Abstract
Objectives
The aim of the study is to assess the weight loss programme with regards to the long-term effectiveness of weight reduction and weight maintenance, using completion rate and BMI, blood sugar, cholesterol and blood pressure levels as outcomes. The aim of the study also includes identifying the factors associated with adherence to the programme.
Methods
The programme was developed by a multidisciplinary team. It included 6 months of introduction and another 18 months of maintenance. The data for 397 participants was collected after 24 months.
Results
346 participants have completed the introduction and 123 have completed the programme. In the introduction, the average weight loss was 12% of the initial weight. The participants, who completed the full programme, lost 9.4% of their initial weight. The participants also significantly (p<0.05) reduced their blood sugar and cholesterol levels, as well as their blood pressure. The factors associated with adherence to the programme are: age over 50, lower educational levels, lower initial weight and higher weight loss in the introduction.
Conclusions
The multi-disciplinary approach to obesity treatment was effective for a selected group of people. The proportion of dropouts was relatively high, but still low compared to similar programmes. Group treatment and mutual support are of a great importance in bringing about and maintaining the changes.
Keywords: obesity therapy, weight reduction programme, primary health care, health care team, Slovenia, patient adherence
IZVLEČEK
Izhodišča
Namen raziskave je bil opredeliti kratkoročno in dolgoročno uspešnost programa glede na vztrajanje v njem, ITM, vrednost krvnega sladkorja, holesterola in krvnega tlaka pri udeležencih, ki so program zaključili. Želeli smo tudi opredeliti dejavnike, ki napovedujejo vztrajanje v programu.
Metode
V programu sodeluje multidisciplinarni tim strokovnjakov: zdravnik, diplomirana medicinska sestra, fizioterapevt in profesor telesne vadbe. Program ima dva dela: 6-mesečni shujševalni del in 18-mesečni vzdrževalni del. V program se je vključilo 397 udeležencev po nasvetu osebnega zdravnika. Podatke smo ocenili po 24 mesecih.
Rezultati
Prvi, shujševalni del programa je zaključilo 346 udeležencev, od tega jih je 123 zaključilo celotni program. V shujševalnem delu je bilo povprečno znižanje teže za 12% začetne teže, pri tistih, ki so zaključili vzdrževalni program, pa za 9,4% začetne teže. Udeležencem se je po dveh letih statistično pomembno (p<0,05) znižala vrednost krvnega sladkorja in holesterola, prav tako sta se znižala tudi sistolični in diastolični krvni tlak. Dejavniki, ki so vplivali na daljše vztrajanje v programu, so bili starost nad 50 let, nižja izobrazba, nižja vstopna teža in večja izguba kilogramov v prvem delu programa.
Zaključek
Z raziskavo smo želeli dokazati, da je multidisciplinarni pristop zdravljenja debelosti za tiste, ki zaključijo program v celoti, učinkovit. Delež tistih, ki so program zaključili predčasno, je relativno visok, vendar v primerjavi z ostalimi podobnimi programi še vedno nizek. Izkazalo se je, da so pogost stik s strokovnjakom, skupinska obravnava ter podpora ljudem z enakimi težavami izrednega pomena pri spreminjanju in vzdrževanju sprememb.
1 INTRODUCTION
Obesity is a chronic disease caused by psychological, social and genetic factors. Its incidence in the world continues to grow (1, 2). This growth is due to an easier access to food, higher food diversity, decreased bodily activity and the stress of modern living. The increased body weight is associated with an increased risk of developing various health problems (3). Even a small weight loss, from 5 to 10%, helps to improve one’s health (4).
The problem of obesity can be addressed on various levels. In 2014, more than 1.9 billion adults aged 18 years and older were overweight worldwide. At least 600 million of them were clinically obese; of which 39% adults were overweight and 13% obese (5). Based on the latest estimates in the European Union countries, 30–70% of the population is overweight, and obesity affects 10–30% of adults (5). The number of overweight children in EU has also been rising steadily (5). Slovenia is among EU countries with a high proportion of obesity, with 37.7% of overweight and 17.2% of obese adults (6). The proportion of adolescents who are overweight and obese is also increasing (7).
