Summary
Background
More than 2 billion people are unable to receive surgical care based on operating theatre density alone. The vision of the Lancet Commission on Global Surgery is universal access to safe, affordable surgical and anaesthesia care when needed. We aimed to estimate the number of individuals worldwide without access to surgical services as defined by the Commission’s vision.
Methods
We modelled access to surgical services in 196 countries with respect to four dimensions: timeliness, surgical capacity, safety, and affordability. We built a chance tree for each country to model the probability of surgical access with respect to each dimension, and from this we constructed a statistical model to estimate the proportion of the population in each country that does not have access to surgical services. We accounted for uncertainty with one-way sensitivity analyses, multiple imputation for missing data, and probabilistic sensitivity analysis.
Findings
At least 4·8 billion people (95% posterior credible interval 4·6–5·0 [67%, 64–70]) of the world’s population do not have access to surgery. The proportion of the population without access varied widely when stratified by epidemiological region: greater than 95% of the population in south Asia and central, eastern, and western sub-Saharan Africa do not have access to care, whereas less than 5% of the population in Australasia, high-income North America, and western Europe lack access.
Interpretation
Most of the world’s population does not have access to surgical care, and access is inequitably distributed. The near absence of access in many low-income and middle-income countries represents a crisis, and as the global health community continues to support the advancement of universal health coverage, increasing access to surgical services will play a central role in ensuring health care for all.
Funding
None.
Introduction
The vision of the Lancet Commission on Global Surgery1 of universal access to safe, affordable surgical care when needed supports the notion that access to surgical care and access to health care are synonymous. Although health-care delivery is a complex enterprise with many interconnected parts, there are four essential components: the staff who do the work, the equipment with which they work, the space they work in, and the systems that help the staffand the equipment work together in a shared space.2
However, evidence and anecdote suggest that the availability of the so-called staff, stuff, space, and systems of surgical care delivery is limited in many, if not most, low-resource settings.3–5 For example, an assessment of operating theatre density showed that 90% of the population of sub-Saharan Africa has access to roughly one operating theatre per 100 000 people.4 The few theatres that do exist have limited capacity to provide safe surgical care. For instance, up to 70% lack pulse oximetry, an anaesthetic monitoring standard.4 Even when adequate surgical capacity and robust safety mechanisms exist, patients in both high-income and low-income settings often confront other barriers to access.6,7 A fully equipped operating theatre serves little purpose for patients who cannot reach the hospital in a timely fashion, or for whom a surgical team is unavailable. Finally, patients who do receive appropriate surgical care often risk impoverishment secondary to out-of-pocket payments.8
Previous estimates have suggested that at least 2 billion people lack access to surgical care based on the density of operating theatres alone.4 We use the more inclusive Commission definition of access, which includes capacity, safety, timeliness, and affordability, and use a mathematical modelling approach to answer the following question: “How many people worldwide lack access to safe, affordable, and timely surgical care?”
Methods
Model construction
We defined access to surgery in a country using four dimensions: timeliness, surgical capacity with respect to workforce and infrastructure, safety, and affordability. Applying these dimensions, we estimated the number of patients worldwide without access to surgical services. Our study population did not include patients who needed surgical services, but identified the population who would not have access to surgical services if needed at any given time. Modelling was done at the country level, and all countries for which the World Bank provides data and for which the necessary data were available were included.
First, we estimated the proportion of the population with access to surgery at the country level. For each country, we used a chance tree to model the probability that an individual had access to surgery (figure 1) with the binary outcome of access (1) or no access (0). Each chance node represents the probability of an access dimension being available to an individual patient conditional on the availability of the preceding dimensions. In view of data for each of these dimensions not being directly available, we used proxies. For baseline results, timeliness was approximated by the proportion of serious injuries transported by an ambulance,9 surgical capacity by the number of surgical procedures under taken in a country as a proportion of the number of surgeries needed to meet demand,3,10 safety by the proportion of operating theatres with pulse oximetry,4 and affordability by the proportion of patients undergoing surgery who are protected from catastrophic expenditure from out-of-pocket payments.8 The appendix provides more detail about each proxy.
Figure 1. Chance tree to assess global access to surgical care.
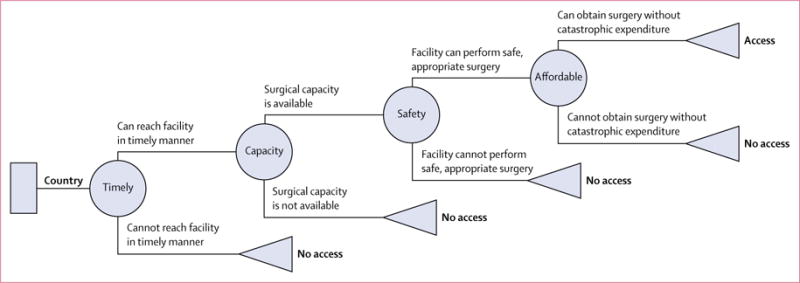
Each chance node represents a dimension of access.
