Abstract
Endoplasmic reticulum (ER) is the site of protein synthesis, protein folding, maintainance of calcium homeostasis, synthesis of lipids and sterols. Genetic or environmental insults can alter its function generating ER stress. ER senses stress mainly by three stress sensor pathways, namely protein kinase R-like endoplasmic reticulum kinase-eukaryotic translation-initiation factor 2α, inositol-requiring enzyme 1α-X-box-binding protein 1 and activating transcription factor 6-CREBH, which induce unfolded protein responses (UPR) after the recognition of stress. Recent studies have demonstrated that ER stress and UPR signaling are involved in cancer, metabolic disorders, inflammatory diseases, osteoporosis and neurodegenerative diseases. However, the precise knowledge regarding involvement of ER stress in different disease processes is still debatable. Here we discuss the possible role of ER stress in various disorders on the basis of existing literature. An attempt has also been made to highlight the present knowledge of this field which may help to elucidate and conjure basic mechanisms and novel insights into disease processes which could assist in devising better future diagnostic and therapeutic strategies.
Keywords: ER stress, UPR, Diseases, Chaperons
Introduction
Recent developments highlighting new insights into the endoplasmic reticulum (ER) stress regulated pathways, and their role in various diseases, have attracted immense attention towards this organelle. ER is a multifunctional organelle coordinating numerous functions fundamental for cell survival. It is the site of protein synthesis, protein folding, synthesis of lipids and sterols, maintenance of calcium homeostasis and post translational modifications of proteins [1–3]. Genetic or environmental insults can alter the functions of ER through calcium imbalance, redox imbalance, glucose starvation, altered glycosylation of glycoproteins and protein misfolding, each of which can induce ER stress [1–4]. In other words ER stress can be pictured as perturbation arising from failure in execution of functions assigned to ER or hindered working capacity of this organelle. To escape such adverse conditions, ER activates stress sensor pathway termed as unfolded protein response (UPR) through complex signaling network of Protein kinase R-like endoplasmic reticulum kinase-eukaryotic translation-initiation factor 2α (PERK-eIF2α), inositol-requiring enzyme 1α-X-box-binding protein 1 (IRE1-XBP1), activating transcription factor 6-CREBH (ATF6-CREBH) transducers. This signaling network initiates changes in the expression of hundreds of genes to restore cellular homeostasis. For instance, halting of the global protein synthesis, through general translation arrest, elevates the expression of ER chaperons which enhances protein folding so as to maintain the quality control of proteins while the misfolded proteins get degraded through the ER-associated degradation (ERAD) and autophagy. However, if the ER stress is prolonged, then UPR activates apoptotic signaling which may progress through mitochondrial dependent or independent pathways [Reviews; 5–8].
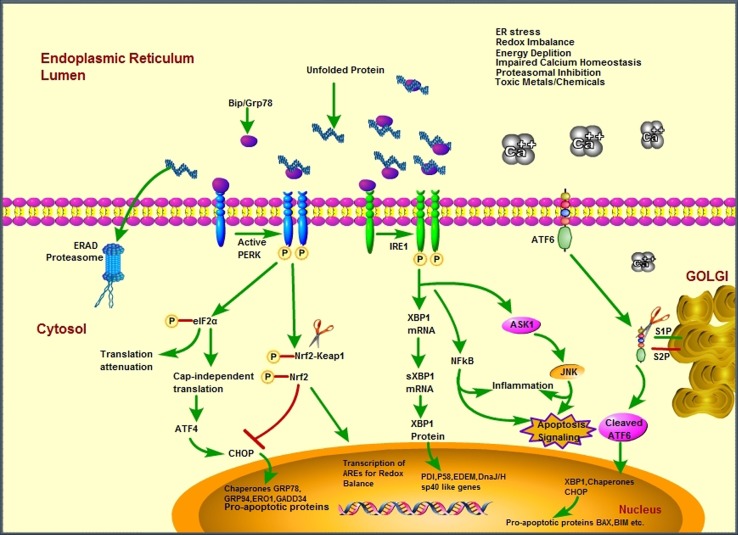
ER senses stress mainly by three stress sensors namely Protein kinase R-like endoplasmic reticulum kinase (PERK), inositol-requiring enzyme 1α (IRE1) and activating transcription factor 6 (ATF6). These sensors induce UPR after the recognition of ER stress/misfolding of proteins. During normalcy, ER-luminal domains of UPR transducers like IRE1, PERK and ATF6 are associated with the glucose-regulated protein 78 (Bip/Grp 78), an HSP 70 family protein. Bip/Grp 78 maintains the homeostasis of these signaling transducers. When ER is subjected to stress, Bip/Grp78 is sequestered by unfolded proteins in ER, resulting in its dissociation from the UPR transducers and hence activation of these molecules [2, 9–11] see Fig. 1.
Fig. 1.
Scheme illustrating the interplay between different signaling pathways induced in an event of unfolded protein response and subsequent endoplasmic reticulum dysfunction in human diseases
ER Stress and Apoptotic Signaling
Apoptosis, while on one hand, is fundamental to normal development and maintenance of tissue homeostasis, on the other, it is also a process by which physiologically normal cells may die under stress or unfavorable conditions. Apoptosis is implicated in several human diseases like diabetes, hepatic disorders, neurodegenerative disorders like Alzheimer’s and Parkinsons disease etc. Prolonged ER stress result into the activation of apoptotic signaling through UPR [12, 13]. During ER stress, calcium (Ca++) effluxes from the ER increase cytosolic Ca++ levels and disturb the mitochondrial membrane potential [14], which results into the release of cytochrome c and forms apoptosome complex with Apaf1 and caspase 9. This complex further activates the executioner caspases like caspase 3 and caspase 7 which leads to apoptosis [15–17]. ER membrane associated caspase 12 is also implicated in the activation of apoptosis through direct activation of caspase 3 or by caspase 9. CHOP/GADD153, sensor of endoplasmic reticulum stress, is highly up-regulated during ER stress [18, 19]. In our studies, caspase 12 activation was observed to be associated with enhanced intracellular calcium levels together with increased mRNA and protein levels of CHOP/GADD153 [20, 21]. CHOP is known to inhibit the expression of antiapoptotic Bcl2 family proteins and disturbs the ratio of Bax/Bcl2 [22, 23]. Several lines of evidences suggest that Bcl2 family member proteins are localized in both mitochondria and ER [24]. Whenever these organelles sense stress, the ratio of pro- and anti-apoptotic proteins gets disturbed which leads to initiation of apoptotic signaling. Furthermore, CHOP activates GADD34, which interacts with the phosphatase 1 and dephosphorylates eIf2α which results into the protein overload in ER [25–27]. IRE1α, an arm of UPR, induces apoptosis in ER stress through its association with TNF-receptor associated factor 2 (TRAF2) which activates caspase 12 and apoptosis signal regulating kinase 1 (ASK1) which in turn activates the pro-apoptotic signaling through c- Jun N-terminal kinase (JNK) [28, 29]. Disturbed apoptotic signaling is associated in various human diseases and the above reports clearly implicate the involvement of ER stress and UPR signaling in apoptosis.
ER Stress and Oxidative Stress
Reactive free radicals, including both reactive oxygen species (ROS) and reactive nitrogen species (RNS), could be substantially produced in response to multiple stresses, in different cellular sub compartments [30–32]. ER provides an exclusive oxidizing environment to the proteins to facilitate disulfide bond formation [33–35], and the ROS generated as a result of this process in ER alone contributes to 25 % of ROS generated by the cell [36]. Two enzymatic components, protein disulfide isomerase (PDI) and endoplasmic reticulum oxidoreductin (ERO-1) are often implicated in promoting oxidative stress in the ER compartment of the cell. PDI catalyzes disulfide bond formation between thiol moieties through thiol-disulfide oxidation, reduction, and isomerization. PDI which is itself reduced in the process is oxidized by ERO-1 via transfer of electrons from reduced PDI to molecular oxygen (O2) resulting in oxidative stress [37]. This may imply that oxidation of multiple disulfide bonds would generate high levels of cellular ROS. Further, any erroneous disulfide bonds so generated in the process are subsequently reduced by glutathione (GSH). This further diminishes the reduced glutathione pool altering the redox environment within the ER.
There are also evidences which suggest that ROS may be generated when accumulation of unfolded proteins in the ER elicits Ca2+ leakage into the cytosol through inositol trisphosphate receptor (IP3R) [36, 38]. The perturbed cytoplasmic calcium levels evoke influx of Ca2+ in the nuclei and mitochondria [39] resulting in generation of ROS. Since protein folding and refolding in the ER lumen are highly energy-dependent processes, ATP depletion consequential to protein misfolding may stimulate mitochondrial oxidative phosphorylation to increase ATP and ROS production. In addition, ER transmembrane protein NADPH oxidase complex, Nox4 may also be involved in producing superoxide anion and hydrogen peroxide [40].
