Abstract
Objective
The Social Communication Questionnaire (SCQ) is a valid and reliable 40-item scale used to assess pervasive developmental disorders (PDDs). The aim of this study was to determine the validity and reliability of the SCQ-Turkish Form (SCQ-TF).
Materials and Methods
The study included 100 children and adolescents aged 4-18 years; 50 were diagnosed as PDD and 50 were diagnosed with intellectual disability (ID) based on DSM-IV-TR criteria. The consistency, test-retest reliability, content validity, and discriminant validity of SCQ-TF for the groups in the study sample were evaluated. SCQ-TF was compared to the Childhood Autism Rating Scale (CARS), Autism Behavioural Checklist (ABC), and Clinical Global Impression-Severity of Illness (CGI-SI). The most appropriate SCQ-TF cut-off point was determined via ROC analysis.
Results
The 4-factor structure of SCQ-TF accounted for 43.0% of the observed total variance. Correlations between SCQ-TF and the other measures were significant. The Cronbach's alpha value for the SCQ-TF total score was 0.80. The intraclass correlation coefficient (ICC) varied between 0.87 and 0.96, and the cut-off point was 15.
Conclusion
The findings show that SCQ-TF is valid and reliable for use in Turkey in those aged 4-18 years.
Keywords: Pervasive developmental disorder, social communication questionnaire, validity, reliability
Introduction
Autism is neurodevelopmental disorder of early childhood characterized by impaired social skills and communication, accompanied by interfering repetitive stereotypical behaviors. Autism can also manifest with restricted interests and functionality, resulting in lifelong negative consequences (American Psychiatric Association 2000). Autistic disorders are classified as pervasive developmental disorders (PDDs) based on DSM-IV-TR diagnostic criteria. Other PDDs include Asperger's syndrome, childhood disintegrative disorder, Rett syndrome, and PDD-not otherwise specified. PDDs are diagnosed based on a reliable developmental history and description of symptoms provided by parents, and direct clinical observation.
Early diagnosis and treatment of PDDs are crucial in terms of prognosis. Appropriate screening scales that provide specific and sensitive data are of vital importance, as they facilitate early diagnosis (Volkmar et al. 2005; Fred et al. 2002). The Childhood Autism Rating Scale (CARS), Autism Behavior Checklist (ABC), and Social Communication Questionnaire (SCQ) can each be used for screening and to determine the severity of symptoms (Volkmar et al. 2005). In Turkey CARS (İncekaş 2009; Sucuoğlu et al. 1996) and ABC (Yılmaz Irmak et al. 2007) have been standardized, while SCQ was standardized for children aged 18-60 months by Öner et al. (2012).
SCQ, previously known as the Autism Screening Questionnaire, is a screening tool developed by Michael Rutter and Catherine Lord that is completed by the primary caregivers of children suspected to have a PDD. It was originally designed as a companion screening measure for the Autism Diagnostic Interview-Revised (ADI-R) (Couteur et al. 2003), which is accepted as the gold standard for diagnosing autism, but which requires at least 2.5 h to complete. The 40-item SCQ was based on ADI-R and is administered to primary caregivers. SCQ was designed for use in those aged ≥4 years and with a mental age ≥2 years. Presumed malfunctioning in 3 main domains of autism disorder (AD) are assessed: social responsiveness, verbal communication, and restricted repetitive stereotyped behaviors. There are 2 versions of SCQ: Lifetime and Current. The former assesses a child's entire developmental history, whereas the latter assesses a child's behavior during the previous 3-month period. The SCQ is useful for the evaluation of treatment plans and educational interventions. The SCQ items assess social responsiveness, verbal communication, and restricted repetitive stereotyped behaviors, and are based on DSM-IV PDD criteria. The items can generally be completed by a child in <10 min and scored by a clinician in under 5 min. The validity and reliability of SCQ was originally reported by Berument et al. (Rutter et al. 2007; Berument et al. 1999).
The most important use of SCQ is for identify individuals that require additional assessment for a PDD; nonetheless, SCQ can also be used to determine the severity of PDD symptoms in those with other medical conditions, including developmental language disorder, Fragile X, tuberous sclerosis, and Down syndrome. Re-administration of SCQ at regular intervals can be used to monitor variations in PDD symptom severity over time (Rutter et al. 2007). The present study aimed to determine the validity, reliability, and cutoff score of the SCQ-Turkish Form (SCQ-TF) for use in 4-18 year-olds in Turkey.