Because the outcome value assigned to no access is zero in our chance tree, the expected value of the chance tree for each country is the joint probability of all four dimensions being available to an individual. The probability of access to surgery in a country, i, can therefore be given by:
where p(A)=probability of access to surgery, p(T)=probability of timely surgical care, p(C)=probability that surgical capacity is available, p(S)=probability that surgery can be delivered in a safe manner, and p(Af)=probability that surgery is affordable (patient does not experience catastrophic expenditure). The ∩ symbol indicates joint probability, and the | symbol indicates conditional probability. For example, p(A∩B) is the joint probability of both event A and B occurring, while p(A|B) is the probability of event A occurring given than event B has occurred. The population without access to surgery in a country is given by:
where NAi=total number of individuals without access to surgery in a country and TPi=total population in a country. The global population without access to surgical care, or NA, is therefore represented by the summation of the country-specific estimates described above:
Because access probably differs between urban and rural populations, we did a secondary analysis in which all four access dimensions are applied to the rural population, but only the probability of catastrophic expenditure and safe surgery was applied to the urban population. The selective application of proxies to the urban population was based on the assumption that timely access and capacity are more likely to be available in a city. Ultimately, assuming that 100% of the urban population can receive surgery quickly, although clearly false, facilitates the creation of a lower-bound estimate for access. Therefore:
where p(A)i,r = probability of access within the rural population and p(A)i,u = probability of access within the urban population. We term this the selective model, and the total global population without access to surgery is given in this model by:
where TPi,r=total rural population and TPi,u=total urban population for each country i. Notably, given that our data originated from countrywide estimates, the selective tree likely underestimates access in rural settings and definitely overestimates access in urban settings. However, we believe it serves as a reasonable lower-bound estimate for the population without access to surgery. 180 countries, representing 6·97 billion people, or 98% of the global population, had data for each proxy readily available. To estimate the global population without access to care, we assumed missingness at random and employed a multiple imputation approach described in the appendix to capture the additional uncertainty of missing data.
Sensitivity analysis
Our baseline results include two sets of assumptions: that the full chance tree is applied to the entire population (full tree), and that all four dimensions are applied to the rural population and only affordability and safety are applied to the urban population (selective tree). To test the robustness of our results, we did several one-way sensitivity analyses. First, baseline assumptions were retested against the exclusion of each dimension of access separately. For example, the first scenario includes capacity, safety, and affordability with timeliness excluded; the second includes timeliness, safety, and affordability with capacity excluded, and so on.
Second, baseline assumptions were tested against different proxies for capacity and affordability. For capacity, our baseline results used an adjustment factor (appendix), to model p(C|T). In a one-way sensitivity analysis, we assumed that p(C|T)=p(C) as an upper-bound, and p(C|T)=min(2*p(C),1·0) as a lower-bound estimate for the population without access to surgical services. We also used results from a model that regresses each country’s surgical procedure rate2 against life-expectancy to establish the optimum procedure rate in the context of life-expectancy, or in other words, the country that achieves the maximum life-expectancy with the minimum-necessary procedure rate (Sweden, in this case).11 The index country’s current surgical procedure rate was taken to be the needed procedure rate (NPR) for all countries. Similar methods were used for under-5 survival (Germany) and maternal survival (Singapore). We also used the definition by Funk and colleagues3 in which countries with less than two operating rooms per 100 000 population were deemed to have no access, with the simplistic yet conservative assumption that those with more than two operating rooms per 100 000 had 100% access to surgical capacity. For affordability, we reran our baseline assumptions with Shrime’s model8 and assumed that out-of-pocket expenditure was a function of only direct medical costs and did not include non-medical costs. Finally, second-order Monte Carlo simulation, with 50 000 draws from the variables (parameterised in appendix) was used to account for parameter uncertainty from our baseline assumptions.
Statistical analysis was done in Excel 2010. Monte Carlo simulation was done with the RiskAmp plugin, and multiple imputation with chained equations was done with the Real Statistics software package for Excel.
Results
Data were readily available to assess surgical access for 180 countries, representing 6·97 billion people (98% of the global population). After accounting for missing data using multiple imputation, our model assessed 196 countries, representing 7·1 billion people. Applying our baseline assumptions, the full tree model estimated that 5·3 billion (95% posterior credible interval [PCI] 5·0–5·5) do not have access to surgical services; the selective tree estimated 4·8 billion (4·6–5·0) (table 1, figure 2). The proportion of the population without access to surgical services varied widely when stratified by World Bank income classification, with the selective tree estimating that 97·7% (95·6–99·5) and 92·3% (89·3–94·5) of the populations in low-income countries and lower-middle-income countries lack access (table 1), compared with 14·9% (11·4–16·3) of the population in high-income countries. We noted a similar pattern when countries were stratified by the Institute for Health Metrics and Evaluation’s global burden of disease regions:12 the selective model estimates that greater than 95% of the population in south Asia and central, eastern, and western sub-Saharan Africa do not have access to care, whereas less than 5% of the population in Australasia, high-income North America, and western Europe lack access to surgery (table 2, figures 3 and 4).
