Abstract
Introduction
It is unclear whether LVH detected by electrocardiogram (ECG-LVH) is equally predictive of heart failure as LVH detected by echocardiography (echo-LVH).
Methods
This analysis included 4,008 white participants (41% male) aged 65 years or older from the Cardiovascular Health Study (CHS) who were free of stroke and major intraventricular conduction defects at baseline. ECG-LVH was defined by the Cornell criteria from baseline ECG data and echo-LVH was computed from baseline echocardiography measurements. Cox regression was used to compute hazard ratios (HR) and 95% confidence intervals (CI) for the association between ECG-LVH and echo-LVH and adjudicated incident stroke events, separately. Harrell’s concordance indices (C-index) were calculated for the Framingham Stroke Risk Score with inclusion of ECG-LVH and echo-LVH, separately.
Results
ECG-LVH was detected in 136 (3.4%) participants and echo-LVH was present in 208 (5.2%) participants. Over a median follow-up of 13 years (interquartile range=7.5, 19.1), a total of 769 (19%; incidence rate=15.4 per 1000 person-years) strokes occurred. In a multivariable Cox regression analysis adjusted for stroke risk factors and potential confounders, ECG-LVH (HR=1.68, 95%CI=1.23, 2.28) and echo-LVH (HR=1.58, 95%CI=1.17, 2.14) were associated with an increased risk of stroke. Similar values were obtained for the C-index when either ECG-LVH (C-index=0.786) or echo-LVH (C-index=0.786) were included in the Framingham Stroke Risk Score.
Conclusion
ECG-LVH and echo-LVH can be used interchangeably in stroke risk scores.
Keywords: stroke, left ventricular hypertrophy, ECG, echocardiography
INTRODUCTION
Left ventricular hypertrophy (LVH) diagnosed by electrocardiography (ECG-LVH) and echocardiography (echo-LVH) have been independently associated with an increased risk for future cardiovascular events, including stroke [1-7]. The Framingham Stroke Risk Score was developed to identify individuals who are high risk for developing future stroke [3]. In addition to other stroke risk factors, a key component of this score is ECG-LVH. Due to its low-cost and widespread availability, ECG risk factors such as ECG-LVH are cost-effective makers for preventive cardiologists to incorporate into models of stroke risk. However, the ECG has a relatively low sensitivity regarding the detection of LVH [8, 9]. Although it has been suggested that ECG-LVH and echo-LVH are distinct clinical entities with separate predictive abilities, it is currently unknown if the addition of echo-LVH, a more sensitive marker for LVH, improves the prediction of stroke risk models. Therefore, the purpose of this analysis was to compare the predictive ability of the Framingham Stroke Risk Score when using ECG-LVH and echo-LVH to determine if these markers can be used interchangeably in a model to identify persons who are high risk for future stroke.
METHODS
Study Population
Details of CHS have been previously described [10]. Briefly, CHS is a prospective population-based cohort study of risk factors for coronary heart disease and stroke in individuals 65 years and older. A total of 5,888 participants with Medicare eligibility were recruited from 4 field centers located in the following locations in the United States: Forsyth County, NC; Sacramento County, CA; Washington County, MD; and Pittsburgh, PA. Subjects were followed with semi-annual contacts, alternating between telephone calls and surveillance clinic visits. CHS clinic exams ended in June of 1999 and since that time 2 yearly phone calls to participants were used to identify events and collect data. The institutional review board at each site approved the study and written informed consent was obtained from participants at enrollment. Participants were excluded if any of the following criteria were met: baseline stroke was present, baseline covariate data were missing, QRS duration ≥120 ms, or follow-up data were missing.
Of the 5,888 participants from the original CHS cohort, we excluded 901 black participants due to the known racial differences that have been reported regarding the criteria for detection of ECG-LVH and echo-LVH [11-14]. Of those that remained, 48 participants with missing follow-up data, 168 participants with baseline stroke, 361 with QRS ≥120 ms, and 402 with missing baseline covariate data also were excluded. A total of 4,008 participants (41% male) with complete data were used in this analysis.