Cellular oxidative stress leads to activation of antioxidant defense genes which are orchestrated mainly by the Nrf bZIP-family of transcription factors [20, 41, 42]. There are reports indicating possible relationship between Nrf bZIP-family proteins and ER stress defenses. Nrf1 and Nrf3 proteins of this family have been reported to be associated with the ER membrane and nuclear envelope which suggest their involvement in ER- related functions [43, 44]. A study in Caenorhabditis elegans [45] revealed that SKN-1, the Nrf ortholog, plays a critical role in resistance to oxidative and ER stress. Moreover, it has been reported that the response mobilized by SKN-1/Nrf under UPR is observed to be overlapping but still distinct from that evoked during oxidative stress conditions [45]. SKN-1/Nrf is reported to be activated by ER stress, independent of ROS signaling, and it provides resistance against reductive stress as well [45]. Furthermore, studies also report that PERK activates nuclear respiratory factor 2 (Nrf2) [17]. Nrf2 in turn regulates the protective mechanism within the cells against oxidative stress by the transcription of antioxidant enzymes. In unstressed cells Nrf2 resides in the cytoplasm, through its association with the kelch-like Ech-associated protein 1(Keap1), however, stress induces the dissociation of Nrf2 from keap1, enabling its nuclear translocation and activation. PERK is also known to phosphorylate Nrf2 [46, 47], during ER stress, leading to its nuclear accumulation, where it binds to the antioxidant response element (ARE) and induces transcription of antioxidant enzymes like heam oxygenase1 and glutathione S-transferase etc. [17] see Fig. 1. Hence, ER signaling has a broader impact on cellular stress defense networks that are critical in coordination of ER and cytoplasmic homeostasis.
ER Stress and Inflammatory Responses
ER stress and inflammatory responses are implicated in the pathogenesis of various diseases including neurodegenerative, respiratory, cardiovascular, cancer, diabetes and other metabolic diseases [48–51]. UPR signaling evokes inflammatory reactions, through three arms of UPR, that are PERK, IRE1 and ATF6, which in turn induce the activation of NF-κB [52, 53]. NF-κB generally resides in the cytoplasm, in inactive form through its association with IkB protein, which prevents its activation and nuclear translocation. Acute or chronic stress results into the activation of NF-κB by the proteosome based degradation of IkB. Studies have revealed that IRE1α degrades IkB and causes activation and nuclear translocation of NF-κB, while PERK activates NF-κB through translational suppression of IkB. Moreover, IRE1 activates AP1, a transcription factor that can induce the expression of tumor necrosis factor (TNF), keratinocyte growth factor (KGF), granulocyte macrophage colony-stimulating factor (GM-CSF), interleukin (IL)-8, and certain cytokine receptors [54–56]. Furthermore, UPR via ATF6 [52, 53] has been implicated in the activation of acute phase response (APR), which is generated immediately after tissue damage, infection and inflammation etc. Acute phase proteins (APPs) concentration increases in serum after the onset of above conditions, ultimately causing fever, neurological and pathological changes.
NLRP3 inflammasome has recently been recognized as an innate immune signaling receptor that plays key role in mediating cell responses to various endo- and exogenous signals. Recent reports indicate that inflammasomes play a critical role in a number of autoimmune and metabolic diseases. NF-κB activates pro-IL1β which is converted to mature IL1β by the NLRP3, ASC and caspase 1 complex [57, 58]. Moreover, ROS and lysosomal damage also activates NALP3 inflammasome pathway and induce pro-inflammatory reactions. Reports clearly indicate that ER stress induces pro IL1β and NLRP3 inflammasome activation [59, 60] through NF-κB pathway. The findings thus surmise the role of ER stress in inflammatory pathways and its related diseases.
ER Stress and Osteoporosis
Osteoporosis is a major health problem in ageing population. It is characterized by reduced bone strength due to which susceptibility of fractures is common. Low bone mineral density (BMD) which is the hallmark of osteoporosis, has been related to ER stress. PERK-eIf2α signaling is required for normal development of the postnatal growth, function and viability of pancreas and skeletal system [61, 62]. A study by Jie Liu et al. showed that low BMD haplotype is distinct, due to associated single nucleotide polymorphism, which is exhibited by increased phosphorylation of eIF2α during ER stress, as compared to alternate haplotype [63]. The balance between osteoblasts (the mesenchymal stem cells derived bone forming cells) and osteoclasts (the hematopoietic stem cells derived bone resorption cells) is very important for the normal functioning and development of bone [64–66]. He et al. reported that blocking of dephosphorylation of eIf2α by Salubrinal increases the osteoblast differentiation. They also hypothesized that ER-stress regulation through eIF2α and ATF4 could be a good system for antiosteoporosis [67]. Diabetic patients are more prone to fractures especially that of hip and upper extremities as compared with the non-diabetics [68]. Insulinopenia and hyperglycemia cause low BMD which impairs bone formation [69]. Moreover, it is reported that diabetes itself induces expression of ER stress specific CHOP in osteoblast cells resulting in the progression of apoptosis in these cells [70]. Therefore, the balance between the osteoblasts and osteoclasts are disturbed which leads to the bone disorders and development of diabetic osteoporosis [70]. IRE1α-XBP1 pathways are crucial for osteoblast maturation and play important role in bone formation and bone resorption under pathological conditions [71]. Furthermore, there are reports that ER specific molecular chaperones like BiP (immunoglobulin heavy-chain binding protein) and PDI (protein-disulfide isomerase) are down-regulated in osteoblasts obtained from osteoporosis patients [72]. These findings suggest the importance of ER stress in osteoporosis, skeletal development and also for devising therapeutic strategies against skeletal diseases.
ER Stress and Cancer
There are reports that cancer cells require high protein folding capacity of ER chaperons due to their enhanced rate of growth and proliferation. The characteristics of tumor microenvironment like hypoxia, redox imbalance, pH fluctuations and nutrient starvation are the inducers of UPR [73]. Moreover, it has been reported that UPR signaling is upregulated in cancer cells [8]. It is also reported that the redox imbalance due to hypoxic condition in cancer cells results in the activation of UPR pathway. Studies have also shown that Grp78 is highly expressed in prostate, lung, breast and colon cancers [74–81]. Furthermore, a study showed that cells which do not expresse Grp78 are unable to form tumor [82]. The above studies validate the importance of Grp78 chaperon in tumor formation. In essence, Grp78 increases the protein folding capacity of ER thus reducing stress evoked cell death in cancer cells. The PERK arm of the UPR also plays important role in tumor proliferation and survival. Inactivation of the PERK pathway by either generating mutations in the kinase domain of PERK or introducing a phosphorylation-resistant form of eIF2α impairs cell survival under extreme hypoxia [83]. Furthermore, PERK limits oxidative DNA damage through Nrf2 activation which further promotes cancer cell proliferation and survival [84]. The involvement of UPR in cancer is currently promising therapeutic target for the treatment of cancer [85].
Tumor suppressor gene TP53, which is activated during different stressful conditions, plays pivotal role in several biological mechanisms including promotion of cell cycle arrest, senescence and apoptosis, [86–90]. TP53 regulation in ER stress is debatable. Studies have revealed that ER stress stabilizes p53 activity and induces p53 mediated apoptosis. On the other end, reports also showed that ER stress induced downregulation of p53 by Gsk3β [91, 92]. In a report from our lab downregulation of p53 was observed in response to aluminium mediated ER stress in SHSY-5Y cells [20]. Moreover, in a clinical setting, tumorigenesis as well as the efficacy of therapy may be influenced by the ability of ER stress to inhibit p53. This would confer resistance to the inhibitory effect of ER stress on p53 functionality and may prove disastrous to tumors that retain wild type p53 gene. Such an effect would enable the cancerous cells to resist DNA damaging effect of agents used in cancer treatment. In such an event, inhibiting ER stress may serve as a useful strategy to augment the efficacy of therapy directed against cancer progression.
ER Stress and Neurodegeneration
Causes of neurodegenerative disorders are multi-factorial including redox imbalance, environmental factors, genetic predisposition, glutamate-induced excitotoxicity, neuroinflammation, disruption in Ca2+ levels, mitochondrial dysfunction and misfolded protein accumulation. In this section of the review we have focused on the relationship between ER stress in terms of UPR activation and its role in neurodegenerative diseases. Accumulation of misfolded proteins is a distinguishing aspect of many neurodegenerative diseases including Alzheimer’s [93] and Parkinson’s disease [94]. As discussed above accumulation of misfolded proteins causes ER stress and activates UPR. Here we discuss the role of UPR in two major neurodegenerative diseases, i.e. AD and PD.
