Abstract
Background:
Dementia is the most devastating cognitive disorder of the elderly and needs extra attention to care. Therefore, this study was conducted to identify the caregiver burden of dementia key caregivers and their Quality of Life (QOL).
Materials and Methods:
Sample consisted of purposively selected 24 dementia key caregivers fulfilling the inclusion criteria from the in-patient of the Department of Geriatric Mental Health, King George's Medical University, Lucknow, Uttar Pradesh, India. Zarit Burden Interview and World Health Organization QOL-BREF were administered. Mean, standard deviation, t-test, Chi-square with Yate's correction were used to analyze the data.
Results:
All key caregivers felt mild to moderate level of burden. Gender-wise significant difference was found on burden area of expectation (P < 0.05). Mean scores on physical, psychological, social relationship, and environmental QOL were found to be on lower side. A negative correlation was found between burden and QOL.
Conclusion:
Professional help and supportive psychotherapy can be provided to the key caregivers of dementia patients to reduce their burden, strengthen the coping skill and thus improve their QOL.
Keywords: Burden and Quality of Life, dementia, key caregiver
INTRODUCTION
Dementia is the most devastating mental health problem of elderly. Around 25 million people worldwide have dementia, and the number of people with dementia is predicted to exceed 80 million by 2040.[1] In Indian context prevalence of dementia varied from 1.4% to 4.4%.[2,3,4,5,6] A rough estimate at average 3% prevalence revealed that at present about 3.7 million elderly are suffering from dementia (2.1 million women and 1.5 million men), in India.[7] Hence, the burden on key caregivers of dementia and health care professionals is also increasing.
Dementia affects patient's personal, social, and occupational life along with significant impairment in their activities of daily living (ADL). Patient of dementia becomes more and more dependent on their caregivers for their ADL as the disease progresses. In the course of this constant caregiving, key caregiver makes lots of sacrifices. Many times key caregiver experiences a lot of strain and burden resulting from this rigorous activity of caregiving, which has a negative impact on their physical, psychological, and social Quality of Life (QOL).[8,9] Thus, they become more prone to develop a psychiatric disorder. About one-third of family caregivers of Alzheimer dementia reported depressive symptoms.[8,9]
Caregiver distress and burden indicate prolonged consequences of poor physical and emotional health.[10,11] Studies on caregivers in India[12,13,14] suggest that caregiving is associated with more psychological complaints and a poor physical and psychological QOL. In this study, we have focused to explore the caregiver burden and QOL of dementia key caregivers. It was hypothesized that there will be no burden on dementia caregivers.
MATERIALS AND METHODS
Sample
The sample consisted of 24 dementia key caregivers from the inpatient of the Department of Geriatric Mental Health, King George's Medical University, Lucknow, Uttar Pradesh, India. The sample was purposively selected fulfilling the inclusion criteria. The study was conducted between the 14-4-2010 and 14-5-2010.
The key caregivers of patients diagnosed with Alzheimer's dementia according to International Classification of Diseases, Tenth Revision criteria, aged more than 18 years, caring and living with the patient for more than 1 year, having no chronic illness since last 1 year and providing written informed consent were included in the study.
Key caregiver
Key caregiver for the study was operationally defined as: Person responsible for providing care to the index case on day to day basis most of the time. The key caregiver could be a spouse, children or any other family member who were living with the index case in the same house and shares same kitchen and is taking responsibility of ADL.
Tools
Zarit Burden Interview
Zarit Burden Interview (ZBI)[15] is a 22-item self-administered rating questionnaire measuring subjective burden, which has demonstrated high consistency and validity, and a higher score indicates greater burden. The items are rated on a four-point rating scale. It has good internal consistency reliability, with a Cronbach's alpha co-efficiency of 0.92. Following is the scoring pattern of ZBI: Score - 0-21 no burden; 22-40 mild-moderate; 41-60 moderate-severe; 61-80 severe-profound burden.