Table 1.
Total assessed population and proportion without access to surgery by World Bank income classification
| Total population (millions) | Full tree | Selective tree | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Population with no access (millions) | 95% posterior CI | Proportion with no access | 95% posterior CI | Population with no access (millions) | 95% posterior CI | Proportion with no access | 95% posterior CI | ||
| High income | 1306 | 344 | 290–396 | 26·4% | 22·2–30·3 | 195 | 159–229 | 14.9% | 12·1–17·5 |
| Upper middle income | 2409 | 1645 | 1344–1855 | 68·3% | 55·8–77·0 | 1413 | 1184–1602 | 58·7% | 49·1–66·5 |
| Lower middle income | 2559 | 2474 | 2426–2505 | 96·7% | 94·8–97·9 | 2363 | 2286–2418 | 92·3% | 89·3–94·5 |
| Low income | 849 | 843 | 832–849 | 99·31% | 98·0–100·0 | 830 | 812–845 | 97·7% | 95·6–99·5 |
| Global* | 7125 | 5312 | 5005–5535 | 74·6% | 70·3–77·7 | 4797 | 4564–5014 | 67.3% | 64.1–70.4 |
CI=credible interval.
The sum of all categories might not equal the global estimate due to rounding.
Figure 2.
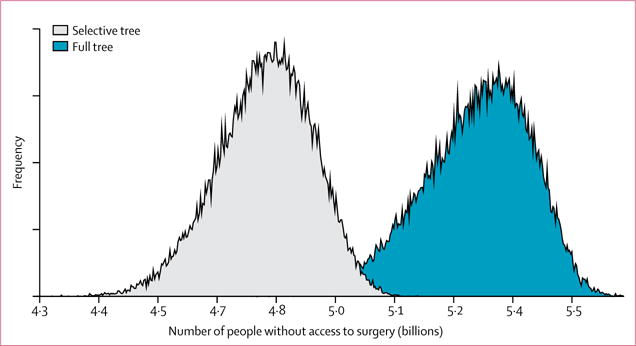
Posterior probability of global population without access to surgery
Table 2.
Total population and proportion of population without access to surgery by Institute for Health Metrics and Evaluation global burden of disease region
| Total population (millions) | Full tree | Selective tree | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Population with no access (millions) | 95% posterior CI | Proportion with no access | 95% posterior CI | Population with no access (millions) | 95% posterior CI | Proportion with no access | 95% posterior CI | ||
| Andean Latin America | 57 | 47 | (41–52) | 83·1% | 72·9–91·7 | 34 | 27–42 | 60·1 | 46·9–73·7 |
| Australasia | 28 | 3 | (1–4) | 9·2% | 4·1–15·0 | 1 | 0–2 | 2·3% | 0·8–6·9 |
| Caribbean | 42 | 37 | (34–40) | 88·2% | 80·7–93·5 | 28 | 25–32 | 67·0% | 58·0–75·8 |
| Central Asia | 86 | 76 | (71–80) | 88·2% | 82·1–93·4 | 74 | 70–78 | 85·9% | 81·4–90·0 |
| Central Europe | 114 | 64 | (53–74) | 56·2% | 46·6–64·6 | 40 | 34–47 | 34·9% | 29·5–41·3 |
| Central Latin America | 246 | 160 | (123–191) | 65·0% | 49·9–77·8 | 82 | 60–112 | 33·4% | 24·2–45·6 |
| Central sub-Saharan Africa | 100 | 100 | (100–100) | 99·6% | 99·1–99·9 | 99 | 97–100 | 98·7% | 97·0–99·6 |
| East Asia | 1405 | 1119 | (825–1319) | 79·6% | 58·7–93·8 | 1052 | 825–1236 | 74·8% | 58·7–88·0 |
| Eastern Europe | 208 | 165 | (135–186) | 79·2% | 64·9–89·4 | 145 | 115–171 | 69·8% | 55·4–81·9 |
| Eastern sub-Saharan Africa | 396 | 394 | (385–396) | 99·4% | 97·2–100·0 | 392 | 384–395 | 99·0% | 96·9–99·8 |
| High-income Asia Pacific | 183 | 97 | (57–135) | 52·8% | 31·3–73·9 | 15 | 9–30 | 8·0% | 4·7–16·4 |
