Abstract
Objective
The aim was to determine whether pregnant women conceiving through in vitro fertilization (IVF) differ from those conceiving spontaneously in terms of psychological well-being and the quality of life.
Methods
In a prospective study we included 75 women conceived after IVF and 78 who conceived spontaneously in the same time period (control group). All the women were sent a self-report questionnaire about demographic and reproductive history, health, pregnancy concerns, containing Subjective Quality of Life Scale (QLS), Positive and Negative Affect Schedule (PANAS), the Psychological Well-Being Scale (PWB), Beck Depression Inventory (BDI), and Zung Self-Assessment Anxiety Scale (SAS); obstetric and newborn’s data were obtained from medical records. Response rate was 66.6% in the IVF and 83.3% in control group.
Results
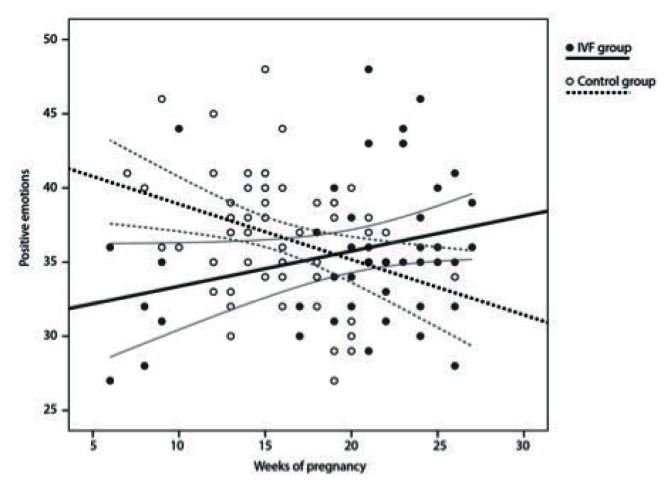
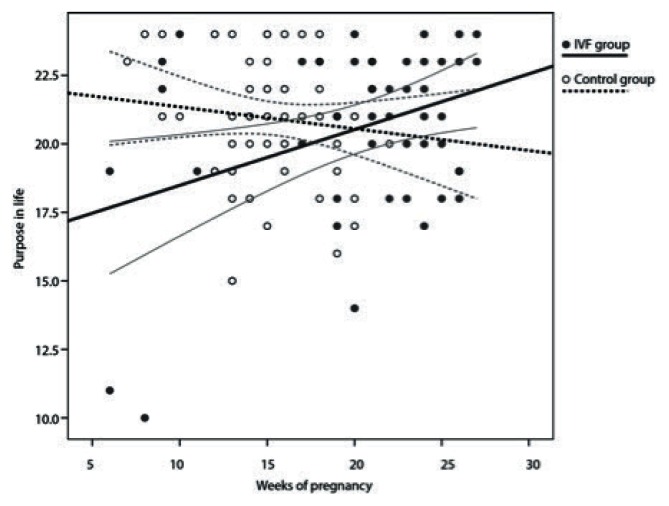
The mean women’s age was 33.8 years in the IVF, and 32.5 years in the control group (NS). There were no significant differences between groups on the most of the outcome measures assessing psychological status. IVF mothers were just less satisfied in “friend/acquaintances” (P=0.03), a higher percentage had sexual problems prior to conception (P=0.03); the length of hospitalization during pregnancy was longer (P=0.02), and the preterm delivery rate was higher (P=0.01). Withingroup changes over gestation time indicated that IVF women, not controls, showed an increase in positive affect (P=0.04) and purpose in life (P=0.05).
Conclusions
IVF women are inclined to social isolation. Despite more medical problems during pregnancy, they reported improved positive emotions and purpose in life as the pregnancy progressed.
Keywords: in vitro fertilization, psychological well-being, quality of life, pregnancy
IZVLEČEK
Namen
Namen študije je bil ugotoviti, ali se počutje in stopnja kvalitete življenja žensk, ki zanosijo s pomočjo postopkov oploditve z biomedicinsko pomočjo (in vitro fertilization - IVF), razlikuje od počutja in stopnje kvalitete življenja žensk, ki zanosijo spontano.
Metode
V prospektivno študijo smo vključili 153 nosečnic; 75 žensk je zanosilo po IVF-metodi (IVF-skupina), 78 pa spontano v istem časovnem obdobju (kontrolna skupina). Odzvalo seje 66,6% žensk v IVF-skupini in 83,3% žensk v kontrolni skupini. Vsem je bil poslan anamnestični vprašalnik o biografskih in reproduktivnih podatkih, zdravstveni zgodovini in doživljanju nosečnosti, ki je vseboval tudi lestvico subjektivne kvalitete življenja (QLS), lestvico pozitivnih in negativnih čustev (PANAS), lestvico dobrega počutja (PWB), Beckov vprašalnik depresije (BDI) in Zinged vprašalnik anksioznosti (SAS). Podatke o porodu in novorojencu smo dobili iz porodnega zapisnika.
