rising and falling patterns reflect an irregular and/or controllable symptom profile. Certainly, a simple comparison of average level over time would point to the former profile as more severe than the latter. However, as we argue below, if these rising and falling levels of anxiety are stable and predictable, periodic variability may in fact reflect a rigid and chronic symptom presentation. To this end, evaluating the shape (i.e. frequency), strength (i.e. amplitude), and predictability of these patterns may hold the key to distinguishing between periodic rigidity and random fluctuation.
Rigidity, flexibility, and instability
The examination of rigidity versus flexibility in psychopathology is not novel to the present study. Several authors have proposed rigidity in physiological systems as an underlying vulnerability marker for psychopathology, as well as a mechanism by which psychopathology exerts deleterious effects on physiologic health (c.f. Friedman, 2007). Additionally, a recent body of literature has begun to assess the role of variability in affective systems as an important quantification of psychopathology (Ebner-Priemer, Eid, Kleindienst, Stabenow, & Trull, 2009; Gruber et al., 2013; Thompson et al., 2012). Of note, the affective literature has emphasized the terms stability and instability in place of rigidity and flexibility. Although these terms are largely synonymous, they invert the valence of association. That is, whereas flexibility is couched as an optimal alternative to rigidity, its synonymous counterpart – instability – is seen as a pathological absence of stability. Should fluctuations in anxious symptomatology be stable or flexible? Is anxious psychopathology marked by increased rigidity or instability? We argue below that the metrics employed for examining these questions and the conditions under which they are applied are instrumental in drawing accurate conclusions. Moreover, the sampling rate of the measurements and the temporal scale of the data analysis will come to bear on the conclusions (c.f. Fisher & Woodward, 2014).
The mean square successive difference (MSSD; Von Neumann, Kent, Bellinson, & Hart, 1941) has been used to quantify instability in both physiological and emotional systems. The MSSD statistic has been touted as an optimal procedure for estimating instability in time series of behavioral data, as it reflects the level of variability in the data while also accounting for temporal order and the degree of temporal dependency (Ebner-Priemer et al., 2009). In a recent review of competing stability methods, Jahng, Wood, and Trull (2008) recommended mean square difference methodologies over within-person variance or spectral analysis for assessing affective instability. Yet, while these authors conducted a direct empirical comparison of mean square and variance methods, spectral analysis was not empirically examined. In eschewing spectral analysis the authors argued that the methodology is problematic because, “an appropriate theoretical base of sinusoidal cyclicity…is required to successfully apply spectral analysis” (Jahng et al., 2008; pg. 373). However, we argue here that cyclical assumptions associated with daily fluctuations of anxious symptoms are both appropriate and directly testable. Moreover, Jahng and colleagues did not consider that under cyclical conditions, a mean square difference approach might incorrectly indicate instability.
Broadly, instability refers to a condition under which a given observation is weakly related to a preceding or successive observation in time. The MSSD reflects putative volatility from observation to observation in a time series – successive values are substantially higher or lower than preceding values. However, as we argue here, sinusoidal patterns are highly coherent and stable and they are composed of values that are – by definition – rising and falling from observation to observation. Thus, although it has recently been argued that mean square difference methods are optimal for testing instability in psychological systems (Ebner-Priemer et al., 2009; Jahng et al., 2008), these statistics may incorrectly reflect instability in the presence of a sinusoidal pattern of variation.
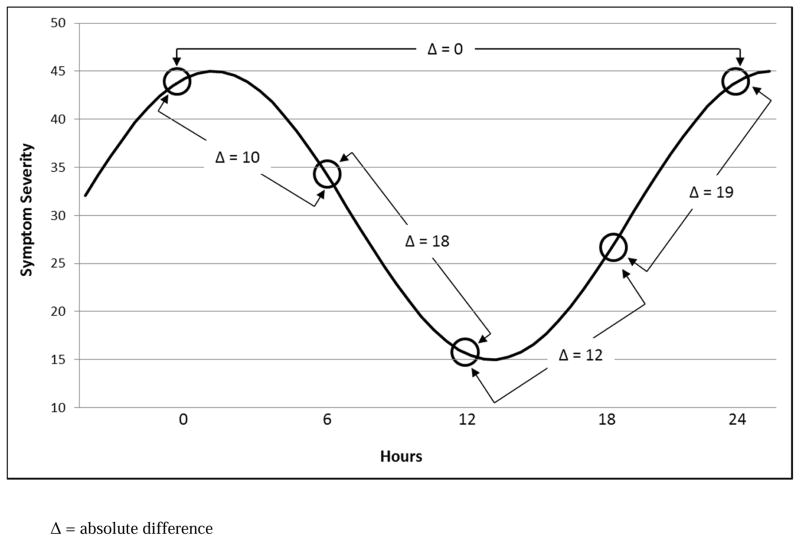
In Figure 1, we have provided a daily sinusoid with five successive observations in time and their respective absolute differences in value. If the successive differences are assessed in these data (lag = 1), the findings will reflect an unstable process – as the data points are consistently rising and falling from observation to observation. Specifically, the average absolute difference from observation-to-observation in this example is 14.75 points on a 50-point scale. However, if the same underlying periodic pattern is measured only once a day, then the average absolute difference between observations will reflect a stable process, as the sinusoidal pattern crosses roughly the same value at the same point in each day. Additionally, if data are collected four times per day but are only analyzed at a temporal scale of once-per-day, then an equivalently “stable” result will follow. Consistent with this, the difference between the two points taken 24 hours apart in Figure 1 is zero.
Figure 1.
Demonstration of varying anxiety levels falling along a sinusoid and the corresponding absolute differences in symptom severity level at lags of 1 observation (lower Δ’s) and 4 observations (uppermost Δ).
Δ = absolute difference
Thus, in our efforts to establish the role of daily fluctuations in anxiety as a reflection of symptomatic rigidity, it is important to demonstrate that spectral power is not conflated with, confounded by, or simply a proxy for other forms of variation in the data; most notably those that ostensibly reflect instability. Moreover, we aim to demonstrate that special consideration must be given to data exhibiting periodic variation in order to avoid conflating rigidity and instability. To this end, in the current paper we examined the MSSD at two scales of temporal analysis, that of four-times-per-day and once-per-day. In addition, we assessed both the spectral power limited to daily to intra-daily frequencies (the high-frequency power) and the total power at all other frequencies along the power spectrum (the non-high-frequency power). Although within-person variance has been deemed a suboptimal index of stability and flexibility (c.f. Jahng et al., 2008), as we examine the role of rigidity in psychotherapy it is important to demonstrate that it is the reduction in daily periodic rigidity specifically, and not reductions in the overall variance more broadly, that is predictive of outcome in CBT for GAD.