World Health Organization Quality of Life-BREF Hindi version
World Health Organization QOL-BREF (WHOQOL-BREF),[16] is an abbreviated 26-item version of the WHOQOL-100. Items are distributed into four domains (physical; psychological; social and environmental QOL). It is a five-point rating scale questionnaire. It has been shown to have good discriminant, content, and test-retest validity. Test-retest reliability was found to be good for each of the four domains (Cronbach alpha 0.66-0.84).
Data were analyzed using percentages, mean, standard deviation, t-test, and Chi-square with Yate's correction wherever applicable.
RESULTS
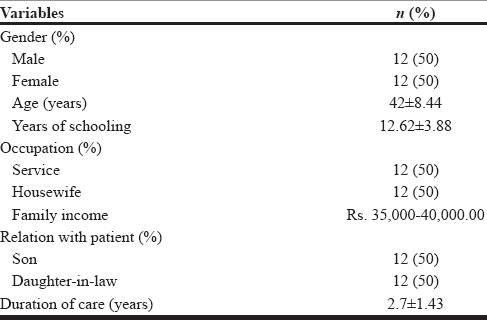
Table 1 shows mean age (42 ± 8.44 years), mean schooling years, occupation, family income relation with patient, and mean duration of caregiving (2.7 ± 1.43 years) of key caregivers of dementia patients.
Table 1.
Sociodemographic profile of key caregivers of dementia patients
There was insignificant difference between male and female mean scores on ZBI. Though, female caregiver (34.75 ± 11.21) felt more burden in comparison to male (28.41 ± 13.33). The mean score on ZBI was found to be 31.53 ± 12.27 of dementia key caregivers that fall in the category of mild to moderate level of burden.
Table 2 reveals that there was a significant difference among male and female in the burden area of “expectation” (P < 0.05) only. Females feel significantly more burdened by “expectations” than males in caregiving of dementia patients.
Table 2.
Gender-wise comparison of burden on Zarit Burden Interview in dementia key caregivers
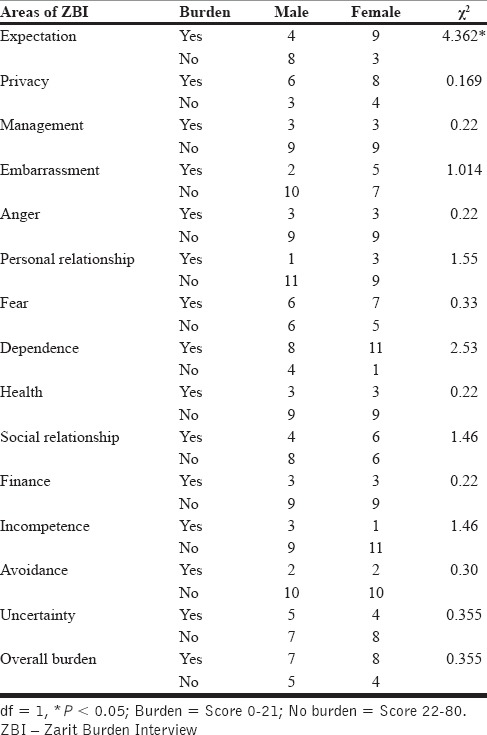
Table 3 reveals that there was insignificant difference between male and female on the domains of QOL. Though, the mean scores on its domain were found to be on the lower side is suggestive of poor QOL of dementia key caregivers.
Table 3.
Domain-wise Quality of Life of key caregivers of dementia patients on World Health Organization Quality of Life-BREF
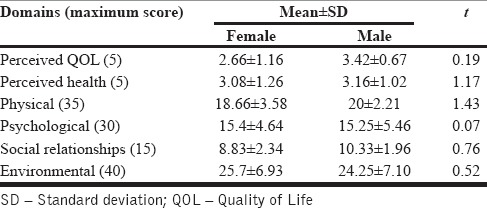
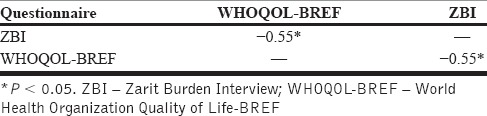
Table 4 shows that there was a negative correlation between the scores on ZBI and WHOQOL-BREF. It means as the burden increases QOL become poorer.