Materials and Methods
Sample
The study group included 50 children and adolescents aged 4-18 years that were diagnosed according to DSM-IV-TR diagnostic criteria, as follows: AD (n = 41); PDD-not otherwise specified (n = 6); Asperger's syndrome (n = 1); Rett syndrome (n = 1); childhood disintegrative disorder (n = 1). The control group included 50 children and adolescents aged 4-18 years that were diagnosed as intellectual disability (ID) according to DSM-IV-TR diagnostic criteria or lagged behind their peers by 30% in overall development based on the Ankara Development Screening Inventory (AGTE), and those that were not diagnosed with PDD or any of its symptoms based on CARS and ABC.
Developmental assessment in 8 of the control patients aged <6 years was performed using AGTE. Among the 42 controls aged ≥6 years, 33 had mild ID (WISC-R IQ total intelligence score 50-70), 6 had moderate ID (WISC-R IQ total intelligence score 35-49), and 3 had serve ID (WISC-R IQ total intelligence score <35). Mean age of the entire study population was 116.44 ± 45.24 months and 16 (16%) were female and 84 (84%) were male.
Data Collection Tools
Social Communication Questionnaire (SCQ)
SCQ is a 40-item parent-report screening tool that assesses the symptomatology associated with PDDs. Each yes/no item (scored as 1 or 0, respectively) indicates whether or not developmentally inappropriate behaviors exist. The first item concerns whether a child is able to speak using phrases or short sentences and is not scored. The SQC total score range is 0-39. The first 19 items assess general behaviors, whereas the last 20 items assess behaviors that occur between the ages of 4 and 5 years. The recommended cutoff score for a PDD is ≥15 (Rutter et al. 2007; Berument et al. 1999).
Childhood Autism Rating Scale (CARS)
CARS is a 15-item behavioral rating scale developed to differentiate between intellectually disabled children with and without autism syndrome. It is especially effective for differentiating autistic children from educable intellectually disabled children. CARS scores can be used to determine the clinical severity of autism as mild-moderate or moderate-severe. Each item is scored between 1 and 4, but midpoint scores of 1.5, 2.5, and 3.5 are also used (Schopler et al. 2007). CARS total score ranges from 15 to 60, and are classified, as follows: 15-29.5: not autistic; 30-36.5: mild-moderate autism; 37-60: severe autism (Mesibov et al. 1989; Garfin et al. 1988; Robert et al. 1988).
CARS was adapted for use in Turkey by Sucuoğlu et al. (1996), and was reported to be valid and reliable by İncekaş (2009). In the present study its Cronbach's alpha coefficient was 0.95. The reliability correlation coefficient amongst evaluators was 0.98. The criterion-related validity was determined via comparison with ABC and CGI-SI. The correlation coefficient between CARS, and ABC and CGI-SI was 0.67 and 0.873, respectively. The cutoff score for the Turkish form was calculated as 30. It was shown by İncekaş (2009) that CARS-Turkish form accurately differentiates intellectually disabled children with and without autism (P < 0.001).
Autism Behavior Checklist (ABC)
ABC is a 57-item assessment tool comprised of the following 5 subscales: sensory, relating, body and object use, language skills, and social and self-help. ABC total score ranges from 0 to 159 (Krug et al. 1993). Yılmaz Irmak et al. (2007) reported that the Turkish version of ABC was valid and reliable for use in Turkey. The cutoff score for the Turkish form is 39.
Clinical Global Impression-Severity of Illness (CGI- SI) Scale
CGI-SI is an observer-rated scale used to assess patients for clinical research purposes and to monitor changes associated with therapy during the monitoring period. CGI-SI is composed of 3 subscales focused on the severity of illness, recovery, and the severity of adverse effects (Guy 1976). In the present study, only the severity of illness subscale (Severity Index-SI) was used.
Sociodemographic Data Form
A sociodemographic data form was used to collect the following data; date of birth, history of birth, birth order (in instances of multi-child families), school attendance, academic performance, peer relationships, and developmental history. The form was also used to collect parental data, including level of education, occupation, number of children, and history of physical and mental illness.
Data Collection
With the permission of Western Psychological Institute, SCQ's legal owner of rights, the scale was translated and back translated independently by 3 experts on mental retardation, autism, and translation. The original SCQ was modified for use in 4-18-year-olds. The resulting translation was compared with that reported by Öner et. al (2012) for use in 0-6-year-olds and its compatibility was thus ascertained.
The participants were diagnosed by a clinician based on DSM-IV-TR criteria. The sociodemographic data form was completed in the case of all participants. The mothers of the participants self completed the SCQ-TF and ABC. After completing the scales the mothers were asked if there were any items they didn`t understand. CGI-SI and CARS were administered by a clinician. SCQ-TF was re-administered 60 ± 10 d after initial administration to determine the scale's test-retest reliability.
