Abstract
Objective:
India suffers lot of disparities in terms of oral health care and 95% of the Indian population suffers from periodontal disease. The aim of this review is to estimate the risk factors responsible for periodontal diseases as well as prevalence for the same in the last decade to make an attempt to develop a strategy to improve formulation of an effective oral health care policy in India.
Materials and Methods:
Keywords such as “prevalence of periodontal diseases,” “epidemiology,” “periodontitis in India,” and “oral hygiene status in India” were searched for appropriate studies to obtain a bibliographic database. The references of selected articles and relevant reviews were searched for any missed publications that included studies conducted in India estimating periodontal diseases with adequate sample size. Clinical parameters, sample size, and findings for each study were tabulated from 2006 to 2015 (till September 15, 2015) in chronological order to observe the prevalence as well as epidemiology of periodontal disease in India.
Results:
The projection of periodontal disease is disturbing. In addition, the majority of studies done have used the Community Periodontal Index of Treatment Needs (CPITN) as its epidemiological tool that can grossly underestimate the presence of deep pockets.
Conclusion:
Current knowledge has shown that periodontitis does not present a linear progression and is not age-dependent. Moreover, its distribution and severity are strongly influenced by host susceptibility and risk factors. A structured all-inclusive survey of all districts of the states is a prerequisite for the constitution of an apt and cogent health care policy in our country.
Keywords: Community Periodontal Index of Treatment Needs, epidemiology, India, periodontal disease, periodontitis in India, prevalence
INTRODUCTION
India represents almost 17.31% of the world's population, which means that one out of six people on this planet live in India. About 72.2% of the population live in approximately 638,000 villages and the remaining 27.8% in approximately 5,480 towns and urban agglomerations.[1] In a federation composed of 29 states and 7 union territories, it was revealed that the population ratio was 940 females per 1,000 males in the Population Census of 2011.[2] In addition, life expectancy in India is at 68 years, with life expectancy for women being 69.6 years and for men 67.3 years.[3]
India reveals a lot of disparities in terms of ratios, one of which is the field of the oral health. The dentist-to-population ratio in the rural areas is dismally low with less than 2% dentists being available for 72% of the rural population. Statistics present the grim reality that 95% of the population in India suffer from periodontal disease, only 50% use a toothbrush, and just 2% visit the dentist;[4] 23,690 undergraduate and 1,138 postgraduate students are educated in 291 dental colleges in India.
