Abstract
Objective:
Diabetes mellitus (DM) is a common chronic disease and it has emerged as a major health-care problem. There are more chances of dentinal caries among diabetics than nondiabetics. DM is responsible for causing ascendancy in the proportion and activity of saliva that impacts the oral health. The objective of the present study is to evaluate the impact of various factors present in saliva on tooth decay amid type-II DM in Jammu.
Materials and Methods:
The subjects in our analysis comprises of 50 patients with type-II DM and 50 controls within the age group of 30–60 years. Diabetic status was assessed by estimating random blood glucose levels. Dental findings were recorded using modified World Health Organization (WHO) Oral health survey-basic method 2013. Salivary samples from all the subjects were collected and sent to the laboratory for interpretation of pH, flow rate, and salivary calcium. The analysis of salivary components decayed tooth was carried using analysis of variance (ANOVA) and Pearson's correlation test. All the parameters were subjected to statistical analysis using Statistical Package for the Social Sciences (SPSS) version 20.0.
Results:
The results have shown a significantly lower values of salivary pH, flow rate, and calcium levels in diabetics than in nondiabetics.
Conclusion:
Within the limits of the present study, the results indicated that patients with type-II DM have high rate of dental caries and are at high risk of caries development. The decline in the salivary components will reduce capability of supporting the mineral compartment of tooth structure to resist the demineralization process by cariogenic potentials thereby creating a favorable environment for caries progression.
Keywords: Dental caries, diabetes, type-II diabetes mellitus, salivary flow rate, salivary pH
INTRODUCTION
Diabetes mellitus (DM) is a common chronic disease that has emerged as a major health-care problem. There was an estimation of 40 million people with diabetes in India in 2007 and this number is predicted to rise to almost 70 million people by 2025. According to the Diabetes Atlas published by the International Diabetes Federation (IDF), every fifth person with diabetes will be an Indian by 2025.[1] DM leads to a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both.[2]
Diabetes includes two forms: Type-I diabetes, in which the pancreas β-cells lose their capacity to produce insulin and type-II diabetes, in which a defect in the β-cells or a reduction in tissue sensitivity to insulin are necessary for disease manifestation. Oral complications include dental caries, periodontal disease, and tooth mobility that is influenced by saliva.[3]
Diabetic patients are associated with intensive loss of fluid due to polyuria, reduced response to infections, impaired connective tissue metabolism, and various microvascular changes. These factors are responsible for various oral diseases in diabetic patients including xerostomia, salivary gland dysfunction, increased susceptibility to bacterial, viral and fungal infection, periapical abscesses, loss of teeth, taste impairment, lichen planus, burning mouth syndrome, and altered orthodontic tooth movements.[4]
A very high and appalling prevalence of dental caries is found in diabetic patients compared to nondiabetics.
It has been reported in the literature from previous studies that risk of dental caries is more prevalent in patients with type-II DM compared to nondiabetics.
DM is responsible for causing ascendancy in the proportion and activity of saliva that impacts the oral health.
Dental caries is caused by demineralization that is triggered by the accumulation of microbial plaque flora, decrease in the flow rate of saliva causing reduction in the cleansing, and buffer activity and diminished levels of calcium that is essential for the repair of decayed tooth.[5]
Saliva is essential for maintaining the oral equilibrium and the effects of saliva and its constituents on the oral microorganisms that influence the development of dental caries. Salivary components (immunoglobulins, salivary protein, salivary calcium, and inorganic phosphorous and alkaline phosphatase levels), its flow rate, viscosity, buffering capacity, pH, etc., plays a major role in initiation and progression of dental caries.[6]
The average value of whole saliva as per various studies conducted on unstimulated saliva is found to be 0.3 mL/min. If the values are found to be less than 0.1 mL/min, it is a case of hyposalivation.[5] The normal value of salivary pH is 5.6–7.9, whereas the normal levels of salivary calcium is found to be 4–6 mg/mL.[7] In Jammu, no studies on changes in salivary constituents in diabetic patients and dental caries were available on search of literature. Thus, there is a need for an investigation focused on the assessment of salivary factors among diabetics. Therefore, this study was intended with the objectives to identify the consanguinity between various components of saliva and its dependence on tooth decay amid patients with type-II diabetes in Jammu City.
MATERIALS AND METHODS
The present case-control study consists of 100 randomly selected patients who visited Indira Gandhi Dental College and Hospital Jammu for a period of 5 month from March to August 2015.