| High-income North America | 351 | 1 | (0–5) | 0·2% | 0·0–1·5 | 1 | 0–5 | 0·2% | 0·0–1·3 |
| North Africa and Middle East | 468 | 366 | (335–394) | 78·3% | 71·5–84·2 | 287 | 261–314 | 61·4% | 55·7–67·1 |
| Oceania | 10 | 9 | (8–9) | 95·6% | 87·8–98·7 | 9 | 8–9 | 89·5% | 82·2–93·8 |
| South Asia | 1650 | 1636 | (1594–1649) | 99·1% | 96·6–100·0 | 1608 | 1540–1642 | 97·4% | 93·3–99·5 |
| Southeast Asia | 632 | 576 | (547–599) | 91·1% | 86·6–94·8 | 512 | 471–549 | 81·0% | 74·5–86·9 |
| Southern Latin America | 62 | 2 | (0–8) | 3·2% | 0·1–13·5 | 2 | 0–8 | 3·2% | 0·3–12·6 |
| Southern sub-Saharan Africa | 75 | 37 | (21–53) | 48·9% | 28·1–70·7 | 27 | 15–39 | 35·7% | 20·3–51·9 |
| Tropical Latin America | 207 | 26 | (7–72) | 12·4% | 3·3–34·7 | 26 | 8–65 | 12·4% | 3·9–31·6 |
| Western Europe | 424 | 25 | (11–44) | 5·9% | 2·7–10·4 | 10 | 5–19 | 2·5% | 1·2–4·4 |
| Western sub-Saharan Africa | 367 | 364 | (360–366) | 99·4% | 98·2–99·9 | 356 | 345–361 | 97·1% | 94·1·9–98·6 |
| Global* | 7125 | 5312 | (5005–5535) | 74·6% | 70·3–77·7 | 4797 | 4564–5014 | 67·3% | 64·1–70·4 |
CI=credible interval.
The sum of all categories may not equal the global estimate due to rounding.
Figure 3. Proportion of population without access to surgery by Institute for Health Metrics and Evaluation global burden of disease super region.
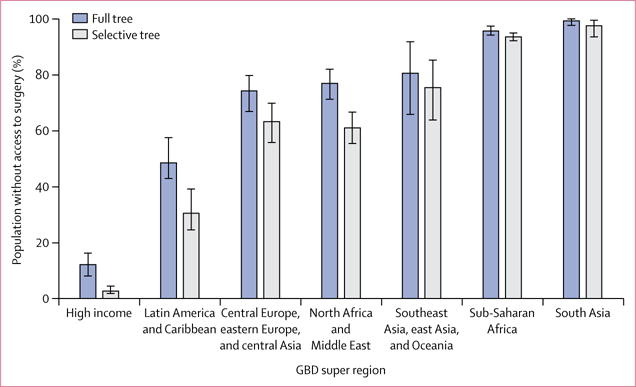
GBD=global burden of disease. Error bars=95% posterior credible interval.
Figure 4.
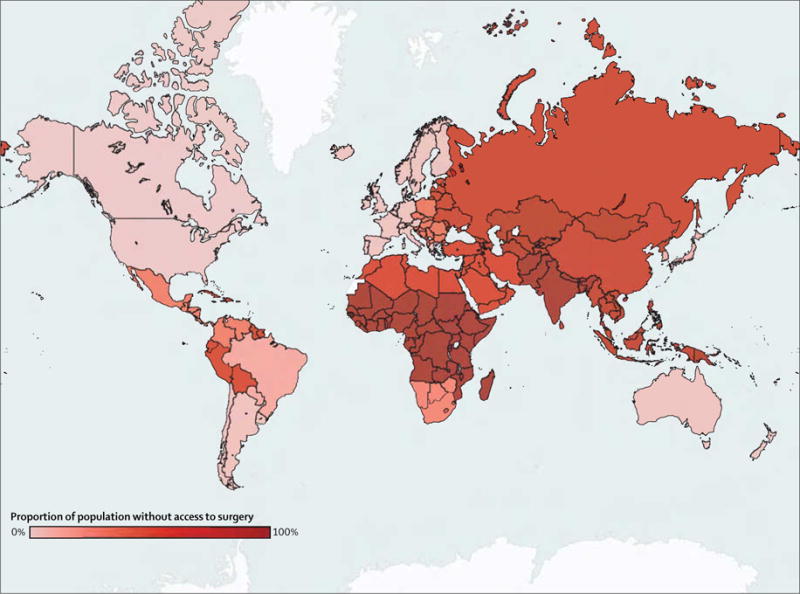
Proportion of population without access to surgery by country (selective tree with baseline assumptions)
We tested several different scenarios to assess the robustness of our results. The baseline assumptions were first tested against the exclusion of each access dimension (table 3). When capacity, timeliness, or safety is excluded, our estimates of the global population without access to surgery remained higher than 4 billion in both the full and selective trees. The affordability dimension had the greatest impact on our estimates, as it is the only dimension that when excluded, results in estimates of less than 4 billion people without surgical access. Specifically, the selective tree estimates that 3·6 billion do not have access to surgical services when affordability is excluded from the model (table 3). We also tested variations of the proxies for timeliness, capacity, and affordability (table 4). For each variation, again with the exception of affordability, the estimates remained well above 4 billion. Figure 2 shows the results of the probabilistic sensitivity analysis, which informs the 95% posterior credible intervals.
