Supplemental Digital Content is available in the text.
Background:
Multiple studies of ovarian cancer and genital talc use have led only to consensus about possible carcinogenicity. Seeking greater clarity, we examined this association in 2,041 cases with epithelial ovarian cancer and 2,100 age- and-residence-matched controls.
Methods:
We defined genital talc use as regular application to the genital/rectal area directly, on sanitary napkins, tampons, or underwear. To estimate “talc-years,” we multiplied applications per year by years used. Unconditional logistic regression, Wald statistics, likelihood-ratio tests, and polytomous logistic regression were used to calculate adjusted odds ratios (OR) and 95% confidence intervals (CI), trends, effect-modification, and heterogeneity by ovarian cancer histologic subtype.
Results:
Overall, genital talc use was associated with an OR (95% CI) of 1.33 (1.16, 1.52), with a trend for increasing risk by talc-years. Women who used talc were more likely to be older, heavier, asthma sufferers, and regular analgesic users—none of which was a confounder. Dose–responses were more apparent for premenopausal women, especially nonsmokers and those heavier or postmenopausal users of menopausal hormones (hormone therapy [HT]). Subtypes of ovarian cancer more likely to be associated with talc included invasive serous and endometrioid tumors and borderline serous and mucinous tumors. Premenopausal women and postmenopausal HT users with these subtypes who had accumulated >24 talc-years had ORs (95% CI) of 2.33 (1.32, 4.12) and 2.57 (1.51, 4.36), respectively.
Conclusion:
Risks for epithelial ovarian cancer from genital talc use vary by histologic subtype, menopausal status at diagnosis, HT use, weight, and smoking. These observations suggest that estrogen and/or prolactin may play a role via macrophage activity and inflammatory response to talc.
In the 1960s, a link between talc and ovarian cancer was suggested by observations that some talc powders contained asbestos1 and that asbestos placed intraperitoneally in animals transformed the single layer of the ovarian surface to a multilayered one with abnormal cells.2 A 1971 study found particles compatible with talc in human ovarian and uterine cancers.3 A 1982 case–control study was the first to link genital talc use with ovarian cancer.4 Dozens more followed confirming the association including some larger ones cited here.5–13 The most recent meta-analysis reported a summary odds ratio (OR) and 95% confidence interval (CI) of 1.35 (1.26, 1.46).14 In 2006, the International Agency for Research on Cancer declared that talc used genitally is possibly carcinogenic.15 However, a study with null results from the Women’s Health Initiative (WHI)16 and accompanying editorial17 cast new skepticism on the association. Here, we present data from combined phases of a case–control study of ovarian cancer involving more than 4,000 women to provide fresh perspectives on this association.
METHODS
Study Population
Data come from three enrollment phases: 1 (1992–1997), 2 (1998–2002), and 3 (2003–2008). Articles we previously published related to talc include a detailed report from phase 1,7 data from phases 1 and 2 combined with Nurses’ Health Study data,18 and phases 1–3 data combined with data from several participants in the Ovarian Cancer Association Consortium (OCAC).19 This is the first detailed examination of talc data from the combined phases of our study.
Details regarding enrollment are described elsewhere.20 In brief, 3,957 women residing in Eastern Massachusetts and New Hampshire diagnosed with ovarian cancer between ages 18 and 80 were identified through tumor boards and registries. Eight hundred and seventy-four cases were ineligible if they had died, moved outside study area, did not have a working telephone number, or had a nonovarian primary tumor. Of the remaining 3,083 cases, 2,203 (71%) were enrolled. Excluding 127 nonepithelial and 35 mixed mesodermal tumors, 2,041 cases with epithelial tumors of ovarian, primary peritoneal, and Fallopian tube origin, including borderline malignancies (henceforth, epithelial ovarian cancer) were included. Pathology reports were reviewed and histologic subtype, grade, and stage recorded. Mixed epithelial ovarian cancer was classified as the predominant type. Undifferentiated, transitional cell, fallopian tube, or primary peritoneal tumors were counted as serous.21 Other mixed epithelial (n = 102), malignant Brenner (n = 5), and unspecified epithelial tumors (n = 27) were classified as other.
Controls were identified through random digit dialing, driver-license lists, and town-resident lists. Between 1992 and 1997, 420 (72%) identified through random digit dialing and 102 (51%) through lists agreed to participate. From 1998 to 2008, 4,366 potential controls were identified using the lists, of whom 1,426 (33%) were ineligible if they had died, moved, or were seriously ill or if they did not have a working telephone, speak English, or have ovaries. Of eligible controls, 1,362 (46%) declined to participate by phone or via “opt-out” postcard and 1,578 (54%) were enrolled (2,100 total). Controls were frequency matched to cases by 5-year age groups and region of residence.