Among the total patients, 50 were having type-II DM and 50 were nondiabetics who were chosen depending on their [fasting blood sugar (FBS)] levels and past medical reports.
The patients were well informed in advance and their consent was taken before the start of the study.
The patients were selected on the basis of following criteria:
Presence of type-II diabetes from at least 3 years
The age of the patient should be between 30 years and 60 years
The patient should be having FBS within the limit of 126 mg/dL (7 mmol/L) and higher than that
Selected patients must be free from diabetic complications and the patients have not undergone any preventive procedure for caries including fluoride exposure.
The nondiabetic patients were selected on the basis of following criteria:
Age group of the controls should also be between 30 to 60 years
The patients should have FBS under normal range <100 mg/dL (5.6 mmol/L)
The patient should not be having any medical and family history of diabetes.
A predesigned questionnaire was used to collect information for recording of general data and demographic information of the patient, type and years since diagnosis of DM, and family history. A modified WHO Oral health survey basic method 2013 performa was used to calculate the clinical data for recording dental caries. For dental caries, dentition status index was included and community periodontal index was used to record periodontal status of the patient.
The analysis of saliva was done by collecting 3–5 mL of saliva that was collected from all the patients in sterilized culture tubes. The salivary samples were stored at –20°C until it was sent to laboratory. The analysis of flow rate of saliva has been done by acquiring saliva in the test tube and measuring it for 60 s. A digital pH meter has been used to determine pH of saliva. The calorimetric method was used to measure salivary calcium.
The armamentarium that has been used in the present study comprise of sterilized sets of odontoscope, no. 23- explorer, CPI probe, and tweezer.
The examination has been done in department of public health dentistry of Indira Gandhi Dental College, Jammu. A single examiner has examined all the cases along with the assistance from a recorder who is well versed with the questionnaire and examination pattern.
Descriptive statistics have been used for analyzing the correlation among various components of saliva and tooth decay amidst type-II diabetics and controls. Pearson's correlation test and parametric one-way analysis of variance (ANOVA) has been done to describe the impact of one variable on the other. Data were entered and analyzed using Statistical Package for Social Sciences (SPSS) version 20 (SPSS-Inc., Chicago, IL).
RESULTS
Table 1 depicts that the values of DMFT and FBS were high, and the levels of calcium, pH, and flow rate of saliva are found to be less in type-II diabetics compared to controls using Student's t-test.
Table 1.
Relationship between salivary factors and DMFT status among patients with type-II diabetes and controls
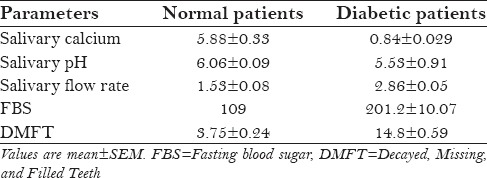
Table 2 depicts the association among various components of saliva and DMFT status using one-way ANOVA, and dental caries show a significant relationship with time span of diabetes and levels of calcium in saliva amidst type-II diabetics.
Table 2.
Association of various components of saliva and DMFT status among type-II diabetics
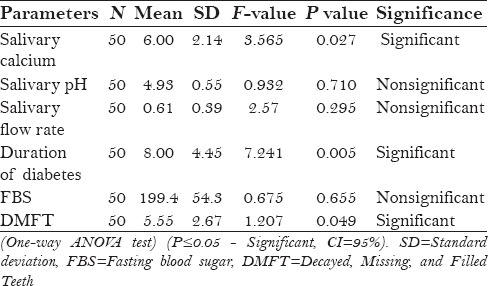
Table 3 shows the association between salivary factors and DMFT status using one-way ANOVA test among non-diabetic patients, and the result shows that dental caries has a nonsignificant relationship with salivary factors.
Table 3.
Association of various components of saliva and DMFT status among normal patients
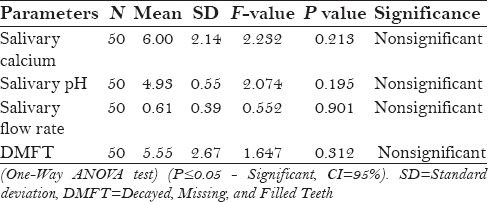
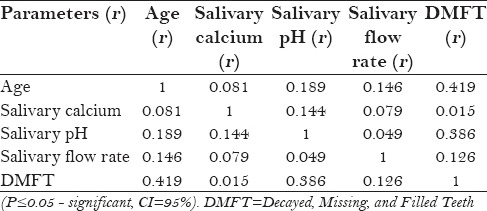
Table 4 depicts the association between components of saliva and DMFT status using Pearson's correlation test among diabetic patients and it has been seen that dental caries show a significant relationship with flow rate, pH, and calcium levels of saliva.