Data Evaluation
SPSS v.15.0 for Windows was used for statistical evaluation of the data. The level of statistical significance was set at P < 0.05. Because some questions of the SCQ include positive expressions while some include negative expressions and for the purpose of changing these questions with different inclinations into the same style, a syntax file was formed and the answers were transformed into the same direction. In order to assess the reliability of SCQ-TF, alpha values, item-total correlations, and test-retest reliability were calculated using the Kuder-Richardson reliability coefficient (KR20) as a measure of internal consistency. Factor analysis was conducted to determine the construct validity of SCQ-TF. In order to assess the dataset's conformity with factor analysis, correlations between variables were checked via the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Barlett's Test. In order to explore the factor structure of SCQ-TF data were subjected to principal component analysis, according to Kaiser Normalization and varimax rotation. Additionally, correlations between SCQ-TF items were analyzed. The validity of SCQ-TF was determined via comparison of SCQ-TF scores with CGI-SI, CARS, and ABC scores using Pearson's correlation coefficient. The most appropriate SCQ-TF cutoff score was obtained via additional ROC analysis, which was performed to calculate the scale's sensitivity, specificity, and negative and positive predictive values. The scale's content validity was analyzed via comparison of SCQ-TF total scores in the study and control groups using the independent samples t test.
Results
The distribution of genders in the study and control groups was the same; each group included 8 females (16%) and 42 males (84%). Mean age in the 2 groups did not differ significantly (study group: 116.44 ± 45.24 months; control group: 117.46 ± 45.53 months; t = 0.112; P = 0.911). Mean mothers' level of education in the study group was 10.64 ± 4.04 years, versus 7.24 ± 3.22 in the control group; the difference was significant (P < 0.000).
Reliability Findings
Reliability was determined via internal consistency and test-retest measurements. Because SCQ-TF uses a binary form of response, to test its internal consistency Kuder & Richardson 20,21 was used and Cronbach's alpha values were computed accordingly, as shown in Table 1. The correlation between domain items and domain total score was 0.22-0.60 for the reciprocal social interaction domain, 0.22-0.66 for the communication domain, and 0.25-0.57 for the restricted repetitive and stereotyped behaviors domain. Item and item total correlations ranged between 0.22 and 0.66. Cronbach's alpha values were between 0.729 and 0.834 when each item was excluded.
Table 1. Correlation between item and total scores, Cronbach's alpha values after dropping non-significant items, and internal consistency of SCQ-TF.
| SCQ-TF | Correlations Between Items and Total Score | Cronbach's Alpha Value after Dropping Nonsignificant Items | Internal Consistency (Cronbach's alpha value) |
|---|---|---|---|
| Reciprocal Social Interaction Domain | 0.83 | ||
| 9. Inappropriate facial expression | .221 | .834 | |
| 10. Use of other's body to communicate | .305 | .831 | |
| 19. Friends | .351 | .828 | |
| 26. Eye gaze | .370 | .827 | |
| 27. Social smiling | .463 | .822 | |
| 28. Showing and directing attention | .537 | .816 | |
| 29. Offering to share | .465 | .821 | |
| 30. Seeking to share enjoyment | .517 | .817 | |
| 31. Offering comfort | .546 | .815 | |
| 32. Quality of social overtures | .417 | .824 | |
| 33. Range of facial expression | .447 | .822 | |
| 36. Interest in children | .466 | .821 | |
| 37. Responses to other children | .568 | .814 | |
| 39. Imaginative play with peers | .501 | .818 | |
| 40. Group play | .601 | .811 | |
| Communication Domain | 0.78 | ||
| 2. Conversation | .259 | .785 | |
| 3. Stereotyped utterances | .545 | .758 | |
| 4. Inappropriate questions | .289 | .783 | |
| 5. Pronoun reversal | .344 | .777 | |
| 6. Neologisms | .229 | .788 | |
| 20. Social chat | .405 | .772 | |
| 21. Imitation | .257 | .785 | |
| 22. Pointing to express interest | .467 | .767 | |
| 23. Gestures | .222 | .789 | |
| 24. Nodding to mean yes | .664 | .746 | |
| 25. Head shaking to mean no | .625 | .750 | |
| 34. Imitative social play | .605 | .752 | |
| 35. Imaginative play | .483 | .764 | |
| Restricted, Repetitive, and Stereotyped Patterns of Behavior Domain | 0.77 | ||
| 7. Verbal rituals | .495 | .744 | |
| 8. Compulsions and rituals | .484 | .745 | |
| 11. Unusual preoccupations | .541 | .736 | |
| 12. Repetitive use of objects | .574 | .729 | |
| 13. Circumscribed interests | .256 | .784 | |
| 14. Unusual sensory interests | .432 | .754 | |
| 15. Hand and finger mannerisms | .484 | .746 | |
| 16. Complex body mannerisms | .527 | .738 | |
| SCQ Total Score | 0.89 |
For the SCQ-TF total score and for such factors as reciprocal social interaction, communication, and restricted repetitive and stereotyped behaviors the intraclass correlation coefficient (ICC) values that were computed in order to assess test-retest reliability were between 0.87 and 0.96, and all were statistically significant (P < 0.0001).