Table 3.
Sensitivity analysis excluding one access dimension from baseline assumptions, by population (billions) and proportion without access
| Full tree | Selective tree | |
|---|---|---|
| Excluding timeliness | 4·97 (70%) | 4·70 (66%) |
| Excluding capacity | 5·02 (70%) | 4·69 (66%) |
| Excluding safety | 4·99 (70%) | 4·27 (60%) |
| Excluding affordability | 4·66 (65%) | 3·62 (51%) |
Table 4.
Sensitivity analysis of variation on proxies, by population (billions) and proportion without access
| Full tree | Selective tree | |
|---|---|---|
| Timeliness | ||
| p(C|T)=p(C) | 5·34 (75%) | 4·82 (68%) |
| p(C|T)=min(2·p(C),1.0) | 5·11 (72%) | 4·72 (66%) |
| Capacity | ||
| Index country=Sweden | 6·05 (85%) | 5·04 (71%) |
| Index country=Germany | 5·90 (83%) | 5·00 (70%) |
| Index country=Singapore | 5·59 (79%) | 4·91 (69%) |
| OR density | 5·07 (71%) | 4·72 (66%) |
| Affordability | ||
| Direct medical costs only | 4·82 (68%) | 3·99 (56%) |
Discussion
We estimate that 4·8 billion (95% PCI 4·6–5·0 billion) people (67% of the world’s population) do not have access to safe, affordable, and timely surgical care. When less restrictive assumptions are applied, our estimate increases to 5·3 billion (95% PCI 5·0–5·5 billion); these estimates are robust to several one-way sensitivity analyses (tables 3 and 4).
We recognise that these results might seem implausible at first; our estimates are more than double those previously reported by Funk and colleagues4 and suggest that less than 1% of individuals in low-income countries and less than 5% of individuals in lower-middle-income countries have access to surgical care.4 However, our definition of access is inclusive of more than simply surgical capacity: it also includes affordability, safety, and timeliness of care. Within this context, these results compare reasonably with other estimates that apply a more limited definition of access. Funk and colleagues suggested that at least 2·2 billion individuals are without access on the basis of operating theatre density alone.4 The World Bank estimates that more than 3 billion people live on less than US$2·50 per day and are, hence, poorly positioned to afford surgical care. Consistent with the distribution of poverty, we find that individuals without access to surgery are overwhelmingly represented in low-income and middle-income countries (figures 3 and 4).
To providers who practice regularly in these parts of the world, these estimates validate a common but untold experience.13 Assessments of surgical infrastructure in low-resources settings describe a stark reality: steady electricity was present in only 81 (35%) of 231 district hospitals in 12 sub-Saharan African countries;14 running water was consistently available in just two of the ten hospitals surveyed in a county in Sierra Leone;15 oxygen sources were only available in 24 (40%) of 60 surgical hospitals surveyed across east Africa;16 and only seven (64%) of 11 surveyed county hospitals in Liberia had an in-house blood bank, and those that did had a mean of four units per hospital.17 In Liberia, even before the Ebola crisis, there were fewer than three native surgeons working in the entire country.18 Our results and these data imply that access to safe, affordable, and timely surgical care is absent for much of the world. Nonetheless, for each access dimension, we argue that, if anything, our model is conservative and risks understating the magnitude of the crisis.