Table 4.
Association between dental caries and salivary factors among diabetic patients
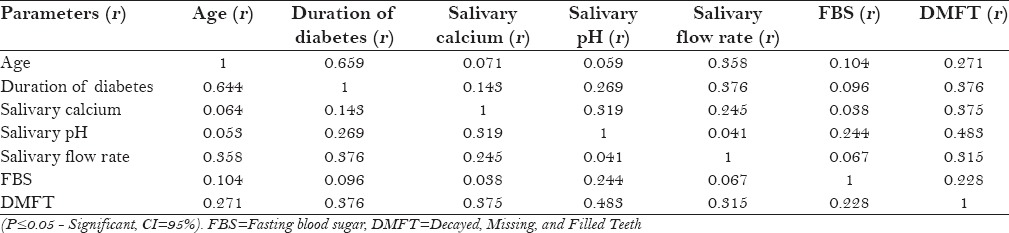
Table 5 depicts the association among various components of saliva and DMFT status in nondiabetics. A significant relationship was seen between DMFT status and the salivary pH.
Table 5.
Association amidst various components of saliva and DMFT status in nondiabetics (Pearson's correlation)
DISCUSSION
DM is a metabolic disease with numerous systemic manifestations that are also noticeable in the oral cavity as first described by Seifert in 1862. Manifestations in the oral cavity include abnormal development of dentition, increased frequency and intensity of caries, pathologies of the oral mucosa, xerostomia as well as atrophic changes in the alveolar process.[8]
Saliva is a very common and useful alternative for blood that is used for the diagnosis of various systemic diseases. One of the important benefits of performing salivary assessment is its cost-effectiveness for screening of large populations.[9]
The present study throws light on salivary factors and their impact on tooth decay among type-II diabetics and normal controls.
According to the results, it has been seen that the DMFT score of the patients with type-II diabetes was very high in comparison with healthy individuals who were taken as controls.
High prevalence of dental caries among diabetic patients have also been reported by Maria Moin et al.[10] (2015), Malicka et al.[11] (2011) in their studies, whereas irreconcilable results were shown in the study done by Qureshi et al.[8] The reasoning behind this high prevalence is that salivary glucose level among the diabetic patients is very high that favors the propagation of microorganisms and adorn their accumulation on tooth surface. These factors also lower the executing tendency of neutrophils that accelerate the microbial accumulation and thus maximize the risk of tooth decay among diabetics.
The shielding roles of salivary pH, salivary flow rate, and salivary calcium against dental caries have been into reported in the past literature. Following our analysis, significantly low levels of salivary pH (4.83 ± 0.08) has been seen among diabetic patients. Similar study conducted by Prathibha[12] (2013) quotes low value of salivary pH thus agreeing to our analysis, indicating favorable conditions for demineralization and thus accelerating cavity formation.
Calcium plays a very important role in tooth disintegration through its solubility that supplies the stable and prolonged reservoir to the decayed tooth area. The other inorganic minerals present in serum also gets exchanged with saliva that surrounds teeth and acts as a pool of calcium to conserve its competent limit.[13] The amount of calcium is low in type-II diabetes patients due to failure of blood glucose level. In the present analysis, we have also seen low level of salivary calcium among type-II diabetics than nondiabetics. Our findings are in agreement with the study conducted by Jawed et al.[14]
The diabetes has a very negative impact on sympathetic and parasympathetic nervous system such as microangiopathy; it also causes dehydration and hormonal changes that are responsible for the alteration in the salivary flow rate.[15] The results of our study also show reduction in the salivary flow rate in type-II diabetics as compared to normal controls. The results of our analysis agree with that of the studies done by Collin's et al.[13] and Avideh Maboudi[16] (2014), but they disagree with the results found in the studies conducted by Aydin et al.[17]
From the present analysis, it has been seen that there exists a dependence of dental caries on salivary calcium, salivary flow rate, and salivary pH among diabetic patients that were found to be very low. There is literature from some older studies suggesting that diabetic patients have threefold times the risk of having dental caries than nondiabetics.[18] An explanation behind these findings is that the salivary components when present in a balanced equation have capability of supporting the mineral compartment of tooth structure to resist the demineralization process by cariogenic potentials. So the decline in the salivary components will create favorable environment for caries progression. The findings of our analysis agree with the results of study conducted by Pearce et al.[18] (2002).