On an individual level, more than 30,000 different methods for weight management have been published (8, 9). A lot of them use alternative and complementary techniques. Many different types of treatment, including dieting by limiting caloric intake, behavioural approach, physical activity, medical therapy or surgery alone, have shown that the reduced weight gradually returns after the completed programme (10, 11). The most successful methods include multidisciplinary approaches, based on an individual work with a patient or a group, which helps maintain their motivation (12). Recently, more emphasis has been put on the long-term effectiveness of multidisciplinary programmes.
The new guidelines (13) recommend programmes that include three key components, namely: a moderately reduced diet, an increased physical activity and the use of behavioural strategies to help patients achieve and maintain a healthy body weight. According to the recommendations, team approach should be used, involving trained professionals, where primary care is considered to be the best setting for this activity.
Because of their complexity, these programmes are rare, poorly evaluated and poorly studied in a systematic manner, or they often fail to achieve and maintain the desired body weight (14).
In Slovenia, a National Health Programme for cardiovascular diseases was implemented in 2001, and its preventive programmes were implemented in health centres. One of the programmes is a programme of weight reduction and lifestyle change, which lasts for 16 weeks.
1.1 Description of the Weight Loss Programme
In an urban health centre in Ljubljana, Slovenia, a long term programme of weight reduction has been developing over the years. Theprogramme is a multidisciplinary one, and it was developed by a group of different experts. Doctors, graduate nurses, a professorof physical education and aphysical therapist all contributed to the creation and the implementation of the programme.
The method is based on the principle that the patient should be monitored even after he/she has reached the target weight, and that the multidimensional problem of obesity should be treated with a multidisciplinary approach.
The programme has two parts. The initial phase is aimed at lowering body weight and it lasts for six months. This phase is followed by the monitoring phase, which is aimed at maintaining the weight and keeping the changes in lifestyle. The total duration of the programme is two years.
There are four objectives or goals that the participants are supposed to achieve in the programme:
To maintain healthy eating habits, including the limitation of the daily caloric intake, from 500 to 1000 kcal from the energy needs of the obese adult.
To engage in an appropriate physical activity.
To improve self–confidence and quality of life.
To maintain the lifestyle changes.
At the beginning, each participant is assessed by the programme physician, who assesses their readiness for health changes, records their history of dieting and assesses their personal eating habits, trigger events for overeating, barriers to success, as well as the time of being obese and maximum body weight at any time. Afterwards, a clinical and laboratory examination is made to identify other potential risk factors. On the basis of this, the physician, together with the participant, sets a healthy, realistic target with regards to the patient’s weight. The target is discussed on an individual level, considering the decrease in body fat percentage while preserving lean mass.
Phase 1: the initial phase
The initial phase of the programme was designed to motivate participants to perform a regularand continuous physical activity of moderate intensity, and it consists of three sessions per week.
The programme starts with a visit to the physician in charge of the programme. These visits are repeated every two weeks. On alternate weeks, group sessions for 12 participants are organized. The group is led by a nurse who has been specially educated in the area of obesity, and who is, at the beginning of the programme, under the supervision of physician. The nurse leads the group, devises an individual meal and activity plan. After this stage, the nurse analyses dietary and activity diaries, identifies lapses, helps solving the problems, monitors change in body weight and body structure, which facilitates motivation.
Additionally, physical activity is organized once a week at a gym and once a week outdoors. These sessions are led by a teacher of physical education, or a physiotherapist. The group sessions in this part of the programme consist of educational and psychotherapeutic elements (behavioural, family and relationship therapy) with an emphasis on self-monitoring and social support for change. The aim of the initial part of the programme was to achieve the target weight through smaller realistic goals, at least for 5–10 % for the initial weight loss. In this period, we help the participants find out how to change their old habits and adhere to a healthier lifestyle.
Phase 2: the maintenance phase
The weight maintenance programme is organized three times a week. It consists of weekly group therapy and twice-a-week physical activity at a health centre. The participants are also encouraged to follow intense exercise at least twice on the remaining days of the week (e.g. brisk walking, jogging, cycling, and swimming) on their own.