Left Ventricular Hypertrophy
LVH was determined from the baseline ECG or echocardiogram. Identical electrocardiographs (MAC PC, Marquette Electronics Inc., Milwaukee, Wisconsin) were used at all clinic sites, and resting, 10-second standard simultaneous 12-lead ECGs were recorded in all participants [15]. ECG-LVH was defined by the Cornell criteria (R wave amplitude AVL plus S wave amplitude V3 ≥28 mm for men and ≥20 mm for women) [16]. A baseline echocardiogram was obtained for each study participant according to previously described techniques [17]. Measurements were made from digitized images using an off-line image-analysis system equipped with customized computer algorithms. Left ventricular mass was derived from standard formulas described by Devereux et al.[18] Echo-LVH was defined by left ventricular mass values >95th sex-specific percentiles (male: >209 g; female: >169 g).
Stroke Events
Baseline and incident cases of stroke were identified by adjudication of medical records, including hospitalization data, and these methods have been previously described [19-21]. Briefly, baseline self-reported cases of transient ischemic attack and stroke were confirmed through review of appropriate medical records. All suspected stroke events and stroke-related deaths were reviewed by the Cerebrovascular Adjudication Committee. This committee was composed of study neurologists from each of the four study sites, a neuroradiologist from the MRI Reading Center, and an internist or neurologist representing the Coordinating Center. Based on this information, which included neuroimaging studies, the Cerebrovascular Adjudication Committee would decide whether a transient ischemic attack, nonfatal stroke, or fatal stroke had occurred and, if appropriate, assign a stroke type: ischemic, hemorrhagic, or uncertain. For this analysis, incident stroke included fatal and non-fatal events and subtypes classified as ischemic or hemorrhagic.
Covariates
Participant characteristics were collected during the initial CHS interview and questionnaire. Age, sex, race, income, education, and smoking status were self-reported. Annual income was dichotomized at $25,000 and education was dichotomized at “high school or less.” Smoking was defined as current or ever smoker. Participants’ blood samples were obtained after a 12-hour fast at the local field center. Measurements of total cholesterol, high-density lipoprotein (HDL) cholesterol, and plasma glucose were used in this analysis. Diabetes was defined as a self-reported history of a physician diagnosis, a fasting glucose value ≥126 mg/dL, or by the current use of insulin or oral hypoglycemic medications. Blood pressure was measured for each participant in the seated position and systolic measurements were used in this analysis. The use of aspirin, statins, and antihypertensive medications were self-reported. Body mass index was computed as the weight in kilograms divided by the square of the height in meters. Baseline cardiovascular disease was determined by a self-reported history or by medical record adjudication of the following diagnoses: myocardial infarction, angina pectoris without myocardial infarction, coronary revascularization procedures (angioplasty and coronary artery bypass graft surgery), congestive heart failure, and claudication [19].
Statistical Analysis
Categorical variables were reported as frequency and percentage while continuous variables were recorded as mean ± standard deviation. Statistical significance for categorical variables was tested using the chi-square method and the Wilcoxon rank-sum procedure for continuous variables. Comparisons were examined between participants with and without ECG-LVH and echo-LVH, separately. We examined the association between ECG-LVH and echo-LVH at baseline with incident stroke, separately. Follow-up time was defined as the time from the initial study exam until one of the following: stroke, death, loss to follow-up, or end of follow-up which was July 1, 2008. Kaplan-Meier estimates were used to compute cumulative incidence of stroke by LVH and the differences in estimates were compared using the log-rank procedure [22]. Cox regression was used to compute hazard ratios (HR) and 95% confidence intervals (CI) for the association between LVH and incident stroke. We examined the effect of ECG-LVH and echo-LVH in isolated Cox regression models and also examined the association of either ECG-LVH or echo-LVH to define LVH to determine the combined effect of both modalities to define LVH and the associated risk of stroke. Multivariable models were constructed as follows: Model 1 adjusted for age, sex, education, and income; Model 2 adjusted for Model 1 covariates plus smoking, systolic blood pressure, diabetes, body mass index, total cholesterol, HDL cholesterol, aspirin, statins, antihypertensive medications, and cardiovascular disease. To explore the potential interchangeability of ECG-LVH and echo-LVH in the Framingham Stroke Risk Score, we computed Harrell’s concordance index (C-index) for models that included ECG-LVH as originally done in the Framingham Stroke Risk Score and echo-LVH using methodology developed for survival analyses [3, 23]. In addition to a marker for LVH, we included the other covariates of the risk score: age, systolic blood pressure, antihypertensive medications, diabetes, smoking, prior cardiovascular disease, and atrial fibrillation. The proportional hazards assumption was not violated in our analyses. Statistical significance was defined as p<0.05. SAS Version 9.3 (Cary, NC) was used for all analyses.