ER Stress and Alzheimer’s Disease
Alzheimer’s disease is characterized by the deposition of toxic senile plaques of β amyloid protein and intracellular neurofibrillary tangles containing hyperphosphorylated tau [95]. The β amyloid proteins are formed as a result of cleavage of amyloid precursor protein (APP) by the action of β-secretase (BACE) and ϒ-secretase. ER stress sensors IRE1 and PERK are greatly influenced by presenilin protein, which is an integral membrane protein and a part of the ϒ-secretase complex, and is widely expressed in both ER and Golgi apparatus [96]. Reports indicate that mutated presenilin reduces the phosphorylation of PERK- eIF2α pathway which results in the accumulation of proteins in ER [97]. Moreover, studies report increased PERK and eIF2α levels in hippocampus neurons of AD brain [98, 99]. These observations necessitate further experimentation to carefully dissect the PERK-eIF2α pathway in AD. Furthermore, mutant presenilin 1 inhibits IRE1 signalling, which in turn stalls or suppresses the transcription of ER chaperones such as GRP78, which has been reported to be down-regulated in AD [97]. XBP1, also implicated in AD, is known to control diverse cell type- and context-dependent transcriptional regulatory networks [100]. Modulation of IRE1 activity can reduce or delay splicing of XBP1, thus switching signalling to a pro-death response [101].
Generation of Aβ, a characteristics hallmark of AD, is also associated with ER [102, 103]. Aβ is reported to induce Ca2+ release from ER stores [104]. However, reports also suggest that influx of Ca2+, through calcium channels located on plasma membrane or ER membrane, increases Aβ generation [105] by alteration in the metabolism and production of Aβ. Whatsoever may be the cause there is no doubt that an intricate relationship exist between Ca2+ dysfunction and AD [106]. Furthermore, Ca2+ homeostasis is essential for the proper functioning of ER chaperons and protein folding. In our previous study we observed an association between increased intracellular calcium and Aβ(1–40) levels in neuronal cells apart from enhanced CHOP and caspase12 levels [20]. It may be stated that another characteristic feature of AD is tau pathology. Tau is a microtubule associated protein present in neurons which maintains microtubule assembly and stabilization. ER stress is normally linked with the early stages of tau pathology [107, 108]. Tau proteins become hyperphosphorylated in pathological conditions, which results in its dissociation from microtubule assembly into unusual toxic filaments [109]. The unfolded protein response activated in pretangle neurons in AD hippocampus has been shown to be closely associated with the presence of phosphorylated tau (p-tau) and GSK-3β [98]. These findings elicit activation of UPR in AD neurons at an early stage of neurofibrillary degeneration. Moreover, prolonged activation of UPR may be involved in both tau phosphorylation and neurodegeneration in AD pathogenesis [110].
ER Stress and Parkinson’s Disease
Parkinson’s disease (PD) is characterized by the loss of dopaminergic neurons in the substantia nigra pars compacta along with the presence of intraneuronal cytoplasmic inclusion bodies, known as Lewy bodies in the neurons [111]. Most of the cases of PD, up to 90 %, are sporadic while only 5–10 % of patients show monogenic form of the disease [112]. Recent studies investigating implication of ER stress in the pathophysiology of PD have reported increased UPR activity in the affected brain regions of PD patients and also in patients suffering from the related multi-systems atrophy syndrome [113, 114]. It has been reported by Silva et al. [115], that deficiency of CHOP, a key ER stress marker, protects the neonatal striatum from neurotoxicant 6-hydroxydopamine. Reports also showed that forced expression of ER stress sensor proteins, ATF6 alpha [117] and spliced XBP1 [116], confines neurotoxin-induced dopaminergic neuronal death [117]. These reports are indicative of the role of ER stress in the death and dysfunction of dopaminergic neurons exposed to neurotoxicant models of PD.
Accumulation of misfolded proteins like α-synuclein and Parkin-associated endothelin receptor-like receptor (Pael-R) has been reported to be a key event which triggers UPR in the ER. α-synuclein is an autosomal dominant PD gene expressed in synaptic vesicles and in nervous tissue. Post-translational modifications, like phosphorylation and nitrosylation, of α-synuclein can cause misfolding and later deposition of the protein into Lewy bodies in the substantia nigra of PD patients [118]. Smith et al. [119] reported that A53T mutation in α-synuclein activates UPR resulting in increased expression of CHOP and GRP78 and increased phosphorylation of eIF2 α. Furthermore, the authors also reported that suppressing UPR through inhibition of eIF2α phosphorylation protected the A53T mutant α-synuclein-overexpressing cells from cell death. These reports suggest that UPR mediates shift of the balance towards apoptosis [119]. Moreover, mutations in leucine-rich repeat kinase 2 (LRRK2), also an autosomal dominant PD gene, causes impairment in protein degradation pathways, accumulation of oxidized proteins, impairment of the autophagy-lysosomal pathway, accumulation of α-synuclein and ubiquitinated proteins [120]. LRRK2 has been observed to localize in core of Lewy bodies [121] and is known to upregulate GRP78, a key cell survival molecule during ER stress [122]. In addition to α-synuclein and LRRK2, Pael-R has also been detected to accumulate in the core of Lewy bodies in sporadic PD [123]. Parkin, an autosomal recessive PD gene, is an E3 ubiquitin ligase that plays an important role in protein degradation of the misfolded Pael-R [124]. Mutational loss of E3 activity of parkin has been observed to cause unfolded Pael-R to accumulate and finally induce ER stress mediated cell death [125].Therefore, ER stress generated in response to accumulation of unfolded Pael-R is suggested to be another pathophysiological mechanism underlying autosomal recessive PD [126–128].
The above findings discussed in relation to AD and PD illustrate the paramount significance of ER stress in development and progression of these diseases. Scientific literature similarly supports the involvement of ER stress in other neurodegenerative disorders like Amyotrophic lateral sclerosis, Huntington diseases and Prions disease etc. (see reviews Cláudia [110], Omura et al. [128], Lindholm et al. [5]).
Conclusion
It may be concluded that ER plays a crucial role in protein synthesis and folding. UPR which forms the critical arm of ER stress signaling, gets activated in response to stress and times when ER stress is prolonged, UPR assumes adverse role, through disruption of cellular homeostasis. Overall the existing literature clearly indicates the role of ER stress in health and diseases (Table 1). Furthermore, dissection of ER stress signaling could unravel new avenues that may potentially be exploited for developing future therapeutics to address ER stress-related anomalies.
Table 1.
Role of UPR transducers and proteins in different human diseases
| Protein | Function | Disease | References |
|---|---|---|---|
| IRE1 | UPR sensor | Human somatic cancers; Alzheimer’s disease; Parkinson’s disease; ALS | [97, 129, 130, 131, 132] |
| CREBH | Regulate expression of PPARα, HNF4α, and ATF6 α | Extreme hypertriglyceridemia | [133, 134, 135] |
| ATF6α | UPR sensor | Type 2 diabetes and pre-diabetic traits; Increased plasma cholesterol levels; Alzheimer’s disease; ALS | [97, 136, 137, 138, 139] |
| PERK | UPR sensor | Wolcott–Rallison syndrome; Alzheimer’s disease; Wolcott–Rallison syndrome; supranuclear palsy; ALS | [5, 97, 98, 131, 140, 141, 142] |
| ATF4 | UPR sensor | Parkinson’s disease | [143] |
| Grp78 (BiP) | Senses ER stress, accumulation of misfolded proteins and regulate expression of ATF6α and ATF4 | Bipolar disorder; Alzheimer’s disease | [144, 145, 146, 147] |