Rezultati
Povprečna starost žensk v IVF-skupini je bila 33,8 leta in v kontrolni skupini 32,5 leta. Skupini se po psihičnem statusu žensk nista razlikovali v večini merjenih spremenljivk. Ženske v IVF-skupini so izražale le manjše zadovoljstvo s svojim socialnim življenjem (P=0,03), imele so več težav v spolnosti pred zanositvijo (P=0,03), odstotek hospitalizacij pri njih je bil višji (P=0,02) in tudi delež prezgodnjih porodov je bil višji (P=0,01). Testiranje sprememb znotraj skupin je pokazalo naraščanje pozitivnih čustev (P=0,04) in občutenja smisla življenja (P=0,05) z napredovanjem nosečnosti v IVF-skupini.
Zaključek
Ženske v IVF-skupini težijo k socialni izolaciji. Kljub večjemu številu zdravstvenih težav pa se z napredovanjem nosečnosti krepijo njihova pozitivna čustva in občutenje smisla življenja.
1 INTRODUCTION
Ever since in vitro fertilization (IVF) was introduced as an infertility treatment option, couples that would never be able to conceive naturally have been given a chance to conceive and have their own biological children. Although many retrospective and some prospective studies on the course and outcome of IVF pregnancies have been performed (1–6), they have not sufficiently elucidated potential unfavourable effects of assisted conception on the course of pregnancy, labour, delivery, and the baby. We believe that in addition to the proven higher multiple pregnancy rate registered in IVF pregnancies (7), which is a known risk factor for preterm delivery and consequently for increased neonatal morbidity and mortality (8), there are other unfavourable effects of IVF conception on pregnancy, as well as the effect of infertility on psychological well-being and quality of life of women who conceive after infertility treatment. The high frequency of multiple births and the high maternal age are interpreted as contributing factors, not the IVF technique itself. Some authors (9, 10) did not find an increased risk for prematurity, low birth weight, or maternal or fetal complications, but a high rate of caesarean sections in singleton IVF mothers compared to age matched control group of singleton spontaneous pregnancies. Obstetric haemorrhages (antepartum haemorrhage, placenta praevia, placental abruption and primary post-partum haemorrhage) are more frequent with singleton births after IVF, ICSI and GIFT (11). Major improvement in the outcome after IVF can be seen during the 25 years period for both obstetric and neonatal variables due to a decline in the rate of multiple births following the reduction in the number of embryos transferred. Some effects are seen also with singleton births and they may be due to a shortening of the period of childlessness before IVF treatment begins and an increased use of ICSI (12).
In spite of the importance of the mind-body connection and fertility, the psychosocial aspects of infertility have not been adequately addressed. Fertility treatment is both a physical and emotional stress for both partners. Depression, state-anxiety, and stress-induced changes in heart rate and cortisol are decreasing the probability of achieving a viable pregnancy (13). A couple that is trying to conceive will undoubtedly experience feelings of frustration and disappointment if pregnancy is not easily achieved, which may result in a severe insult to self-esteem, body image, depression and self-assessed masculinity or femininity (14, 15). There is evidence of three types of relationships between psychological factors and infertility, namely:
Psychological factors are risk factors of subsequent infertility;
the experience of the diagnosis and treatment of infertility causes subsequent psychological distress;
a reciprocal relationship exists between psychological factors and infertility (13).
Infertility treatment is stressful on many levels: physically, psychologically, financially and also time consuming; pregnancy achieved after IVF is considered as a gift for the already exhausted parents (16). Pregnancy itself imposes psychic stress that is further increased in women who conceive after infertility treatment (17). Clinical reports and qualitative studies suggest that pregnancy and parenting may be more complex psychologically after assisted than spontaneous conception (18, 19). Infertile couples who are now expecting frequently experience guilt and shame originating from the time of their infertility and have a feeling of incompetence, defect, and possibly shame due to the method of conception (20). Some studies have presented longitudinal data on the emotional response of pregnant women or young mothers after successful IVF; no differences have been reported between the women who conceived through IVF and those who conceived spontaneously, indicating that the stress of the treatment disappeared when a pregnancy was achieved (3, 10, 21).
Due to the lack of satisfactory data in Slovenia as well as worldwide, we carried out a cross-sectional study to define psychological factors, and also some somatic factors accompanying the pregnancy achieved through IVF.
The aim of this cross-sectional study was to find whether the women conceiving through IVF differ from those conceiving spontaneously in terms of psychological well-being and quality of life, the course and outcome of pregnancy, and the neonate’s condition.
2 MATERIALS AND METHODS
A cross-sectional study on well-being of Slovenian women who conceived through IVF (IVF group) and those who conceived spontaneously (control group) was carried out at the Department of Human Reproduction, Division of Obstetrics and Gynaecology, University Medical Centre Ljubljana in a nine month period.
Women between 5th and 26th weeks of pregnancy were eligible to participate in the study. The IVF women were recruited from the IVF registry, and the control group from among the pregnant women who came to regular gynaecologic examinations at outpatient clinics of the Division of Obstetrics and Gynaecology.