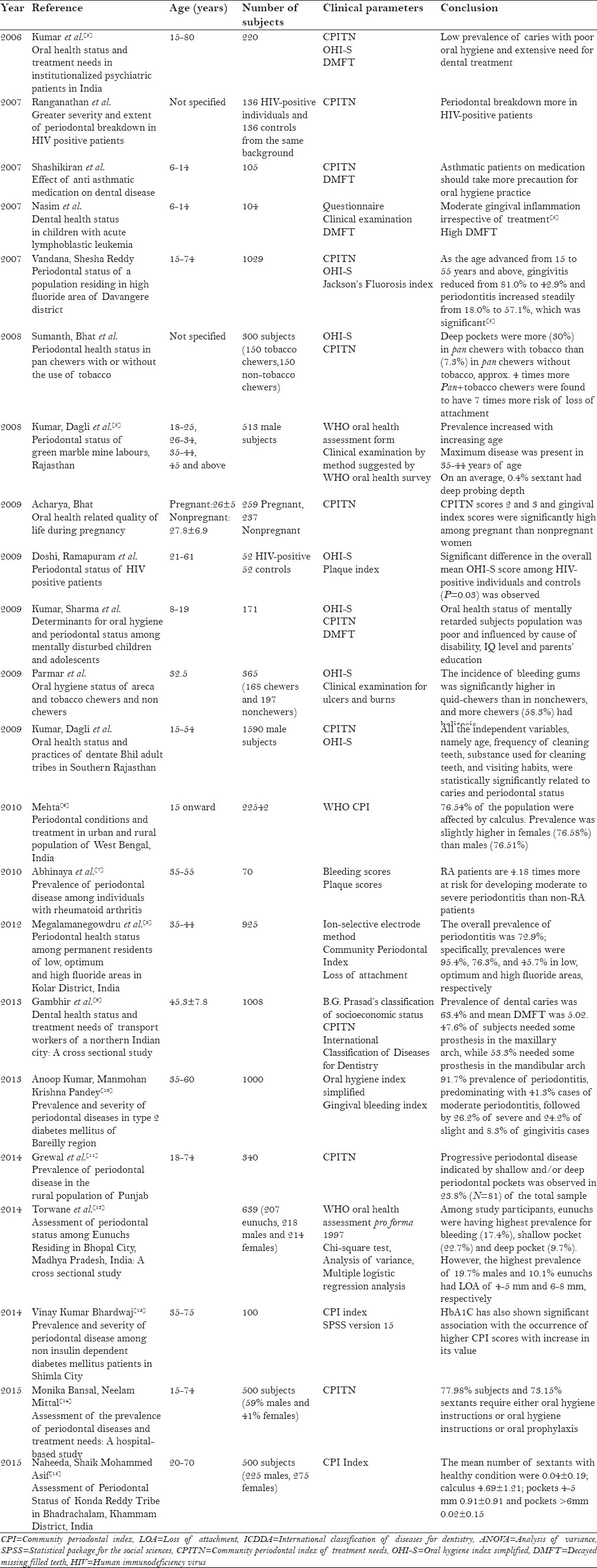
In order to calculate the risk factors responsible for periodontal diseases as well as prevalence of the same, various local as well as regional surveys have been directed across the country. A brief description is mentioned in Table 1 for some of the surveys that were done since the last decade in India.
Table 1.
Local/regional surveys conducted in India to estimate periodontal diseases
MATERIALS AND METHODS
“Prevalence of periodontal diseases,” “epidemiology,” “periodontitis in India,” and “oral hygiene status in India” were the key words used to search Medline, the National Library of Medicine, PubMed, EBSCOhost, and Google to obtain a bibliographic database of the biomedical literature produced. About 30 studies were retrieved. Inclusion criteria were: (1) Adequate sample size (2) Study conducted in India to estimate prevalence of periodontal diseases (3) Study conducted in last 10 years, i.e., from 2006 to 2015 at the time of writing (September 15, 2015). Data were organized in tabulated form and arranged in chronological order for easy and comprehendible understanding of the prevalence as well as the epidemiology of periodontal diseases. Sample size, clinical parameters, and findings for each of the study was taken into account.
DISCUSSION
In the last 10 years, the alarming rate of prevalence of periodontal disease in India has drawn interest from various parts of the country. The dentist-to-population ratio of about 1:200000 in rural areas necessitates building up of the dental infrastructure at the primary health care center level. Sikri et al. observed that there is a direct effect on the prevalence of periodontal disease if access to the village health center is easy. Community health centers serve as a good option for the upliftment of oral health, but due to lack of dental equipment, materials, and instruments, they are not fully functional. Most of the hospitals and teaching institutions that organize regular dental checkups and encourage people regarding the prevention and treatment of existing dental disease are located in urban areas. Therefore it is less likely for rural areas to avail benefits from these because of conveyance problem.[16]
About half of the world's autochthonous people, comprising 635 tribal communities including 75 primitive tribal communities, live in India. The accessibility of these tribes to medical and dental care is minimal. They practice their own traditional methods to treat disease and alleviate pain. A recent study was conducted with an aim to determine the prevalence of periodontal disease in Konda Reddy tribes residing in Bhadrachalan, Khammam District[15] and it was observed that a majority of 93.60% of them cleaned their teeth using twigs and only 6.20% of them cleaned their teeth with a combination of toothbrush, finger, and twig with toothpaste and charcoal.