RESULTS
ECG-LVH was detected in 136 (3.4%) participants and echo-LVH was present in 208 (5.2%) participants. A total of 54 (19%) had both ECG-LVH and echo-LVH. Baseline characteristics stratified by ECG-LVH and echo-LVH are shown in Table 1.
Table 1.
Baseline Characteristics (N=4,008)
| Characteristic | ECG-LVH (n=136) |
No ECG-LVH (n=3,872) |
P-value* | Echo-LVH (n=208) |
No Echo-LVH (n=3,800) |
P-value* |
|---|---|---|---|---|---|---|
| Age, years | ||||||
| 65-70 (%) | 45 (33) | 1,736 (45) | 108 (52) | 1,673 (44) | ||
| 71-74 (%) | 35 (26) | 911 (24) | 44 (21) | 902 (24) | ||
| 75-80 (%) | 37 (27) | 866 (22) | 46 (22) | 857 (23) | ||
| >80 (%) | 19 (14) | 359 (9.3) | 0.032 | 10 (4.8) | 368 (10) | 0.040 |
| Male (%) | 36 (26) | 1,609 (42) | 0.0004 | 84 (40) | 1,561 (41) | 0.84 |
| High school or less (%) | 75 (55) | 2,174 (56) | 0.82 | 138 (66) | 2,111 (56) | 0.0023 |
| Income <$25,000 (%) | 84 (62) | 2,343 (61) | 0.77 | 138 (66) | 2,289 (60) | 0.079 |
| Body mass index, mean (SD), kg/m2 | 26 (3.5) | 26 (4.0) | 0.23 | 31 (3.9) | 26 (3.8) | <0.0001 |
| Current or former smoker (%) | 52 (38) | 2,084 (54) | 0.0003 | 103 (50) | 2,033 (54) | 0.26 |
| Diabetes (%) | 27 (20) | 526 (14) | 0.037 | 60 (29) | 493 (13) | <0.0001 |
| Atrial fibrillation (%) | 16 (12) | 180 (4.7) | 0.0002 | 21 (10) | 175 (4.6) | 0.0003 |
| Systolic blood pressure, mean (SD), mm Hg | 150 (22) | 138 (19) | <0.0001 | 143 (20) | 138 (20) | 0.0002 |
| Total cholesterol, mean (SD), mg/dL | 216 (40) | 213 (39) | 0.31 | 212 (42) | 213 (39) | 0.42 |
| HDL-cholesterol, mean (SD), mg/dL | 51 (16) | 54 (16) | 0.015 | 47 (12) | 55 (16) | <0.0001 |
| Antihypertensive medication use (%) | 87 (64) | 1,623 (42) | <0.0001 | 134 (64) | 1,576 (41) | <0.0001 |
| Statin use (%) | 2 (1.5) | 76 (2.0) | 0.68 | 4 (1.9) | 74 (2.0) | 0.98 |
| Aspirin use (%) | 46 (34) | 1,264 (33) | 0.77 | 80 (38) | 1,230 (32) | 0.068 |
| Cardiovascular disease (%) | 42 (31) | 705 (18) | 0.0002 | 75 (36) | 672 (18) | <0.0001 |
Statistical significance for continuous data was tested using Wilcoxon rank-sum procedure and categorical data was tested using the chi-square test.
ECG-LVH=electrocardiographic left ventricular hypertrophy; echo-LVH=echocardiographic left ventricular hypertrophy; HDL=high-density lipoprotein; SD=standard deviation.