Exposure Assessment
Subjects were personally interviewed about potential ovarian cancer risk factors that occurred more than 1 year before diagnosis, for cases, and interview, for controls. Subjects were asked whether they “regularly” or “at least monthly” applied powder to the genital or rectal area, sanitary napkins or tampons, underwear, or areas other than the genital-rectal area. Additional details included type of powder, age begun, years used, and applications per month. Lifetime exposure was estimated by multiplying frequency of applications per month by months used. This was divided by 360 (i.e., daily use coded as 30/month) to yield talc-years. To create categorical variables for talc-years, we chose cut points based on quartiles for exposed controls and rounded to the nearest integer. In addition, we asked participants if their partners dusted or sprayed powder to their genital or rectal areas. Condom and diaphragm use as potential sources of talc exposure were also recorded.
We calculated ovulatory cycles by subtracting age at menarche from age at last period, reduced this by time spent pregnant, breastfeeding, or using oral contraceptives, and dividing the remainder by each woman’s average cycle length. Family history was defined as a mother or sister with ovarian or premenopausal breast cancer. Women who reported postmenopausal hormone use were classified as hormone therapy (HT) users and type(s) of HT was recorded. Participants completed a food-frequency questionnaire22 from which grams of alcohol consumed per day were estimated.
Statistical Methods
Unconditional logistic regression was used to model the OR and 95% CI adjusted first for matching factors (age, study center, and phase) and then fully by potential confounders. Likelihood ratio tests comparing models with and without interaction terms were used to test for effect modification. Tests for trend were based on the Wald statistic using continuous variables weighted by category midpoints with zero assigned as the exposure for nonusers. Polytomous logistic regression was used to simultaneously estimate separate ORs and 95% CIs for genital talc use by histologic subtypes. Likelihood-ratio tests were used to calculate P values for heterogeneity by comparing polytomous logistic regression models in which the talc association was held constant over case subgroups to models that allowed the association to differ between case subgroups.23 Analyses were performed using SAS v9.3 (SAS Institute, Cary, NC) and polytomous logistic regression analyses were performed in Stata (StataCorp LP, College Station, TX). Sensitivity analyses to assess the influence of exposure misclassification were performed with Excel using quantitative analysis methods described previously.24
Ethical Approval
Institutional review boards approved the study. All participants provided written informed consent.
RESULTS
Genital use of talc, either alone or in combination with body use, was associated with elevated epithelial ovarian cancer risk (Table 1). Among women with no personal use, there was no increased risk with potential exposure from diaphragms, condoms, or partner use. Therefore, only those with personal genital talc exposure were classified as ever-users. Genital talc use was associated with an OR (95% CI) of 1.33 (1.16, 1.52) adjusted only for age, study center, and phase. Most women reported using Johnson & Johnson’s Baby Powder or Shower to Shower. Fourteen women who reported exclusive use of a cornstarch-based powder were considered unexposed. The average age women began using talc was 20.0 for cases and 19.8 for controls. Almost half of users were currently using or had only recently discontinued powder use at the reference date. Risk decreased with increased time since last use. The trend for frequency of use was significant, but the trend for years used was flat. Some subjects reported they used talc only seasonally, but our original questionnaire did not capture this detail. A question to capture months-per-year-used was added in 1998 and was available for 54% of cases and 56% of controls. Year-round use was the most common pattern, and more cases than controls used powder year-round. ORs for talc-years among those who reported months-per-year-used are shown as the next-to-final entry in Table 1. An OR of 1.49 (95% CI = 1.06, 2.10) was associated with more than 20 talc-years (>7,200 applications) and a dose–response. For subjects missing the seasonal-use variable, we assumed 12 months per year in calculating talc-years in the final entry in Table 1, as well as in subsequent tables and figures examining talc-years. Even with this imprecision, the trend remained, although the increase was less monotonic.
TABLE 1.