The goal of the maintenance programme is to enable the participants to maintain the lifestyle changes they have adopted in the previous phase. It showed that 20% could afford the occasional minor offenses in diet, but had to be constantly corrected by an increased physical activity. The results of the inspection were regularly monitored, recorded, and compared with the agreed objectives. They compared the old and new habits in their lifestyle, and were motivated to maintain the new, lower weight and a healthy lifestyle. The participants in this part of the programme are given more information on anti-stress techniques, maintaining weight during holidays, picnics, visits to restaurants, and other everyday situations.
The aim of the paper is to evaluate the programme with regards to the short-term effectiveness of the weight loss programme, as well as to confirm the effectiveness of the programme with regards to health risk reduction, including BMI, blood sugar, cholesterol and blood pressure, which influence the development of chronic non-infectious diseases. The paper also aims to determine the impacts of social factors, age, sex, education and social status on persevering in the programme, and the maintenance of a lower weight after the completed weight-reduction process.
2 METHODS
The programme was advertised in the health centre and offered to people who had problems with obesity. Patients were recruited at the advice of their physician.
2.1 Subjects
The study included the participants, who visited the Health centre Ljubljana, between 2005 and 2010, and were invited to participate in the programme. Among the people invited, 397 agreed to enter a two-year Obesity treatment programme. We included persons with BMI above 27, with one or more risk factors, and those with BMI of more than 30, regardless of other risk factors.
Exclusion criteria were BMI < 27, and severe physical diseases, for example, patients with serious chronic or acute diagnosis, patients with psychotic diseases and pregnant women.
2.2 Measurements
The nutritional status was assessed anthropometrically (body weight, body height) and by means of indices, such as body mass and BMI. Weight was measured using a calibrated electronic scale, to the nearest 0.1 kg. Height was measured by Martin anthropometer to the nearest 0.1 cm.
On the basis of the data obtained and BMI, still the best proxy for body fat percentage among rations of weight and height (15), the targeted body weight was calculated. The target weight was established on the individual level, taking into account patients’ maximum weight and the duration of their weight gainin years (16).
The risk factors, i.e. blood sugar and cholesterol, were examined in serum every six months using laboratory methods and by measuring the blood pressure.
2.3 Success Criteria
The success criteria were: long term effectiveness, completion rate and BMI, blood sugar, cholesterol and blood pressure in patients that had finished the programme.
We assessed the effectiveness by the share of those who achieved and maintained, at the end of the 24 months’ programme, at least 5 to 10% lower than their initial weight. We also wanted to identify the factors associated with a greater likelihood of finishing the programme.
2.4 Statistical Analyses
Logistic regression was used as a method of determining the factors that influence success. The accepted risk was 5%. The analysis was made using SPSS for Windows software version 13.
2.5 Ethical Considerations
We received written consent from all the participants allowing us to analyse the data. The study was approved by the National Ethics Committee of Slovenia, No.:24PK/06/11, Date: 27. 5. 2011
3 RESULTS
3.1 Description of the Sample
The number of participants who participated in the programme between 2005 and 2010 was 397 (352 women, 45 men). The initial programme was completed by 345 participants (34 men and 312 women). Out of them, about a third (123: 109 women and 14 men) then completed the full programme, which contained a cycle of 12 individual medical treatments, 12 group medical treatments and 24 hours of physical activities in health centre in six months. The average age of the participants that entered the programme was 53.3 (±11.7) years. The youngest participant was 19 years old and the oldest one 73. The majority of those in the two-year programme had a secondary school education (69 participants), the second greatest number included those with a lower education (34 participants), while the number of those with a college or university degree was the lowest (19 participants).
3.2 Success Criteria
3.2.1 Adherence
The BMI decrease was statistically significant (p<0.05), the gender difference was not statistically significant (Table 2).
Table 2.
BMI before and after the programme.