Waerhaug et al. gave an explanation for a strong correlation between age and periodontal breakdown. The equilibrium between plaque attack and host response may be disturbed and as a consequence, progression of periodontal disease can occur. Numerous studies done have given unswerving results.[5] Despite remarkable progress in the field of diagnostic, curative, and preventive medicine, we are yet to see optimum oral health in subjects with mental retardation,[17] Human immunodeficiency virus (HIV) positive status, pregnancy, diabetes, and rheumatoid arthritis.[5] Less efficiency in maintaining oral hygiene is one of the causes for compromised oral health in subjects with low intelligence quotient (IQ).
As the 21st century proverb goes, the mouth is the portal to the body; we must know that periodontal health is not only related to the diseases, it has also proven its association with osteoporosis,[18] preterm births (Lopez et al.),[19] preeclampsia (Ramos et al. 1995),[20] and erectile dysfunction (Zadik et al. 2008,[21] Sharma et al. 2011[22]). There is growing evidence of an association between periodontitis and sporadic late-onset Alzheimer's disease. Recent epidemiologic, microbiologic, and inflammatory findings strengthen this association.[23] The association of periodontitis and peptic ulcers appeared largely consistent for gastric and duodenal ulcers as well as H. pylori-positive and H. pylori-negative ulcers. These observed associations persisted even after adjusting for putative risk factors, including smoking, alcohol intake, and regular use of aspirin and nonsteroidal antiinflammatory drugs (NSAIDs).[24] However, there is a lack of literature available on the epidemiological surveys conducted on these diseases with adequate sample size.
We observe that the majority of surveys conducted in the last decade have used Community Periodontal Index of Treatment Needs (CPITN) as an epidemiological tool but a plethora of studies point out the demerits of the same. The hierarchical principles underlying its use are not universally valid (Takahashi 1988,[25] Miller 1988[26]). Ainamo (1985),[27] Gaengler (1988),[28] and Miller (1990)[29] suggested that the partial recording approach of CPITN may grossly underestimate the prevalence of deep pockets. Baelum et al. in 1995[30] observed that CPITN yields extensively distorted estimates of the prevalence and severity of periodontal destruction in a population. Given the very severe shortcomings of CPITN, we see no place for this particular system in this context.
Shah[31] observed that for periodontal diseases, the projection is alarming, with prevalence at present being 45% for the 15+ years age group and the actual prevalence in lakhs at 3413.8 (year 2010) and 3624.8 (year 2015). Due to the rampant use of pan masala and gutkha by persons of all age groups, the proportion of the population above the age of 15 years with this disease could be 80–90%. Concerned[32] with the urgent need for action, it is vital to promote sound oral health, prevent dental caries and periodontal diseases, and give impetus to activities that promote oral health.