All the enrolled women were sent a questionnaire in order to obtain their basic socio-demographic data and infertility history, report on pregnancy complications, mother’s and their partner’s feelings about the pregnancy (5 level rating scale: 1 - never, 5 - mostly; e.g. “Experiencing fear for the child”), past difficulties with physical and mental health, sexuality, violence, drugs, etc (e.g.: “Have you had sexual problems?” 1. No, 2. Yes; “Have you been a victim of sexual violence?” 1. No, 2. Yes), and a subjective evaluation of experiencing stress in infertility treatment on the Likert scale (from 1 “not even stressful” to 5 “very stressful”) and tests / inventories for the assessment of their psychological well-being.
The comparison between the groups involved socio-demographic characteristics, psychological well-being, and quality of life. Additionally, we analysed the data on infertility history, complications during pregnancy and the course of labour obtained from delivery records, and neonatal data obtained from neonatal records. We were also interested whether well-being is changing during pregnancy and we have therefore tested for differences before and after 20th week of pregnancy within the IVF group. At the same time we tested for differences during pregnancy between the IVF and control group.
The women signed a written consent form before they were enrolled in the study allowing their medical records to be accessed for the purpose of the study.
For the assessment of the women’s psychological condition, Beck Depression Inventory (BDI) (22) and Zung Self-Rating Anxiety Scale (SAS) (23) were used.
The women’s quality of life was assessed using the following tests: Subjective Quality of Life Scale (QLS) (24) which assesses the importance of individual components of quality of life (‘friends/acquaintances’, ‘leisure time/hobbies’, ‘health’, ‘income/financial security’, ‘occupation/work’, ‘housing/living conditions’, ‘family life/children’, and ‘partner relationship/sexuality’) and satisfaction with them, the Positive and Negative Affect Scale (PANAS) (25) which assesses the expression of positive and negative emotions; the Psychological Well-Being Scale (PWB) (26) which assesses the ways in which a person copes with existential problems using the score composed of six dimensions (autonomy, environmental mastery; self-acceptance, personal growth, positive relations with others and purpose in life). It took 15–20 minutes to fill out all the questionnaires.
2.1 Statistical Analysis
Statistical analyses were performed using SPSS for Windows version 21 (IBM Corp., Armonk, NY, USA). The difference between the groups was tested using parametric and non-parametric tests (t-test, ANOVA, Pearson’s correlation test, chi-square test, Mann-Whitney and Wilcoxon test) considering 95% confidence interval. Statistical significance was set at P<0.05.
3 RESULTS
Study subjects consisted of 153 pregnant women who conceived in the observed nine month, 75 in the IVF group and 78 in the control group. Twenty-five women in the IVF group and 13 in the control group declined their participation; the response rate was 66.6% and 83.3% in the IVF and control group, respectively. One woman in the IVF group and 2 in the control group were later excluded from study for spontaneous abortion, leaving 49 women in the IVF and 63 women in the control group. In the IVF group, 57 babies were born, eight pairs of them were twins (16.33%); in the control group, 64 babies were born, with only one pair of twins among them (1.59%).
The groups were homogeneous by age (33.7 vs. 32.5 years), marital status (65% vs. 50% married), educational level (52% vs. 58% higher education), and employment status (81% vs. 80% with reliable employment). All women in the IVF group conceived after an IVF procedure, whereas the women in the control group conceived spontaneously, but 2 (3.2%) conceived after surgical treatment of infertility and 2 (3.2%) after hormonal therapy for infertility.
There was no difference in the number of previous pregnancies, but we observed more extrauterine pregnancies in IVF group that were statistically significant (16.3% vs. 0.0%) and more childless women in the IVF group (75.5% vs. 44.4%).
In the IVF group the time interval between first attempts to conceive to eventually seeking help for infertility was mean 2 years and 8 months, and the mean time interval between the infertility diagnosis and treatment, IVF attempts included, and achieved pregnancy was 2 years and 6 months. The women’s subjective assessment of infertility treatment and IVF procedures was as follows: 2 (4.1%) as highly stressful, 20 (40.8%) as rather stressful, 17 (34.7%) as moderately stressful, and 8 (16.3%) as little stressful.
The women did not differ between the groups regarding their feelings about pregnancy (ambivalence, fear, happiness, disappointment, doubt ...).
Improved psychological well-being in comparison to that from the previous pregnancy was reported by 10 (20.4%) IVF mothers, and by 3 (4.8%) mothers in the control group, the difference was statistically significant (P = 0.03).
Furthermore, IVF mothers experienced sex problems before pregnancy (n=4; 8.2%), whereas those in the control group did not (P=0.03).
Among the items assessing the quality of life (QLS), a significant difference was observed only in the dimension ‘friends/acquaintances’ which was significantly lower in the IVF than in the control group mothers (P=0.03) There were no statistically significant differences between the groups in positive and negative affects (PANAS), in environmental mastery, self-acceptance, interpersonal relationship, autonomy, personal growth, and purpose in life (PWB scale), and in the level of depression (BDI) and anxiety (SAS questionnaires) (Table 1).
Table 1.