| PPT1 | Palmitoylprotein thioesterase-1 | Batten disease/infantile neuronal ceroid lipofuscinosis | [148] |
| CHOP | Regulate expression of ATF4 and ATF6α | Early-onset type 2 diabetes in Italians | [116, 149, 150, 151, 152] |
| WFS1 | Regulate expression of XBP1 s | Wolfram syndrome; risk of type 2 diabetes in Japanese and European populations | [153, 154, 155, 156] |
| XBP1? | UPR sensor | Bipolar disease | [157, 158] |
? Denotes discrepancy in outcome of studies exploring the relation between XBP1 and bipolar disorder
Acknowledgments
This work was supported by Indian Council of Medical Research (ICMR) [Project No. 45/6/2013 BIO/BMS] and [Project No. 45/9/2013 Nan/BMS]. We are grateful to Indian Council of Medical Research (ICMR) for award of fellowships to SHMR and AP.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Paschen W, Frandsen A. Endoplasmic reticulum dysfunction a common denominator for cell injury in acute and degenerative diseases of the brain? J Neurochem. 2001;79:719–725. doi: 10.1046/j.1471-4159.2001.00623.x. [DOI] [PubMed] [Google Scholar]
- 2.Schroder M, Kaufman RJ. ER stress and the unfolded protein response. Mutat Res. 2005;569:29–63. doi: 10.1016/j.mrfmmm.2004.06.056. [DOI] [PubMed] [Google Scholar]
- 3.Rao RV, Ellerby HM, Bredesen DE. Coupling endoplasmic reticulum stress to the cell death program. Cell Death Differ. 2004;11:372–380. doi: 10.1038/sj.cdd.4401378. [DOI] [PubMed] [Google Scholar]
- 4.Breckenridge DG, Germain M, Mathai JP, Nguyen M, Shore GC. Regulation of apoptosis by endoplasmic reticulum pathways. Oncogene. 2003;22:8608–8618. doi: 10.1038/sj.onc.1207108. [DOI] [PubMed] [Google Scholar]
- 5.Lindholm D, Wootz H, Korhonen L. ER stress and neurodegenerative diseases. Cell Death Differ. 2006;13:385–392. doi: 10.1038/sj.cdd.4401778. [DOI] [PubMed] [Google Scholar]
- 6.Zhao L, Ackerman SL. Endoplasmic reticulum stress in health and disease. Curr Opin Cell Biol. 2006;18:444–452. doi: 10.1016/j.ceb.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Doyle KM, Kennedy D, Gorman AM, Gupta S, Healy SJ, Samali A. Unfolded proteins and endoplasmic reticulum stress in neurodegenerative disorders. J Cell Mol Med. 2011;15:2025–2039. doi: 10.1111/j.1582-4934.2011.01374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang S, Kaufman RJ. The impact of the unfolded protein response on human disease. J Cell Biol. 2012;197(7):857–867. doi: 10.1083/jcb.201110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertolotti A, Zhang Y, Hendershot LM, Harding HP, Ron D. Dynamic interaction of BiP and ER stress transducers in the unfoldedprotein response. Nat Cell Biol. 2000;2:326–332. doi: 10.1038/35014014. [DOI] [PubMed] [Google Scholar]
- 10.Ma K, Vattem KM, Wek RC. Dimerization and release of molecular chaperone inhibition facilitate activation of eukaryotic initiation factor- 2 kinase in response to endoplasmic reticulum stress. J Biol Chem. 2002;2002(277):18728–18735. doi: 10.1074/jbc.M200903200. [DOI] [PubMed] [Google Scholar]
- 11.Shen J, Chen X, Hendershot L, Prywes R. ER stress regulation of ATF6 localization by dissociation of BiP/GRP78 binding and unmasking of Golgi localization signals. Dev Cell. 2002;3:99–111. doi: 10.1016/S1534-5807(02)00203-4. [DOI] [PubMed] [Google Scholar]
- 12.Jäger R, Bertrand MJ, Gorman AM, Vandenabeele P, Samali A. The unfolded protein response at the crossroads of cellular life and death during endoplasmic reticulum stress. Biol Cell. 2012;104:259–270. doi: 10.1111/boc.201100055. [DOI] [PubMed] [Google Scholar]
- 13.Gorman AM, Healy SJ, Jäger R, Samali A. Stress management at the ER: regulators of ER stress-induced apoptosis. Pharmacol Ther. 2012;134:306–316. doi: 10.1016/j.pharmthera.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Logue SE, Cleary P, Saveljeva S, Samali A. New directions in ER stress-induced cell death. Apoptosis. 2013;18:537–546. doi: 10.1007/s10495-013-0818-6. [DOI] [PubMed] [Google Scholar]
- 15.Bravo R, Gutierrez T, Paredes F, Gatica D, Rodriguez AE, Pedrozo Z, et al. Endoplasmic reticulum: ER stress regulates mitochondrial bioenergetics. Int J Biochem Cell Biol. 2012;44:16–20. doi: 10.1016/j.biocel.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bravo R, Vicencio JM, Parra V, Troncoso R, Munoz JP, Bui M, et al. Increased ERmitochondrial coupling promotes mitochondrial respiration and bioenergetics during early phases of ER stress. J Cell Sci. 2011;124:2143–2152. doi: 10.1242/jcs.080762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szegezdi E, MacDonald DC, Ni Chonghaile T, Gupta S, Samali A. Bcl-2 family on guard at the ER. Am J Physiol Cell Physiol. 2009;296:941–953. doi: 10.1152/ajpcell.00612.2008. [DOI] [PubMed] [Google Scholar]
- 18.Sánchez AM, Martínez-Botas J, Malagarie-Cazenave S, Olea N, Vara D, Lasunción MA, et al. Induction of the endoplasmic reticulum stress proteinGADD153/CHOP by capsaicin in prostate PC-3 cells: a microarray study. Biochem Biophys Res Commun. 2008;372:785–791. doi: 10.1016/j.bbrc.2008.05.138. [DOI] [PubMed] [Google Scholar]
- 19.Zinszner H, Kuroda M, Wang X, Batchvarova N, Lightfoot RT, Remotti H, et al. CHOP is implicated in programmed cell death in response to impaired function of the endoplasmic reticulum. Genes Dev. 1998;12:982–995. doi: 10.1101/gad.12.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rizvi SHM, Parveen A, Verma AK, Ahmad I, Arshad M, Mahdi AA. Aluminium induced endoplasmic reticulum stress mediated cell death in SH-SY5Y neuroblastoma cell line is independent of p53. PLoS One. 2014;9(5):e98409. doi: 10.1371/journal.pone.0098409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parveen A, Rizvi SHM, Mahdi F, Tripathi S, Ahmad I, Mahdi AA, et al. Silica nanoparticles mediated neuronal cell death in corpus striatum of rat brain: implication of mitochondrial, endoplasmic reticulum and oxidative stress. J Nanopart Res. 2014;16:2664. doi: 10.1007/s11051-014-2664-z. [DOI] [Google Scholar]
- 22.McCullough KD, Martindale JL, Klotz LO, Aw TY, Holbrook NJ, et al. Gadd153 sensitizes cells to endoplasmic reticulum stress by down-regulating Bcl2 and perturbing the cellular redox state. Mol Cell Biol. 2001;21:1249–1259. doi: 10.1128/MCB.21.4.1249-1259.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim H, Tu HC, Ren D, Takeuchi O, Jeffers JR, Zambetti GP, et al. Stepwise activation of BAX and BAK by tBID, BIM, and PUMA initiates mitochondrial apoptosis. Mol Cell. 2009;36:487–499. doi: 10.1016/j.molcel.2009.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodriguez D, Rojas-Rivera D, Hetz C. Integrating stress signals at the endoplasmic reticulum: the BCL-2 protein family rheostat. Biochim Biophys Acta. 2011;1813:564–574. doi: 10.1016/j.bbamcr.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 25.Novoa I, Zeng H, Harding HP, Ron D. Feedback inhibition of the unfolded protein response by GADD34- mediated dephosphorylation of eIF2α. J Cell Biol. 2001;153:1011–1021. doi: 10.1083/jcb.153.5.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brush MH, Weiser DC, Shenolikar S. Growth arrest and DNA damage-inducible protein GADD34 targets protein phosphatase 1α to the endoplasmic reticulum and promotes dephosphorylation of the α subunit of eukaryotic translation initiation factor 2. Mol Cell Biol. 2003;23:1292–1303. doi: 10.1128/MCB.23.4.1292-1303.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kojima E, Takeuchi A, Haneda A, Yagi A, Hasegawa T, Yamaki K, et al. The function of GADD34 is a recovery from a shutoff of protein synthesis induced by ER stress: elucidation by GADD34-deficient mice. FASEB J. 2003;17:1573–1575. doi: 10.1096/fj.02-0462com. [DOI] [PubMed] [Google Scholar]
- 28.Yoneda T, Imaizumi K, Oono K, Yui D, Gomi F, Katayama T, et al. Activation of Caspase- 12, an endoplastic reticulum (ER) resident caspase, through tumor necrosis factor receptor-associated factor 2-dependent mechanism in response to the ER stress. J Biol Chem. 2001;276:13935–13940. doi: 10.1074/jbc.M010677200. [DOI] [PubMed] [Google Scholar]