Type, Timing, and Duration of Genital Talc Use
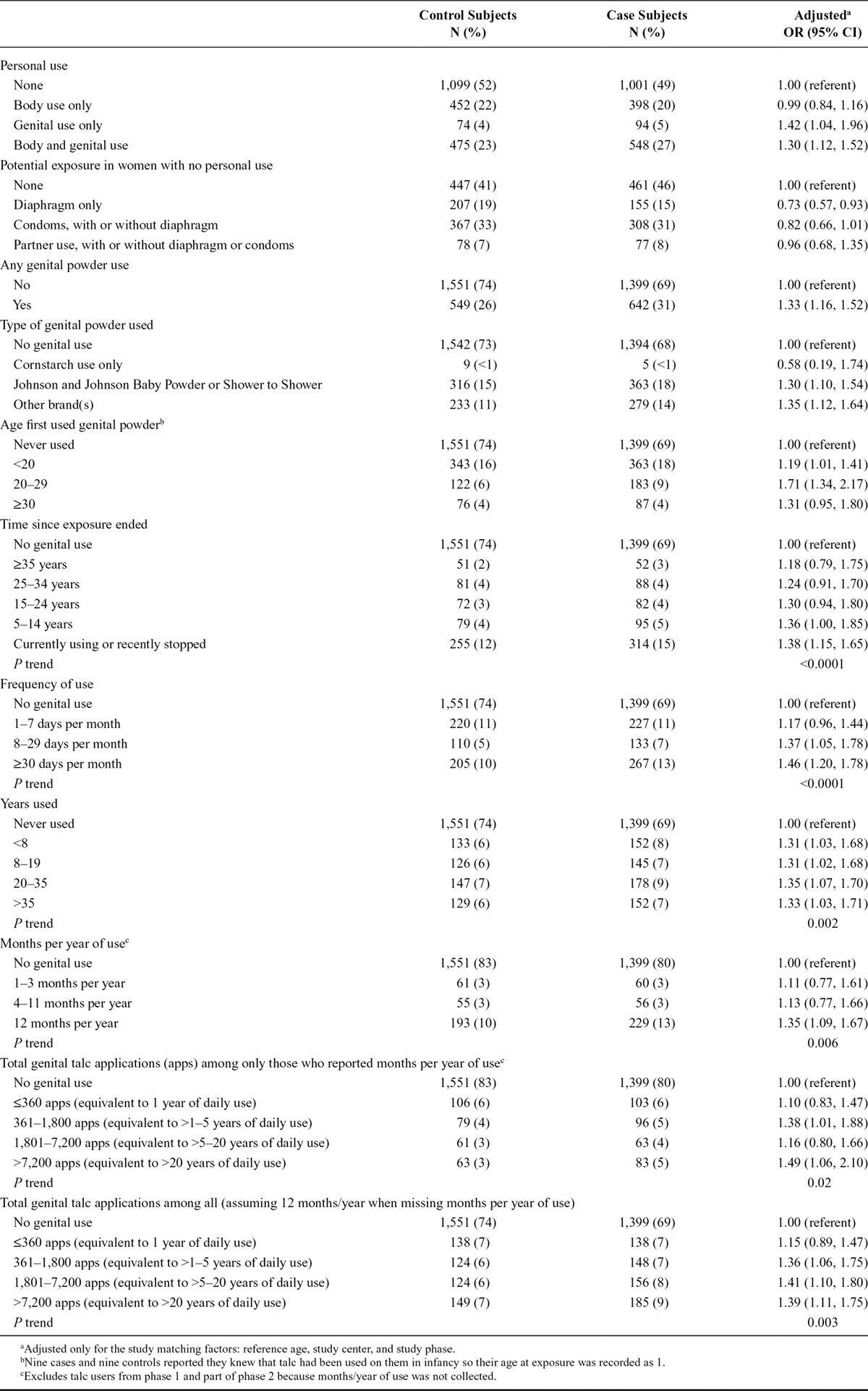
Figure 1 shows the proportions of cases and controls who used talc in the genital area by decade of birth and age at diagnosis or interview. In 13 of the 16 age-and-birth categories, a greater proportion of cases used talc compared with controls. This suggests that the association between genital use of talc and epithelial ovarian cancer is not confined to any particular age or birth cohort.
FIGURE 1.
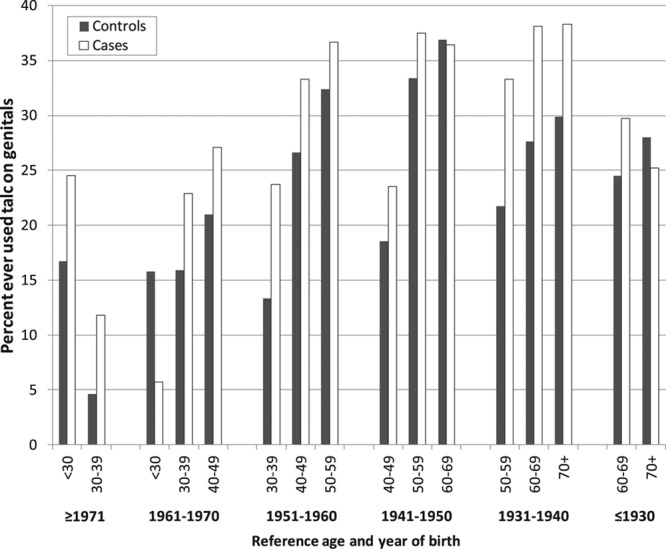
Proportions of cases and controls who ever used talc on genitals in categories by decade of birth and reference age.