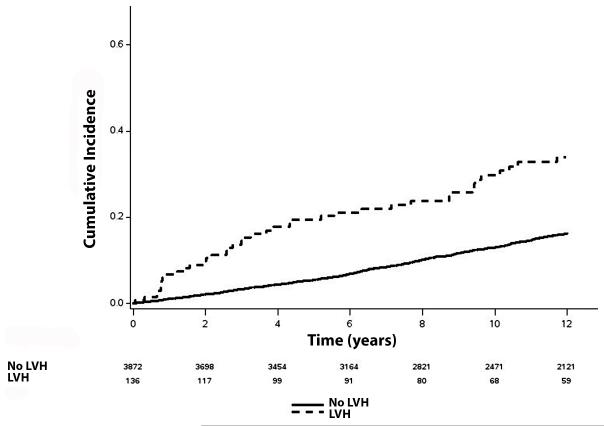
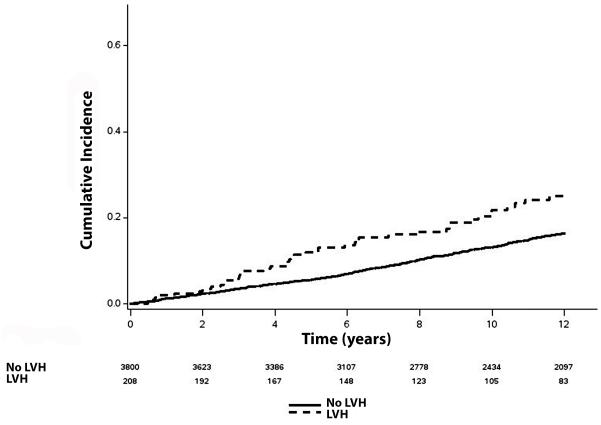
Over a median follow-up of 13 years (interquartile range=7.5, 19.1), a total of 769 (19%; incidence rate=15.4 per 1000 person-years) strokes occurred. The unadjusted cumulative incidence curves of stroke by ECG-LVH and echo-LVH are shown in Figure 1 and Figure 2, respectively. In a multivariable Cox regression analysis, ECG-LVH and echo-LVH were associated with a nearly 68% (p=0.0010) and 58% (p=0.0028) increased risk of stroke, respectively (Table 2). ECG-LVH and echo-LVH were associated with an increased risk of stroke when included in the Framingham Stroke Risk Score (Table 3). Similar C-index values were obtained when either ECG-LVH (C-index: 0.786) or echo-LVH (C-index: 0.786) were included in the Framingham Stroke Risk Score (Table 3).
Figure 1. Risk of Stroke by ECG-LVH*.
*The cumulative incidence curves are statistically different (log-rank p<0.0001). ECG-LVH=electrocardiographic left ventricular hypertrophy; LVH=left ventricular hypertrophy.
Figure 2. Risk of Stroke by echo-LVH*.
*The cumulative incidence curves are statistically different (log-rank p=0.0004). echo-LVH=echocardiographic left ventricular hypertrophy; LVH=left ventricular hypertrophy.
Table 2.
Risk of Stroke (N=4,008)
| Events/ No. at risk |
Incidence Rate per 1000 person-years (95%CI) |
Model 1* HR (95%CI) |
P-value | Model 2† HR (95%CI) |
P-value | |
|---|---|---|---|---|---|---|
| ECG | ||||||
| No LVH | 724/3,872 | 14.9 (13.9, 16.0) | 1.0 | - | 1.0 | - |
| LVH | 45/136 | 32.2 (24.0, 43.1) | 2.08 (1.53, 2.81) | <0.0001 | 1.68 (1.23, 2.28) | 0.0010 |
| Echocardiogram | ||||||
| No LVH | 716/3,800 | 15.0 (13.9, 16.1) | 1.0 | - | 1.0 | - |
| LVH | 53/208 | 24.3 (18.6, 31.8) | 1.75 (1.32, 2.32) | <0.0001 | 1.58 (1.17, 2.14) | 0.0028 |
| ECG or Echocardiogram | ||||||
| No LVH | 692/3,718 | 14.8 (13.7, 15.9) | 1.0 | - | 1.0 | - |
| LVH | 77/290 | 25.6 (20.5, 32.0) | 1.78 (1.41, 2.26) | <0.0001 | 1.55 (1.21, 1.99) | 0.0005 |
Adjusted for age, sex, education, and income.
Adjusted for Model 1 covariates plus smoking status, systolic blood pressure, diabetes, body mass index, total cholesterol, HDL-cholesterol, aspirin, statins, antihypertensive medications, and cardiovascular disease.
CI=confidence interval; ECG=electrocardiogram; HDL=high-density lipoprotein; LVH=left ventricular hypertrophy; HR=hazard ratio.