Table 4.
Correlation between Zarit Burden Interview and World Health Organization Quality of Life-BREF scores
DISCUSSION
The study was conducted to assess caregiver burden and QOL of dementia key caregivers. The key caregivers experienced burden in areas such as expectation, privacy, management, embarrassment, anger, personal and social relationships, fear, dependence, finance, incompetence, uncertainty, and avoidance. This burden, affect their physical, psychological, social relationship, and environmental QOL. The findings are in consonance with the Indian[11,12,13,14] and Western country studies[7,8,9,10] where physical and psychological health was found to be affected of caregivers.
Mild to moderate range of burden, suggests that caring for dementia impose great stress on the key caregiver, which, increase with progression of cognitive and behavioral symptoms, and the duration of caring for the loved one, and it can lead to depression and other illnesses. This result is similar as reported by Dementia India Report[6] and study of Burns.[17]
Males reported more burden in social relationship, incompetence and dependence. This may be due to lack of time to maintain a social relationship after work and caring dementia patient. Females reported more burden in areas of expectation, management, dependence, and in overall burden. This could be due to the pressure of their responsibility toward other members of the family, while caring for the patient.[18] Females are emotional and empathetic in comparison to males, and thus are more prone to caregiver's stress leading to depression.[14]
Significantly more females were found to burdened due to “expectation” of caregiving. This may be because India, a male dominated society where females are entrusted to do home related affairs and males are responsible to do work outside of the home. It is still prevailing in rural areas but, this scenario is gradually changing now in urban areas where both are working. Thus, in near future trained professionals will be required for caregiving.
On WHOQOL-BREF domains females having mean score slightly lower compared to males on “perceived QOL” and “physical” domain. It suggests that males had better QOL in comparison to females in these domains. Probably because males are the bread earners in their family and help received both financially and otherwise relieve the pressures on one's life and health as well as reducing the possibility of burden, overload and burnout due to caregiving. This finding is similar as reported by Jathanna et al. and Burns.[14,17] On “psychological” domain of QOL females scored better than males. The study report that males are at extraordinarily high risk for depression, perhaps especially if they are husbands caring for impaired wives.[19] “Social relationships” QOL was found better of males compared to females. Females are more dissatisfied in their personal, social, sexual life, and they do not get enough support from their friends and other family members to share their responsibilities. The “environmental” QOL was found to be better of male key caregivers compared to females.
A negative correlation with burden and QOL indicates that QOL of dementia key caregivers hampered due to burden in caregiving. Similar findings recently reported that burden and depressive symptoms were related to QOL of caregivers of dementia patients.[20]
CONCLUSION
Professional help and supportive psychotherapy can be provided to the key caregivers of dementia patients to reduce their burden, strengthen the coping skill and thus improve their QOL.
Limitations of the study
Small sample size hence, results cannot be generalized. Other group of caregivers, different social and family characteristics could not be studied. The severity of dementia and ADL was not assessed at the time of the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgments
We are grateful to the Dean of King George's Medical University, Lucknow, Uttar Pradesh, India for permitting me to collect data from the Department of Geriatric Mental Health.