- 29.Tabas I, Ron D. Integrating the mechanisms of apoptosis induced by endoplasmic reticulum stress. Nat Cell Biol. 2011;13:184–190. doi: 10.1038/ncb0311-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parveen A, Rizvi SHM, Gupta A, Singh R, Ahmad I, Mahdi F, et al. NMR-based metabonomics study of sub-acute hepatotoxicity induced by silica nanoparticles in rats after intranasal exposure. Cell Mol (Noisy-le-Grand France) 2012;58:196–203. [PubMed] [Google Scholar]
- 31.Tripathi S, Mahdi AA, Nawab A, Chander R, Hasan M, Siddiqui MS, et al. Influence of age on aluminum induced lipid peroxidation and neurolipofuscin in frontal cortex of rat brain: abehavioral, biochemical and ultrastructural study. Brain Res. 2009;1253:107–116. doi: 10.1016/j.brainres.2008.11.060. [DOI] [PubMed] [Google Scholar]
- 32.Tripathi S, Somashekar BS, Mahdi AA, Gupta A, Mahdi F, Hasan M, et al. Aluminum-mediated metabolic changes in rat serum and urine: a proton nuclear magnetic resonance study. J Biochem Mol Toxicol. 2008;22:119–127. doi: 10.1002/jbt.20219. [DOI] [PubMed] [Google Scholar]
- 33.Gorlach A, Klappa P, Kietzmann T. The endoplasmic reticulum: folding, calcium homeostasis, signaling, and redox control. Antioxid Redox Signal. 2006;8:1391–1418. doi: 10.1089/ars.2006.8.1391. [DOI] [PubMed] [Google Scholar]
- 34.Tu BP, Weissman JS. Oxidative protein folding in eukaryotes: mechanisms and consequences. J Cell Biol. 2004;164:341–346. doi: 10.1083/jcb.200311055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sevier CS, Kaiser CA. Ero1 and redox homeostasis in the endoplasmic reticulum. Biochim Biophys Acta. 2008;1783:549–556. doi: 10.1016/j.bbamcr.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 36.Malhotra JD, Kaufman RJ. Endoplasmic reticulum stress and oxidative stress: a vicious cycle or a double-edged sword? Antioxid Redox Signal. 2007;9:2277–2293. doi: 10.1089/ars.2007.1782. [DOI] [PubMed] [Google Scholar]
- 37.Higa A, Chevet E. Redox signaling loops in the unfolded protein response. Cell Signal. 2012;24:1548–1555. doi: 10.1016/j.cellsig.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 38.Cioffi DL. Redox regulation of endothelial canonical transient receptor potential channels. Antioxid Redox Signal. 2011;15:1567–1582. doi: 10.1089/ars.2010.3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murphy MP. How mitochondria produce reactive oxygen species. Biochem J . 2009;417:1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Santos CX, Tanaka LY, Wosniak J, Laurindo FR. Mechanisms and implications of reactive oxygen species generation during the unfolded protein response: roles of endoplasmic reticulum oxidoreductases, mitochondrial eletron transport, and NADPH oxidase. Antioxid Redox Signal. 2009;11:2409–2427. doi: 10.1089/ars.2009.2625. [DOI] [PubMed] [Google Scholar]
- 41.Harding HP, Zhang Y, Zeng H, Novoa I, Lu PD, Calfon M, et al. An integrated stress response regulates amino acid metabolism and resistance to oxidative stress. Mol Cell. 2003;2003(11):619–633. doi: 10.1016/S1097-2765(03)00105-9. [DOI] [PubMed] [Google Scholar]
- 42.Rizvi F, Shukla S, Kakkar P. Essential role of PH domain and leucine-rich repeat protein phosphatase 2 in Nrf2 suppression via modulation of Akt/GSK3β/Fyn kinase axis during oxidative hepatocellular toxicity. Cell Death Dis. 2014;27(5):e1153. doi: 10.1038/cddis.2014.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chevillard G, Blank V. NFE2L3 (NRF3): the Cinderella of the Cap‘n’Collar transcription factors. Cell Mol Life Sci. 2011;68:3337–3348. doi: 10.1007/s00018-011-0747-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang Y, Hayes JD. Identification of topological determinants in the N-terminal domain of transcription factor Nrf1 that control its orientation in the endoplasmic reticulum membrane. Biochem J . 2010;430:497–510. doi: 10.1042/BJ20100471. [DOI] [PubMed] [Google Scholar]
- 45.Glover-Cutter KM, Lin S, Blackwell TK. Integration of the unfolded protein and oxidative stress responses through SKN-1/Nrf. PLoS Genet. 2013;9(9):e1003701. doi: 10.1371/journal.pgen.1003701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cullinan SB, Diehl JA. PERK-dependent activation of Nrf2 contributes to redox homeostasis and cell survival following endoplasmic reticulum stress. J Biol Chem. 2004;279:20108–20117. doi: 10.1074/jbc.M314219200. [DOI] [PubMed] [Google Scholar]
- 47.Cullinan SB, Zhang D, Hannink M, Arvisais E, Kaufman RJ, Diehl JA. Nrf2 is a direct PERK substrate and effector of PERKdependent cell survival. Mol Cell Biol. 2003;23:7198–7209. doi: 10.1128/MCB.23.20.7198-7209.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garg AD, Kaczmarek A, Krysko O, Vandenabeele P, Krysko DV, Agostinis P. ER stress induced inflammation: does it aid or impede disease progression? Trends Mol Med. 2012;10:589–598. doi: 10.1016/j.molmed.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 49.Chaudhari N, Talwar P, Parimisetty A, Lefebvre d’Hellencourt C, Ravanan P. A molecular web: endoplasmic reticulum stress, inflammation, and oxidative stress. Front Cell Neurosci. 2014;29(8):213. doi: 10.3389/fncel.2014.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lin JH, Walter P, Yen TSB. Endoplasmic reticulum stress in disease pathogenesis. Annu Rev Pathol. 2008;3:399–425. doi: 10.1146/annurev.pathmechdis.3.121806.151434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hotamisligil GS. Role of endoplasmic reticulum stress and c- Jun NH2-terminal kinase pathways in inflammation and origin of obesity and diabetes. Diabetes. 2005;54(Suppl 2):S73–S78. doi: 10.2337/diabetes.54.suppl_2.S73. [DOI] [PubMed] [Google Scholar]
- 52.Verfaillie T, Garg AD, Agostinis P. Targeting ER stress induced apoptosis and inflammation in cancer. Cancer Lett. 2010;332(2):249–264. doi: 10.1016/j.canlet.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 53.Hotamisligil GS, Erbay E. Nutrient sensing and inflammation in metabolic diseases. Nat Rev Immunol. 2008;8:923–934. doi: 10.1038/nri2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang K, Kaufman RJ. From endoplasmic-reticulumstress to the inflammatory response. Nature. 2008;454:455–462. doi: 10.1038/nature07203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rius J, Guma J, Schachtrup J, Akassoglou J, Zinkernagel J, Nizet J, et al. NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1alpha. Nature. 2008;453:807–811. doi: 10.1038/nature06905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Angel P, Szabowski A, Schorpp-Kistner M, et al. Function and regulation of AP-1 subunits in skin physiology and pathology. Oncogene. 2001;20:2413–2423. doi: 10.1038/sj.onc.1204380. [DOI] [PubMed] [Google Scholar]
- 57.Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17:179–188. doi: 10.1038/nm.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Horng T, Hotamisligil GS. Linking the inflammasome to obesity-related disease. Nat Med. 2011;17:164–165. doi: 10.1038/nm0211-164. [DOI] [PubMed] [Google Scholar]
- 59.Shenderov K, Riteau N, Yip R, Mayer-Barber KD, Oland S, Hieny S, et al. Cutting edge:endoplasmic reticulum stress liceses macrophages to produce mature IL-1beta in response toTLR4stimulation through a caspase-8- and TRIF-dependent pathway. J Immunol. 2014;192:2029–2033. doi: 10.4049/jimmunol.1302549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Oslowski CM, Hara T, O’sullivan-Murphy B, Kanekura K, Lu S, Hara M, et al. Thioredoxin-interacting protein mediates ERstress-induced beta cell death through initiation of the inflammasome. Cell Metab. 2012;16:265–273. doi: 10.1016/j.cmet.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang P, McGrath B, Li S, Frank A, Zambito F, Reinert J, et al. The PERK eukaryotic initiation factor 2 alpha kinase is required for the development of the skeletal system, postnatal growth, and the function and viability of the pancreas. Mol Cell Biol. 2002;22:3864–3874. doi: 10.1128/MCB.22.11.3864-3874.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Harding HP, Zeng H, Zhang Y, Jungries R, Chung P, Plesken H, et al. Diabetes mellitus and exocrine pancreatic dysfunction in perk-/- mice reveals a role for translational control in secretory cell survival. Mol Cell. 2001;7:1153–1163. doi: 10.1016/S1097-2765(01)00264-7. [DOI] [PubMed] [Google Scholar]