Table 3.
Harrell’s C-index for Framingham Stroke Risk Score
| HR (95%CI) | P-value | C-index (95%CI) | |
|---|---|---|---|
| ECG-LVH | 1.65 (1.21, 2.24) | 0.0015 | 0.786 (0.725, 0.841) |
| Echo-LVH | 1.39 (1.05, 1.85) | 0.024 | 0.786 (0.725, 0.841) |
| ECG- or echo-LVH | 1.43 (1.12, 1.82) | 0.0038 | 0.785 (0.724, 0.841) |
Age, systolic blood pressure, antihypertensive medications, diabetes, smoking, prior cardiovascular disease, atrial fibrillation.
CI=confidence interval; ECG-LVH=electrocardiographic left ventricular hypertrophy; echo-LVH=echocardiographic left ventricular hypertrophy; HR=hazard ratio.
DISCUSSION
In this analysis from CHS, we have shown that ECG-LVH and echo-LVH are associated with an increased risk of stroke. Additionally, ECG-LVH and echo-LVH are able to be used interchangeably in the Framingham Stroke Risk Score to identify high risk individuals for future stroke events.
Data from the Framingham Heart Study, CHS, and Progetto Ipertensione Umbria Monitoraggio Ambulatoriale (PIUMA) study have shown that LVH, whether detected by ECG or echocardiography, is associated with an increased risk of future stroke [3-5]. However, few studies have examined the predictive ability of these modalities to determine future stroke risk. The Framingham Stroke Risk Score was developed to identify high risk individuals for stroke and included ECG-LVH in addition to several conditions that influence the development of stroke [3]. When ECG-LVH was included in our analysis, the model performed well with high-yield regarding participant discrimination in our population of older adults. The addition of echo-LVH did not improve the discriminatory capacity beyond the original model which included ECG-LVH, suggesting that measures to define LVH, such as the ECG-LVH, perform equally well in risk models designed to estimate stroke risk. Due to the known racial differences in the performance of ECG criteria for LVH, we only included white participants in our analysis and this limits the generalizability of our findings to populations of white, older adults similar to the Framingham Study [11-14].
It has been suggested that ECG-LVH and echo-LVH detect different conditions. The QRS changes that occur with ECG-LVH have been shown to represent a combination of anatomic and electric remodeling [24, 25]. In contrast, echo-LVH commonly relies entirely on left ventricular mass [26]. Although differences potentially exist in the cardiac pathology that is detected, equally important prognostic information regarding stroke risk is obtained from both ECG-LVH and echo-LVH. The implication for the clinician assessing stroke risk associated with LVH is that the combination of clinically relevant risk factors and data from the standard 12-lead ECG are able to provide valuable prognostic information regarding future stroke risk instead of relying on more costly imaging modalities which provide similar information.
Each year, nearly 800,000 persons experience a stroke event in the United States [27]. The yearly cost of direct medical care related to stroke is around $28 billion, with projections to exceed $95 billion by 2030 [28]. The identification of high risk individuals is of paramount importance for public health officials with aims of targeted preventions to reduce the future burden that stroke will place on the healthcare system. Due to its low-cost and widespread availability, the ECG is a cost-effective tool for identifying individuals who are at risk for the development of stroke in addition to other common risk factors included in stroke risk models. Therefore, our data support the use of the ECG to detect LVH to include in risk prediction models of stroke in place of methods such as echocardiography that are not as widely available. However, further research is needed to determine the optimal model for stroke risk prediction in minority populations, as the risk afforded with ECG-LVH and echo-LVH possibly varies by race.
The results of the current analysis should be interpreted in the context of several limitations. We defined ECG-LVH by the Cornell criteria and our results may vary with other definitions (e.g., Sokolow-Lyon). Similarly, we defined echo-LVH by left ventricular mass values >95th sex-specific percentiles. Other definitions for echo-LVH have been proposed and the results may vary with alternative definitions [26]. Additionally, the definition of echo-LVH used was based on left ventricular mass which depends on assumptions of left ventricular geometry and the indexing method. Thus, cases of echo-LVH may have been missed. However, other studies have shown that the predictive value of left ventricular geometry beyond left ventricular mass for heart failure prediction is negligible [29, 30]. The outcome of interest included ischemic and hemorrhagic stroke events, and the results possibly differ when examining each stroke subtype in isolation. However, due to the limited number of stroke events, we included all stroke events as the main endpoint. Also, several potential confounders were included in our multivariable models that likely influenced the development of incident stroke and we acknowledge the possibility of residual confounding.