Validity Findings
The Kaiser-Meyer-Olkin value, which was used to assess the data set's conformity value, which was used to assess the data set's conformity with factor analysis, was 0.65 and based on Barlett's Test (P = 0,000) was significant; therefore, the data set was determined to comply with factor analysis. Principal components analysis of all factors showed that 13 factors, which accounted for 73.3% of the distribution whose self-value statistics, was higher than 1 were found; however, except for 4 factors(reciprocal social interaction, communication, abnormal language and stereotyped repetitive behaviors), it was seen that in all the other factors, there were one or two items, which were also common items that have factor loadings in other items. Because of an easier and more meaningful interpretation compatible with its 3-dimensional structure of the scale, 4 factors accounted for 43% of the distribution with self-values higher than 1 according to varimax rotation were included in the evaluation; these factors were reciprocal social interaction, communication, abnormal language and stereotyped repetitive behaviors respectively (Table 2).
Table 2. SCQ-TF factor loadings and communalities.
| Factor 1: Social Interaction | Factor 2: Communication | Factor 3: Abnormal Language | Factor 4: Stereotyped Behavior | Communalities | ||
|---|---|---|---|---|---|---|
| Item 28 | (S) | .768 | .788 | |||
| Item 31 | (S) | .610 | .662 | |||
| Item 36 | (S) | .605 | .750 | |||
| Item 20 | (C) | .598 | .745 | |||
| Item 22 | (C) | .597 | .417 | .695 | ||
| Item 21 | (C) | .584 | .607 | |||
| Item 32 | (S) | .578 | .764 | |||
| Item 39 | (S) | .574 | .717 | |||
| Item 35 | (C) | .546 | .734 | |||
| Item 40 | (S) | .534 | .507 | .740 | ||
| Item 37 | (S) | .508 | .744 | |||
| Item 27 | (S) | .494 | .685 | |||
| Item 34 | (C) | .494 | .456 | .800 | ||
| Item 33 | (S) | .477 | .602 | |||
| Item 12 | (R) | .670 | .586 | |||
| Item 4 | (C) | .626 | .764 | |||
| Item 3 | (C) | .615 | .823 | |||
| Item 11 | (R) | .607 | .720 | |||
| Item 6 | (C) | .599 | .786 | |||
| Item 7 | (R) | .570 | .381 | .758 | ||
| Item 8 | (R) | .556 | .284 | .842 | ||
| Item 13 | (R) | .527 | .420 | .684 | ||
| Item 15 | (R) | .419 | .418 | .693 | ||
| Item 14 | (R) | .410 | .321 | .672 | ||
| Item 38 | (–) | .252 | .386 | .245 | .698 | |
| Item 26 | (S) | .377 | .771 | |||
| Item 2 | (C) | .565 | .730 | |||
| Item 17 | (–) | .563 | .781 | |||
| Item 19 | (S) | .562 | .616 | |||
| Item 10 | (S) | .522 | .748 | |||
| Item 18 | (–) | .510 | .307 | .641 | ||
| Item 5 | (C) | .503 | .677 | |||
| Item 16 | (R) | .372 | .436 | .741 | ||
| Item 23 | (C) | .399 | .404 | .382 | .706 | |
| Item 30 | (S) | .262 | .567 | .782 | ||
| Item 24 | (C) | .371 | .558 | .895 | ||
| Item 25 | (C) | .446 | .522 | .881 | ||
| Item 29 | (S) | .299 | .395 | .400 | .759 | |
| Item 9 | (S) | .349 | .820 |
S: Reciprocal social interaction domain; C: communication domain; R: restricted, repetitive, and stereotyped patterns of behavior domain; –: not in algorithm
Communality is the level of variance a variable shares with all the other variables analyzed. The highest variance was for the SCQ-TF's 24th item (0.89) (nodding to mean yes) and the lowest variance was for the 12th item (0.58) (repetitive use of objects) (Table 2). There was a moderately significant correlation between SCQ-TF total score, and CARS total score (r = 0.35, P < 0,05), CGI-SI total score (r = 0.35, P < 0.05), and ABC total score (r = 0.46, P < 0.01).