CONCLUSION
The final purpose of epidemiology is to apply the knowledge gained from studies to “promote, protect and restore health.” For planning of national or regional oral health promotion programs, to prevent and treat oral health problems, baseline data about a magnitude of problems and various epidemiological factors are required. There is a dire need for a comprehensive survey of all districts of the State to access the prevalence of periodontal disease over a wider geographic area in order to develop a strategy to improve the periodontal status of the population as a whole. Such surveys do help the government to take the necessary steps to improve the health and living status of the population. Government hospitals, health centers and dispensaries, dental teaching institutions, and even private practitioners can generate such data, which will contribute tremendously to the formulation of a sound and effective oral health care policy in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Malisetty VS. Text on Retail Management. 1st ed. Solapur: Laxmi Book Publication; 2012. p. 121. [Google Scholar]
- 2.Stein B. A History of India. 1st ed. Oxford: Wiley-Blackwell; 1998. [Google Scholar]
- 3.Ram P. Life in India. Great Britain: Anvi; 2014. p. 12. [Google Scholar]
- 4.Blas E, Kurup AS. Equity, Social Determinants and Public Health Programmes. Geneva: World Health Organization; 2010. p. 291. [Google Scholar]
- 5.Agarwal V, Khatri M, Singh G, Gupta G, Marya CM, Kumar V. Prevalence of periodontal diseases in India. J Oral Health Community Dent. 2010;4:7–16. [Google Scholar]
- 6.Mehta R, Kundu D, Chakrabarty S, Bharati P. Periodontal conditions and treatment in urban and rural population of West Bengal, India. Asian Pac J Trop Med. 2010;3:152–7. [Google Scholar]
- 7.Abinaya P, Kumar R. Prevalence of periodontal disease among individuals with rheumatoid arthritis. J Indian Acad Dent Spec. 2010;1:16–23. [Google Scholar]
- 8.Megalamanegowdru J, Ankola AV, Vathar J, Vishwakarma P, Dhanappa KB, Balappanavar AY. Periodontal health status among permanent residents of low, optimum and high fluoride areas in Kolar District, India. Oral Health Prev Dent. 2012;10:175–83. [PubMed] [Google Scholar]
- 9.Gambhir RS, Sogi GM, Veeresha KL, Sohi RK, Randhawa A, Kakar H. Dental health status and treatment needs of transport workers of a northern Indian city: A cross-sectional study. J Nat Sci Biol Med. 2013;4:451–6. doi: 10.4103/0976-9668.117010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar A, Pandey MK, Singh A, Mittra P, Kumar P. Prevalence and severity of periodontal diseases in type 2 diabetes mellitus of Bareilly region (India) Int J Med Sci Public Health. 2013;2:77–83. [Google Scholar]
- 11.Grewal Y, Datta R, Singh K, Singh G, Singh S, Kaur P. Prevalence of Periodontal Disease in the Rural Population of Punjab. J Pharm Biomed Sci. 2014;4:532–5. [Google Scholar]
- 12.Torwane AN, Hongal S, Saxena E, Rana PT, Jain S, Gouraha A. Assessment of periodontal status among Eunuchs Residing in Bhopal City, Madhya Pradesh, India: A cross-sectional study. Oral Health Dent Manag. 2014;13:628–33. [PubMed] [Google Scholar]
- 13.Bhardwaj VK. Prevalence and severity of periodontal disease among non-insulin-dependent diabetes mellitus patients in Shimla City, Himachal Pradesh, India. J Cranio Max Dis. 2014;3:11–6. [Google Scholar]
- 14.Bansal M, Mittal N, Singh TB. Assessment of the prevalence of periodontal diseases and treatment needs: A hospital-based study. J Indian Soc Periodontol. 2015;19:211–5. doi: 10.4103/0972-124X.145810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naheeda, Asif SM, Padma M, Paul A. Assessment of periodontal status of Konda Reddy Tribe in Bhadrachalam, Khammam District, India. J Clin Diagn Res. 2015;9:ZC23–5. doi: 10.7860/JCDR/2015/13430.6051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vimal S. National Community Dentistry. 1st ed. Bangalore: CBS Publication; 1999. pp. 19–38. [Google Scholar]