Comparison of satisfaction with various sections of quality of life (QLS), dominant emotions (PANAS), psychological well-being (PWB), depression (BDI) and anxiety SAS) between IVF group and control group (ANOVA test).
| IVF group (n=49) | Control group (n=63) | P-value | |||
|---|---|---|---|---|---|
|
|
|
||||
| mean | SD | mean | SD | ||
| Subjective quality of life scale - QLS | |||||
| Friends / Acquaintances | 9.16 | 6.04 | 11.56 | 5.66 | 0.033 |
| Free time / Hobbies | 7.78 | 6.63 | 8.62 | 6.34 | 0.495 |
| Health | 13.38 | 6.19 | 13.51 | 7.05 | 0.918 |
| Income / Financial security | 5.90 | 6.06 | 7.94 | 5.57 | 0.067 |
| Profession / Work | 7.29 | 7.66 | 9.06 | 5.98 | 0.174 |
| Home / Life circumstances | 15.82 | 4.72 | 13.81 | 6.35 | 0.067 |
| Family life / Children | 16.17 | 4.78 | 17.08 | 4.40 | 0.308 |
| Relationship with partner | 17.16 | 4.90 | 15.67 | 6.61 | 0.188 |
| Sexuality | 11.54 | 6.92 | 12.75 | 6.18 | 0.336 |
|
| |||||
| Positive and Negative Affect Schedule. PANAS | |||||
| Positive emotions | 35.87 | 4.97 | 36.79 | 4.13 | 0.299 |
| Negative emotions | 20.31 | 5.89 | 19.94 | 6.10 | 0.747 |
|
| |||||
| Psychological Well-Being (PWB) Scale | |||||
| Environmental mastery | 19.96 | 2.64 | 19.78 | 2.59 | 0.716 |
| Self-acceptance | 20.84 | 2.49 | 20.74 | 2.44 | 0.834 |
| Interpersonal relations | 19.53 | 3.75 | 20.10 | 3.01 | 0.379 |
| Autonomy | 26.94 | 4.75 | 26.53 | 4.41 | 0.648 |
| Personal growth | 26.19 | 2.97 | 26.42 | 3.35 | 0.706 |
| Purpose in life | 20.68 | 3.19 | 20.90 | 2.36 | 0.676 |
|
| |||||
| Beck Depression Inventory - BDI | 5.35 | 4.93 | 4.35 | 3.27 | 0.202 |
|
| |||||
| Self-Rating Anxiety Scale - SAS | 30.63 | 6.54 | 31.27 | 7.49 | 0.638 |
The level of stress during infertility treatment showed an important negative correlation between stress and health (self-assessed): the higher the level of stress the lower the satisfaction of IVF mothers with their personal health (P=0.04) (Table 2).
Table 2.
Correlation of degree of stress with various sections of quality of life (QLS), dominant emotions (PANAS), results of the PWB Scale, depressive mood (BDI) and anxiety (SAS) in the IVF group.
| Pearson’s correlation coefficient | P-value | |
|---|---|---|
| Quality of life scale QLS | ||
| Friends / Acquaintances | 0.23 | 0.09 |
| Free time / Hobbies | 0.11 | 0.45 |
| Health | −0.30 | 0.04* |
| Income / Financial security | −0.09 | 0.55 |
| Profession / Work | −0.09 | 0.54 |
| Home / Life circumstances | −0.19 | 0.17 |
| Family life / Children | 0.00 | 0.99 |
| Relationship with partner | −0.11 | 0.45 |
| Sexuality | −0.09 | 0.53 |
|
| ||
| Positive and Negative Affect Schedule. PANAS | ||
| Positive emotions | 0.01 | 0.96 |
| Negative emotions | 0.22 | 0.14 |
|
| ||
| Psychological Well-Being (PWB) | ||
| Environmental mastery | −0.07 | 0.62 |
| Self-acceptance | −0.16 | 0.26 |
| Interpersonal relations | 0.14 | 0.35 |
| Autonomy | 0.12 | 0.43 |
| Personal growth | −0.01 | 0.97 |
| Purpose in life | −0.13 | 0.39 |
|
| ||
| Degree of depression (Beck Depression Inventory - BDI) | 0.25 | 0.08 |
|
| ||
| Degree of anxiety (Self-Rating Anxiety Scale - SAS) | 0.07 | 0.63 |
The comparison between IVF mothers pregnant up to 20 weeks (n=18) and those pregnant beyond 20 weeks (n=31) at the time of completing the questionnaire showed a significantly stronger expression of positive emotions (P=0.04), and significantly more purpose in life (P=0.05) in the latter subgroup (Table 3).
Table 3.