Mean and standard deviation.
| BMI (kg/m2) | The beginning of the programme | The end of the programme | P |
|---|---|---|---|
| Men | 36.1 (3.3) | 32.4 (4.3) | P<0.05 |
| Women | 34.5 (4.4) | 32.0 (4.1) | P<0.05 |
| Total | 34.7 (4.3) | 32.1 (4.1) | P<0.05 |
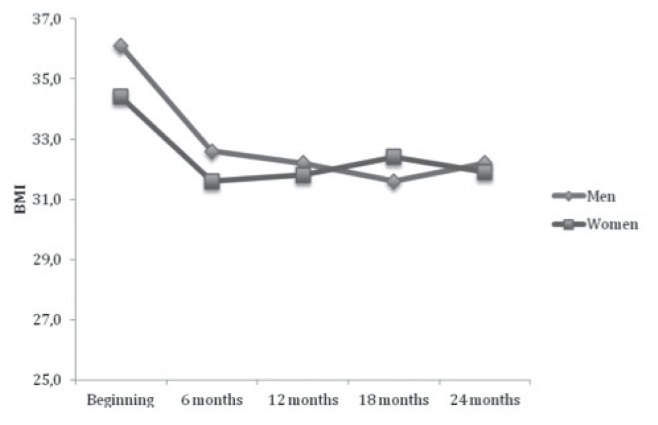
3.2.2 Changes in BMI
Upon entering the programme, the average BMI was 34.7 (SD 4.3). Figure 1 shows the changes in BMI throughout the programme.
Figure 1.
Values of BMI in the participants at the beginning and after 6, 12, 18 and 24 months.
3.2.3 Cholesterol, Glucose and Blood Pressure Levels
After two years, the participants showed a statistically significant reduction in their blood sugar value (p<0.001), cholesterol (p<0.01), as well as systolic (p<0.001) and diastolic blood pressure (p<0.001). The results are shown in Table 3.
Table 3.
The average values and SD of glucose, cholesterol, systolic and diastolic blood pressure (BP) before and after the programme.
| BMI (kg/m2) | The beginning of the programme | The end of the programme | P |
|---|---|---|---|
| Glucose (mmol/l) | 6.2 (1.6) | 5.8 (1.3) | P<0.001 |
| Cholesterol | 5.7 (0.9) | 5.5 (0.9) | P<0.005 |
| Systolic BP (mmHg) | 135.1 (19.0) | 130.4 (15.6) | P<0.001 |
| Diastolic BP (mmHg) | 84.8 (11.0) | 81.2 (9.4) | P<0.001 |
3.3 Predicting the Factors of Adherence
The factors influencing adherence to the programme are: age over 50, lower education levels, lower initial weight, and higher weight loss in the first part of programme (Table 4).
Table 4.
Factors determining adherence to the programme.
| B | SE | Wald | Df | P | Exp (B) | 95.0% interval EXP (B) | ||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Min | Max | |||||||
| Education (1) | 0.6430 | 0.2951 | 4.747 | 1 | 0.029 | 1.902 | 1.067 | 3.392 |
| Age (1) | −0.6219 | 0.2545 | 5.968 | 1 | 0.015 | 0.537 | 0.326 | 0.884 |
| Weight | −0.0089 | 0.0034 | 6.640 | 1 | 0.010 | 0.991 | 0.985 | 0.998 |
| Difference in weight after 6 Months | 0.0363 | 0.0196 | 3.430 | 1 | 0.064 | 1.037 | 0.998 | 1.077 |
4 DISCUSSION
4.1 Methodological Considerations
The sample of people participating in the programme does not reflect the prevalence of obesity in the population: there were nine times more women than men; the sample was not representative of Slovenia, since the programme was only conducted in urban health centres. Moreover, the sample consisted of significantly more women than men, because women were much more likely to decide to participate. Other authors also cited higher participation of women than men in the weight loss programmes (17, 18), which is due to the fact that obesity seems a more important issue for women than men, and that women tend to use health services more often (19), although statistics show that men are more likely to be overweight or obese (20). The relative non-attendance of men is probably an issue for the future, therefore alternative approaches more suitable for men should be considered.