REFERENCES
- 1.Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: A Delphi consensus study. Lancet. 2005;366:2112–7. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaji S, Bose S, Verghese A. Prevalence of dementia in an urban population in Kerala, India. Br J Psychiatry. 2005;186:136–40. doi: 10.1192/bjp.186.2.136. [DOI] [PubMed] [Google Scholar]
- 3.Tiwari SC, Srivastava G, Tripathi RK, Pandey NM, Agarwal GG, Pandey S, et al. Prevalence of psychiatric morbidity amongst the community dwelling rural older adults in Northern India. Indian J Med Res. 2013;138:504–14. [PMC free article] [PubMed] [Google Scholar]
- 4.Tiwari S, Tripathi R. Neuro-psychiatric morbidity amongst urban and rural elderlies in Northern India: Report from a community based epidemiological study. Int Psychogeriatr. 2009;21:S136. [Google Scholar]
- 5.Tiwari SC, Tripathi RK, Kumar A, Kar AM, Singh R, Kohli VK, et al. Prevalence of psychiatric morbidity among urban elderlies: Lucknow elderly study. Indian J Psychiatry. 2014;56:154–60. doi: 10.4103/0019-5545.130496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. [Last accessed on 2011 Aug 05]. Available from: http://www.dementia-care-notes.in/dementia/dementia-and-caregiving-in-india .
- 7.Anthony-Bergstone CR, Zarit SH, Gatz M. Symptoms of psychological distress among caregivers of dementia patients. Psychol Aging. 1988;3:245–8. doi: 10.1037//0882-7974.3.3.245. [DOI] [PubMed] [Google Scholar]
- 8.Cohen D, Eisdorfer C. Depression in family members caring for a relative with Alzheimer's disease. J Am Geriatr Soc. 1988;36:885–9. doi: 10.1111/j.1532-5415.1988.tb05780.x. [DOI] [PubMed] [Google Scholar]
- 9.Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. Gerontologist. 1995;35:771–91. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- 10.Kalikaya G, Yukse G, Varlibas F, Tireli H. Caregiver burden in dementia: A study in the Turkish population. [Last accessed on 2015 Dec 31];Internet J Neurol. 2004 4:2. Available from: https://www.ispub.com/IJN/4/2/12633 . [Google Scholar]
- 11.Srivastava G, Tripathi RK, Kumar A, Tiwari SC. Care needs of Indian urban elderlies and strain in their caregivers. Int Psychogeriatr. 2009;21:S198. [Google Scholar]
- 12.Tiwari S, Kohli A, Gupta B, Tiwari SC. Quality of Life in Dementia Care Givers. Proceedings in 6th Annual Conference of Indian Association for Geriatric Mental Health; 3rd-5th September, 2010; Hotel Mirage, Mumbai. [Google Scholar]
- 13.Emmatty LM, Bhatti RS, Mukalel MT. The experience of burden in India: A study of dementia caregivers. Dementia. 2006;5:223–32. [Google Scholar]
- 14.Jathanna RPN, Latha KS, Bhandary PV. Burden and Coping in Informal Caregivers of Persons with Dementia: A Cross Sectional Study. Online J Health Allied Sci. 2010;9:7. http://www.ojhas.org/issue36/2010-4-7.htm. Open Access Archives: http://cogprints.org/view/subjects/OJHAS.html. and http://openmed.nic.in/view/subjects/ojhas.html . [Google Scholar]
- 15.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649–55. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 16.Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 17.Burns A. The burden of Alzheimer's disease. Int J Neuropsychopharmacol. 2000;3:31–8. doi: 10.1017/S1461145700001905. [DOI] [PubMed] [Google Scholar]
- 18.Das PC, Kumar P, Amara A, Dey AB. Dementia care in India: Issues & prospects. Int J Med Pharm Sci. 2014;4:29–36. [Google Scholar]
- 19.Tower RB, Kasl SV, Moritz DJ. The influence of spouse cognitive impairment on respondents’ depressive symptoms: The moderating role of marital closeness. J Gerontol B Psychol Sci Soc Sci. 1997;52:S270–8. doi: 10.1093/geronb/52b.5.s270. [DOI] [PubMed] [Google Scholar]
- 20.Santos RL, Sousa MF, Simões-Neto JP, Nogueira ML, Belfort TT, Torres B, et al. Caregivers’ quality of life in mild and moderate dementia. Arq Neuropsiquiatr. 2014;72:931–7. doi: 10.1590/0004-282X20140155. [DOI] [PubMed] [Google Scholar]


