Abstract
Melanomais one of the most dreaded and aggressive neoplasms, being derived from epidermal melanocytes. The majority of melanomas are seen to involve the skin, and primary mucosal melanomas account for less than 1% of all melanomas. Oral malignant melanomas (OMM) are asymptomatic at the initial presentation, but later they become painful with growth and expansion. In the late stages, the patient may present with ulceration, bleeding, tooth mobility, paresthesia, ill-fitting prosthesis, and delayed healing of the extraction sockets. Diagnosis is often delayed due to asymptomatic clinical presentation, with silent progression of the lesion. OMM are associated with poor prognosis due to their invasive and metastasizing tendencies. The condition has poor survival rates, and metastatic melanomas show even worse prognosis. The 5-year survival rate for OMM ranges 4.5–29%, with 18.5 months being the mean survival rate. The tumor is best managed by wide surgical resection; however, consideration should also be made for adjunctive therapies such as chemotherapy, immunotherapy, and radiotherapy. Recurrences may be seen even 10–15 years after the primary therapy. This paper aims to present an interesting report of aggressive OMM in a 50-year-old male patient and emphasizes the role of dental professionals in maintaining a high degree of vigilance for the pigmented lesions of the oral cavity. Pigmented lesions of uncertain origin should be routinely biopsied to rule out malignancy. Early diagnosis of this dreadful entity entails thorough history taking, physical examination, and radiographic features coupled with histopathology.
Keywords: Melanocytes, oral malignant melanoma, pigmentary lesions
INTRODUCTION
Melanoma is a malignancy of the melanocytic cells, which are derivatives of neural crest cells. The majority of melanomas originate from the skin; however, they may also originate from mucosal surfaces or other sites where neural crest cells migrate.[1] Primary oral malignant melanoma (OMM) is an uncommon malignancy, which is derived from melanocytes seen in the basal layer of the oral mucosa,[2] and contributes to 0.2–8% of all melanomas and 0.5% of all oral malignancies.[3,4] A change in the size, shape, or color of a mole is usually the first sign in melanomas.[5] Oral melanomas are associated with an extremely aggressive behavior, vertical growth pattern, high risk for metastasis, and poor survival rates.[6] Wide surgical excision with adequate negative margins with or without neck dissection forms the mainstay of treatment for malignant melanoma. Radiotherapy and chemotherapy have been attributed as adjunctive treatment modalities. Distant metastasis of the tumor may be minimized by the chemotherapy and immunotherapy.
Dacarbazine (DTIC) and interferon-alfa-2b (IFNa2b) are used for chemotherapeutical and immunotherapical treatments, with the first line of drug being DTIC, either alone or in combination with nimustine hydrochloride and vincristine, or different combinations of bacillus Calmette–Guérin (BCG) and recombinant interleukin 2 (IL-2)[7]
CASE REPORT
A 50-year-old male patient of low socioeconomic status reported to the outpatient department of Oral Medicine and Radiology, with a chief complaint of a painless, slow-growing swelling in the right maxillary teeth region for the past 5 months. The swelling was initially small and had gradually increased to the present size. There was no associated history of trauma and pain. The medical history was noncontributory. The patient gave negative history for smoking and other deleterious habits. Extraoral examination revealed diffuse swelling in the anterior region of the right maxilla. The swelling extended anteroposteriorly from the tip of the nose to 3 