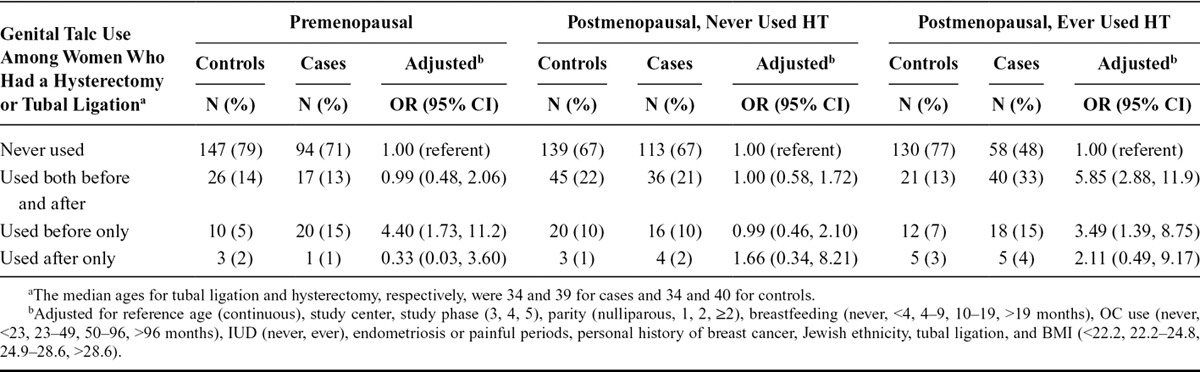
Powder users, both cases and controls, were more likely to be older, heavier, asthma sufferers, and regular analgesic users (Table 2). By tests for interaction (column 3), the association was significantly greater for women who were African American, had no personal history of breast cancer, had a tubal ligation or hysterectomy, were premenopausal, or were postmenopausal and used HT. The latter finding, together with the dose–response data, is illustrated in Figure 2. Among the HT users, 92% used estrogen (alone or in combination), 2% used progesterone alone, and 5% used creams or suppositories. Increased epithelial ovarian cancer risk with genital talc use was found in both women who had used estrogen alone or estrogen plus progesterone. Too few women used progesterone only HT or estrogen creams or suppositories to examine risk with talc use in these groups (data not shown). The median duration of HT use was 5 years. Subjects with <5 years of HT use had an overall OR (95% CI) for EOC risk with ever-use of talc on genitals of 2.93 (1.86, 4.62). Subjects with ≥5 years of HT use had an OR (95% CI) that was slightly lower, 1.73 (1.15, 2.62), but a clearer trend for increasing risk with talc-years was more apparent in the longer term HT users (data not shown). To explore the potential interaction between talc use and hysterectomy or tubal ligation, we restricted this analysis to subjects who had either or both procedures (Table 3). For premenopausal women, risk for EOC was increased in women who used talc before the procedure, while risk was elevated for use both before and after the procedure in postmenopausal women who used HT. No associations were seen in postmenopausal women who had not used HT. There were too few subjects who had used talc only after a hysterectomy or tubal ligation to permit reliable estimates of risk.
TABLE 2.
Illustrating Potential Effect Modification and Confounding