Comparison of satisfaction with various sections of quality of life (QLS), dominant emotions (PANAS), psychological well-being (PWB), depression (BDI) and anxiety SAS) among women pregnant up to 20 weeks, and women pregnant beyond 20 weeks within the IVF group (ANOVA test).
| IVF group to 20th week (n=18) | IVF group beyond 20th week (n=31) | P-value | |
|---|---|---|---|
|
|
|
||
| mean (SD) | mean (SD) | ||
| Subjective quality of life scale - QLS | |||
| Friends / Acquaintances | 9.72 (6.75) | 8.84 (5.67) | 0.63 |
| Free time / Hobbies | 6.83 (6.96) | 8.32 (6.48) | 0.45 |
| Health | 13.59 (7.61) | 13.26 (5.40) | 0.86 |
| Income / Financial security | 5.67 (5.89) | 6.03 (6.25) | 0.84 |
| Profession / Work | 7.06 (7.48) | 7.42 (7.88) | 0.88 |
| Home / Life circumstances | 15.00 (5.06) | 16.29 (4.53) | 0.36 |
| Family life / Children | 16.44 (5.03) | 16.00 (4.69) | 0.76 |
| Relationship with partner | 16.11 (6.59) | 17.77 (3.57) | 0.26 |
| Sexuality | 12.50 (6.71) | 10.97 (7.09) | 0.46 |
|
| |||
| Positive and Negative Affect Schedule. PANAS | |||
| Positive emotions | 33.94 (4.34) | 36.97 (5.04) | 0.04* |
| Negative emotions | 21.56 (7.89) | 19.58 (4.33) | 0.26 |
|
| |||
| Psychological Well-Being (PWB) Scale | |||
| Environmental mastery | 19.83 (3.26) | 20.03 (2.26) | 0.80 |
| Self-acceptance | 20.28 (3.25) | 21.16 (1.90) | 0.23 |
| Interpersonal relations | 18.50 (4.25) | 20.13 (3.36) | 0.15 |
| Autonomy | 26.41 (6.29) | 27.23 (3.69) | 0.57 |
| Personal growth | 25.67 (3.25) | 26.50 (2.80) | 0.35 |
| Purpose in life | 19.44 (4.47) | 21.32 (2.09) | 0.05* |
|
| |||
| Beck Depression Inventory - BDI | 5.94 (5.56) | 5.00 (4.58) | 0.52 |
|
| |||
| Self-Rating Anxiety Scale - SAS | 29.33 (4.69) | 31.39 (7.38) | 0.29 |
ANOVA test revealed statistically significant interaction term group*gestation which means different trends of positive emotions (as measured by PANAS) with the ongoing weeks of pregnancy (P=0.001) (Figure 1). The similar conclusion holds for the purpose of life (PWB) (P=0.02) (Figure 2).
Figure 1.
Change of positive emotions during pregnancy.
Figure 2.
Change of “purpose in life” during pregnancy.
Complications during pregnancy were reported by 13 (26.5%) women in the IVF group, and 9 (14.3%) women in the control group (P=0.08), with bleeding being the most frequent complication (12; 24.5% IVF group vs. 8; 12.7% control group; P=0.09). Consequently, the percentage of hospitalization was statistically higher in the IVF than in the control group (n=13; 26.5% vs. n=7; 11.5%; P=0.02). Furthermore, the use of spasmolytics and gestagens was higher in the IVF than in the control group (n=13; 16.5% vs. n=6; 9.8%; P=0.02, and n=20; 40.8% vs. n=1; 1.6%; P<0.01, respectively).
4 DISCUSSION
The present study is the first in Slovenia that analysed not only health complications of IVF mothers and their neonates but also the psychological well-being and quality of life in the course of pregnancy after infertility treatment with IVF.
We have found that mothers who conceive through IVF do not experience a higher degree of anxiety or depression. However, we have observed a tendency of these women to social isolation and sex problems before pregnancy that may eventually result in poorer quality of some aspects of life, in comparison with pregnant women who conceive spontaneously.
The sample of mothers who conceived through IVF has two flaws: a relatively old age of control group mothers and a relatively short treatment period before conception.
The mean age of IVF mothers at delivery was 33.8 years (range 26–42 years), and that of control group mothers was 32.5 years (range 24–43 years), which is more than the mean age in the general population of Slovenian mothers. On average, IVF mothers conceived 30 months after starting seeking infertility treatment which is a relatively short interval for infertile mothers. This might be the reason why the effects of infertility treatment on psychological well-being of mothers were not manifested to the extent these effects would have been manifested after a longer treatment period. This relatively short treatment period is partly due to full reimbursement of the costs of IVF treatment which allows a rather rapid successful management of infertile couples, which consequently means less stress in the treated couples. Additionally, we may speculate that the mothers who were under a greater psychological pressure due to infertility and subsequent treatment were very likely not willing to participate in the study. Thus, there might have been an unintended selection of mothers before the data collection. Similarly, when interpreting the results, it should be borne in mind that the sample of IVF mothers was relatively small due to their poor participation; the response rate was 66.6%; it might have been difficult for them to once again go through all the stressful procedures or events they underwent.
As we found later, the control group mothers did conceive spontaneously, but some after surgical treatment on the reproductive tract (1 myomectomy, 3 resections of the septum, and 4 surgeries on ovaries). These women might have carried some of the characteristics of IVF mothers. Namely, the inclusion criterion depended on the mode of conception: either IVF or spontaneous, whereas the anamnestic questionnaire was more specific about conception problems.
Interestingly, 8.2% of IVF mothers reported sexual problems before pregnancy, with 37.5% of them confirming that the change of sexual life was due to infertility, whereas none of the control group mothers reported them. Sexual problems have been stressed in some studies (27, 28).The origin of these problems lies in the time when the couple was infertile, when sexual intercourse became a purely mechanical act with the sole aim to achieve pregnancy. The spontaneity and intimacy between the partners are lost, which further negatively affects their relationship. Sexuality might remain the problem between the partners for years after successful pregnancy of the couple, infertile by then. Also, we were surprised to find that 5 (7.9%) control group mothers were victims of sexual violence; among the IVF mothers there were none.