In conclusion, we have demonstrated that ECG-LVH and echo-LVH are associated with an increased risk of stroke and both conditions can be used interchangeably in stroke risk scores. Further research is needed to explore the clinical utility of current stroke risk prediction models to target groups who are high risk for developing stroke and also to develop race-specific models that are representative of minority populations.
Acknowledgements
This Manuscript was prepared using CHS Research Materials obtained from the NHLBI Biologic Specimen and Data Repository Information Coordinating Center and does not necessarily reflect the opinions or views of the CHS or the NHLBI.
Footnotes
Disclosures
None of the authors reports a conflict of interest.
REFERENCES
- [1].Levy D, Salomon M, D'Agostino RB, Belanger AJ, Kannel WB. Prognostic implications of baseline electrocardiographic features and their serial changes in subjects with left ventricular hypertrophy. Circulation. 1994;90:1786–93. doi: 10.1161/01.cir.90.4.1786. [DOI] [PubMed] [Google Scholar]
- [2].Kannel WB, Gordon T, Castelli WP, Margolis JR. Electrocardiographic left ventricular hypertrophy and risk of coronary heart disease. The Framingham study. Ann Intern Med. 1970;72:813–22. doi: 10.7326/0003-4819-72-6-813. [DOI] [PubMed] [Google Scholar]
- [3].Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–8. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- [4].Bikkina M, Levy D, Evans JC, Larson MG, Benjamin EJ, Wolf PA, et al. Left ventricular mass and risk of stroke in an elderly cohort. The Framingham Heart Study. JAMA. 1994;272:33–6. [PubMed] [Google Scholar]
- [5].Manolio TA, Kronmal RA, Burke GL, O'Leary DH, Price TR. Short-term predictors of incident stroke in older adults. The Cardiovascular Health Study. Stroke. 1996;27:1479–86. doi: 10.1161/01.str.27.9.1479. [DOI] [PubMed] [Google Scholar]
- [6].Verdecchia P, Porcellati C, Reboldi G, Gattobigio R, Borgioni C, Pearson TA, et al. Left ventricular hypertrophy as an independent predictor of acute cerebrovascular events in essential hypertension. Circulation. 2001;104:2039–44. doi: 10.1161/hc4201.097944. [DOI] [PubMed] [Google Scholar]
- [7].Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Left ventricular mass and incidence of coronary heart disease in an elderly cohort. The Framingham Heart Study. Ann Intern Med. 1989;110:101–7. doi: 10.7326/0003-4819-110-2-101. [DOI] [PubMed] [Google Scholar]
- [8].Levy D, Labib SB, Anderson KM, Christiansen JC, Kannel WB, Castelli WP. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation. 1990;81:815–20. doi: 10.1161/01.cir.81.3.815. [DOI] [PubMed] [Google Scholar]
- [9].Woythaler JN, Singer SL, Kwan OL, Meltzer RS, Reubner B, Bommer W, et al. Accuracy of echocardiography versus electrocardiography in detecting left ventricular hypertrophy: comparison with postmortem mass measurements. J Am Coll Cardiol. 1983;2:305–11. doi: 10.1016/s0735-1097(83)80167-3. [DOI] [PubMed] [Google Scholar]
- [10].Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–76. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- [11].Rautaharju PM, Park LP, Gottdiener JS, Siscovick D, Boineau R, Smith V, et al. Race- and sex-specific ECG models for left ventricular mass in older populations. Factors influencing overestimation of left ventricular hypertrophy prevalence by ECG criteria in African-Americans. J Electrocardiol. 2000;33:205–18. doi: 10.1054/jelc.2000.7667. [DOI] [PubMed] [Google Scholar]
- [12].Lee DK, Marantz PR, Devereux RB, Kligfield P, Alderman MH. Left ventricular hypertrophy in black and white hypertensives. Standard electrocardiographic criteria overestimate racial differences in prevalence. JAMA. 1992;267:3294–9. [PubMed] [Google Scholar]