cm lateral to the right ala of the nose, and suprainferiorly extended up to the ala-tragus line to the lower border of the upper lip. The swelling caused mild deviation of the tip of the nose to the left side with obliteration of the right nasolabial fold. On palpation, the swelling was nontender and firm in consistency [Figure 1]. A single, firm, fixed, and tender right submental lymph node was also appreciated on palpation. On intraoral clinical examination, a lobulated, pigmented (purplish-black) growth, measuring 5 × 4 cm2 was noticed between the maxillary right central incisor and the maxillary right first molar. The growth was seen to involve the marginal, attached, and interdental gingival region on the labiobuccal aspect of the maxillary alveolus. However, there was no palatal extension of the growth. Palpatory findings were suggestive of a firm, nontender growth, which bled when probed. The maxillary right canine and the first and second premolars were clinically missing with slight displacement of the maxillary right lateral incisor [Figure 2]. The patient presented with poor oral hygiene. Thorough clinical examination ruled out the presence of any other primary site of the lesion. A provisional diagnosis of primary OMM was assigned, based on the history and clinical features. Differential diagnosis of lymphoma and squamous cell carcinoma was taken into consideration. Complete blood cell count as well as biochemical and urine analysis were insignificant and within normal limits. Distant metastasis of the lesion was ruled out on the clinical, radiographic, and ultrasonographic examination. The pantomogram revealed partially edentulous jaws and an irregular radiolucent lesion with ill-defined margins, extending from the maxillary right canine to the maxillary first molar [Figure 3]. Magnetic resonance imaging (MRI) morphology suggested a mass lesion involving the anterior wall of the right maxillary sinus and right maxillary alveolar arch up to the second molar and extending to involve the gingivobuccal sulcus and the buccinator muscle, and the zygomatic prominence laterally with extension into the adjacent anterior part of soft tissue with heterogenous postcontrast enhancement [Figure 4]. Histologic section showed a piece of tissue with pigmented connective tissue stroma under a thin, irregular, and ulcerated epithelium. Under higher magnification, connective tissue showed clusters of tumor cells in small foci and in sheets. Cells are spindle-shaped with large nuclei, prominent nucleoli (suggestive of melanocytes), and pigmented cytoplasm. Tumor cells are seen to invade and ulcerate the overlying stratified squamous epithelium. The deeper connective tissue showed dense chronic inflammatory infiltrate and endothelial-lined blood vessels with red blood cells (RBCs) [Figure 5]. The clinical, radiological, and histological features confirmed the diagnosis of malignant melanoma. The tumor cells showed strong positivity for immunohistochemical marker HMB-45, thus reconfirming the diagnosis [Figure 6]. The patient and his family members were informed about the diagnosis, treatment plan, and prognosis of the condition. However, the patient declined the invasive treatment and did not appear for regular follow-up.
Figure 1.

Diffuse extraoral swelling in the right maxillary anterior region
Figure 2.

Pigmented, lobulated growth in the right maxillary alveolus region
Figure 3.

Cropped pantomogram showing a radiolucent lesion with ill-defined margins in relation to maxillary canine to maxillary first molar
Figure 4.
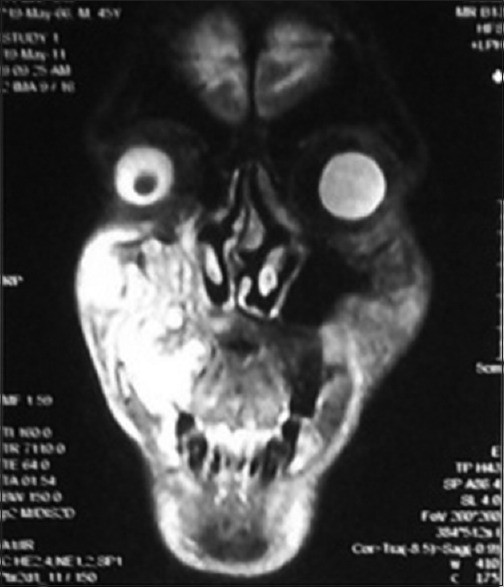
MRI showing a hyperintense lesion involving the right maxillary sinus and right maxillary alveolar arch with extension to gingivobuccal sulcus
Figure 5.