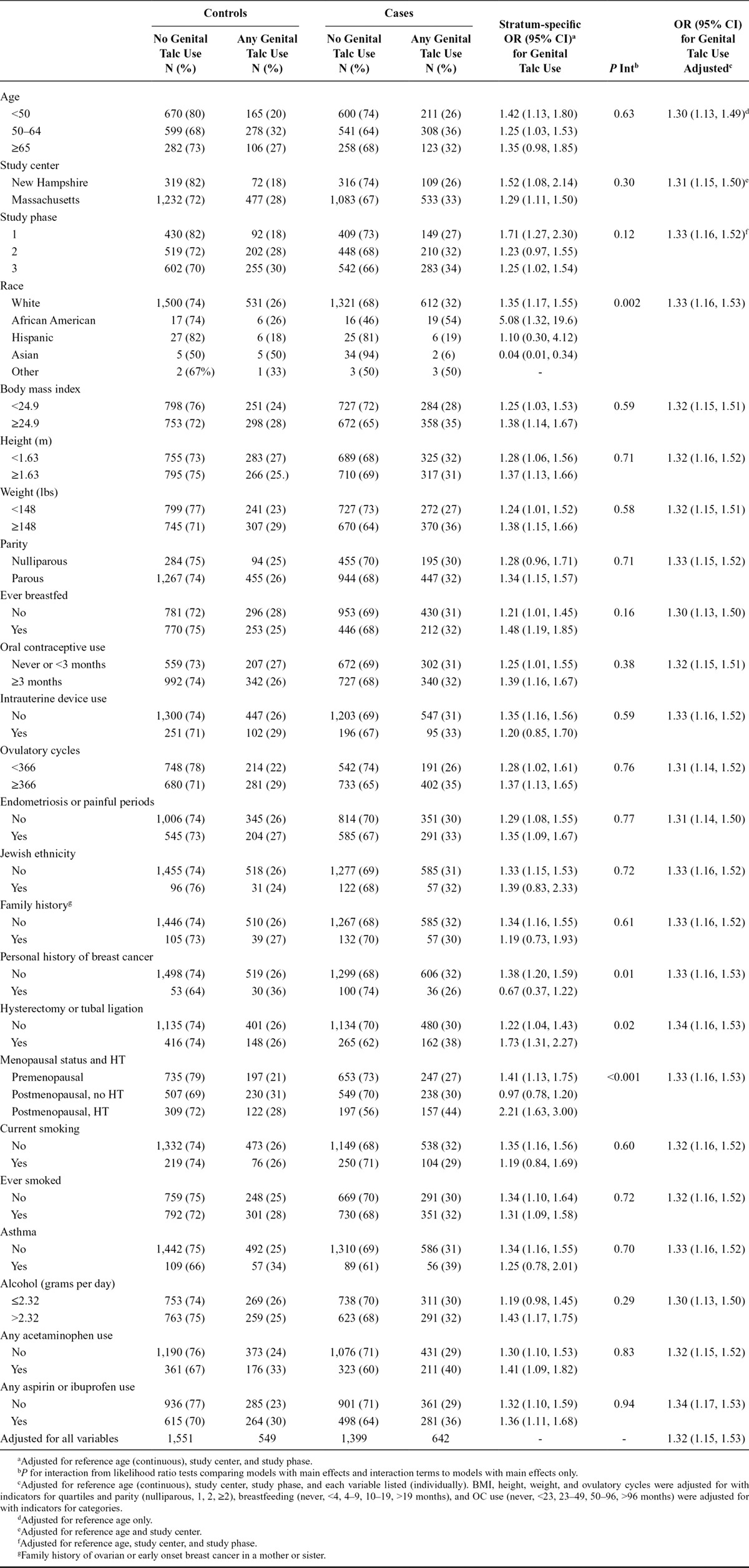
FIGURE 2.
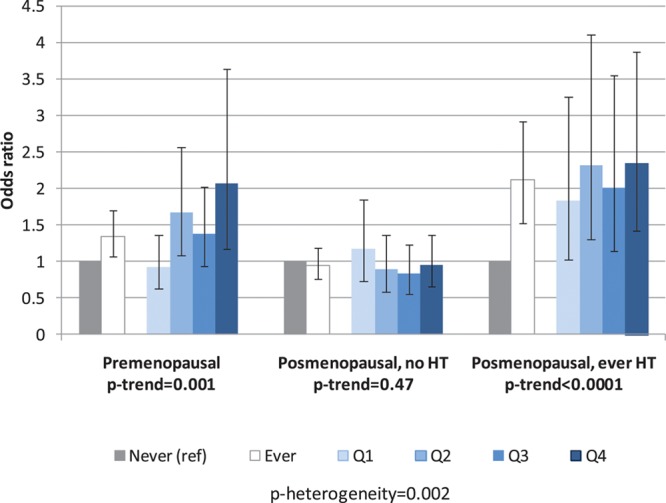
Associations between use of talc on genitals (never/ever and quartiles of talc-years) and ovarian cancer by menopausal status and postmenopausal hormone therapy.
TABLE 3.
Effect of Tubal Ligation and Hysterectomy by Menopausal Status and Hormone Therapy on Association Between Genital Talc Use and Ovarian Cancer
Returning to Table 2, we applied the convention that a variable may be a confounder if adjustment yields a 10% difference compared with the crude OR (or, in our study, compared with the OR of 1.33 adjusted for age, study center, and study phase). A 10% lower or greater change corresponds to an OR ≤1.20 or ≥1.46. As seen in the far right column, the OR of 1.33 for ovarian cancer risk was not materially changed after adjustment for any individual or all variables.
Because Figure 2 suggests that EOC risk with talc varies by menopausal status, we revisited the issue of interaction in eTable 1 (http://links.lww.com/EDE/B2) in which subjects are stratified by menopausal status. Although few significant interactions were seen, categories for several variables revealed contrasting overall associations and/or clearer dose–responses (Fig. 3). For premenopausal women, these included women with a BMI > 25, those who had breastfed, those who were not current smokers, and those who consumed more than 2.32 g of alcohol per day. In addition, the association was stronger for both pre- and post-menopausal women who were least likely to have a genetic basis for their ovarian cancer, defined as women with no personal history of breast cancer, without a primary relative with either ovarian cancer or premenopausal breast cancer, and non-Jewish women (eTable 1; http://links.lww.com/EDE/B2). No important interactions were observed for postmenopausal women, except for weight and BMI, HT use, and the combined “genetic” variable.
FIGURE 3.