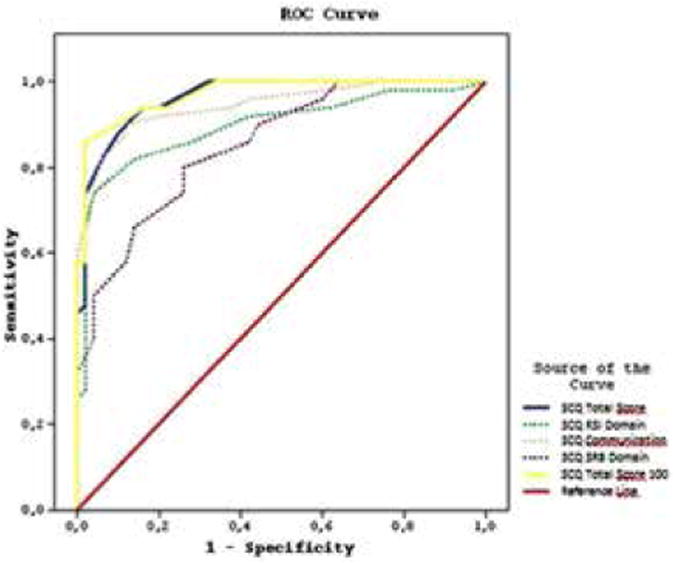
The results of ROC analysis used to determine the SCQ-TF cutoff score for differentiating between autism and intellectual disability are presented in Figure 1. The area under the curve was determined to be 96% for the SCQ-TF total score (reliability range: 0.93-0.99; P < 0,0001), 89% for the reciprocal social interaction domain (reliability range: 0.83-0.96; P < 0,0001), 94% for the communication domain (reliability range: 0.90-0.98; P < 0,0001), and 85% for the restricted repetitive stereotyped behaviors domain (reliability range: 0.78-0.92; P < 0,0001). The most appropriate sensitivity (0.94) and specificity (0.84) values for the SCQ-TF total score were obtained for the cutoff score of 14.5. According to AD diagnosis, the sensitivity of the scale was 100% and its specificity as 33.3%. The positive predictive value for AD in the study group was 0.87, whereas the negative predictive value was 1. For the diagnosis of PDD the sensitivity and specificity of SCQ-TF were 94% and 100%, respectively. Evaluation of the entire study population showed that the positive predictive value for PDD was 1 and the negative predictive value was 0.94.
Figure 1.
Discussion
Reliable and valid screening tools are required for early diagnosis and treatment of PDDs. The primary aim of the present study was to determine if SCQ-TF was valid and reliable for use in 4-18-year-olds in Turkey by researchers and clinicians. By assessing the internal consistency of the scale it is tried to identify whether a desired feature can be measured thoroughly. A high internal consistency coefficient is important, as the items used for the measurement are indicators that they measure a homogenous structure. SCQ-TF was found strongly reliable, in reciprocal social interaction and SCQ-TF total score, whereas it was found fairly reliable in communication and restricted repetitive stereotyped behaviors. SCQ-TF is not homogenous, as its communication domain includes items related to abnormal language and communication. The communication domain items do not coincide with each other enough which may have had a negative effect on the internal consistency of the scale's communication domain.
As in the present study, Öner et al. (2012) observed that the SCQ-TF was strongly reliable in terms of the reciprocal social interaction domain and total score, whereas it was fairly reliable in terms of the communication and restricted repetitive stereotyped behavior domains.
In Öner et al.'s (2012) study the correlation between the communication domain items and total score was quite low when their SCQ-TF was administered to 0-6-year-olds. In their study more than 80% of the autistic children aged 0-6 years didn't acquire the ability to speak; children without the ability to speak automatically receive a score of 0 for the SCQ communication domain, which has no effect on total score. In the present study 75% of the sample had acquired the ability to speak and the correlation between the SCQ-TF communication domain items and total score was high (0.222-0.664).
In patients with PDDs stereotyped behaviors and restricted interests progress in severity with age. The frequency of these behaviors increase after age 3 years in PDD (Stone et al. 1999). Among the pre-school age group, the Cronbach's alpha value for the SCQ-TF stereotyped behaviors and restricted interests domain was reported to be 0.68 (Öner et al. 2012). The PDD patients in the present study were older. The Cronbach's alpha value for the SCQ-TF stereotyped behaviors and restricted interests domain in the present study was 0.77, which is similar to earlier reports. SCQ-TF can identify stereotyped behaviors and restricted interests with higher internal consistency in older age groups.