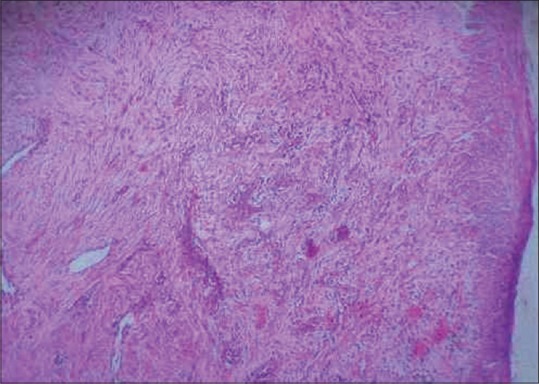
Histopathology showing spindle-shaped melanocytic cells with large nuclei, prominent nucleoli, and pigmented cytoplasm invading and ulcerating the epithelium
Figure 6.
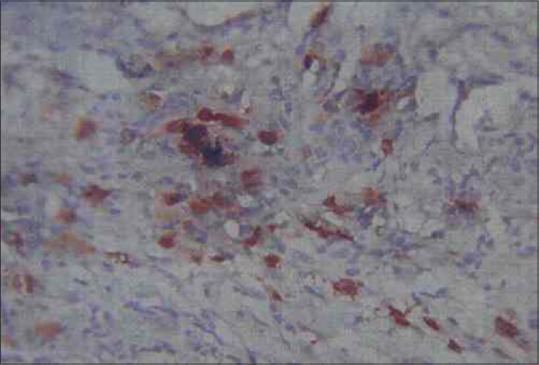
Immunohistochemistry showing strong reactivity of tumor cells to HMB-45
DISCUSSION
Weber was the first to report a case of OMM as early as in 1856.[8] The etiology of malignant melanoma remains obscure. However, the predisposing factors are the following: Excessive exposure to sunlight [ultraviolet (UV) radiation]; psoralen and UV A radiation (PUVA) therapy; tanning salons; skin (freckles) and hair color; large, atypical nevi; xeroderma pigmentosum, immunosuppression; ill-fitting denture; and environmental exposure to chemicals, tobacco, petroleum, and printing products. Primary oral melanomas originate either from a nevus or preexisting pigmented lesion, currently most thought to arise de novo.[9,10,11]
The mucosa of the upper jaw accounts for nearly 80% of oral melanomas, with the keratinizing mucosa of the palate and the alveolar gingiva being the most common sites of occurrence.[12] The disease has a male preponderance (male-to-female ratio 2.8:1) and the age range is 20–83 years with an average age of 56 years.[13] Japanese, black Africans, American Indians, and Hispanics are the most commonly affected ethnic groups.[14]
OMM usually has an asymptomatic clinical appearance and progresses unnoticed by the patient, and this results in a delayed diagnosis. Pigmented growths or swellings are usually the early presenting features in most cases of OMM. The surface may be smooth, with an intact or ulcerated overlying mucosa. OMM are usually uniformly brown or black in color or may show color variation (black, brown, red, purple, and grey shades) or depigmentation.[15] Bleeding, faulty prostheses, loosened teeth, late healing of tooth sockets, and, rarely, pain are some of the reported uncommon manifestations.[16] About 78% of cases are associated with widespread bone destruction.[17]
The clinical features of OMM may be summarized by the ABCDE rule: Asymmetry, where one half show variation from the other; Border irregularity, with blurred, notched, or ragged edges; Color disparity, with varied pigmentation, such as black, brown, tan, red, white, or blue; Diameter more than 6 mm; and Elevated surface of the lesion.[10]
Malignant melanoma usually manifests in the following five clinical types: Pigmented nodular type, nonpigmented nodular type, pigmented macular type, pigmented mixed type, and nonpigmented mixed type.[12,13]
Atypical melanocytes (usually larger than normal melanocytes, along with nuclear pleomorphism and hyperchromatism), high density of melanocytes, and atypical cells in the biopsy of melanotic lesions of the oral mucosa contribute to the histopathology of OMM.[18] Based on its histopathological pattern, the Western Society of Teachers of Oral Pathology (WESTOP) classifies OMM into: (a) Melanoma in situ, in which the tumor cells are seen in the epidermis and its interface with the connective tissue; (b) invasive melanomas, in which the tumor cells invade the connective tissue; and (c) melanomas with a combined pattern between invasive and in situ.[15]
Immunohistochemistry studies show a strong reactivity of tumor cells to S-100 protein, melan- A, and HMB-45, and are beneficial in distinguishing oral melanomas from other malignancies.[18]
Clinical staging of tumor, node, metastases (i.e. TNM) in association with histopathological microstaging is a beneficial factor in the prognosis of OMM, as given below.[3,19]
Stage I: Presence of primary tumor (Tany N0 M0)
Level I: Pure in situ melanoma with either absence of invasion or in situ melanoma with “microinvasion”
Level II: Involvement of the lamina propria
Level III: Invasion into the deep skeletal tissue (skeletal muscle, bone, or cartilage)
Stage II: Metastasis of tumor to regional lymph nodes (Tany N1 M0)
Stage III: Metastasis of tumor to distant sites (Tany Nany M1).