The comparison of the impact of satisfaction with various items determining the quality of life (QLS) showed statistically significant differences only in social life between the groups in this study (Table 1). In IVF couples the tendency to social isolation has been established in various studies (28, 29). The reason for such behaviour may lie in the wish of these couples to avoid family reunions menacing with a constant and emphasized pressure through questions on when they are going to have children. They also avoid friends who have children as they begin to think they do not have anything in common anymore. Infertile couples mourn in solitude thinking that nobody understands them. Some feelings of otherness remain present even after the couple conceives. A pregnant woman, who was infertile, often thinks that the experience related to infertility and infertility treatment separates her from other pregnant women (20). In our study, both groups of pregnant women were, on average, equally satisfied with the relationships with their partners, which is in agreement with the findings of some either studies (30, 31).. There are two studies (10, 32) that have found a significantly better quality of relationship, higher degree of confidence and closer connection between the partners in IVF couples. On the other hand, some other authors (3) found lesser satisfaction of IVF mothers with the relationship with their partner in early pregnancy.
Regarding the results of the PWB scale assessing autonomy, environmental mastery; personal growth, positive relations with others, purpose in life and self-acceptance, there were no differences between the groups; similar results were obtained in the studies focussing on self-confidence and self-trust of women who conceived after IVF (3, 33, 34).
The analysis of the degree of depression and anxiety did not reveal statistically significant differences between the groups, which is in agreement with the results of some studies (3, 34–36). On the other hand, some authors (37) reported a higher incidence of mood disorders in women who conceived after IVF. Moreover, some other studies (32, 38) reported a lower incidence of depression symptoms in infertile mothers compared to mothers who conceived spontaneously.
As expected, the percentage of hospitalizations during the current pregnancy was statistically higher in IVF mothers in this study, and so was the rate of complications, bleeding ranking the highest, although the difference was not statistically significant, which might be due to a small sample size.
The occurrence of complications in these women often deteriorates the self-image and confidence in their own body and abilities, and strengthens the feeling of guilt and ambivalent feelings about pregnancy and the baby (16). Women who conceived through IVF/ICSI had higher levels of general anxiety and psychological stress than the women who conceived naturally, around the time of the first trimester screening (39), which was not confirmed in the present study. Recent studies (40–42) analysing congenital anomalies reported a slightly increased risk in IVF babies compared to spontaneously conceived babies. We have also found a slightly higher overall congenital anomaly rate in the IVF (9.1%) compared to the control group (3.2%), but the number of patients was too small for making a firm conclusion.
We may conclude that mothers who conceive after IVF do not experience a higher degree of anxiety or depression, although some women in our sample showed subclinical and clinical levels of anxiety (scoring 45 or more on SAS) and depression (scoring 13 or more on BDI). However, we have observed a tendency of these women to social isolation and sex problems prior conception that may eventually result in poorer quality in some aspects of life if compared to pregnant women that conceive spontaneously. As such, some patients may still need or want interventions to improve quality of life during IVF treatment and pregnancy.
5 CONCLUSIONS
IVF mothers significantly more frequently observed an improvement in their psychological well-being during pregnancy, whereas the psychological well-being of mothers in the control group remained generally unchanged. Nevertheless, the surprising fact is that despite the higher incidence of complications during pregnancy, some of which even require hospitalization, and a higher rate of preterm deliveries, the satisfaction of IVF mothers increases as the pregnancy progresses; moreover, there is growing hope that they will finally have a baby, which increases their purpose in life.
ACKNOWLEDGMENTS
The authors wish to thank Mrs Sara Hajdarevič for translating and copy editing the text.
Footnotes
CONFLICTS OF INTEREST
The authors declare that no conflicts of interest exist.
FUNDING
No funding has been received for the conduct of this study and/or preparation of this manuscript.
ETHICAL APPROVAL
Research was conducted according to ethical principles, and was approved by The National Ethics Committee in 2008, reference number 174/07/08.