Our estimates of the probability of receiving timely surgical care, for example, rely on the WHO’s estimates of the proportion of road traffic injuries transported to a hospital by ambulance.9 They overestimate timely access in several important ways. First, these estimates, which reflect the likelihood of the presence of a prehospital system, consist of broad country-level assessments, and ignore geospatial realities. For example, the proportion of patients with serious injuries transported by ambulance in India is estimated to range from 11% to 50%. Since our model applies the upper bound of the interval, it ascribes timely access to half of the rural population even though the scarcity of rural surgical providers means most of these patients live hours away from the nearest surgeon, which would preclude timely access even in the presence of excellent prehospital transportation.19
Second, although the WHO data are a reasonable proxy for timeliness in patient transport during emergencies, they do not capture delays associated with chronic conditions (ie, the inability of a surgical facility to offer planned surgical care given overwhelming acute volume), nor do they directly account for the delay in the decision to seek care.1 Additionally, the practical delays related to receiving care on reaching the hospital from seemingly trivial issues like patients navigating the hospital environment, or poor triage processes, for example, are not insignificant.13,16
Third, this proxy does not account for known inequities in access in high-income countries, which would require more granularity than can be afforded with aggregate country-level data. Assessed at the local level, for example, the USA often performs poorly with prehospital delays. This phenomenon is best shown by the so-called trauma deserts of Chicago, in which gun-shot victims who lived more than 5 miles from a trauma centre had significant increased odds of mortality.7 Delays in surgical care for chronic disorders are also found in high-income countries as shown by the fact that late-stage presentation of cancer in the USA is associated with ethnic origin and insurance status.20 For instance, in Boston, black women have a breast cancer mortality rate that is more than twice that of white women.21
Next we assessed surgical capacity in each country by constructing a ratio of present surgical procedure rate to the necessary surgical procedure rate to meet demand, and this can also result in an overestimate of access. The ability to perform surgical procedures requires a functioning operating theatre, supplies, and staff, and therefore procedure rates are a reliable indicator of gross surgical capacity. However, although surgical volume can reveal deficits in capacity, it says little about case mix or where surgical capacity exists. The thousand cleft-lip repairs done in the tertiary centre in the city can provide a false impression of the access to laparotomy or caesarean delivery in the rural setting. In 2013, for example, rural Sierra Leone had a surgeon-to-population ratio almost four times lower than that of the urban areas.19 Therefore, low surgical rates are a specific but insensitive indicator of access; if surgery is not being done, it follows that surgical care is not being delivered; however, high surgical rates cannot speak to the distribution of surgical access.
Additionally, the inherent uncertainty in the models used to estimate surgical capacity deserves special mention. The estimate of necessary procedure rates created by Rose and colleagues,10 although based on prevalence data for most disorders included in global burden of disease studies, does not capture all diseases and is consequently a conservative estimate of need. If the true necessary procedure rate, inclusive of all disease disorders, is actually higher than the one proposed by Rose and colleagues, our model would overestimate access at all procedure levels. If country-specific surgical procedure rates are under estimated in the model developed by Weiser and colleagues,22 our estimates will underestimate access; however, we believe that in view of its methods, on the whole, our estimates of capacity lead to net overestimates of access.
Next, our model’s sole use of the presence of pulse oximetry as a proxy for safety can overestimate access as pulse oximetry, by itself, is a necessary but insufficient criterion for safe surgery.23,24 As described, low-resource environments face severe deficits in trained workforce, equipment, supplies, and basic physical infrastructure, in many cases precluding provision of what could be regarded as safe surgery (even if a pulse oximeter was present). Consequently, the use of pulse oximetry penetrance as the main requisite for safe surgery amounts to a conservative estimate of the lower bound without access. More encompassing indicators of safety such as the perioperative mortality rate might provide a more accurate assessment of the upper bound without access to safe surgical care. However the paucity of these data collected worldwide precludes their use in our present model.1
Finally, our affordability proxy, based on Shrime and colleagues’ model for catastrophic expenditure,8 estimates affordability at a conservative boundary by only accounting for patients who would be impoverished should they need surgery. For our baseline estimates, we chose to use Shrime and colleagues’ estimates for catastrophic expenditure that are inclusive of direct medical costs and indirect medical costs (eg, cost of transportation to a health facility and lost wages) because we believed it was only sensible that all costs experienced by the patient be included to reasonably assess the risk of impoverishment.25,26 Ultimately, in a just world, affordability should hardly be defined as simply an expense that does not impoverish. As such, billions of people are at risk of losing financial security due to payments for surgical care even if they do not force them below the poverty line.27,28
As mentioned previously, affordability not only affects those who receive care, but also influences the decision to seek it. Grimes and colleagues6 noted that, from cataracts to maternal health, direct and indirect costs prevent patients from using the health system. Therefore, affordability and timeliness are closely related, and our model is unable to account for patients who avoid the health-care system entirely.
Our study has many important limitations, most of which are addressed in the discussion of each access dimension. More broadly, we recognise that any model is restricted by the quality of inputs, and in view of the absence of empirical data in many low-income and middle-income countries; much of the data used in this study are the result of a model. To account for this, we tested our assumptions against a number of one-way sensitivity analyses and incorporated uncertainty in our parameters with probabilistic sensitivity analysis. Data were missing for 2% of the global population, and therefore we used statistical techniques to impute the parameters for this segment of the population. Although every attempt was made to capture this additional uncertainty in our 95% PCIs, we still need to acknowledge the missing data as a major limitation.