- 63.Liu J, Hoppman N, O’Connell JR, Wang H, Streeten EA, McLenithan JC, et al. A functional haplotype in EIF2AK3, an ER stress sensor, is associated with lower bone mineral density. J Bone Miner Res. 2012;27:33–41. doi: 10.1002/jbmr.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Goltzman D. Discoveries, drugs and skeletal disorders. Drug Discov. 2002;1(10):784–796. doi: 10.1038/nrd916. [DOI] [PubMed] [Google Scholar]
- 65.Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423(6937):337–342. doi: 10.1038/nature01658. [DOI] [PubMed] [Google Scholar]
- 66.Aubin JE. Regulation of osteoblast formation and function. Rev Endocr Metab Disord. 2001;2(1):81–94. doi: 10.1023/A:1010011209064. [DOI] [PubMed] [Google Scholar]
- 67.He L, Lee J, Jang JH, Sakchaisri K, Hwang J, Cha-Molstad HJ. Osteoporosis regulation by salubrinal through eIF2α mediated differentiation of osteoclast and osteoblast. Cell Signal. 2013;25(2):552–560. doi: 10.1016/j.cellsig.2012.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Norris R, Parker M. Diabetes mellitus and hip fracture: a study of 5966 cases. Injury. 2011;42:1313–1316. doi: 10.1016/j.injury.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 69.Follak N, Kloting I, Merk H. Influence of diabetic metabolic state on fracture healing in spontaneously diabetic rats. Diabetes Metab Res Rev. 2005;21:288–296. doi: 10.1002/dmrr.537. [DOI] [PubMed] [Google Scholar]
- 70.Liu W, Zhu X, Wang Q, Wang L. Hyperglycemia induces endoplasmic reticulum stress-dependent CHOP expression in osteoblasts. Exp Ther Med. 2013;5(5):1289–1292. doi: 10.3892/etm.2013.978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tohmonda T, Chiba K, Toyama Y, Horiuchi K. Unfolded protein response mediator, the IRE1α-XBP1 pathway is involved in osteoblast differentiation. Arthritis Res Ther. 2012;14(Suppl 1):P70. doi: 10.1186/ar3671. [DOI] [Google Scholar]
- 72.Hino S, Kondo S, Yoshinaga K, Saito A, Murakami T, Kanemoto S, et al. Regulation of ER molecular chaperone prevents bone loss in a murine model for osteoporosis. J Bone Miner Metab. 2010;28(2):131–138. doi: 10.1007/s00774-009-0117-z. [DOI] [PubMed] [Google Scholar]
- 73.Schonthal AH. Pharmacological targeting of endoplasmic reticulum stress signaling in cancer. Biochem Pharmacol. 2013;85:653–666. doi: 10.1016/j.bcp.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 74.Fernandez PM, Tabbara SO, Jacobs LK, Manning FC, Tsangaris TN, Schwartz AM, et al. Overexpression of the glucose-regulated stress gene GRP78 in malignant but not benign human breast lesions. Breast Cancer Res Treat. 2000;59:15–26. doi: 10.1023/A:1006332011207. [DOI] [PubMed] [Google Scholar]
- 75.Lee AS. GRP78 induction in cancer: therapeutic and prognostic implications. Cancer Res. 2007;67:3496–3499. doi: 10.1158/0008-5472.CAN-07-0325. [DOI] [PubMed] [Google Scholar]
- 76.Li J, Lee AS. Stress induction of GRP78/BiP and its role in cancer. Curr Mol Med. 2006;6:45–54. doi: 10.2174/156652406775574523. [DOI] [PubMed] [Google Scholar]
- 77.Uramoto H, Sugio K, Oyama T, Nakata S, Ono K, Yoshimastu T, et al. Expression of endoplasmic reticulum molecular chaperone Grp78 in human lung cancer and its clinical significance. Lung Cancer. 2005;49:55–62. doi: 10.1016/j.lungcan.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 78.Wang Q, He Z, Zhang J, Wang Y, Wang T, Wang T, Tong S, et al. Over expression of endoplasmic reticulum molecular chaperone GRP94 and GRP78 in human lung cancer tissues and its significance. Cancer Detect Prev. 2005;29:544–551. doi: 10.1016/j.cdp.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 79.Wang XP, Qiu FR, Liu GZ, Chen RF. Correlation between clinicopathology and expression of heat shock protein 70 and glucose-regulated protein 94 in human colonic adenocarcinoma. World J Gastroenterol. 2005;11:1056–1059. doi: 10.3748/wjg.v11.i7.1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zheng HC, Takahashi H, Li XH, Hara T, Masuda S, Guan YF, et al. Overexpression of GRP78 and GRP94 are markers for aggressive behavior and poor prognosis in gastric carcinomas. Hum Pathol. 2008;39:1042–1049. doi: 10.1016/j.humpath.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 81.Dong D, Ni M, Li J, Xiong S, Ye W, Virrey JJ, et al. Critical role of the stress chaperone GRP78/BiP in tumor proliferation, survival, and tumor angiogenesis in transgene-induced mammary tumor development. Cancer Res. 2008;68:498–505. doi: 10.1158/0008-5472.CAN-07-2950. [DOI] [PubMed] [Google Scholar]
- 82.Jamora C, Dennert G, Lee AS. Inhibition of tumor progression by suppression of stress protein GRP78/BiP induction in fibrosarcoma B/C10ME. Proc Natl Acad Sci USA. 1996;93:7690–7694. doi: 10.1073/pnas.93.15.7690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fels DR, Koumenis C. The perk/eif2alpha/atf4 module of the upr in hypoxia resistance and tumor growth. Cancer Biol Ther. 2006;5:723–728. doi: 10.4161/cbt.5.7.2967. [DOI] [PubMed] [Google Scholar]
- 84.Bobrovnikova-Marjon E, Grigoriadou C, Pytel D, Zhang F, Ye J, Koumenis C, et al. Perk promotes cancer cell proliferation and tumor growth by limiting oxidative DNA damage. Oncogene. 2010;29:3881–3895. doi: 10.1038/onc.2010.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Healy SJ, Gorman AM, Mousavi-Shafaei P, Gupta S, Samali A. Targeting the endoplasmic reticulum-stress response as an anticancer strategy. Eur J Pharmacol. 2009;625:234–246. doi: 10.1016/j.ejphar.2009.06.064. [DOI] [PubMed] [Google Scholar]
- 86.Pluquet O, Hainaut P. Genotoxic and non-genotoxic pathways of p53 induction. Cancer Lett. 2001;174:1–15. doi: 10.1016/S0304-3835(01)00698-X. [DOI] [PubMed] [Google Scholar]
- 87.Shen Y, White E. p53-dependent apoptosis pathways. Adv Cancer Res. 2001;82:55–84. doi: 10.1016/S0065-230X(01)82002-9. [DOI] [PubMed] [Google Scholar]
- 88.Madan E, Gogna R, Bhatt M, Pati U, Kuppusamy P, Mahdi AA. Regulation of glucose metabolism by p53: emerging new roles for the tumor suppressor. Oncotarget. 2011;2:948–957. doi: 10.18632/oncotarget.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Madan E, Gogna R, Kuppusamy P, Bhatt M, Mahdi AA, Pati U. SCO2 induces p53-mediated apoptosis by Thr845 phosphorylation of ASK-1 and dissociation of the ASK-1-Trxcomplex. Mol Cell Biol. 2013;33:1285–1302. doi: 10.1128/MCB.06798-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Madan E, Gogna R, Kuppusamy P, Bhatt M, Pati U, Mahdi AA. TIGAR induces p53-mediated cell-cycle arrest by regulation of RB-E2F1 complex. Br J Cancer. 2012;107:516–526. doi: 10.1038/bjc.2012.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Qu L, Huang S, Baltzis D, Rivas-Estilla AM, Pluquet O, Hatzoglou M, et al. Endoplasmic reticulum stress induces p53 cytoplasmic localization and prevents p53-dependent apoptosis by a pathway involving glycogen synthase kinase-3β. Genes Dev. 2004;18:261–277. doi: 10.1101/gad.1165804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Elena S, Elena S, Halazonetis TD. p53 and stress in the ER. Genes Dev. 2004;18:241–244. doi: 10.1101/gad.1181704. [DOI] [PubMed] [Google Scholar]
- 93.Tabira T, Chui DH, Kuroda S. Significance of the intracellular Ab42 accumulation in Alzheimer’s disease. Front Biosci. 2002;7:44–49. doi: 10.2741/tabira. [DOI] [PubMed] [Google Scholar]
- 94.Baba M, Nakajo S, Tu PH, Tomita T, Nakaya K, Lee VM, et al. Aggregation of a-synuclein in lewy bodies of sporadic Parkinson’s disease and dementia with lewy bodies. Am J Pathol. 1998;152:879–884. [PMC free article] [PubMed] [Google Scholar]