REFERENCES
- 1.De Sutter P, Bontinck J, Schutysers V, Van der Elst J, Gerris J, Dhont M. First-trimester bleeding and pregnancy outcome in singletons after assisted reproduction. Hum Reprod. 2006;21:1907–11. doi: 10.1093/humrep/del054. [DOI] [PubMed] [Google Scholar]
- 2.Hansen M, Bower C, Milne E, de Klerk N, Kurinczuk JJ. Assisted reproductive technologies and the risk of birth defects: a systematic review. Hum Reprod. 2005;20:328–38. doi: 10.1093/humrep/deh593. [DOI] [PubMed] [Google Scholar]
- 3.Klock SC, Greenfeld DA. Psychological status of in vitro fertilization patients during pregnancy: a longitudinal study. Fertil Steril. 2000;73:1159–64. doi: 10.1016/s0015-0282(00)00530-6. [DOI] [PubMed] [Google Scholar]
- 4.Moll AC, Imhof SM, Cruysberg JR, Schouten-van Meeteren AY, Boers M, van Leeuwen FE. Incidence of retinoblastoma in children born after in-vitro fertilisation. Lancet. 2003;361:309–10. doi: 10.1016/S0140-6736(03)12332-X. [DOI] [PubMed] [Google Scholar]
- 5.Reddy UM, Wapner RJ, Rebar RW, Tasca RJ. Infertility, assisted reproductive technology, and adverse pregnancy outcomes: executive summary of a National Institute of Child Health and Human Development workshop. Obstet Gynecol. 2007;109:967–77. doi: 10.1097/01.AOG.0000259316.04136.30. [DOI] [PubMed] [Google Scholar]
- 6.Stromberg B, Dahlquist G, Ericson A, Finnstrom O, Koster M, Stjernqvist K. Neurological sequelae in children born after in-vitro fertilisation: a population-based study. Lancet. 2002;359:461–5. doi: 10.1016/S0140-6736(02)07674-2. [DOI] [PubMed] [Google Scholar]
- 7.Korosec S, Tomazevic T, Virant Klun I, Meden Vrtovec H. Characteristics of twin-prone women undergoing in vitro fertilization and double blastocyst transfer - the Slovenian experience. Geburtshilfe Frauenheilkd. 2007;67:1109–13. [Google Scholar]
- 8.Adamson D, Baker V. Multiple births from assisted reproductive technologies: a challenge that must be met. Fertil Steril. 2004;81:517–22. doi: 10.1016/j.fertnstert.2003.09.041. , discussion 26. [DOI] [PubMed] [Google Scholar]
- 9.Reubinoff BE, Samueloff A, Ben-Haim M, Friedler S, Schenker JG, Lewin A. Is the obstetric outcome of in vitro fertilized singleton gestations different from natural ones?: a controlled study. Fertil Steril. 1997;67:1077–83. doi: 10.1016/s0015-0282(97)81442-2. [DOI] [PubMed] [Google Scholar]
- 10.Sydsjo G, Wadsby M, Kjellberg S, Sydsjo A. Relationships and parenthood in couples after assisted reproduction and in spontaneous primiparous couples: a prospective long-term follow-up study. Hum Reprod. 2002;17:3242–50. doi: 10.1093/humrep/17.12.3242. [DOI] [PubMed] [Google Scholar]
- 11.Healy DL, Breheny S, Halliday J, Jaques A, Rushford D, Garrett C, et al. Prevalence and risk factors for obstetric haemorrhage in 6730 singleton births after assisted reproductive technology in Victoria Australia. Hum Reprod. 2010;25:265–74. doi: 10.1093/humrep/dep376. [DOI] [PubMed] [Google Scholar]
- 12.Kallen B, Finnstrom O, Lindam A, Nilsson E, Nygren KG, Otterblad Olausson P. Trends in delivery and neonatal outcome after in vitro fertilization in Sweden: data for 25 years. Hum Reprod. 2010;25:1026–34. doi: 10.1093/humrep/deq003. [DOI] [PubMed] [Google Scholar]
- 13.Cwikel J, Gidron Y, Sheiner E. Psychological interactions with infertility among women. Eur J Obstet Gynecol Reprod Biol. 2004;117:126–31. doi: 10.1016/j.ejogrb.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Domar AD, Broome A, Zuttermeister PC, Seibel M, Friedman R. The prevalence and predictability of depression in infertile women. Fertil Steril. 1992;58:1158–63. [PubMed] [Google Scholar]
- 15.Verhaak CM, Smeenk JM, Evers AW, Kremer JA, Kraaimaat FW, Braat DD. Women’s emotional adjustment to IVF: a systematic review of 25 years of research. Hum Reprod Update. 2007;13:27–36. doi: 10.1093/humupd/dml040. [DOI] [PubMed] [Google Scholar]
- 16.Covington SN, Burns LH. Infertility counseling: a comprehensive handbook for clinicians. Cambridge, New York: Cambridge University Press; 2006. [Google Scholar]
- 17.Brockington IF. Motherhood and mental health. Oxford: Oxford University Press; 1996. [Google Scholar]
- 18.Dunnington RM, Glazer G. Maternal identity and early mothering behavior in previously infertile and never infertile women. J Obstet Gynecol Neonatal Nurs. 1991;20:309–18. doi: 10.1111/j.1552-6909.1991.tb01694.x. [DOI] [PubMed] [Google Scholar]
- 19.Sandelowski M, Harris BG, Holditch-Davis D. Pregnant moments: the process of conception in infertile couples. Res Nurs Health. 1990;13:273–82. doi: 10.1002/nur.4770130503. [DOI] [PubMed] [Google Scholar]