Further, we recognise that our estimates are sensitive to the definition of access that is applied. Specifically, exclusion of the affordability parameter has a significant effect on our estimates, such that when removed from our selective model, our estimate of the global population without access to surgery falls to 3·6 billion. Although this is still greater than the previously reported 2·2 billion, it falls short of the 4·8 billion reported in our baseline results. Nonetheless, we find it unreasonable to ignore affordability in assessing access to care which often hinges on the ability to pay. The remaining sensitivity analyses suggest, however, that our results are robust and resilient to a number of different assumptions (tables 3 and 4).
The world’s population without access to surgical care is significantly greater than previously reported, as prior estimates relied on a relatively narrow definition of access. In a world focusing on universal health coverage, the vision of the Lancet Commission on Global Surgery is universal access to safe and affordable surgical and anaesthesia care when needed. When all components of this vision are examined, at least 4·8 billion people do not have access to surgical care. The burden of this inequity falls most heavily on the world’s rural poor people. Expanding access to surgery and anaesthesia care will require coordinated investment in surgical scale-up that grows the workforce, builds infrastructure, removes cultural and geographic barriers, and provides financial protection.
Supplementary Material
Research in context.
Evidence before this study
During preparation for this study, we searched Medline and Google Scholar to identify studies that had attempted to estimate the global population without access to surgery. We were able to identify one study that used an arbitrary cutoff of operating theatres per person (the primary measure) to derive an estimate of the population without access to surgery. We found no other global estimates in the scientific literature. Furthermore, the Lancet Commission on Global Surgery only recently defined access as inclusive of timeliness, capacity, safety, and affordability. For these reasons, we did not do a systematic review. We would note that others have provided indirect assessments of our primary outcome. Funk and colleagues estimated operating theatres per person by country; from these estimates, they identified countries with less than two operating theatres per 100 000 people and then added the population of these countries to estimate the global population without access to surgery, arriving at 2·2 billion. Weiser and colleagues indirectly assessed equity in access to care by estimating surgical procedure rates by country and noted that, although countries that expend less than US$100 gross domestic product per person make up 35% of the global population, only 3·5% of the total volume of surgery takes place in these countries.
Added value of this study
At least 4·8 billion people in the world do not have timely access to safe, affordable surgical care. This estimate is substantially higher than the 2·2 billion estimate commonly referenced in the global surgery literature. When considered with recent estimates that suggest that up to 30% of the global burden of disease is surgical, the estimates of this study suggest that there is an urgent need to address the undersupply of surgical services. The Lancet Commission on Global Surgery has made recommendations for a way forward, including the appropriate allocation of financial resources to build surgical capacity and strengthen health systems, building a robust surgical workforce, ensuring that surgery is delivered in a safe manner, and providing for financial protection against impoverishment through universal health coverage. Our estimates suggest there is a long way to go, but if the global health community wishes to address ongoing inequities and the growing burden of disease, improving access to surgical care cannot be ignored.
Implications of all the available evidence
The world’s population without access to surgical care is much greater than previously reported, since previous estimates relied on a rather narrow definition of access. In a world focusing on universal health coverage, the vision of the Lancet Commission on Global Surgery is universal access to safe, affordable surgical and anaesthesia care when needed. When all components of this vision are assessed, at least 4·8 billion people do not have access to surgical care. The burden of this inequity falls most heavily on the world’s rural poor. Expanding access to surgery and anaesthesia care will require a coordinated investment in surgical scale-up that grows the workforce, builds infrastructure, removes cultural and geographical barriers, and provides financial protection.
Acknowledgments
We thank Jong Hun Kim (Tufts University School of Medicine), Gloria Boye (Boston Children’s Hospital), and Alireza Shirazian (Tufts University School of Medicine), for their contributions to searching the scientific literature and data collection.
Footnotes
Contributors
All coauthors have made substantial intellectual contributions in terms of conception, drafting, and critical appraisal of this manuscript.
Declaration of interests
We declare no competing interests.