Analysis of the construct validity of SCQ-TF was carried out in the present study using principal components analysis. Following varimax rotation, factor analysis was performed for the 4 factors that accounted for 43.0% of the distribution with Eigen values were >1: reciprocal social interaction, communication, abnormal language, and restricted stereotyped repetitive behavior. In Öner et al.'s (2012) study of the SCQ for 0-6-year-olds principle component analysis, followed by varimax rotation, showed that 3 factors accounted for 41% of the total variance: communication, reciprocal social interaction, and stereotyped behavior and restricted interests.
Berument et al.'s (1999) original standardization study of SCQ also reported a 4-factor structure based on principle component analysis that explained 42.4% of the total variance: social interaction, communication, abnormal language, and stereotyped behavior. In the factor analysis of the SCQ for 0-6-year-olds the abnormal language factor was excluded, which differs from both the present study and the original standardization study by Berument et al.. (1999) The abnormal language domain assesses qualitative deficiencies in language. Perhaps the abnormal language domain was not included in Öner et al.'s (2012) study because the 0-6year-old age group range is rather young for language development and the high percentage of children in their study that were unable to speak.
One of the methods used to assess a scale's validity is criterion validity. With convergent validity, which is a part of criterion validity, the correlation coefficient between the scale being analyzed and another scale with higher validity also measuring the same property is compared. In order to contribute to the criterion validity of the SCQ-TF mean CGI-SI, CARS, and ABC scores for the mothers of the study group patients, were compared to the SCQ-TF mean score. The correlation between SCQ-TF, and CARS, CGI-SI, and ABC might have been low in the present study because of differences in the scales' scoring methods (binary versus Likert-type) and assessment methods (clinician observation versus caregiver assessment).
In the present study the sensitivity and specificity of SCQ-TF for diagnosing AD were 100% and 33.3%, respectively, versus 94% and 100%, respectively, for diagnosing PDD. The specificity value of SCQ-TF in terms of identifying AD, that is, the scale's power to identify the true healthy individuals among the healthy ones was lower in the present study than noted in other studies, indicating that there was a high number of false positive cases. Berument et al. (1999) reported that SCQ's ability to differentiate AD from other PDDs was low, whereas its ability to differentiate PDD and ID from non-PDD cases was quite high. They also reported that SCQ's ability to differentiate AD from other PDDs was low, whereas its ability to differentiate PDD from non-PDD cases was high.
In the present study the study and control groups were more homogenous than those in earlier studies. The control group included only patients with ID, whereas in other studies control groups were more heterogeneous, with fewer patients diagnosed as ID than as PDD (Norris and Lecavalier 2010; Snow and Lecavalier 2008; Allen et al. 2007; Corsello et al. 2007; Lee et al. 2007; Wigging et al. 2007; Witwer and Lecavalier 2007; Eaves et al. 2006a, 2006b; Wigging et al. 2006; Berument et al. 1999). The present study's control group consisted of only those diagnosed as ID because it is possible that some individuals with ID might also have impaired social interactions, communication, and language skills, and repetitive behaviors. Use of such a homogenous control group made it possible to compare the SCQ-TF with a control group in terms of harder to diagnose PDD.
The area under the curve as a result of the ROC analysis by Berument et al. (1999) was 92% for the SCQ total score, 90% for the reciprocal social interaction domain, 83% for the communication domain, and 70% for the restricted repetitive stereotyped behaviors domain. When the cutoff score for the SCQ total score was taken as 15, the scale's sensitivity was 0.85, specificity was 0.75, positive predictive value was 0.93, and negative predictive value was 0.55. As a result of the ROC analysis used to determine the cutoff score for the SCQ-TF in the present study, the area under the curve was 96% for the total score; in other words, the scale correctly classified PDD and ID patients with an estimated accuracy of ≤96%. Just as in Berument et al.'s (1999) study, in the present study the SCQ-TF total score differentiated PDD from ID successfully. When the cutoff score for SCQ-TF was determined, the sensitivity and specificity values were expected to be high.
As sensitivity increases the correct positive rate increases, whereas as specificity increased the false positive rate decreases. For SCQ its sensitivity represents the degree to which it can differentiate those that exhibit the characteristics typical of autism from those that don't. High sensitivity causes non-autistic people that exhibit the signs typical of autism to be diagnosed with autism. Specificity serves the purpose of differentiating those with autism from those that exhibit the signs typical of autism. High specificity causes a poor distinction between those who have clues characteristic to autism and those who are diagnosed as so in the population. As SCQ is a screening tool, it is important that it identify those that exhibit characteristics specific to autism, but do not meet the diagnostic criteria because if an individual is mistakenly diagnosed with autism it is possible that the diagnosis will be corrected during subsequent assessments; however, if an autistic individual is not diagnosed as autism the treatment process will likely be delayed.