A simple and practical method for the clinical diagnosis of OMM was proposed by Delgado-Azañero and Mosqueda-Taylor, and 84.6% of OMM cases may be diagnosed by this method. In this test, the lesion is rubbed with a gauze piece and observed for black staining (lesional melanin pigment attributes for the black staining). The method is highly sensitive and aids in diagnosis.[20]
Metastasis to the regional submandibular and cervical lymph nodes may be demonstrated by the computed tomography and MRI. However, incisional biopsy remains as the gold standard for diagnosis.[21] Exfoliative cytology and fine-needle aspiration of the primary pigmentary lesion may cause the malignant cells to not only spread within the adjacent tissues, but also cause hematogenous and lymphatic spread. This may contribute to a higher risk of local recurrence and metastasis to the regional or distant sites.[14]
In this case, MRI showed a hyperintense lesion involving the right maxillary sinus and right maxillary alveolar arch with extension to the gingivobuccal sulcus.
According to Greene et al., the following three parameters aids in the diagnosis of primary oral melanoma:[22]
Presence of malignant melanoma in the oral mucosa
Positive “junctional activity”
Absence of malignant melanoma at any other primary site.
The lymph nodes, liver, and lungs are the common sites of metastases. The tumor is best managed by an excisional biopsy followed by a wide surgical excision. Radiotherapy and chemotherapy are used as adjunctive treatment modalities.[9]
Surgical exploration forms the cornerstone for the management of malignant melanoma, and vigorous surgical extirpation of local disease may result in extended disease-free survival.[23,24] However, preoperatively confirmed cases of lymph node metastases should be managed with neck dissection.[5] The enblock resection minimizes the chances of local recurrence, with insignificant effect on metastasis and survival.
Melanoma was earlier considered to be radioresistant in nature, but radiotherapy is now believed to be a significant adjuvant in attaining local control and may even have merit as a primary treatment option.[25] In addition, primary irradiation is considered as a possible substitute for surgery for inoperable cases.
A breakthrough in the evaluation and management of malignant melanoma has been achieved by the use of biotherapy including interferons (IFNs) and IL-2. IL-2 may have a direct action on a biologically distinct subset of melanoma cells, thus, leading to upregulation of tumor suppressor IL-24.[26]
Minimal success has been achieved by the use of imunotherapeutic agents, such as BCG, which aims at activation of the host immune response. IFN and cimetidine are the other immunotherapeutic drugs, which act synergistically on killer and suppressor T cells, thereby causing a reduction in the tumor size.
The patient in the present case declined the invasive surgical treatment and did not follow up.