4.2 Measures of Success
The first measure of success was adherence to the programme. The reported failure rates in the literature range from 10 to 80% (21). Patients tend to drop out of weight-loss programmes relatively quickly; usually in or around the sixth month of their treatment (22). From this perspective, our programme has been relatively successful, since nearly 87% of all patients finished the initial six months’ part of the programme. The adherence rate to the long-term programme was, of course, lower, but still at the respectable 31%. In the literature, success rates between 20 and 45% are considered satisfactory (23, 24), so we can conclude that the adherence rate in our programme was relatively high for this type of health problem.
Other measures of success were expected: the average weight loss in the first six months of the initial programme was almost 10kg or 12% of the initial weight, which is comparable to similar published programmes in the world (14, 25). It is interesting to note that men were more successful than women in losing weight, which was also shown in studies by Petek (17) and Bishof (25). These results indicate, as does our study, a relatively greater success in maintaining low weight for men.
A lot of studies that have followed up patients for a longer period of time report a re-lapse of body weight after six months (26). Our study showed that women have indeed increased their weight slightly, while men still managed to reduce their weight up to 12 months after the programme. After that period, male and female participants increased their body weight moderately. Nevertheless, the increases of 2.2 kg at 12 months and of 2.6 kg after 24 months are small and within the success criteria in the guidelines, which consider that the maintenance programme has been successful, if patients do not gain more than 3 kg from the lowest achieved weight in the programme in two years (27).
The long-term success of those who completed the programme is also important, since, after two years, 40% of participants still maintained 10% less weightand less than 5% lower weight was maintained by 66% of participants. This is better than in the study by Teixeira, where, at the 24 month follow up, 45% of participants had retained a weight loss of at least 5% of their initial body weight. (28)
BMI is a better indicator of weight loss, as an important indication of the reduction and as an indicator of health risk (29) reached by the programme participants. The BMI in both sexes decreased significantly. As in other studies (30, 31), we found that there was a significant reduction in other risk factors as well, such as blood pressure, sugar and cholesterol.
We can also see that, although the youngest age group was most successful in losing weight during the first part of the programme, the long-term effects were better in the age group between 51, while, in another study (32), no difference was observed for the degree of weight loss when classified by age.
4.3 Factors Influencing Adherence
Educational level, age over 50 years, a lower initial weight and weight loss within the first six months were important predictors of adherence to the programme. Maybe the cause for the higher dropout rate of those with a higher education were, as stated in the study by Grossi et al. (33), practical problems, problems at work and logistics, whereas, in the study by Greenberg, the level of education made no difference (34).
The effect of initial weight was observed by Baautista et al. (35); in their study, a higher initial BMI was also associated with a higher drop-out rate. A greater weight loss in the first part of the programme was also described in the study by Greenbergdb (34). In another study (36), the amount of weight loss during the first three weeks of treatment had a marginal effect on reducing adherence. Social status and sex had no impact on perseverance in our study. Interestingly, however, the fact that, in the first part of the programme, men were more successful did not affect greater persistence.
5 CONCLUSION
Our study shows that a multidisciplinary approach to treating obesity works for a selected group of patients, and that this approach has long-term effects. The complexity of the programme reflects the complexity of obesity as a health care problem, which requires long term commitment on behalf of both patients and healthcare providers. Frequent contacts with an expert, based on empathy, group treatment and mutual support between persons with equal problems are of great importance in bringing about and maintaining changes.
The multidisciplinary programme requires a commitment of the participants and staff, so this raises the question of the cost benefit.
On a systemic level, this programme fulfils the criteria to be upgraded to primary health care, the family medicine area of healthy weight loss.
Nevertheless, the issue of how to approach the groups of patients who find such methods unsuitable for them still remain. Obviously, new approacheswhich are more suitable for men need to be developed.
Table 1.
The adherence to the programme by sex.
| Men | Women | P | |
|---|---|---|---|
| Patients that have finished the six month programme | 20 (44.4%) | 203 (57.7%) | P<0.005 |
| Patients that have finished the whole programme | 14 (31.1%) | 109 (30.9%) | P=0.995 |
| Drop-outs | 11 (24.4%) | 40 (11.4%) | P<0.005 |
| Total | 45 (100%) | 352 (100%) |
The sex difference in the adherence was statistically important (p<0.005): women were more likely to adhere to the programme.