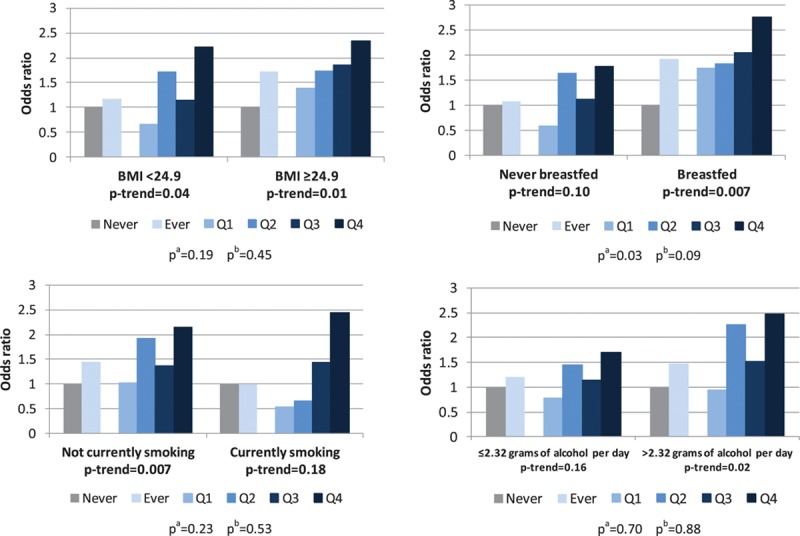
Variables modifying the talc association in premenopausal women. aP heterogeneity from likelihood ratio tests comparing a model with ever/never talc use and the effect modifier to a model with these plus the interaction term between them. bP heterogeneity from likelihood ratio tests comparing a model with indicators for each quartile of talc-years and the effect modifier to a model with these plus their interacton terms.
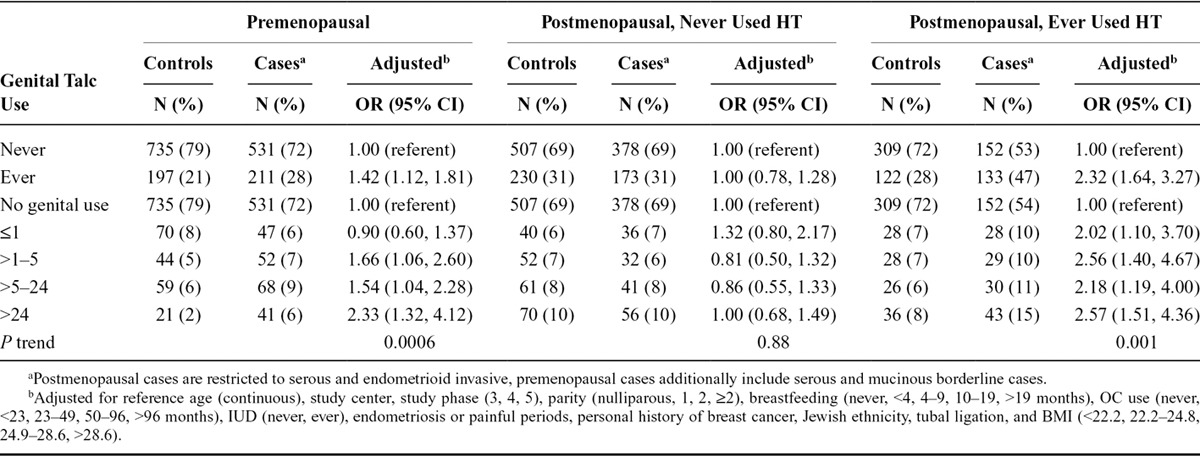
Table 4 shows ORs stratified by menopausal status and histologic subtype of epithelial ovarian cancer. Overall, talc use increased risk for serous and endometrioid invasive and serous borderline tumors with the dose–response most apparent for serous invasive cancer. For premenopausal women, both the overall associations and dose–responses were stronger with serous invasive and serous borderline tumors. Premenopausal women also had an increased risk for mucinous borderline tumors at the highest quartile of talc use OR = 2.28 (1.23, 4.26) and a dose–response. For postmenopausal women, dose–responses were strongest for women with invasive serous and endometrioid tumors. Talc use was not associated with clear cell or mucinous invasive epithelial ovarian cancer regardless of menopausal status. The ORs and dose–responses for the combined histologic subtypes relevant to pre- and post-menopausal women are shown in Table 5. Except for a few categories, these were not materially different than those illustrated in Figure 2. However, notably, premenopausal women and postmenopausal HT-users with the relevant subtypes who had accumulated >24 talc-years had ORs (95% CI) of 2.33 (1.32, 4.12) and 2.57 (1.51, 4.36), respectively.
TABLE 4.