- 20.Olshansky EF. Identity of self as infertile: an example of theory-generating research. ANS Adv Nurs Sci. 1987;9:54–63. doi: 10.1097/00012272-198701000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Hjelmstedt A, Widstrom AM, Wramsby H, Collins A. Emotional adaptation following successful in vitro fertilization. Fertil Steril. 2004;81:1254–64. doi: 10.1016/j.fertnstert.2003.09.061. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 23.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–9. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 24.Henrich G, Herschbach P. Questions on life satisfaction (FLZ(M)): a short questionnaire for assessing subjective quality of life. Eur J Psycholog Ass. 2000;16:150–9. [Google Scholar]
- 25.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 26.Ryff CD. Happiness is everything, or is it - explorations on the meaning of psychological well-being. J Personality Soc Psychol. 1989;57:1069–81. [Google Scholar]
- 27.Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol. 2007;21:293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Imeson M, McMurray A. Couples’ experiences of infertility: a phenomenological study. J Adv Nurs. 1996;24:1014–22. doi: 10.1111/j.1365-2648.1996.tb02938.x. [DOI] [PubMed] [Google Scholar]
- 29.Hirsch AM, Hirsch SM. The effect of infertility on marriage and self-concept. J Obst Gynecol Neon Nurs. 1989;18:13–20. doi: 10.1111/j.1552-6909.1989.tb01611.x. [DOI] [PubMed] [Google Scholar]
- 30.Hjelmstedt A, Widstrom AM, Wramsby H, Matthiesen AS, Collins A. Personality factors and emotional responses to pregnancy among IVF couples in early pregnancy: a comparative study. Acta Obstet Gynecol Scand. 2003;82:152–61. doi: 10.1034/j.1600-0412.2003.00040.x. [DOI] [PubMed] [Google Scholar]
- 31.Ulrich D, Gagel DE, Hemmerling A, Pastor VS, Kentenich H. Couples becoming parents: something special after IVF? J Psychosom Obstet Gynaecol. 2004;25:99–113. doi: 10.1080/17402520400004599. [DOI] [PubMed] [Google Scholar]
- 32.Fisher JR, Hammarberg K, Baker GH. Antenatal mood and fetal attachment after assisted conception. Fertil Steril. 2008;89:1103–12. doi: 10.1016/j.fertnstert.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 33.Cox SJ, Glazebrook C, Sheard C, Ndukwe G, Oates M. Maternal self-esteem after successful treatment for infertility. Fertil Steril. 2006;85:84–9. doi: 10.1016/j.fertnstert.2005.07.1287. [DOI] [PubMed] [Google Scholar]
- 34.Stanton F, Golombok S. Maternal-fetal attachment during pregnancy following in vitro fertilization. J Psychosom Obstet Gynaecol. 1993;14:153–8. doi: 10.3109/01674829309084438. [DOI] [PubMed] [Google Scholar]
- 35.Harf-Kashdaei E, Kaitz M. Antenatal moods regarding self, baby, and spouse among women who conceived by in vitro fertilization. Fertil Steril. 2007;87:1306–13. doi: 10.1016/j.fertnstert.2006.11.035. [DOI] [PubMed] [Google Scholar]
- 36.Hjelmstedt A, Widstrom AM, Collins A. Psychological correlates of prenatal attachment in women who conceived after in vitro fertilization and women who conceived naturally. Birth. 2006;33:303–10. doi: 10.1111/j.1523-536X.2006.00123.x. [DOI] [PubMed] [Google Scholar]
- 37.Demyttenaere K, Bonte L, Gheldof M, Vervaeke M, Meuleman C, Vanderschuerem D, et al. Coping style and depression level influence outcome in in vitro fertilization. Fertil Steril. 1998;69:1026–33. doi: 10.1016/s0015-0282(98)00089-2. [DOI] [PubMed] [Google Scholar]
- 38.Repokari L, Punamaki RL, Poikkeus P, Vilska S, Unkila-Kallio L, Sinkkonen J, et al. The impact of successful assisted reproduction treatment on female and male mental health during transition to parenthood: a prospective controlled study. Hum Reprod. 2005;20:3238–47. doi: 10.1093/humrep/dei214. [DOI] [PubMed] [Google Scholar]
- 39.Darwiche J, Lawrence C, Vial Y, Wunder D, Stiefel F, Germond M, et al. Anxiety and psychological stress before prenatal screening in first-time mothers who conceived through IVF/ICSI or spontaneously. Women Health. 2014;54:474–85. doi: 10.1080/03630242.2014.897677. [DOI] [PubMed] [Google Scholar]
- 40.Ceelen M, van Weissenbruch MM, Vermeiden JP, van Leeuwen FE, Delemarre-van de Waal HA. Growth and development of children born after in vitro fertilization. Fertil Steril. 2008;90:1662–73. doi: 10.1016/j.fertnstert.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 41.Hansen M, Kurinczuk JJ, Milne E, de Klerk N, Bower C. Assisted reproductive technology and birth defects: a systematic review and meta-analysis. Hum Reprod Update. 2013;19:330–53. doi: 10.1093/humupd/dmt006. [DOI] [PubMed] [Google Scholar]
- 42.Kallen B, Finnstrom O, Lindam A, Nilsson E, Nygren KG, Otterblad PO. Congenital malformations in infants born after in vitro fertilization in Sweden. Birth Defects Res Clin Mol Teratol. 2010;88:137–43. doi: 10.1002/bdra.20645. [DOI] [PubMed] [Google Scholar]