To put this in clinical terms: the degree to which a varying data signal may reflect rigidity or instability may be difficult to detect with either the naked eye or traditional analytic methods. Vital clinical inferences – such as whether a given individual is reactive and emotionally labile or rigidly unresponsive to environmental contingencies – could have important implications for both diagnosis and treatment. We hypothesize that GAD is defined by the latter. Because this disorder is principally characterized by worrisome mentation about future outcomes, both the engagement with and representation of feared stimuli are largely internally derived. Unlike social anxiety disorder, where peaks and troughs of anxious experience are related to exposure to (and then avoidance of) social contact, the feared outcomes contained in worry episodes can be invoked – and responded to – regardless of external context. We therefore propose that individuals with GAD are entrained to internally-regulated, fixed patterns of anxiety on a day-today basis and that successful therapeutic intervention serves to mitigate this entrainment, facilitating flexible responding to environmental demands.
Aims and hypotheses
The present study is a secondary analysis of a treatment outcome study of CBT for GAD (Borkovec, Newman, Pincus, & Lytle, 2002). The aim of this study was to demonstrate that under conditions of sinusoidal cyclicity, the degree of stable periodic fluctuation in daily symptoms can be considered a reflection of diurnal rigidity. In addition, we sought to articulate the role of diurnal symptom rigidity in psychotherapy, assess changes in rigidity during therapy, determine the degree to which these changes predicted outcome, and examine the potentially confounding role of other measures of variation – specifically the MSSD and total variance. Moreover, in order to isolate the rigidity versus flexibility of daily anxiety as a process of therapeutic change, it was important for the present study to demonstrate that symptom rigidity and symptom severity were dissociable constructs – in order to rule out potentially tautological scenarios. Given our theoretical assumption that increased symptom rigidity is reflective of maladaptive and pathological systems, we predicted that anxiety rigidity would exhibit a moderate positive correlation with anxiety severity at baseline and across the therapy period.
We then assessed the rate of change in the rigidity of daily anxiety during a 14-week trial of CBT for GAD. We sought to demonstrate that it was the reduction of rigidity during therapy, and not individual differences irrespective of therapy, that predicted greater therapeutic change. Because prior work has examined only single measures of spectral power across the entire therapy period (Fisher et al., 2011), it remains an empirical question whether individuals would exhibit relatively fixed differences in symptom rigidity, or whether reductions in rigidity represent a process of therapeutic action. We hypothesized that greater reductions in daily spectral power would predict greater therapeutic change at post-treatment, as a reflection of reductions in diurnal rigidity. Finally, we hypothesized that this effect would not be confounded by or conflated with competing measures of variability such as the overall variance or MSSD.
Method
As noted above, the present study was a secondary analysis of Borkovec, Newman, Pincus, and Lytle (2002). These authors examined differences in therapeutic efficacy between CBT and its constituent components, cognitive therapy (CT) and behavior therapy (referred to as self-control desensitization; SCD). Borkovec et al., 2002 found no differences in psychotherapy outcome between these conditions. Thus, the present study collapsed across these groups2.
Participants
Four hundred and fifty-nine people responded to local newspaper advertisements or referrals from mental health practitioners. Of these, 320 were ruled out by phone screens for not meeting study inclusion criteria, 54 clients were ruled out via an initial structured interview, and 9 clients were ruled out during a second structured interview, leaving 76 participants with primary generalized anxiety disorder who entered treatment. However, 7 clients dropped out at early stages of treatment (4 in SCD, 2 in CT, and 1 in CBT), leaving 69 clients who completed treatment. Average age was 36.62 years (SD = 11.56), and average duration of GAD diagnosis was 12.28 years (SD = 11.87). Clients were mostly Caucasian (89.5%) and women (68.4%). Only 2 clients were taking psychotropic medications for anxiety; they agreed to maintain dosage and frequency during therapy. None of these characteristics were significantly different across treatment conditions. All participants consented to the study, and IRB approval was attained. Comorbidities in the sample were: agoraphobia, 2.6% (n = 2), posttraumatic stress disorder, 2.6% (n = 2), social phobia, 43.4% (n = 33), simple phobia, 11.8% (n = 9), dysthymia, 7.9% (n = 6), major depressive disorder (MDD), 10.5% (n = 8), any comorbid disorder, 60.5% (n = 46), and no comorbid disorders 39.5%, (n = 30).
Procedure
Selection and assessor outcome ratings
Admission criteria included consensus between the two diagnostic interviewers on: a principal diagnosis of GAD, no diagnosable panic disorder (as recommended by the funding agency’s review committee), a Clinician’s Severity Rating (CSR) for GAD of 4 (moderate) or more, absence of concurrent psychosocial therapy, no history of having received CBT methods in prior therapy, no medical contributions to the anxiety, no antidepressant medication, and absence of severe MDD, substance abuse, psychosis, and organic brain syndrome. All but two clients (97.1%) concurrently met both DSM-III-R and DSM-IV criteria for GAD.
Advanced clinical graduate students trained to reliability in diagnostic interviewing administered 30-min. phone screens as well as the Anxiety Disorders Interview Schedule–III–R (ADIS-R; Di Nardo & Barlow, 1988) to determine diagnostic suitability. Those not ruled out by phone screen were administered a modified version of the ADIS-R (Di Nardo & Barlow, 1988), which included the Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959), Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960a), CSRs for GAD and comorbid disorders, and additional questions corresponding to two GAD criteria being proposed at the time of study initiation by the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV; American Psychiatric Association, 1994) subcommittee for GAD (i.e., uncontrollable worrying, and three of six associated symptoms). A second ADIS-R was administered within two weeks by the therapist who would see the client in therapy to reduce the likelihood of false positive cases. Pre-treatment diagnoses, both primary and comorbid, were based on consensus between the independent structured interviewers. A random subsample of 20% of pre-treatment audiotapes of ADIS-R interviews conducted by the primary assessor (prior to developing consensus) was reviewed for reliability purposes. For the presence of GAD, kappa agreement was 1. Outcome measures were administered at pre and post-treatment. The client daily diary was completed 4x/day during the treatment period.