Oral melanoma is associated with poor prognosis. Anatomical considerations (proximity of bone and muscles) facilitate the early invasion of deeper structures, thus increasing the chances of metastasis. Another contributing factor in the dissemination of melanoma is the rich vascular supply of oral cavity.[27]
CONCLUSION
OMM is a rare tumor of melanocytic cells. It is considered a dreaded condition because of its rapidly invasive and metastatic nature. The primary objective of reporting this rare case is to emphasize the need for vigorous scrutinizing of the indolent pigmented lesions and highlighting the significance of biopsy as an aid in the prompt diagnosis of OMM. The bizarre morphological features, extreme rarity of occurrence (less than 1%), and an unpredictable and aggressive behavior necessitate that such cases should be reported, thus facilitating the timely diagnosis, treatment, and better prognosis of this uncommon pathology. This case report is unique in the sense that the primary lesion is seen on the maxillary gingiva, and metastatic lesion has been ruled out by thorough clinical and radiographical examination.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Femiano F, Lanza A, Buonaiuto C, Gombos F, Di Spirito F, Cirillo N. Oral malignant melanoma: A review of the literature. J Oral Pathol Med. 2008;37:383–8. doi: 10.1111/j.1600-0714.2008.00660.x. [DOI] [PubMed] [Google Scholar]
- 2.Tremblay JF, O'Brien EA, Chauvin PJ. Melanoma in situ of the oral mucosa in an adolescent with dysplastic nevus syndrome. J Am Acad Dermatol. 2000;42:844–6. doi: 10.1067/mjd.2000.105556. [DOI] [PubMed] [Google Scholar]
- 3.Prasad ML, Patel S, Hoshaw-Woodard S, Escrig M, Shah JP, Huvos AG, et al. Prognostic factors for malignant melanoma of the squamous mucosa of the head and neck. Am J Surg Pathol. 2002;26:883–92. doi: 10.1097/00000478-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Gu GM, Epstein JB, Morton TH. Intraoral melanoma: Long-term follow up and implication for dental clinicians. A case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:404–13. doi: 10.1016/s1079-2104(03)00320-2. [DOI] [PubMed] [Google Scholar]
- 5.Sharma N. Primary oral malignant melanoma: Two case reports and review of literature. Case Rep Dent. 2012;2012:975358. doi: 10.1155/2012/975358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Little JW. Melanoma: Etiology, treatment, and dental implications. Gen Dent. 2006;54:61–7. [PubMed] [Google Scholar]
- 7.Munde A, Juvekar MV, Karle RR, Wankhede P. Malignant melanoma of the oral cavity: Report of two cases. Contemp Clin Dent. 2014;5:227–30. doi: 10.4103/0976-237X.132352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vikey AK, Vikey D. Primary malignant melanoma, of head and neck: A comprehensive review of literature. Oral Oncol. 2012;48:399–403. doi: 10.1016/j.oraloncology.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 9.Gondivkar SM, Indurkar A, Degwekar S, Bhowate R. Primary oral malignant melanoma - A case report and review of the literature. Quintessence Int. 2009;40:41–6. doi: 10.3290/j.qi.a14113. [DOI] [PubMed] [Google Scholar]
- 10.Rajendran R, Sivapathasundharam B. Shafer, Hine, Levy's Shafer's Text Book of Oral Pathology. 6th ed. Vol. 80. India: Elsevier; Benign and malignant tumors of the oral cavity; 2009. p. 215. [Google Scholar]
- 11.Manganaro A, Hammond H, Dalton M, Williams TP. Oral melanoma: Case report and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;85:670–6. doi: 10.1016/s1079-2104(05)80250-1. [DOI] [PubMed] [Google Scholar]