ACKNOWLEDGEMENTS
We would like to thank our colleagues and others who have helped to shape the weight- loss programme, and all the participants involved in the programme.
Footnotes
CONFLICTS OF INTEREST
The authors declare that no conflicts of interest exist.
FUNDING
The study was financed by Health Centre Ljubljana.
ETHICAL APPROVAL
The study was approved by the National Ethics Committee of Slovenia, No.:24PK/06/11.
REFERENCE
- 1.Molorious SA, Sedell JC, Sans S, Tuomilehto J, Kuulasamaa K. Educational level, relative body weight and changes in their association over 10 years: an international perspective from the WHO MONICA Project. Am J Publ Health. 2000;90:1260–8. doi: 10.2105/ajph.90.8.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Overweight and obesity-BMI statistics. Available Nov 2011 from: http://epp.eurostat.ec.europa.eu/statistics_explained/index.php/Overweight_and_obesity_BMI_statistic.
- 3.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health care. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 4.Seagle HM, Strain GW, Makris A, Reeves RS. Position of the American Dietetic Association: weight management. J Am Diet Assoc. 2009;109:330–46. doi: 10.1016/j.jada.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Obesity and overweight: fact sheet 311. Available Jan 2015 from: http://www.who.int/mediacentre/factsheets/fs311/en/
- 6.Hlastan-Ribič C. Izzivi v izboljšanju vedenjskega sloga in zdravja: desetletje CINDI raziskav. Ljubljana: NIJZ; 2014. pp. 35–41. [Google Scholar]
- 7.Strel J, Star G, Kovač M. SLOFIT sIstem - analiza telesnega in gibalnega razvoja otrok in mladine slovenskih osnovnih in srednjih šol v šolskem letu 2011/2012. Ljubljana: Fakulteta za šport; 2012. [Google Scholar]
- 8.Anonymous. Obesity in primary health care: a literature review. London: Health Education Authority; 1995. [Google Scholar]
- 9.Malik VS, Hu FB. Popular weight-loss diets: from evidence to practice. Nat Clin Cardiovasc Med. 2007;4:34–41. doi: 10.1038/ncpcardio0726. [DOI] [PubMed] [Google Scholar]
- 10.Wadden TA, Frey DL. A multicenter evaluation of property weight loss program for treatment of marked obesity: a five- year follow-up. Int J Eat Disord. 1997;22:203–12. doi: 10.1002/(sici)1098-108x(199709)22:2<203::aid-eat13>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 11.Anderson JW, Kons BC, Wood Cl. Long–term weight loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74:579–84. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 12.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(Suppl 2):S102–38. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai AG, Wadden TA. An evaluation of major commercial weight loss programs in the United States: a systematic review. Ann Intern Med. 2005;142:56–66. doi: 10.7326/0003-4819-142-1-200501040-00012. [DOI] [PubMed] [Google Scholar]
- 15.Singer-Vine J. Beyond BMI: “why doctors won’t stop using an outdated measure for obesity?”. Available Dec 2013 from: State.com.