Outcome measures
Clinician’s Severity Rating
For each diagnosis, interviewers assigned a 0–8 rating of the degree of distress and interference in functioning associated with the disorder (0 = none to 8 = very severely disturbing/disabling). Clients who met criteria for any diagnosis were assigned a CSR of 4 (definitely disturbing/disabling) or higher. If key features of a disorder were present but were not extensive or severe enough to warrant a formal diagnosis (or for disorders in partial remission), a CSR of 1–3 was assigned. When no features of a disorder were present, CSRs of 0 were given. Diagnostic reliability of CSRs in the current study ranged from an intraclass correlation of .77 to 1, and Finn’s r for GAD which corrects for a restricted range of CSRs (Whitehurst, 1984) was .74.
State Trait Anxiety Inventory- Trait Version (STAI-T; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983)
This 20-item scale is used to measure trait anxiety. Internal consistency reliability is high (in the .80’s and .90’s; .86 in the current sample), and retest reliability is much higher for the trait form (high .70’s) than the state form (from .27 to .54). Convergent and discriminant validity has also been demonstrated for this questionnaire (Spielberger et al., 1983).
Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959)
This 14-item clinician administered scale provides a rating of severity of each overarching anxiety symptom cluster on a scale from 0 (not present) to 4 (very severe/incapacitating). Internal consistency was good in the present sample (α =.82). Retest reliability was ICC = .86 across 2 days and inter-rater reliability ranged from an ICC of .74 –.96 (Bruss, Gruenberg, Goldstein, & Barber, 1994).
Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990)
The PSWQ is a 16 item self-report measure of pathological worry. Factor analysis indicated that the PSWQ assesses a unidimensional construct with internal consistency of .91 (Meyer et al., 1990; .83 in the current sample). High retest reliability (ranging from .74–.93) was also demonstrated across periods ranging from 2–10 weeks (Molina & Borkovec, 1994). Correlations between the PSWQ and measures of anxiety, depression, and emotional control supported the convergent and discriminant validity of the measure (Brown, Antony, & Barlow, 1992).
Reliable change index
Similar to other treatment studies (Clark et al., 1999), we created a single continuous variable to represent GAD severity. A single composite is considered more valid than any one measure of symptoms. A composite not only provides a more valid measure of the construct of interest, but it also provides one means of reducing experiment-wise error rate, since it replaces four sets of analyses with a single, more powerful one (Horowitz, Inouye, & Siegelman, 1979). The four measures used for the composite were significantly correlated with one another (ranging from .62 to .84). Raw scores for the PSWQ, HARS, CSRs for GAD, and STAI-T were converted to standardized z-scores and averaged for each participant.
We also created a GAD-change measure by calculating the average reliable change index (RCI; Jacobson & Truax, 1991) across the four GAD outcome measures. RCI reflects the degree of change that occurred beyond the fluctuations of an imprecise measure (McGlinchey, Atkins, & Jacobson, 2002). RCI is favored over the use of categorical classifications because of its greater statistical power as a continuous variable (Steketee & Chambless, 1992). The following values were used in the RCI formulae in the present study: GAD CSR: SD = 0.91, reliability = .72; STAI-T: SD= 7.66, reliability = .84; PSWQ: SD = 8.09, reliability = .91; HARS: SD = 6.9, reliability = .80. Standard deviations represent the standard deviation of the pooled sample at pre-therapy assessment, and the reliability estimates represent reported retest reliability coefficients for each measure (Bruss et al., 1994; Meyer et al., 1990; Newman, Przeworski, Fisher, & Borkovec, 2010; Spielberger et al., 1983). Mean RCIs were calculated for change immediately after treatment relative to pre-therapy assessment.
Process Measures
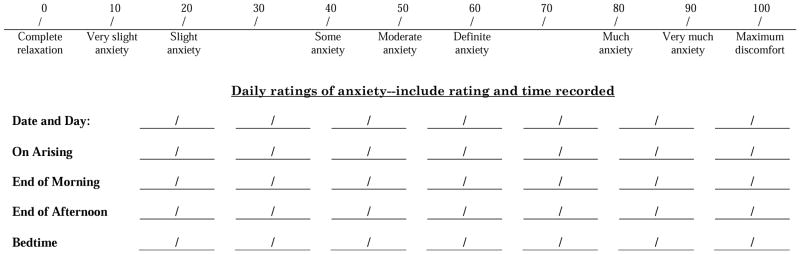
Client daily diary (CDD)
Patients recorded anxiety levels 4 times a day (upon arising, end of morning, end of afternoon, and end of evening) via a pencil and paper format, rating their overall level of anxiety during the preceding period of the day on a 0–100 scale. CDDs were completed for two weeks prior to the start of therapy (baseline), for 14 weeks of therapy, and for an additional two weeks post-treatment. Clients were asked to complete this measure daily for at least two weeks before treatment, and throughout the entire treatment period. Two-week retest reliability between the initial baseline and start of therapy was .80. One week’s worth of data was collected at a time and reviewed in-session between the therapist and client. Figure 2 presents an example of the client daily diary form completed by participants each week.
Figure 2.
Client daily diary.
Results
Spectral analysis of times series data
In spectral analysis a series of observations in time with length N can be decomposed into N/2 sinusoidal waveforms with cycle lengths N/1, N/2, N/3…down to N/[N/2] (Warner, 1998). Thus, for data measured 4/day for 14 days, the maximum identifiable frequency is .07/day (a two-week cycle) and the minimum frequency is 2/day (a twice-per-day cycle). Each frequency has a corresponding degree of power, and a power spectrum is produced that indicates the range of frequencies and their respective spectral power estimates. These power spectra reflect the contribution of each frequency to the overall variability. Specifically, the amount of power at a given frequency is the contribution of that frequency to the observed variability in the time series.