- 12.Dimitrakopoulos I, Lazaridis N, Skordalaki A. Primary malignant melanoma of the oral cavity. Report of an unusual case. Aust Dent J. 1998;43:379–81. [PubMed] [Google Scholar]
- 13.Tanaka N, Mimura M, Ichinose S, Odajima T. Malignant melanoma in the oral region: Ultrastructural and immunohistochemical studies. Med Electron Microsc. 2001;34:198–205. doi: 10.1007/s007950100016. [DOI] [PubMed] [Google Scholar]
- 14.Meleti M, Leemans CR, Mooi WJ, Vescovi P, van der Waal I. Oral malignant melanoma: A review of the literature. Oral Oncol. 2007;43:116–21. doi: 10.1016/j.oraloncology.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Barker BF, Carpenter WM, Daniels TE, Kahn MA, Leider AS, Lozada-Nur F, et al. Oral mucosal melanomas: The WESTOP Banff workshop proceedings. Western Society of Teachers of Oral Pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:672–9. doi: 10.1016/s1079-2104(97)90318-8. [DOI] [PubMed] [Google Scholar]
- 16.Lopez-Graniel CM, Ochoa-Carrillo FJ, Meneses-García A. Malignant melanoma of the oral cavity: Diagnosis and treatment Experience in a Mexican population. Oral Oncol. 1999;35:425–30. doi: 10.1016/s1368-8375(99)00017-2. [DOI] [PubMed] [Google Scholar]
- 17.Prabhu SR, Wilson DF, Daftary DK. Oral Diseases in the Tropics. New York: Oxford University Press; 1992. pp. 460–1. [Google Scholar]
- 18.Neville BW, Damm D, Allenc R, Bouquot JE. Oral and Maxillofacial Pathology. 2nd ed. Philadelphia: WB Saunders; 2002. pp. 334pp. 376–80. [Google Scholar]
- 19.Prasad ML, Busam KJ, Patel SG, Hoshaw-Woodard S, Shah JP, Huvos AG. Clinicopathologic differences in malignant melanoma arising in oral squamous and sinonasal respiratory mucosa of the upper aerodigestive tract. Arch Pathol Lab Med. 2003;127:997–1002. doi: 10.5858/2003-127-997-CDIMMA. [DOI] [PubMed] [Google Scholar]
- 20.Delgado-Azañero WA, Mosqueda-Taylor A. A practical method for clinical diagnosis of oral mucosal melanomas. Med Oral. 2003;8:348–52. [PubMed] [Google Scholar]
- 21.Greenberg MS, Glic KM. Burket's Oral Medicine. 9th ed. Hamilton: BC Decker; 2003. pp. 131–2.pp. 214–5. [Google Scholar]
- 22.Greene GW, Haynes JW, Dozier M, Blumberg JM, Bernier JL. Primary malignant melanoma of the oral mucosa. Oral Surg Oral Med Oral Pathol. 1953;6:1435–43. doi: 10.1016/0030-4220(53)90242-4. [DOI] [PubMed] [Google Scholar]
- 23.Rapidis A, Apostolidis C, Vilos G, Valsamis S. Primary malignant melanoma of the oral mucosa. J Oral Maxillofac Surg. 2003;61:1132–9. doi: 10.1016/s0278-2391(03)00670-0. [DOI] [PubMed] [Google Scholar]
- 24.Bhullar RP, Bhullar A, Vanaki SS, Puranik RS, Sudhakara M, Kamat MS. Primary melanoma of oral mucosa: A case report and review of literature. Dent Res J (Isfahan) 2012;9:353–6. [PMC free article] [PubMed] [Google Scholar]
- 25.Trotti A, Peters LJ. Role of radiotherapy in the primary management of mucosal melanoma of the head and neck. Semin Surg Oncol. 1993;9:246–50. [PubMed] [Google Scholar]
- 26.Jen EY, Poindexter NJ, Farnsworth ES, Grimm EA. IL-2 regulates the expression of the tumor suppressor IL-24 in melanoma cells. Melanoma Res. 2012;22:19–29. doi: 10.1097/CMR.0b013e32834d2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wanjari PV, Warhekar AM, Wanjari SP, Reddy V, Tekade S, Shrivastava P. Primary oral malignant melanoma. J Indian Acad Oral Med Radiol. 2011;23:76–9. [Google Scholar]