- 16.Pokorn D. Higiena prehrane. Ljubljana: Medicinska fakulteta; 1996. [Google Scholar]
- 17.Petek D, Kern N, Kovač Blaž M, Kersnik J. Efficiency of community based intervention programme on keeping lowered weight. Zdrav Var. 2011;50:160–8. [Google Scholar]
- 18.Kolsek M. Long-term results of intensive treatment of obesity in the health centre Litija, Slovenia: a clinical audit. Int J Obes Relat Metab Disord. 1999;23:702–5. doi: 10.1038/sj.ijo.0800908. [DOI] [PubMed] [Google Scholar]
- 19.Pagoto S, Schneider K, Oleski J, Lucani I, Bodenlos J, Whited M. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity. 2012;20:1234–9. doi: 10.1038/oby.2011.140. [DOI] [PubMed] [Google Scholar]
- 20.Flegal K, Carroll M, Ogden C, Curtin L. Prevalence and trends in obesity among U.S. adults, 1999–2008. Jama. 2010;3003:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 21.Farley RL, Wade TD, Bircmore L. Factors influencing attendance at cardiac rehabilitation among coronary heart disease patients. Eur J Cardiovasc Nurs. 2003;2:205–12. doi: 10.1016/S1474-5151(03)00060-4. [DOI] [PubMed] [Google Scholar]
- 22.Wing RR, Venditi E, Jakicic JM, Polley BA, Lang W. Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care. 1998;21:350–9. doi: 10.2337/diacare.21.3.350. [DOI] [PubMed] [Google Scholar]
- 23.Garaulet M, Perez-Llamas F, Zamora S, Tebart FJ. Weight loss and possible reasons for dropping out of dietary/behavioural programmes in the treatment of overweight patients. J Hum Nutr Diet. 1999:219–27. [Google Scholar]
- 24.Clark MM, Niura R, King TK, Pera V. Depression, smoking, activity level, and health status: pre-treatment predictors of attrition in obesity treatment. Addict Behav. 1996;21:509–13. doi: 10.1016/0306-4603(95)00081-x. [DOI] [PubMed] [Google Scholar]
- 25.Bischof SC, Damms–Machado A, Betz C, Herpetz S, Legenbauer T, Low T. Multicenter evaluation of an interdisciplinary 52-week weight loss program for obesity with regard to body weight, comorbidities and quality of life: a prospective study. Int Obesity. 2012;36:614–24. doi: 10.1038/ijo.2011.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franz MJ, Van Vormer JJ, Crain AL, Boucher JL. Weight-loss outcomes: a systematic review and meta–analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–67. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 27.Anonymous. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 28.Teixera JP, Silva MN, Countinho SR, Palmera AL, Mata J, Viera PN, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity. 2010;18:725–35. doi: 10.1038/oby.2009.281. [DOI] [PubMed] [Google Scholar]
- 29.Seidell JC, Flegal KM. Assessing obesity: classification and epidemiology. Br Med Bull. 1997;53:238–52. doi: 10.1093/oxfordjournals.bmb.a011611. [DOI] [PubMed] [Google Scholar]
- 30.Klein S, Burke LE, Bray GA, Blair S, Allison DB, Pi- Sunyer X, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity and Metabolism. Circulation. 2004;110:2952–67. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 31.American Diabetes Association and National Institute of Diabetes, Digestive, and Kidney Diseases. The prevention or delay of type 2 diabetes. Diabetes Care. 2002;25:742–9. doi: 10.2337/diacare.25.4.742. [DOI] [PubMed] [Google Scholar]
- 32.Rojo-Tivado M, Benito PJ, Atienza D, Rincon E, Calderon FJ. Effects of age, sex, and treatment on weight-loss dynamics in overweight people. Appl Physiol Nutr Metabol. 2013;38:967–76. doi: 10.1139/apnm-2012-0441. [DOI] [PubMed] [Google Scholar]
- 33.Grossi E, Dalle Grave R, Mannucci E, Molinari E, Compare A, Cuzzolaro M, et al. Complexity of attrition in the treatment of obesity: clues from a structured telephone interview. Int J Obesity. 2006;30:1132–7. doi: 10.1038/sj.ijo.0803244. [DOI] [PubMed] [Google Scholar]
- 34.Greenberg I, Stamper MJ, Schwarzfuchs D, Shai I. Adherence and success in long-term weight loss diets: the dietary intervention randomized controlled triala (DIRECT) J Am Coll Nutr. 2009;28:159–68. doi: 10.1080/07315724.2009.10719767. [DOI] [PubMed] [Google Scholar]
- 35.Bautista-Castano I, Molina-Cabrillana J, Montoya-Alonsoc JA, Serra- Majem L. Variables predictive of adherence to diet and physical activity recommendations in the treatment of obesity and overweight, in a group of Spanish subjects. Int J Obesity. 2004;28:697–705. doi: 10.1038/sj.ijo.0802602. [DOI] [PubMed] [Google Scholar]
- 36.Fabricatore AN, Wadden TA, Moore RH, Butryn ML. Predictors of attrition and weight loss success: results from a randomized controlled trial. Behav Res Ther. 2009;47:685–91. doi: 10.1016/j.brat.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]