Classical approaches to the spectral analysis of times series assume an even spacing of observations in time. The present data were collected roughly 4, 4, 4, and 12 hours apart each day and thus, they do not meet this assumption. The present study employed the Lomb-Scargle periodogram (Lomb, 1976; Scargle, 1982), applied via the CTS package (Wang & Nash, 2012) in R (version 2.15.1). The Lomb-Scargle periodogram uses least-squares fitting to test the presence and influence of sinusoids in the data. This approach utilizes a vector of cumulative time to appropriately space unevenly sampled data. Additionally, it is capable of accommodating missing data, which can be seen as a variant of unequal spacing in the time series. We were interested in the power at frequencies of once-per-day and greater – i.e. daily to intra-daily oscillatory patterns – referred to as the high-frequency power because these represent the highest frequencies in the power spectrum. Such oscillations correspond to daily and intra-daily patterns of anxious symptomatology at the level of the individual. Greater power in this frequency range connotes the presence and influence of fluctuations in anxious symptoms with rigid daily to intra-daily periodic structure. We calculated the raw spectral power in the daily to intra-daily range (high-frequency power), as well as the power across all remaining frequencies (non-high-frequency power). For each individual, data were analyzed in eight successive two-week segments (baseline, weeks 1 and 2, weeks 3 and 4, and so forth), each containing 56 total observations. All power spectral estimates (high-frequency and non-high-frequency) were strongly right-skewed and were thus log-transformed in the analyses described below.
The mean square of successive differences
The MSSD statistic represents the average difference in absolute value between successive observations. Because positive and negative differences can cancel each other out, each difference value is squared. In the case of the MSSD statistic, these squared difference values are simply summed and averaged. However, this often results in a positively skewed distribution and takes the difference statistic out of the original scale of measurement. Thus, taking the square root of the squared differences can normalize the distribution of the differences and returns the output to the original scale of measurement. All references to the MSSD henceforth refer to the square root of the MSSD (sometimes referred to specifically as the RMSSD). We calculated the MSSD for successive observations with a lag of 1 observation and a lag of 4 observations. The single lag reflects the average absolute difference between each successive observation in the 4x/day data. Calculating the same statistic with a lag of 4 observations reflects the average absolute difference between observations that are a full 24-hours apart – and thus on a daily cycle (see Figure 1 for visual reference).
Missing data
Of the 69 participants, one had insufficient data for calculating spectral power across baseline – requisite for subsequent calculations of change in power – and four exhibited enough missing data to preclude calculation of spectral power in a given within-therapy period. These participants exhibited 211, 230, 244, 280, and 335 missing observations (44%, 48%, 51%, 59%, and 70% missingness respectively). These individuals were retained in linear mixed effect models, as full-information maximum likelihood estimation can accommodate missing cases. However, for ordinary least squares regression analyses, these participants were removed as a function of listwise deletion. Of the remaining 64 participants the average number of missing observations was 60.31 (12.6%), with a standard deviation of 47.69. However, the distribution of missingness was strongly right-skewed and thus, the median of 48 missing observations (10%) may better represent the central tendency of the data. The minimum number of missing observations was 0 (0%) and the maximum was 194 (41%).
Relationship between symptom rigidity and symptom severity
The Pearson’s product-moment correlation between high-frequency power in daily diary entries and the mean level of the daily diary entries was calculated for each of the eight sections of time series data (baseline, weeks 1 and 2, weeks 3 and 4, and so forth). Correlations, with accompanying t statistics, and p values are provided in Table 1. High-frequency power and anxiety severity were significantly positively correlated at the early and late stages of therapy, with the strongest correlations seen at baseline (r = .39) and end of therapy (r = .44). The average correlation across the therapy period was r = .28.
Table 1.
Correlations between symptom severity and symptom rigidity over pre-therapy baseline and complete psychotherapy period.
| Pearson’s r | t | p | |
|---|---|---|---|
| Baseline | .39 | 3.40 | .001 |
| Weeks 1 & 2 | .005 | .04 | .97 |
| Weeks 3 & 4 | .30 | 2.43 | .02 |
| Weeks 5 & 6 | .33 | 2.75 | .008 |
| Weeks 7 & 8 | .21 | 1.66 | .10 |
| Weeks 9 & 10 | .22 | 1.76 | .08 |
| Weeks 11 & 12 | .36 | 2.94 | .005 |
| Weeks 13 & 14 | .44 | 3.72 | < .001 |
Change in diurnal rigidity
Linear mixed-effect regression models were used to examine the change in high-frequency power as a proxy for diurnal rigidity during psychotherapy. The LME4 package in R (version 2.15.1) was used for all analyses. Table 2 presents the results of these models. We first examined the coefficient for change over time – referred to as Time – in isolation from other covariates. This analysis revealed a significant decrease in high-frequency power over the treatment period. We then entered the non-high-frequency power variable in the next iteration of the model. Here Time remained a significant predictor, but the effect size was reduced by half. Non-high-frequency power exhibited strong, positive covariation with high-frequency power. Finally, we added the MSSD variables of lag 1 and lag 4 – which reflect the instability from observation to observation and day to day, respectively. As expected, the MSSD lag 1 variable showed a strong positive correlation with high-frequency power and the MSSD lag 4 variable showed a strong negative correlation. That is, greater instability at the observation-to-observation level was associated with greater high-frequency spectral power, given the position of successive observations within a day along a daily sinusoid. However, greater instability of day-to-day measurements was associated with lesser high-frequency spectral power, as the latter reflects stability in the form of rigid periodic fluctuations in daily symptoms. Thus, the scale of temporal analysis was vital to determining whether high-frequency power indeed reflected rigidity or instability.
Table 2.
Linear mixed-effect regression for change in high-frequency power (daily rigidity) on time, non-high-frequency power (all remaining frequencies), MSSD with a lag of one observation, and MSSD with a lag of four observations.
| Estimate | SE | t value | p value | Cohen’s d | |
|---|---|---|---|---|---|
| Block 1 | |||||
| Time (Weeks) | −.085 | .011 | −7.89 | < .001 | −1.42 |
| Block 2 | |||||
| Time (Weeks) | −.021 | .005 | −4.05 | < .001 | −.73 |
| Non-HF Power | .764 | .021 | 36.03 | < .001 | 6.48 |
| Block 3 | |||||
| Time (Weeks) | −.001 | .004 | −.25 | .80 | .05 |
| Non-HF Power | .690 | .031 | 22.40 | < .001 | 4.03 |
| MSSD–Lag 1 | .104 | .006 | 18.11 | < .001 | 3.26 |
| MSSD–Lag 4 | −.056 | .007 | −8.03 | < .001 | −1.45 |
Non-HF Power = non-high-frequency power (spectral power summed across all frequencies lower than 1x/day); MSSD = the square root of the mean squared successive difference; Cohen’s d calculated via (Dunlap, Cortina, Vaslow, & Burke, 1996).