- 17.Jain M, Mathur A, Sawla L, Choudhary G, Kabra K, Duraiswamy P, et al. Oral health status of mentally disabled subjects in India. J Oral Sci. 2009;51:333–40. doi: 10.2334/josnusd.51.333. [DOI] [PubMed] [Google Scholar]
- 18.Ruggiero SL. Special Committee on Medication Related Osteonecrosis of the Jaws. Illinois, United States: American Association of Oral and Maxillofacial Surgeons; 2014. pp. 1–26. [Google Scholar]
- 19.Lopez NJ, Da Silva I, Ipinza J, Gutiérrez J. Periodontal therapy reduces the rate of preterm low birth weight in women with pregnancy-associated gingivitis. J Periodontol. 2005;76(Suppl):2144–53. doi: 10.1902/jop.2005.76.11-S.2144. [DOI] [PubMed] [Google Scholar]
- 20.Sanchez-Ramos L, Jones DC, Cullen MT. Urinary calcium as an early marker for preeclampsia. Obstet Gynecol. 1991;77:685–8. [PubMed] [Google Scholar]
- 21.Zadik Y, Bechor R, Galor S, Justo D, Heruti RJ. Erectile dysfunction might be associated with chronic periodontal disease: Two ends of the cardiovascular spectrum. J Sex Med. 2009;6:1111–6. doi: 10.1111/j.1743-6109.2008.01141.x. [DOI] [PubMed] [Google Scholar]
- 22.Sharma A, Pradeep AR, Raju PA. Association between chronic periodontitis and vasculogenic erectile dysfunction. J Periodontol. 2011;82:1665–9. doi: 10.1902/jop.2011.110049. [DOI] [PubMed] [Google Scholar]
- 23.Gurav AN. Alzheimer's disease and periodontitis-An elusive link. Rev Assoc Med Bras. 2014;60:173–80. doi: 10.1590/1806-9282.60.02.015. [DOI] [PubMed] [Google Scholar]
- 24.Boylan MR, Khalili H, Huang ES, Michaud DS, Izard J, Joshipura KJ, et al. A prospective study of periodontal disease and risk of gastric and duodenal ulcer in male health professionals. Clin Transl Gastroenterol. 2014;5:e49. doi: 10.1038/ctg.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Takahashi Y, Kamijyo H, Kawanishi S, Takaesu Y. Presence and absence of bleeding in association with calculus in segments given Code 2 in the Community Periodontal Index of Treatment Needs (CPITN) Community Dent Oral Epidemiol. 1988;16:109–11. doi: 10.1111/j.1600-0528.1988.tb01854.x. [DOI] [PubMed] [Google Scholar]
- 26.Miller NA, Benamghar L, Roland E, Martin J, Abt F. An analysis of the CPITN periodontal treatment needs in France. Community Dent Health. 1987;4:415–23. [PubMed] [Google Scholar]
- 27.Ainamo J, Tervonen T, Ainamo A. CPITN-assessment of periodontal treatment needs among adults in Ostrobothnia, Finland. Community Dent Health. 1986;3:153–61. [PubMed] [Google Scholar]
- 28.Gaengler P, Goebel G, Kurbad A, Kosa W. Assessment of periodontal disease and dental caries in a population survey using the CPITN, GPM/T and DMF/T indices. Community Dent Oral Epidemiol. 1988;16:236–9. doi: 10.1111/j.1600-0528.1988.tb01762.x. [DOI] [PubMed] [Google Scholar]
- 29.Miller NA, Benamghar L, Roland E, Martin G, Penaud J. An analysis of the Community Periodontal Index of Treatment Needs. Studies on adults in France. III-Partial examinations versus full-mouth examinations. Community Dent Health. 1990;7:249–53. [PubMed] [Google Scholar]
- 30.Baelum V, Manji F, Wanzala P, Fejerskov O. Relationship between CPITN and periodontal attachment loss findings in an adult population. J Clin Periodontol. 1995;22:146–52. doi: 10.1111/j.1600-051x.1995.tb00126.x. [DOI] [PubMed] [Google Scholar]
- 31.Shah N. Oral and Dental Diseases: Causes, Prevention and Treatment Strategies In NCMH Background Papers-Burden of Disease in India (New Delhi, India) New Delhi: India; National Commission on Macroeconomics and Health, Ministry of Health and Family Welfare; pp. 275–98. [Google Scholar]
- 32.Doifode VV, Ambadekar NN, Lanewar AG. Assessment of oral health status and its association with some epidemiological factors in population of Nagpur, India. Indian J Med Sci. 2000;54:261–9. [PubMed] [Google Scholar]