Genital Talc Applications by Histologic Type and Menopausal Status
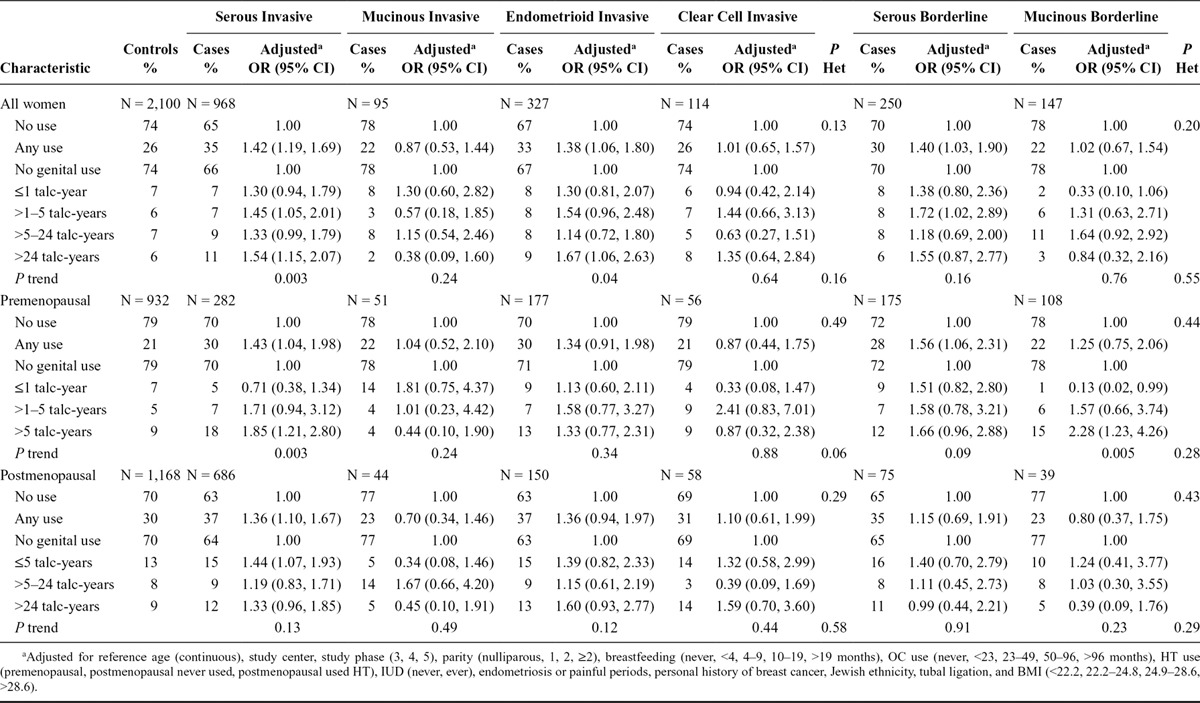
TABLE 5.
Associations Between Genital Talc Use (Never/Ever and Quartiles of Talc-years) and Ovarian Cancer by Menopausal Status and Postmenopausal Hormone Therapy Among Restricted Histologic Types
DISCUSSION
We analyzed case–control data collected over 16 years on talc use and epithelial ovarian cancer risk to address issues related to definition of the exposure, bias and confounding, effect modification, histologic heterogeneity, and dose–response. Talc used regularly in the genital area was associated with a 33% increase in ovarian cancer risk overall while no apparent risk was associated with talc used only in nongenital areas. Our results are consistent with a recent pooled analysis from the OCAC which reported that use of powder on genitals is associated with a 24% increased risk and no effect of nongenital use of talc.19 There was general agreement on risk by histologic type of epithelial ovarian cancer except that OCAC found an association with clear cell cancer and we did not. The findings from OCAC and our study contrast with null results from the WHI cohort analysis17 raising the issue of recall bias in case–control studies.
Addressing recall bias, we conducted a sensitivity analysis that assumed truly nonexposed cases and controls were accurately classified as unexposed (i.e., specificity 99%) and truly exposed cases were also correctly classified (sensitivity 99%). The OR of 1.33 in our study would be nullified if the sensitivity of correctly classified controls fell to 82% or 18% misclassification. Unfortunately, there are no external records to validate talc use reported by study participants to assess whether this degree of misclassification is reasonable. Somewhat analogous to talc and ovarian cancer is alcohol use and breast cancer. Nurses’ Health Study investigators examined the latter association both with prospective data collected at baseline and retrospective data obtained by resurveying subjects after diagnosis.25 They found an (age adjusted) OR for breast cancer of 1.42 associated with 30 or more grams of alcohol/day relative to nondrinkers from the prospective data compared with 1.33 from the retrospective data. This change between two analyses would occur if the sensitivity of controls correctly recalling alcohol use dropped to 91% (or 9% misclassification). This suggests some degree of misclassification in retrospective data but not as great as the 18% required to nullify the association between use of talc on genitals and ovarian cancer risk in our study. No comparable study on talc comparing results from prospective versus retrospective data has been performed. However, several observations are incompatible with the possibility that recall bias explains the association: (1) ORs are generally lower in studies which asked about “ever use” of talc5,8,11 compared with those that specified regular use,6,7,9,12,13 whereas higher ORs would be expected if cases are more likely to recall limited ever-use; (2) no association with nongenital talc use; (3) risk varies by histologic type; (4) the association is stronger in premenopausal women who are closer in time to talc use and less likely to have forgotten it; and (5) ORs from recent studies11,13 are lower than those from earlier ones,6,7 whereas increasing publicity about the association over time might lead to greater recall bias and higher ORs in more recent studies. Related arguments that cases initiate talc use because of treatment of ovarian cancer or early symptoms of disease also lack merit because we censored exposures 1 year before the date of diagnosis and most talc-users began the habit around age 20—a decade or more before the ovarian cancer diagnosis.