Of note, the Time coefficient was non-significant in the final iteration of the model, as the time-varying covariation with non-high-frequency power and MSSD variables accounted for the variance in the change over time in the high-frequency power.
Relationship between rigidity and specific symptom domains
Finally, regarding our predictive analyses of diurnal rigidity, we were interested in examining the covariance between rigidity and specific sub-domains of GAD-related psychopathology. We selected the PSWQ, which specifically isolates the severity of worry, the Hamilton Rating Scale for Anxiety, which includes somatic and fear-based symptoms of anxiety, and the Hamilton Rating Scale for Depression (Hamilton, 1960b). We regressed the log-transformed, baseline high-frequency power on the Hamilton rating scales for anxiety and depression and the PSWQ. Worry significantly predicted rigidity at baseline (β = 0.033, SE = 0.011, t = 2.93, p = .004), but anxiety (β = 0.011, SE = 0.017, t = 0.65, p = .52) and depression (β = 0.010, SE = 0.016, t = 0.62, p = .54) did not.
Having identified worry as a significant covariate of rigidity at baseline, we conducted a follow-up analysis to assess whether levels of worry at baseline moderated the change in rigidity over the treatment period. We again used a linear mixed-effect regression model (via the LME4 package in R) to predict the time-varying, log-transformed high-frequency power over the treatment period. The linear trend for time (in weeks) was significant (β = −0.378, SE = 0.048, t = 7.85, p < .001), as was the effect of baseline worry (β = 0.274, SE = 0.072, t = 3.81, p < .001); however, the interaction between time and worry was not significant (β = 0.023, SE = 0.048, t = 0.48, p = .63). Thus, baseline worry predicted level but not trend in high-frequency power during the psychotherapy period.
Predicting post-treatment reliable change
In order to assess the degree to which psychotherapy outcome was predicted by change in symptom rigidity, we conducted a linear regression in five successive, additive blocks. Due to the presence of outliers in the MSSD change statistics, a robust regression via M-estimation (Huber, 1964) was employed via the MASS package in R (version 2.15.1). In order to examine the relative contribution of the four variability measures, we regressed post-treatment RCI on the overall change in high-frequency power, non-high-frequency power, and MSSD at lags of 1 and 4 observations. The change in high-frequency power was a strong positive predictor of RCI at post-treatment, whereby larger reductions in high-frequency power predicted greater reliable change. Importantly, this effect was not mitigated by the addition of non-high-frequency power, MSSD–lag 1, or MSSD–lag 4 to the model. In fact, the relationship between change in high-frequency power and RCI appeared to be strengthened by the addition of these covariates. Finally, we added the composite measure of baseline anxiety severity to control for level of anxiety across participants, and then change in the Hamilton Rating Scale for Depression. Both anxiety severity and change in depression significantly predicted reliable change; however, change in high-frequency power remained a significant predictor of outcome. The (robust) zero-order correlations among the predictor variables and post-treatment reliable change are presented in Table 3 and the results of the regression analyses are provided in Table 4.
Table 3.
Robust zero-order correlations among study variables
| Δ HF Power | Δ Non-HF Power | Δ MSSD–1 | Δ MSSD–4 | Baseline Composite | Δ Dep. | |
|---|---|---|---|---|---|---|
| Δ Non-HF Power | .87 | |||||
| Δ MSSD–1 | .38 | .33 | ||||
| Δ MSSD–4 | .65 | .65 | .89 | |||
| Baseline Composite | .10 | −.02 | .17 | .17 | ||
| Δ Depression | .25 | .23 | .11 | .17 | .40 | |
| Reliable Change | .41 | .21 | .10 | .16 | .49 | .45 |
Δ HF Power = change in high-frequency power; Δ Non-HF Power = change in portion of power in power spectrum other than the high-frequency range; Δ MSSD–4 = change in the square root of mean successive differences at a lag of 4 observations (daily cycle). Baseline composite = average of Penn State worry questionnaire, Hamilton anxiety rating scale, state-trait anxiety inventory, and ADIS-IV assessor severity rating at baseline; Δ Depression = change in Hamilton rating scale for depression.
Table 4.
Multiple regression for reliable change at post-treatment on changes: in high-frequency power, non-high-frequency power, and MSSD–Lags 1 and 4.
| Coefficient | SE | t value | p value | Cohen’s d | |
|---|---|---|---|---|---|
| Block 1 | |||||
| Δ HF Power | .756 | .239 | 3.16 | .002 | .57 |
| Block 2 | |||||
| Δ HF Power | 1.515 | .465 | 3.26 | .002 | .59 |
| Δ Non-HF Power | −.879 | .456 | −1.93 | .06 | −.35 |
| Block 3 | |||||
| Δ HF Power | 1.751 | .502 | 3.49 | .001 | .63 |
| Δ Non-HF Power | −1.245 | .663 | −1.88 | .06 | −.34 |
| Δ MSSD–1 | −.058 | .066 | −.87 | .39 | −.16 |
| Δ MSSD–4 | .079 | .116 | .68 | .50 | .12 |
| Block 4 | |||||
| Δ HF Power | 1.176 | .438 | 2.68 | .009 | .49 |
| Δ Non-HF Power | −.339 | .595 | −.57 | .57 | −.10 |
| Δ MSSD–1 | −.007 | .057 | −.12 | .90 | −.02 |
| Δ MSSD–4 | −.042 | .102 | −.41 | .68 | −.07 |
| Baseline Composite | 1.827 | .375 | 4.87 | < .001 | .88 |
| Block 5 | |||||
| Δ HF Power | 1.140 | .468 | 2.44 | .02 | .44 |
| Δ Non-HF Power | −.479 | .635 | −.75 | .46 | −.14 |
| Δ MSSD–1 | −.008 | .061 | −.13 | .90 | −.02 |
| Δ MSSD–4 | −.027 | .109 | −.25 | .80 | −.05 |
| Baseline Composite | 1.333 | .431 | 3.10 | .003 | .56 |
| Δ Depression | .112 | .042 | 2.68 | .009 | .49 |
Δ HF Power = change in high-frequency power; Δ Non-HF Power = change in portion of power in power spectrum other than the high-frequency range; Δ MSSD–4 = change in the square root of mean successive differences at a lag of 4 observations (daily cycle). Baseline composite = average of Penn State worry questionnaire, Hamilton anxiety rating scale, state-trait anxiety inventory, and ADIS-IV assessor severity rating at baseline; Δ Depression = change in Hamilton rating scale for depression.