Within the limitation of this study, there can be alteration in the physicochemical properties of saliva, such as decreased salivary flow rate, pH, and calcium, also there are various other factors such as increased total proteins and total antioxidant capacity that plays very important role in the progression of caries. Hence, there is requirement of further investigation to evaluate the role of other parameters of saliva among diabetic subjects and dental caries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Goyal D, Kaur H, Jawanda MK, Verma S, Parhar S. Salivary pH and dental caries in diabetes mellitus. Int J Oral Maxillofac Surg. 2012;3:13–6. [Google Scholar]
- 2.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–97. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 3.Darnell JA, Saunders MJ. Oral manifestations of the diabetic patient. Tex Dent J. 1990;107:23–7. [PubMed] [Google Scholar]
- 4.Diabetes Action Now. Vol. 58. Geneva, Switzerland: Int Dent J; 2008. WHO/International diabetes federation; pp. 265–8. [Google Scholar]
- 5.Singh A, Thomas S, Dagli RJ, Kaţ R, Solanki J, Bhateja GA. To access the effects of salivary factors on dental caries among diabetic patients and non diabetic patients in Jodhpur City. J Adv Oral Res. 2014;5:10–4. [Google Scholar]
- 6.Clarkson BH. Introduction to cariology. Dent Clin North Am. 1999;43:569–78, v. [PubMed] [Google Scholar]
- 7.Baliga S, Muglikar S, Kale R. Salivary pH: A diagnostic biomarker. J Indian Soc Periodontol. 2013;17:461–5. doi: 10.4103/0972-124X.118317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qureshi A, Qureshi A, Qureshi H, Khan AA. Blood glucose level, Salivary pH and oral bacterial count in type 1 diabetic children. Infect Dis J. 2007;16:45–8. [Google Scholar]
- 9.Pfaffe T, Cooper-White J, Beyerlein P, Kostner K, Punyadeera C. Diagnostic potential of saliva: Current state and future applications. Clin Chem. 2011;57:675–87. doi: 10.1373/clinchem.2010.153767. [DOI] [PubMed] [Google Scholar]
- 10.Moin M, Malik A. Frequency of dental caries and level of risk among type II diabetics. Dentistry. 2015;5:1–5. [Google Scholar]
- 11.Malicka B, Kaczmarek U, Ziętek M. Dental caries in adult patients with type 1 and 2 diabetes mellitus. J Stoma. 2011;64:9–24. [Google Scholar]
- 12.Johnson P, Ganesh M, Subhashini AS. Evaluation of salivary profile among adult type 2 diabetes mellitus patients in South India. J Clin Diagn Res. 2013;7:1592–5. doi: 10.7860/JCDR/2013/5749.3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collin HL, Uusitupa M, Niskanen L, Koivisto AM, Markkanen H, Meurman JH. Caries in patients with non-insulin-dependent diabetes mellitus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:680–5. doi: 10.1016/s1079-2104(98)90035-x. [DOI] [PubMed] [Google Scholar]
- 14.Jawed M, Shahid SM, Qader SA, Azhar A. Dental caries in diabetes mellitus: Role of salivary flow rate and minerals. J Diabetes Complications. 2011;25:183–6. doi: 10.1016/j.jdiacomp.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Mortazavi H, Jazaeri M, Baharvand M, Abdolsamadi H. Salivary alpha-amylase alteration as a possible indicator for diabetes. J Basic Appl Sci Res. 2014;4:284–8. [Google Scholar]
- 16.Amiri AA, Maboudi A, Bahar A, Farokhfar A, Daneshvar F, Khoshgoeian HR, et al. Relationship between type 2 diabetic retinopathy and periodontal disease in Iranian adults. N Am J Med Sci. 2014;6:139–44. doi: 10.4103/1947-2714.128476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aydin S. A comparison of ghrelin, glucose, alpha-amylase and protein levels in saliva from diabetics. J Biochem Mol Biol. 2007;40:29–35. doi: 10.5483/bmbrep.2007.40.1.029. [DOI] [PubMed] [Google Scholar]
- 18.Pearce EI, Dong YM, Yue L, Gao XJ, Purdie GL, Wang JD. Plaque minerals in the prediction of caries activity. Community Dent Oral Epidemiol. 2002;30:61–9. doi: 10.1034/j.1600-0528.2002.300109.x. [DOI] [PubMed] [Google Scholar]