- 95.Anand R, Gill KD, Mahdi AA. Therapeutics of Alzheimer’s disease: past, present and future. Neuropharmacology. 2014;76:27–50. doi: 10.1016/j.neuropharm.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 96.Cook DG, Sung JC, Golde TE, Felsenstein KM, Wojczyk BS, Tanzi RE, et al. Expression and analysis of presenilin 1 in a human neuronal system: localization in cell bodies and dendrites. Proc Natl Acad Sci USA. 1996;93:9223–9228. doi: 10.1073/pnas.93.17.9223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Katayama T, Imaizumi K, Honda A, Yoneda T, Kudo T, Takeda M, et al. Disturbed activation of endoplasmic reticulum stress transducers by familial Alzheimer’s disease-linked presenilin-1 mutations. J Biol Chem. 2001;276:43446–43454. doi: 10.1074/jbc.M104096200. [DOI] [PubMed] [Google Scholar]
- 98.Hoozemans JJM, van Haastert ES, Nijholt DAT, Rozemuller AJM, Eikelenboom P, Scheper W. The unfolded protein response is activated in pretangle neurons in Alzheimer’s disease hippocampus. Am J Pathol. 2009;174:1241–1251. doi: 10.2353/ajpath.2009.080814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Unterberger U, Hoftberger R, Gelpi E, Flicker H, Budka H, Voigtlander T. Endoplasmic reticulum stress features are prominent in Alzheimer’s disease but not in prion diseases in vivo. J Neuropathol Exp Neurol. 2006;65:348–357. doi: 10.1097/01.jnen.0000218445.30535.6f. [DOI] [PubMed] [Google Scholar]
- 100.Gupta SDA, Deepti A, Deegan S, Lisbona F, Hetz F, Samali A. HSP72 protects cells from ER stress induced apoptosis via enhancement of IRE1a-XBP1 signaling through a physical interaction. PLoS Biol. 2010;8:e1000410. doi: 10.1371/journal.pbio.1000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Acosta-Alvear D, Zhou Y, Blais A, Tsikitis M, Lents NH, Arias C, et al. XBP1 controls diverse cell type- and condition-specific transcriptional regulatory networks. Mol Cell. 2007;27:53–66. doi: 10.1016/j.molcel.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 102.Coleman PD, Yao PJ. Synaptic slaughter in Alzheimer’s disease. Neurobiol Aging. 2003;24:1023–1027. doi: 10.1016/j.neurobiolaging.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 103.Marwarha G, Raza S, Prasanthi JRP, Ghribi O. Gadd153 and NF-kB crosstalk regulates 27-hydroxycholesterol-induced increase in BACE1 and b-amyloid production in human neuroblastoma SH-SY5Y cells. PLoS One. 2013;8:e70773. doi: 10.1371/journal.pone.0070773. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 104.Paula-Lima AC, Adasme T, SanMartin C, Sebollela A, Hetz C, Carrasco MA, et al. Amyloid β-peptide oligomers stimulate RyR-mediated Ca2+ release inducing mitochondrial fragmentation in hippocampal neurons and prevent RyR-mediated dendritic spine remodeling produced by BDNF. Antioxid Redox Signal. 2011;14:1209–1223. doi: 10.1089/ars.2010.3287. [DOI] [PubMed] [Google Scholar]
- 105.Querfurth HW, Selkoe DJ. Calcium ionophore increases amyloid-beta peptide production by cultured cells. Biochemistry. 1994;33:4550–4561. doi: 10.1021/bi00181a016. [DOI] [PubMed] [Google Scholar]
- 106.Green KN, LaFerla FM. Linking calcium to A beta and Alzheimer’s disease. Neuron. 2008;59:190–194. doi: 10.1016/j.neuron.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 107.Ferreiro E, Pereira CMF. Endoplasmic reticulumstress: a new play ER in tauopathies. J Pathol. 2012;226:687–692. doi: 10.1002/path.3977. [DOI] [PubMed] [Google Scholar]
- 108.Hoozemans JJ, Scheper W. Endoplasmic reticulum: the unfolded protein response is tangled in neurodegeneration. Int J Biochem Cell Biol. 2012;44:1295–1298. doi: 10.1016/j.biocel.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 109.Ballatore C, Lee VM, Trojanowski JQ. Tau-mediated neurodegeneration in Alzheimer’s disease and related disorders. Nat Rev Neurosci. 2007;8:663–672. doi: 10.1038/nrn2194. [DOI] [PubMed] [Google Scholar]
- 110.Cláudia MF. Pereira Crosstalk between endoplasmic reticulum stress and protein misfolding in neurodegenerative diseases. ISRN Cell Biol. 2013. Article ID 256404.
- 111.Healy DG, Abou-Sleiman PM, Wood NW. PINK, PANK, or PARK? A clinicians’ guide to familial parkinsonism. Lancet Neurol. 2004;3:652–662. doi: 10.1016/S1474-4422(04)00905-6. [DOI] [PubMed] [Google Scholar]
- 112.Lesage S, Brice A. Parkinson’s disease: from monogenic forms to genetic susceptibility factors. Hum Mol Genet. 2009;18:48–59. doi: 10.1093/hmg/ddp012. [DOI] [PubMed] [Google Scholar]
- 113.Hoozemans JJ, van Haastert ES, Eikelenboom P, de Vos RA, Rozemuller JM, Scheper W. Activation of the unfolded protein response in Parkinson’s disease. Biochem Biophys Res Commun. 2007;354:707–711. doi: 10.1016/j.bbrc.2007.01.043. [DOI] [PubMed] [Google Scholar]
- 114.Makioka K, Yamazaki T, Fujita Y, Takatama M, Nakazato Y, Okamoto K. Involvement of endoplasmic reticulum stress defined by activated unfolded protein response in multiple system atrophy. J Neurol Sci. 2010;297:60–65. doi: 10.1016/j.jns.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 115.Silva R, Ries V, Oo T, Yarygina O, Jackson-Lewis V, Ryu E, et al. Chop/gadd153 is a mediator of apoptotic death in substantia nigra dopamine neurons in an in vivo neurotoxin model of parkinsonism. J Neurochem. 2005;95:974–986. doi: 10.1111/j.1471-4159.2005.03428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sado M, Yamasaki Y, Iwanaga T, Onaka Y, Ibuki T, Nishihara S, et al. Protective effect against Parkinson’s disease-related insults through the activation of xbp1. Brain Res. 2009;1257:16–24. doi: 10.1016/j.brainres.2008.11.104. [DOI] [PubMed] [Google Scholar]
- 117.Egawa N, Yamamoto K, Inoue H, Hikawa R, Nishi K, Mori K, et al. The endoplasmic reticulum stress sensor, atf6α protects against neurotoxin-induced dopaminergic neuronal death. J Biol Chem. 2010;286:7947–7957. doi: 10.1074/jbc.M110.156430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Brundin P, Li JY, Holton JL, Lindvall O, Revesz T. Research in motion: the enigma of Parkinson’s disease pathology spread. Nat Rev Neurosci. 2008;9:741–745. doi: 10.1038/nrn2477. [DOI] [PubMed] [Google Scholar]
- 119.Smith WW, Jiang H, Pei Z, Pei Z, Pei Z, et al. Endoplasmic reticulum stress and mitochondrial cell death pathways mediate A53T mutant alpha-synuclein-induced toxicity. Hum Mol Genet. 2005;14:3801–3811. doi: 10.1093/hmg/ddi396. [DOI] [PubMed] [Google Scholar]
- 120.Tong Y, Yamaguchi H, Giaime E, Boyle S, Kopan R, Kelleher RJ, et al. Loss of leucine-rich repeat kinase 2 causes impairment of protein degradation pathways, accumulation of a-synuclein, and apoptotic cell death in aged mice. Proc Natl Acad Sci USA. 2010;107:9879–9884. doi: 10.1073/pnas.1004676107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vitte J, Traver S, Maués De Paula AM, Lesage S, Rovelli G, Corti O, et al. Leucine-rich repeat kinase 2 is associated with the endoplasmic reticulum in dopaminergic neurons and accumulates in the core of Lewy bodies in Parkinson disease. J Neuropathol Exp Neurol. 2010;69:959–972. doi: 10.1097/NEN.0b013e3181efc01c. [DOI] [PubMed] [Google Scholar]
- 122.Yuan Y, Cao P, Smith MA, Kramp K, Huang Y, Hisamoto N, et al. Dysregulated LRRK2 signaling in response to endoplasmic reticulum stress leads to dopaminergic neuron degeneration in C. elegans. PLoS One. 2011;6(8):e22354. doi: 10.1371/journal.pone.0022354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Murakami T, Shoji M, Imai Y, Inoue H, Kawarabayashi T, Matsubara E, et al. Pael-R is accumulated in Lewy bodies of Parkinson’s disease. Ann Neurol. 2004;2004(55):439–442. doi: 10.1002/ana.20064. [DOI] [PubMed] [Google Scholar]
- 124.Imai Y, Soda M, Inoue H, Hattori N, Mizuno Y, Takahashi R. An unfolded putative transmembrane polypeptide, which can lead to endoplasmic reticulum stress, is a substrate of Parkin. Cell. 2001;105:891–902. doi: 10.1016/S0092-8674(01)00407-X. [DOI] [PubMed] [Google Scholar]
- 125.Imai Y, Soda M, Takahashi R. Parkin suppresses unfolded protein stress-induced cell death through its E3 ubiquitinprotein ligase activity. J Biol Chem. 2000;275:35661–35664. doi: 10.1074/jbc.C000447200. [DOI] [PubMed] [Google Scholar]
- 126.Kitada T, Asakawa S, Hattori N, Matsumine H, Yamamura Y, Minoshima S, et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature. 1998;392:605–608. doi: 10.1038/33416. [DOI] [PubMed] [Google Scholar]