Cohen’s d calculated via (Dunlap et al., 1996).
Discussion
In the present study our primary objective was to demonstrate that diurnal rigidity could be modeled as the rigid adherence of repeated observations in daily anxiety to periodic fluctuations that, while variable, exhibited a fixed and predictable variation (i.e. sinusoidal cyclicity). In addition, we examined whether changes in rigidity during psychotherapy – as opposed to static individual differences – significantly predicted psychotherapy outcome at post-treatment. Finally, we sought to clarify the role of diurnal rigidity – as operationalized by the spectral power attributable to daily periodicities – relative to other forms of variability (such as the overall variance and the mean square difference).
Results indicated that rigidity was significantly positively correlated with concurrent levels of anxiety at baseline and at the end-of-therapy (rs = .39 and .44 respectively). The average correlation between periodic rigidity and anxiety severity across the therapy period was .28, reflecting a small to moderate degree of positive covariation. Nevertheless, these data indicate that symptom rigidity and symptom severity are dissociable constructs, and one should not be considered a proxy for the other. Examining the relationship between rigidity and symptom severity within particular sub-domains of GAD symptomatology, we found that worry severity, and neither depression nor somatic and fear-based anxiety predicted rigidity at baseline. Moreover, worry was a predictor of rigidity level across the therapy period, but did not moderate the change in rigidity. Regarding changes in rigidity over time, we found that high-frequency spectral power exhibited a large linear decrease across the therapy period. We also examined the covariation between high-frequency power and MSSD at lags of one and four observations. Mean square difference methods measure the instability in successive observations in a time series and have been recommended as an optimal measure of relative stability in psychological processes (Ebner-Priemer et al., 2009; Jahng et al., 2008). However, we hypothesized that the MSSD of successive observations would inaccurately reflect an unstable process due to the position of such observations along a sinusoidal pattern of variation (see Figure 1); whereas we hypothesized that the MSSD of observations 24 hours apart would reflect a stable (i.e. rigid) process. Our results bore this pattern out, as the MSSD–lag 1 variable exhibited a large positive correlation with high-frequency power and the MSSD–lag 4 variable exhibited a large negative correlation with high-frequency power over the therapy period.
Finally, we assessed the degree to which post-treatment RCI was predicted by changes in (a) high-frequency power, (b) non-high-frequency power, (c) MSSD–lag 1, and (d) MSSD–lag 4 during the therapy period in a hierarchical multiple regression. The degree of change in high-frequency power – that is, the degree to which anxious responding moved from rigid periodicity to more (ostensibly flexible) aperiodicity – significantly predicted reliable change in GAD symptomatology following treatment. Moreover, change in diurnal periodic rigidity remained a significant predictor of treatment outcome when controlling for concurrent changes in non-high-frequency power (i.e. the variance attributable to patterns at all remaining frequencies) and MSSD at lags of one observation and four observations. Finally, the change in high-frequency power remained a significant predictor of reliable change at post-treatment when controlling for baseline anxiety severity and change in depression symptoms during treatment.
It may seem paradoxical that variability could be utilized to reflect rigidity. A more intuitive conceptualization of rigidity may suggest a system that is static or unchanging. However, while we argue that rigidity can apply to patterns of variation – yielding rigid variations day-to-day – we also contrasted our conceptualization of rigidity against a more linear and perhaps intuitive measurement-to-measurement representation. The MSSD has received a great deal of recent attention as a measure of stability and instability in repeated measures data (Ebner-Priemer et al., 2009; Jahng et al., 2008). The size of the absolute differences between observations relates to the amplitude of variation from observation to observation, while providing a measure of the dispersion in the data that accounts for the temporal ordering of observations. However, as we have shown here, the MSSD can provide misleading results in the presence of periodic fluctuations in the data. Whereas the moment-to-moment (lag 1) measure of MSSD in the present study reflected an unstable process, the day-to-day (lag 4) measure of MSSD reflected a highly stable process; exhibiting a strong negative correlation with symptomatic rigidity in daily levels of anxiety. This is a potentially vital distinction for understanding the mechanics of daily anxiety in individuals with GAD; one which can affect the inferences we draw about the effect of CBT on pathological anxiety. To wit, if the variations in daily anxiety symptoms in the present study are interpreted as initially unstable and moving from instability to stability during treatment, then we might assume that GAD is characterized by a symptomatic lability that is stabilized during successful psychotherapy. However, if these variations are interpreted as rigid – and thus, highly stable – then we might conclude that individuals with GAD are potentially under-reactive to environmental stimuli and entrained to stable patterns of anxious responding.
Consistent with prior data (Fisher et al., 2011), the current findings present additional evidence for the latter hypothesis and imply that a potential process of therapeutic change in CBT for GAD is the reduction of rigidity in daily symptomatic experience. The Lomb-Scargle periodogram method employed in the present study uses least-squares fitting to test the presence and influence of periodic fluctuations in time series data. The high-frequency spectral power returned from this analysis reflects consistent and predictable fluctuations in daily symptoms that exhibit periodic constancy day-to-day. Under such circumstances, levels of anxiety are driven by rigidly fixed processes and are not free to covary with changing environmental demands moment-to-moment. However, reductions in the high-frequency power indicate that diary entries fit less well to fixed periodicities, perhaps reflecting increased flexibility in symptom responding.
We argue that the pattern of results in the present study indicate that GAD is marked by heightened rigidity in daily symptomatic experience, whereby individuals are entrained to relatively stable and fixed patterns of anxious responding. Over the course of treatment, it is possible that the rigidity of daily symptoms is reduced as clients are better able to flexibly respond to their environment. Alternatively, it is also possible that individuals with GAD are initially (i.e. typically) rigid in their daily schedules and that over treatment they are less rigidly adherent to pre-existing schedules and habits, thus becoming more varied in their daily experiences. Nevertheless, reductions in the high-frequency power in anxious symptoms reflects a corresponding reduction in symptom rigidity and predictability, and increases in flexibility – whether psychological, emotional, or behavioral.