See Online for appendix
For the RiskAmp plugin see www.riskamp.com
For the Real Statistics see www.real-statistics
References
- 1.Meara JG, Leather AJM, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015 doi: 10.1016/j.surg.2015.02.009. published online April 27. http://dx.doi.org/10.1016/S0140-6736(15)60160-X. [DOI] [PubMed]
- 2.Kim JY, Farmer PE. What’s missing from the Ebola fight in West Africa. The Washington Post. 2014 Aug 31, 2014. [Google Scholar]
- 3.Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372:139–44. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- 4.Funk LM, Weiser TG, Berry WR, et al. Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet. 2010;376:1055–61. doi: 10.1016/S0140-6736(10)60392-3. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee JK. Analysing outcome of surgical development–rural surgery as an example. Indian J Surg. 2003;65:68–72. [Google Scholar]
- 6.Grimes CE, Bowman KG, Dodgion CM, Lavy CBD. Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg. 2011;35:941–50. doi: 10.1007/s00268-011-1010-1. [DOI] [PubMed] [Google Scholar]
- 7.Crandall M, Sharp D, Unger E, et al. Trauma deserts: distance from a trauma center, transport times, and mortality from gunshot wounds in Chicago. Am J Public Health. 2013;103:1103–09. doi: 10.2105/AJPH.2013.301223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shrime MG, Dare A, Alkire B, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery: a modelling study. Lancet Glob Health. 2015;3:S38–44. doi: 10.1016/S2214-109X(15)70085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Global status report on road safety 2013: Supporting a decade of action. Geneva: World Health Organization; 2013. [Google Scholar]
- 10.Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler SW. Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health. 2015;3:S13–20. doi: 10.1016/S2214-109X(15)70087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shrime MG, Daniels KM, Meara JG. How much surgery is enough? Aligning surgical delivery with best-performing health systems. Lancet. 2015;385:S13. doi: 10.1016/S0140-6736(15)60808-X. (Global Surgery special issue) [DOI] [PubMed] [Google Scholar]
- 12.Murray CJ, Ezzati M, Flaxman AD, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–66. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 13.Raykar NP, Yorlets RR, Liu C, et al. A qualitative study exploring contextual challenges to surgical care provision in 21 LMICs. Lancet. 2015;385:S15. doi: 10.1016/S0140-6736(15)60810-8. (Global Surgery special issue) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belle J, Cohen H, Shindo N, et al. Influenza preparedness in low-resource settings: a look at oxygen delivery in 12 African countries. J Infect Dev Ctries. 2010;4:419–24. doi: 10.3855/jidc.859. [DOI] [PubMed] [Google Scholar]
- 15.Kingham TP, Kamara TB, Cherian MN, et al. Quantifying surgical capacity in Sierra Leone: a guide for improving surgical care. Arch Surg. 2009;144:122–27. doi: 10.1001/archsurg.2008.540. discussion 128. [DOI] [PubMed] [Google Scholar]
- 16.Jochberger S, Ismailova F, Lederer W, et al. “Helfen Berührt” Study Team Anesthesia and its allied disciplines in the developing world: a nationwide survey of the Republic of Zambia. Anesth Analg. 2008;106:942–48. doi: 10.1213/ane.0b013e318166ecb8. [DOI] [PubMed] [Google Scholar]
- 17.Knowlton LM1, Chackungal S, Dahn B, LeBrun D, Nickerson J, McQueen K. Liberian surgical and anesthesia infrastructure: a survey of county hospitals. World J Surg. 2013;37:721–29. doi: 10.1007/s00268-013-1903-2. [DOI] [PubMed] [Google Scholar]
- 18.WHO. Joint WHO-MOH facilitators meeting on integrated management for emergency and essential surgical care report. Monrovia: WHO; 2008. http://apps.who.int/medicinedocs/documents/s15344e/s15344e.pdf (accessed April 21, 2015) [Google Scholar]
- 19.Raykar NP, Bowder AN, Liu C, et al. Geospatial mapping to estimate timely access to surgical care in nine low-income and middle-income countries. Lancet. 2015;385:S16. doi: 10.1016/S0140-6736(15)60811-X. (Global Surgery special issue) [DOI] [PubMed] [Google Scholar]
- 20.Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9:222–31. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 21.Hunt BR, Whitman S, Hurlbert MS. Increasing black-white disparities in breast cancer mortality in the 50 largest cities in the United States. Cancer Epidemiol. 2014;38:118–123. doi: 10.1016/j.canep.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Weiser TG, Haynes AB, Molina G, et al. Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet. 2015;385:S11. doi: 10.1016/S0140-6736(15)60806-6. (Global Surgery special issue) [DOI] [PubMed] [Google Scholar]
- 23.Jubran A. Applied Physiology in Intensive Care Medicine. Springer; 2009. Pulse oximetry; pp. 45–8. [Google Scholar]
- 24.Merry AF, Eichhorn JH, Wilson IH. Extending the WHO ‘Safe Surgery Saves Lives’ project through global oximetry. Anaesthesia. 2009;64:1045–48. doi: 10.1111/j.1365-2044.2009.06104.x. [DOI] [PubMed] [Google Scholar]
- 25.Shrime MG, Alkire BC, Mock A. Global burden of surgical disease: an estimation from the provider perspective. Lancet Glob Health. 2015;3:S8–9. doi: 10.1016/S2214-109X(14)70384-5. [DOI] [PubMed] [Google Scholar]
- 26.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–17. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 27.Chen S, Ravallion M, World Bank . The developing world is poorer than we thought, but no less successful in the fight against poverty. Washington, DC: World Bank; 2008. (Policy research working paper 4703). [Google Scholar]
- 28.Kruk ME, Goldmann E, Galea S. Borrowing and selling to pay for health care in low- and middle-income countries. Health Aff (Millwood) 2009;28:1056–66. doi: 10.1377/hlthaff.28.4.1056. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