Because sensitivity is thought to be more important that specificity, in the present study the cutoff score was accepted as 14.5, which indicates high sensitivity. This cutoff score with relevant sensitivity (0.94) and specificity (0.80) values is considered to be fairly good for a screening instrument. A cutoff score of 14.5 was also recommended for the SCQ-TF for 0-6-year-olds (Öner et al. 2012). Similar sensitivity and specificity values for the SCQ-TF have been observed in those of 0-6-year-olds and those aged 4-18 years. The cutoff score for SCQ-TF obtained in the present study is compatible with the cutoff score (15) originally reported by Berument et al. (1999).
Limitations
The present study has some limitations. Firstly, the number of participants was insufficient for conducting factor analysis of SCQ-TF; a larger study sample would have increased the statistical power of the findings. Evaluation of SCQ-TF's factor analysis in a larger sample is required. Secondly, the mothers of the patients in the study group had significantly more years of education than the control group mothers; however, to prevent this educational difference between the mothers from causing a difference in the comprehension of the scales' items, each mother was asked whether there were any scale items they didn't understand, and when necessary an experienced clinician provided explanations. Lastly, none of the participants was aged <4 years, which might limit the generalizability of the study's findings.
Conclusion
Autism is a disorder that affects the individual and the family throughout their lives and also causes significant loss of important mental abilities. The prevalence of autism has been increasing for the last twenty years and standardized autism screening and diagnosis tools are needed in Turkey. The present study aimed to meet the needs in this area by determining the validity and reliability of the SCQ-TF. The SCQ-TF for 0-6-year-olds was reported to be valid and reliable for use in Turkey (Öner et al. 2012), and its validity and reliability for those aged 4-18 years was demonstrated in the present study.
The SCQ is considered to be a valid and reliable assessment instrument used for screening in many countries (Norris and Lecavalier 2010), and can be used to screen for autism, with regard to its help in distinguishing autism, being easy and applicable in short time, usability in areas like planning and evaluating education, and ability of assessment in different areas of development.
Acknowledgments
We thank Associate Professor Özgür Öner for his translation of SCQ into Turkish and subsequent corrections, which were invaluable to the present study.
References
- Allen CW, Silove N, Williams K, et al. Validity of the Social Communication Questionnaire in Assessing Risk of Autism in Preschool Children with Developmental Problems. J Autism Dev Disord. 2007;37:1272–8. doi: 10.1007/s10803-006-0279-7. [DOI] [PubMed] [Google Scholar]
- Köroğlu E, editor. Amerikan Psikiyatri Birliği. Psikiyatride Hastalıkların Tanımlanması ve Sınıflandırılması Elkitabı, Yeniden Gözden Geçirilmiş Dördüncü Baskı (DSM-IV-TR) Hekimler Yayın Birliği; Ankara: 2000. 2007. [Google Scholar]
- Berument K, Rutter M, Lord C, et al. Autism Screening Questionnaire: Diagnostic Validity. Br J Psychiatry. 1999;173:444–51. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- Corsello C, Hus V, Pickles A, et al. Between a ROC and a hard place:decisions about using the SCQ. Jounal of Child Psychology and Psychiatry. 2007;48:932–40. doi: 10.1111/j.1469-7610.2007.01762.x. [DOI] [PubMed] [Google Scholar]
- Couteur AL, Lord C, Rutter M. Autism Diagnostic Interview-Revised. Western Psychological Service; 2003. [Google Scholar]
- Eaves L, Wingert H, Ho H. Screening for autism. Autism. 2006a;10:229–42. doi: 10.1177/1362361306063288. [DOI] [PubMed] [Google Scholar]
- Eaves L, Wingert H, Ho H, et al. Screening for Autism Spectrum Disorders with the Social Communication Questionnaire. Developmental and Behavioral Pediatrics. 2006b;27:95–103. doi: 10.1097/00004703-200604002-00007. [DOI] [PubMed] [Google Scholar]