We propose that, as an individual’s anxiety becomes less rigidly tied to daily periodic fluctuations, it is free to vary in response to environmental demands, which are inherently less periodic. Cognitive-behavioral therapy may facilitate increases in flexible responding by interrupting patterns of threat anticipation and worry that otherwise maintain anxious responding (unrelated to true threat in the environment). In the course of CBT for GAD, individuals practice self-monitoring skills to identify worry triggers, helping them to better understand the causal relationships between environmental stressors and anxious responses. Moreover, CBT helps to build mastery of anxious responding and perceptions of self-efficacy. Consistent with Woodworth’s S-O-R model, CBT for GAD may help clients to perceive that as an individual organism, they mediate the relationship between (external) stimuli and (anxious) responses (Woodworth, 1929). Thus, the logical relationship between environmental cues and cognitive-affective responses may begin to define the system – as opposed to habitual patterns.
Several limitations should be acknowledged. Perhaps most importantly, the current study employed randomized controlled trial data on CBT for GAD. Therefore, it is unknown whether these findings would generalize either to other diagnostic groups or treatment modalities. Specifically, CBT for GAD places a major emphasis on self-monitoring practices, wherein clients are specifically encouraged to observe and understand the connections between external and internal events – an intervention that may promote the observed shifts in rigidity. Thus, additional work remains to establish whether these effects will generalize to other therapeutic modalities. Additionally, although the client daily diaries were utilized within therapy as an important tool for tracking progress and providing feedback to clients, the diaries were completed by paper and pencil with no means to objectively verify the time of completion. Thus, some assumptions of periodicity may have been affected by non-compliant diary completion. Specifically, participants – possibly completing multiple entries at once – may have introduced periodicity into their diary data by unintentionally employing patterned responding across days. Future research utilizing electronic collection techniques with time-stamped data should seek to replicate these findings and assess the degree to which periodic rigidity can be identified with superior methodological control. However, we would offer that the consistency of the present findings across the sample – (a) that periodicity significantly related to severity, (b) that periodicity was reduced across the therapy period, and (c) that these reductions predicted the degree of reliable change in anxiety symptoms – makes faulty diary entries an unlikely source of systematic variance. It is more likely that inaccurate or fabricated diary data would have substantially undermined the present analyses. Nevertheless, further confirmation with additional samples, clinical diagnoses, and electronic methodologies are indicated.
Another potential weakness in the present study is the absence of comparison groups – either healthy controls or other diagnostic groups. Although our hypotheses about diurnal rigidity were specific to GAD phenomenology (i.e. internally-mediated patterns of anxiety related to worrisome mentation), it would nevertheless strengthen the conclusions of the present study to demonstrate divergent patterns between GAD and another disorder. For instance, we might hypothesize that the peaks and troughs of fearful experience in phobic disorder would be related to engagement with phobia-related stimuli, and not entrained to internal daily rhythms. Moreover, we might expect to see aperiodicity (i.e. noise) in the time series of healthy controls. However, at present, these remain empirical questions in need of further examination. Finally, the sample was predominantly White, and therefore our results may not generalize to more diverse samples. Future work should endeavor to apply the current methodology to diverse sets of psychological disorders, treatment modalities, and cultural groups in order to better identify whether the current findings represent universalities of psychotherapy process and outcome.
The present study provides compelling evidence that GAD is marked by heightened rigidity in symptom expression and that a potentially important process in CBT for GAD is the reduction of daily symptom rigidity. Additionally, we demonstrated that our conceptualization of rigidity – the high-frequency power in 4x/day levels of anxious symptoms – was not confounded by or conflated with other sources of variation in the data. Moreover, we propose that the contrast between the high-frequency spectral power and MSSD has important implications for future studies utilizing ecological momentary assessment data. Both the measurement frequency and the temporal scale of analysis should be taken into account when planning data collection and data analysis, and researchers should make efforts to inspect their data for periodic components. Although the physiological, psychological, and affective literatures have benefitted from recent attention to the nature of variability in time series data – assessing constructs such as stability, rigidity, inertia, and reactivity – great care should be taken in determining the quantitation of these terms and the conditions under which they are appropriately applied.
Highlights.
Stable periodic fluctuation can be considered a reflection of symptom rigidity.
Spectral analysis can be used to reflect the degree of diurnal rigidity in symptoms.
Rigidity as reflected by spectral power is not conflated with other measures of variability or volatility, such as the total variance or mean squared successive difference.
Symptom rigidity appears to be elevated in individuals with generalized anxiety disorder.
Symptom rigidity is reduced during the course of CBT for GAD, as the rigid adherence to internally-entrained patterns of anxiety are reduced, allowing flexible responding to environmental demands.
Footnotes
It should be noted that spectral power is a function of the frequency and the amplitude of the wave. Simply put, the larger the rise and fall of the waveform (the amplitude), the more variance the waveform carries – and, thus, the greater the spectral power. Related to this, all results reported below are consistent when utilizing either the normalized power or the raw spectral power. Readers are referred to Warner (1998) for a more detailed discussion.