- 127.Mizuno Y, Hattori N, Matsumine H. Neurochemical and neurogenetic correlates of Parkinson’s disease. J Neurochem. 1998;1998(71):893–902. doi: 10.1046/j.1471-4159.1998.71030893.x. [DOI] [PubMed] [Google Scholar]
- 128.Omura T, Kaneko M, Okuma Y, Matsubara K, Nomura Y. Endoplasmic reticulum stress and Parkinson’s disease: the role of HRD1 in averting apoptosis in neurodegenerative disease. Oxid Med Cell Longev. 2013. Article ID 239854. [DOI] [PMC free article] [PubMed]
- 129.Greenman CP, Stephens R, Smith GL, Dalgliesh C, Hunter G, Bignell H, et al. Patterns of somatic mutation in human cancer genomes. Nature. 2007;446:153–158. doi: 10.1038/nature05610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Holtz WA, O’Malley KL. Parkinsonian mimetics induce aspects of unfolded protein response in death of dopaminergic neurons. J Biol Chem. 2003;278:19367–19377. doi: 10.1074/jbc.M211821200. [DOI] [PubMed] [Google Scholar]
- 131.Atkin JD, Farg MA, Walker AK, Walker AK, Walker AK, Walker AK. Endoplasmic reticulum stress and induction of the unfolded protein response in human sporadic amyotrophic lateral sclerosis. Neurobiol Dis. 2008;30:400–407. doi: 10.1016/j.nbd.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 132.Nishitoh H, Kadowaki H, Nagai A, Maruyama T, Yokota T, Fukutomi H, et al. ALS-linked mutant SOD1 induces ER stress- and ASK1-dependent motor neuron death by targeting Derlin-1. Genes Dev. 2008;22:1451–1464. doi: 10.1101/gad.1640108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang K, Shen X, Wu J, Sakaki K, Saunders T, Rutkowski DT, et al. Endoplasmic reticulum stress activates cleavage of CREBH to induce a systemic inflammatory response. Cell. 2006;124:587–99. [DOI] [PubMed]
- 134.Vecchi C, Montosi G, Zhang K, Lamberti I, Duncan SA, Kaufman RJ, et al. ER stress controls iron metabolism through induction of hepcidin. Science. 2009;325:877–80. [DOI] [PMC free article] [PubMed]
- 135.Lee JH, Giannikopoulos P, Duncan SA, Wang J, Johansen CT, Brown JD, et al. The transcription factor cyclic AMP-responsive element-binding protein H regulates triglyceride metabolism. Nat Med. 2011;17:812–815. doi: 10.1038/nm.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chu WS, Das SK, Wang H, Chan JC, Deloukas P, Froguel P, et al. Activating transcription factor 6 (ATF6) sequence polymorphisms in type 2 diabetes and pre-diabetic traits. Diabetes. 2007;56:856–62. [DOI] [PMC free article] [PubMed]
- 137.Wu J, Rutkowski DT, Dubois M, Swathirajan J, Saunders T, Wang J, et al. ATF6alpha optimizes long-term endoplasmic reticulum function to protect cells from chronic stress. Dev Cell. 2007;13:351–64. [DOI] [PubMed]
- 138.Meex SJ, Weissglas-Volkov D, van der Kallen CJ, Thuerauf DJ, van Greevenbroek MM, Schalkwijk CG, et al. The ATF6-Met[67]Val substitution is associated with increased plasma cholesterol levels. Arterioscler Thromb Vasc Biol. 2009;29:1322–7. [DOI] [PMC free article] [PubMed]
- 139.Gkogkas C, Middleton S, Kremer AM, Wardrope C, Hannah M, Gillingwater TH, et al. VAPB interacts with and modulates the activity of ATF6. Hum Mol Genet. 2008;17:1517–26. [DOI] [PubMed]
- 140.Harding HP, Ron D. Endoplasmic reticulum stress and the development of diabetes: a review. Diabetes. 2002;51:S455–61. [DOI] [PubMed]
- 141.Delépine M, Nicolino M, Barrett T, Golamaully M, Lathrop GM, Julier C. EIF2AK3, encoding translation initiation factor 2-alpha kinase 3, is mutated in patients with Wolcott–Rallison syndrome. Nat Genet. 2000;25:406–409. doi: 10.1038/78085. [DOI] [PubMed] [Google Scholar]
- 142.Höglinger GU, Melhem NM, Dickson DW, Sleiman PM, Wang LS, Klei L, et al. PSP Genetics Study Group. Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. Nat Genet. 2011;43:699–705. [DOI] [PMC free article] [PubMed]
- 143.Bouman L, Schlierf A, Lutz AK, Shan J, Deinlein A, Kast J, et al. Parkin is transcriptionally regulated by ATF4: evidence for an interconnection between mitochondrial stress and ER stress. Cell Death Differ. 2011;18:769–782. doi: 10.1038/cdd.2010.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kakiuchi C, Ishiwata M, Nanko S, Kunugi H, Minabe Y, Nakamura K, et al. Functional polymorphisms of HSPA5: possible association with bipolar disorder. Biochem Biophys Res Commun. 2005;336:1136–1143. doi: 10.1016/j.bbrc.2005.08.248. [DOI] [PubMed] [Google Scholar]
- 145.Luo S, Mao C, Lee B, Lee AS. GRP78/BiP is required for cell proliferation and protecting the inner cell mass from apoptosis during early mouse embryonic development. Mol Cell Biol. 2006;26:5688–5697. doi: 10.1128/MCB.00779-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ye R, Jung DY, Jun JY, Li J, Luo S, Ko HJ, et al. Grp78 heterozygosity promotes adaptive unfolded protein response and attenuates diet-induced obesity and insulin resistance. Diabetes. 2010;59:6–16. doi: 10.2337/db09-0755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kudo T, Katayama T, Imaizumi K, Yasuda Y, Yatera M, Okochi M, et al. The unfolded protein response is involved in the pathology of Alzheimer’s disease. Ann N Y Acad Sci. 2002;977:349–355. doi: 10.1111/j.1749-6632.2002.tb04837.x. [DOI] [PubMed] [Google Scholar]
- 148.Kim SJ, Zhang Z, Lee YC, Mukherjee AB. Palmitoyl-protein thioesterase-1 deficiency leads to the activation of caspase-9 and contributes to rapid neurodegeneration in INCL. Hum Mol Genet. 2006;15:1580–1586. doi: 10.1093/hmg/ddl078. [DOI] [PubMed] [Google Scholar]
- 149.Oyadomari S, Koizumi A, Takeda K, Gotoh T, Akira S, Araki E. Targeted disruption of the Chop gene delays endoplasmic reticulum stress-mediated diabetes. J Clin Investig. 2002;109:525–532. doi: 10.1172/JCI0214550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Marciniak SJ, Yun CY, Oyadomari S, Novoa I, Zhang Y, Jungreis R, et al. CHOP induces death by promoting protein synthesis and oxidation in the stressed endoplasmic reticulum. Genes Dev. 2004;18:3066–3077. doi: 10.1101/gad.1250704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gragnoli C. CHOP T/C and C/T haplotypes contribute to early-onset type 2 diabetes in Italians. J Cell Physiol. 2008;217:291–295. doi: 10.1002/jcp.21553. [DOI] [PubMed] [Google Scholar]
- 152.Song B, Scheuner D, Ron D, Pennathur S, Kaufman RJ. Chop deletion reduces oxidative stress, improves beta cell function, and promotes cell survival in multiple mouse models of diabetes. J Clin Investig. 2008;118:3378–3389. doi: 10.1172/JCI34587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Karasik A, O’Hara C, Srikanta S, Swift M, Soeldner JS, Kahn CR, et al. Genetically programmed selective islet betacell loss in diabetic subjects with Wolfram’s syndrome. Diabetes Care. 1989;12:135–138. doi: 10.2337/diacare.12.2.135. [DOI] [PubMed] [Google Scholar]
- 154.Inoue, Tanizawa HY, Wasson J, Behn P, Kalidas K, Bernal-Mizrachi E, et al. A gene encoding a transmembrane protein is mutated in patients with diabetes mellitus and optic atrophy (Wolfram syndrome) Nat Genet. 1998;20:143–148. doi: 10.1038/2441. [DOI] [PubMed] [Google Scholar]
- 155.Ishihara H, Takeda S, Tamura A, Takahashi R, Yamaguchi S, Takei D, et al. Disruption of the WFS1 gene in mice causes progressive beta-cell loss and impaired stimulus secretion coupling in insulin secretion. Hum Mol Genet. 2004;13:1159–1170. doi: 10.1093/hmg/ddh125. [DOI] [PubMed] [Google Scholar]
- 156.Mita M, Miyake K, Zenibayashi M, Hirota Y, Teranishi T, Kouyama K, et al. Association study of the effect of WFS1 polymorphisms on risk of type 2 diabetes in Japanese population. Kobe J Med Sci. 2008;54:E192–E199. [PubMed] [Google Scholar]
- 157.Kakiuchi C, Iwamoto K, Ishiwata M, Bundo M, Kasahara T, Kusumi I, et al. Impaired feedback regulation of XBP1 as a genetic risk factor for bipolar disorder. Nat Genet. 2003;35:171–175. doi: 10.1038/ng1235. [DOI] [PubMed] [Google Scholar]
- 158.Cichon S, Buervenich S, Kirov G, Akula N, Dimitrova A, Green E, et al. Lack of support for a genetic association of the XBP1 promoter polymorphism with bipolar disorder in probands of European origin. Nat Genet. 2004;36:783–784. doi: 10.1038/ng0804-783. [DOI] [PubMed] [Google Scholar]