- Garfin DG, Mc Callon D, Cox R. Validity and relaibility of the childhood autism rating scale with autistic adolescents. J Autism Dev Disord. 1988:367–78. doi: 10.1007/BF02212193. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville: National Institude of Mental Health; 1976. pp. s.76–338. Revised US Dept Health, Education and Welfare publication (ADM) [Google Scholar]
- İncekaş S. Yayınlanmamış Tıpta Uzmanlık Tezi. Dokuz Eylül Üniversitesi Tıp Fakültesi; 2009. Çocukluk Otizmini Derecelendirme Ölçeği Geçerlik ve Güvenirlik Çalışması. [Google Scholar]
- Krug DA, Arick JR, Almond PA. Autism Screening Instrument for Educational Planning. Second. Pro-ed Inc; Austin, Texas: 1993. [Google Scholar]
- Lee L, David A, Rusyniak J, et al. Performance of the Social Communication Questionnaire in children receving preschool special education services. Research in Autism Spectrum Disorders. 2007;1:126–38. [Google Scholar]
- Mesibov G, Schopler E, Schaffer B, et al. Use of childhood autism rating scale with autistic adolescents and adults. J Am Acad Child Adolesc Psychiatry. 1989;28:538–41. doi: 10.1097/00004583-198907000-00012. [DOI] [PubMed] [Google Scholar]
- Norris M, Lecavalier L. Screening Accuracy of Level 2 Autism Spectrum Disorder Rating Scales. Autism. 2010;14:263–84. doi: 10.1177/1362361309348071. [DOI] [PubMed] [Google Scholar]
- Öner P, Öner Ö, Çöp E, et al. Sosyal İletişim Ölçeğinin Okul Öncesi Çocuklardaki Geçerlik ve Güvenirliği. Klinik Psikofarmakoloji Bülteni. 2012;22:43–50. doi: 10.5455/bcp.20111212091514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert J, Reichler RJ, Rochen Renner B, et al. Practice DVD on Using the CARS. Western Psychological Services; 1988. [Google Scholar]
- Rutter M, Bailey A, Lord C. The Social Communication Questionnaire (SCQ), second printing. Western Psychological Services; 2007. [Google Scholar]
- Schopler E, Reichler RJ, Rochen Renner B. The Childhood Autism Rating Scale (CARS), 11 Baskı. Western Psychological Services; 2007. [Google Scholar]
- Snow A, Lecavalier L. Sensitivity and specificity of the Modified Checklist for Autism in Toddlers and the Social Communication Questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism. 2008;12:627–44. doi: 10.1177/1362361308097116. [DOI] [PubMed] [Google Scholar]
- Sucuoğlu B, Öktem F, Akkök F, et al. Otistik Çocukların Değerlendirilmesinde Kullanılan Ölçeklere İlişkin Bir Çalışma. 3P Dergisi. 1996;4:116–21. [Google Scholar]
- Stone WL, Lee EB, Ashford L, et al. Can autism be diagnosed accurately in children under 3 years? J Child Psychol Psychiatry. 1999;40:219–26. [PubMed] [Google Scholar]
- Volkmar Fred R, Klin A. Issues in the Classification of Autism and Related Conditions. In: Volkmar Fred R, Paul R, Klin A., editors. Handbook of Autism and Pervasive Developmental Disorders, Volume 1: Diagnosis, Development, Neurobiology, and Behavior. 3rd. John Wiley & Sons, Incorporated; 2005. pp. s.5–42. [Google Scholar]
- Volkmar Fred R, Lord C, Klin A, et al. In: Autism and the Pervasive Developmental Disorders Chapter 46, Child and adolescent psychiatry, a comprehensive textbook. Lewis M, editor. Lippincott Williams and Wilkins; Baltimore: 2002. [Google Scholar]
- Wigging LD, Baio J, Rice C. Examination of the time between first evaluation and first autism spectrum diagnosis in a population-based sample. Developmental and Behavioral Pediatrics. 2006;27:79–87. doi: 10.1097/00004703-200604002-00005. [DOI] [PubMed] [Google Scholar]
- Wigging LD, Bakeman R, Adamson LB, et al. The utility of the Social Communication Questionnaire in screening for autism in children referred for early intervention. Focus on Autism and Developmental Disabilities. 2007;22:33–8. [Google Scholar]
- Witwer A, Lecavalier L. Autism screening tools: An evaluation of Social Communication Questionnaire and the Developmental Behaviour Checklist-Autism Screening Algorithm. Journal of Intellectual and Developmental Disability. 2007;32:179–87. doi: 10.1080/13668250701604776. [DOI] [PubMed] [Google Scholar]
- Yılmaz Irmak T, Tekinsav Sütçü S, Aydın A, et al. Otizm Davranış Kontrol Listesinin (ABC) Geçerlik ve Güvenirliğinin İncelenmesi. Çocuk ve Gençlik Ruh Sağlığı Dergisi. 2007;14 [Google Scholar]