We tested potential group differences in the distributions of all study variables. Individuals in the CT condition exhibited a small, significantly lesser degree of change in non-high-frequency power during therapy (t = 2.00, p = .05). However, further tests revealed no moderation effect of CT condition on RCI at post-treatment.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders: DSM 5. 2013 bookpointUS. [Google Scholar]
- Ashby WR. The Nervous System as Physical Machine: With Special Reference to the Origin of Adaptive Behavior. Mind. 1947a;56(221):44–59. doi: 10.1093/mind/lvi.221.44. [DOI] [PubMed] [Google Scholar]
- Ashby WR. Principles of the self-organizing dynamic system. The Journal of general psychology. 1947b;37(2):125–128. doi: 10.1080/00221309.1947.9918144. [DOI] [PubMed] [Google Scholar]
- Ashby WR. Principles of the self-organizing system. In: Von Foerster H, Zopf GW Jr, editors. Principles of Self-Organization: Transactions of the University of Illinois Symposium. London, UK: Pergamon Press; 1962. pp. 255–278. [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;61(4):611–619. doi: 10.1037/0022-006X.61.4.611. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70(2):288–298. doi: 10.1037/0022-006X.70.2.288. [DOI] [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy. 1992;30(1):33–37. doi: 10.1016/0005-7967(92)90093-V. [DOI] [PubMed] [Google Scholar]
- Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton Anxiety Rating Scale Interview Guide: Joint interview and test-retest methods for interrater reliability [Journal; Peer Reviewed Journal; Journal Article] Psychiatry Research. 1994;53(2):191–202. doi: 10.1016/0165-1781(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Ludgate J, Gelder M. Brief cognitive therapy for panic disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 1999;67(4):583–589. doi: 10.1037/0022-006X.67.4.583. [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Barlow DH. Anxiety Disorders Interview Schedule-Revised (ADIS-R) Albany: Center for Stress and Anxiety Disorders; 1988. [DOI] [PubMed] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1(2):170. [Google Scholar]
- Ebner-Priemer UW, Eid M, Kleindienst N, Stabenow S, Trull TJ. Analytic strategies for understanding affective (in)stability and other dynamic processes in psychopathology. Journal of Abnormal Psychology. 2009;118(1):195–202. doi: 10.1037/a0014868. [DOI] [PubMed] [Google Scholar]
- Fisher AJ. Toward a dynamic model of psychological assessment: Implications for personalized care. Journal of Consulting and Clinical Psychology. 2015;83(4):825–836. doi: 10.1037/ccp0000026. [DOI] [PubMed] [Google Scholar]
- Fisher AJ, Newman MG, Molenaar PCM. A quantitative method for the analysis of nomothetic relationships between idiographic structures: Dynamic patterns create attractor states for sustained posttreatment change. Journal of Consulting and Clinical Psychology. 2011;79(4):552–563. doi: 10.1037/a0024069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher AJ, Woodward SH. Cardiac stability at differing levels of temporal analysis in panic disorder, post-traumatic stress disorder, and healthy controls. Psychophysiology. 2014;51(1):80–87. doi: 10.1111/psyp.12148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman BH. An autonomic flexibility-neurovisceral integration model of anxiety and cardiac vagal tone. Biological Psychology. 2007;74(2):185–199. doi: 10.1016/j.biopsycho.2005.08.009. [DOI] [PubMed] [Google Scholar]
- Gruber J, Kogan A, Quoidbach J, Mauss IB. Happiness is best kept stable: Positive emotion variability is associated with poorer psychological health. Emotion. 2013;13(1):1–6. doi: 10.1037/a0030262. [DOI] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960a;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960b;23(1):56. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoehn-Saric R, McLeod DR, Funderburk F, Kowalski P. Somatic symptoms and physiologic responses in generalized anxiety disorder and panic disorder: an ambulatory monitor study. Archives of General Psychiatry. 2004;61(9):913–921. doi: 10.1001/archpsyc.61.9.913. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Inouye D, Siegelman EY. On averaging judges’ ratings to increase their correlation with an external criterion. Journal of Consulting and Clinical Psychology. 1979;47(3):453–458. doi: 10.1037/0022-006x.47.3.453. [DOI] [PubMed] [Google Scholar]
- Huber PJ. Robust estimation of a location parameter. The Annals of Mathematical Statistics. 1964;35(1):73–101. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jahng S, Wood PK, Trull TJ. Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychological Methods. 2008;13(4):354–375. doi: 10.1037/a0014173. [DOI] [PubMed] [Google Scholar]
- Lomb N. Least-squares frequency analysis of unequally spaced data. Astrophysics and space science. 1976;39(2):447–462. [Google Scholar]
- McGlinchey JB, Atkins DC, Jacobson NS. Clinical significance methods: Which one to use and how useful are they? Behavior Therapy. 2002;33(4):529–550. [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford, England: Wiley; 1994. pp. 265–283. [Google Scholar]
- Newman MG, Fisher AJ. Mediated moderation in combined cognitive behavioral therapy versus component treatments for generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 2013;81(3):405–414. doi: 10.1037/a0031690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Przeworski A, Fisher AJ, Borkovec TD. Diagnostic comorbidity in adults with generalized anxiety disorder: impact of comorbidity on psychotherapy outcome and impact of psychotherapy on comorbid diagnoses. Behavior Therapy. 2010;41(1):59–72. doi: 10.1016/j.beth.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scargle JD. Studies in astronomical time series analysis. II-Statistical aspects of spectral analysis of unevenly spaced data. The Astrophysical Journal. 1982;263:835–853. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory STAI (Form Y) Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- Steketee G, Chambless DL. Methodological issues in prediction of treatment outcome. Clinical Psychology Review. 1992;12(4):387–400. doi: 10.1016/0272-7358(92)90123-P. [DOI] [Google Scholar]
- Thompson RJ, Mata J, Jaeggi SM, Buschkuehl M, Jonides J, Gotlib IH. The everyday emotional experience of adults with major depressive disorder: Examining emotional instability, inertia, and reactivity. Journal of Abnormal Psychology. 2012;121(4):819–829. doi: 10.1037/a0027978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallacher RR, Nowak A. The dynamical perspective in personality and social psychology. The Dynamic Perspective in Personality and Social Psychology: A Special Issue of Personality and Social Psychology Review. 2002;6(4):264–273. [Google Scholar]
- Von Neumann J, Kent R, Bellinson H, Hart Bt. The mean square successive difference. The Annals of Mathematical Statistics. 1941;12(2):153–162. [Google Scholar]
- Wang Z, Nash J. Continuous Time Autoregressive Models (Version 1.0–12) 2012 http://CRAN.R-project.org/package=cts.
- Warner RM. Spectral analysis of time-series data. New York, NY: Guilford Press; 1998. [Google Scholar]
- Whitehurst GJ. Interrater agreement for journal manuscript reviews. American Psychologist. 1984;39(1):22. [Google Scholar]
- Woodworth RS. Psychology. Oxford, England: Holt; 1929. [Google Scholar]
- Wright AGC, Pincus AL, Lenzenweger MF. Interpersonal development, stability, and change in early adulthood. Journal of Personality. 2012;80(5):1339–1372. doi: 10.1111/j.1467-6494.2012.00761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]