- [13].Jaggy C, Perret F, Bovet P, van Melle G, Zerkiebel N, Madeleine G, et al. Performance of classic electrocardiographic criteria for left ventricular hypertrophy in an African population. Hypertension. 2000;36:54–61. doi: 10.1161/01.hyp.36.1.54. [DOI] [PubMed] [Google Scholar]
- [14].Okin PM, Wright JT, Nieminen MS, Jern S, Taylor AL, Phillips R, et al. Ethnic differences in electrocardiographic criteria for left ventricular hypertrophy: the LIFE study. Losartan Intervention For Endpoint. Am J Hypertens. 2002;15:663–71. doi: 10.1016/s0895-7061(02)02945-x. [DOI] [PubMed] [Google Scholar]
- [15].Furberg CD, Manolio TA, Psaty BM, Bild DE, Borhani NO, Newman A, et al. Major electrocardiographic abnormalities in persons aged 65 years and older (the Cardiovascular Health Study). Cardiovascular Health Study Collaborative Research Group. Am J Cardiol. 1992;69:1329–35. doi: 10.1016/0002-9149(92)91231-r. [DOI] [PubMed] [Google Scholar]
- [16].Devereux RB, Casale PN, Eisenberg RR, Miller DH, Kligfield P. Electrocardiographic detection of left ventricular hypertrophy using echocardiographic determination of left ventricular mass as the reference standard. Comparison of standard criteria, computer diagnosis and physician interpretation. J Am Coll Cardiol. 1984;3:82–7. doi: 10.1016/s0735-1097(84)80433-7. [DOI] [PubMed] [Google Scholar]
- [17].Gardin JM, Wong ND, Bommer W, Klopfenstein HS, Smith VE, Tabatznik B, et al. Echocardiographic design of a multicenter investigation of free-living elderly subjects: the Cardiovascular Health Study. J Am Soc Echocardiogr. 1992;5:63–72. doi: 10.1016/s0894-7317(14)80105-3. [DOI] [PubMed] [Google Scholar]
- [18].Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8. doi: 10.1016/0002-9149(86)90771-x. [DOI] [PubMed] [Google Scholar]
- [19].Psaty BM, Kuller LH, Bild D, Burke GL, Kittner SJ, Mittelmark M, et al. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–7. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- [20].Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–85. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- [21].Price TR, Psaty B, O'Leary D, Burke G, Gardin J. Assessment of cerebrovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:504–7. doi: 10.1016/1047-2797(93)90105-d. [DOI] [PubMed] [Google Scholar]
- [22].Gray RJ, Tsiatis AA. A linear rank test for use when the main interest is in differences in cure rates. Biometrics. 1989;45:899–904. [PubMed] [Google Scholar]
- [23].Harrell FE, Jr., Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982;247:2543–6. [PubMed] [Google Scholar]
- [24].Bacharova L, Szathmary V, Kovalcik M, Mateasik A. Effect of changes in left ventricular anatomy and conduction velocity on the QRS voltage and morphology in left ventricular hypertrophy: a model study. J Electrocardiol. 2010;43:200–8. doi: 10.1016/j.jelectrocard.2009.07.014. [DOI] [PubMed] [Google Scholar]
- [25].Bacharova L, Szathmary V, Potse M, Mateasik A. Computer simulation of ECG manifestations of left ventricular electrical remodeling. J Electrocardiol. 2012;45:630–4. doi: 10.1016/j.jelectrocard.2012.07.009. [DOI] [PubMed] [Google Scholar]
- [26].Armstrong AC, Gjesdal O, Almeida A, Nacif M, Wu C, Bluemke DA, et al. Left ventricular mass and hypertrophy by echocardiography and cardiac magnetic resonance: the multi-ethnic study of atherosclerosis. Echocardiography. 2014;31:12–20. doi: 10.1111/echo.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- [29].Bluemke DA, Kronmal RA, Lima JA, Liu K, Olson J, Burke GL, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–55. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Krumholz HM, Larson M, Levy D. Prognosis of left ventricular geometric patterns in the Framingham Heart Study. J Am Coll Cardiol. 1995;25:879–84. doi: 10.1016/0735-1097(94)00473-4. [DOI] [PubMed] [Google Scholar]