Whether the association is a result of confounding must also be addressed. A 1998 article identified BMI, smoking, and alcohol use as potential correlates of talc use in the general population.26 In our study, powder users were more likely to be older, from more urban/suburban areas, heavier, asthma sufferers, and regular analgesics users. However, none of these or other Table 2 variables altered the overall association by more than 10%, providing no indication of confounding. Talc use was also greater in African Americans and notably associated with a high, albeit imprecise, OR (and 95% CI) of 5.08 (1.32, 19.6). This finding clearly requires further study.
The observation that talc users, both case and control subjects, were more likely to say they had asthma has not been previously reported. The link between powder use and asthma may not be fully appreciated from Table 2 since women who used talc as a body powder but not to the genital area were classified as nonexposed. Making no body or genital exposure the nonexposed referent group and asthma the outcome, the ORs (and 95% CI) for asthma for body exposure to talc is 1.27 (0.80, 2.03) for cases and 1.02 (0.66, 1.57) for controls. The comparable OR for genital use of talc with or without body use is 1.48 (1.00, 2.18) for cases and 1.45 (1.00, 2.10) for controls. Sixty of 85 cases (70%) with asthma and 57 of 89 (64%) controls reported that talc use predated asthma onset. Although chance must be considered a possible explanation for this novel finding, talc is a cause of occupational asthma27 and respiratory distress has been reported in infants after talc was accidentally inhaled.28 That asthma may be associated with use of talc is important not only because of health consequences on its own but also because it may shed light on biologic mechanisms potentially relevant to the talc and ovarian cancer association.
Although we found no evidence of confounding, we did find several examples of effect modification of the association between talc and epithelial ovarian cancer. Overall, the association was greater in women with no personal history of breast cancer, those who had a tubal ligation or hysterectomy, in premenopausal women, and postmenopausal women who had used HT. Among these factors, perhaps the most important is effect modification of the association by menopausal status and menopausal HT.
Apparent lack of an elevated risk for epithelial ovarian cancer from talc use in postmenopausal women without HT use has not been reported previously. Explanations might include that there is no association with talc use in the absence of endogenous or exogenous estrogen, fading memory of past exposures, women who will develop ovarian cancer from talc use leave the at risk pool before they reach menopause, or more complex interactions with multiple risk factors and gene–environment interactions. Of possible relevance, Moorman et al.29 observed that reproductive events that clearly affect risk in premenopausal women may not affect risk to the same degree in postmenopausal women. Whatever the explanation, our observation challenges the relevance of the WHI study to the ovarian cancer/talc association since only postmenopausal women were enrolled in WHI and HT use was examined only as a confounder, not an effect modifier.16 Further study will be necessary to clarify the role that talc may play in postmenopausal women who did not use HT with a focus on those factors that may increase endogenous estrogen, such as greater BMI.
That the association is more apparent in premenopausal women and in postmenopausal women who used hormonal therapy suggests that estrogen plays a role in the association. In talc inhalation studies conducted by the National Toxicology Program, only female rats developed lung tumors.30 Literature on airway inflammation from particulates is also relevant. Citing evidence that asthma may be exacerbated during pregnancy, Zhang et al.31 postulated this may be due to an effect of estrogen on macrophage activity and inflammatory response to particulates normally considered inert, like titanium dioxide (TiO2). Their in-vivo studies demonstrated that macrophages from pregnant mice transplanted to nonpregnant recipients conferred an inflammatory phenotype in response to TiO2. Such studies should be repeated with talc, another particulate considered “inert.”
An exploratory analysis of other potential effect modifiers led to several other observations that may have biologic relevance. The overall associations and dose–responses were “stronger” for premenopausal women who had a greater BMI, had breastfed, were not current smokers, and consumed alcohol (Fig. 3). Due to the large number of associations tested, chance must be the first explanation considered. However, a common denominator could be prolactin since its levels are higher in women who have greater BMI,32 breastfed,33 do not currently smoke,34 consume alcohol,35 and are postmenopausal and use HT.36 Like estrogen, prolactin may have multiple effects on immune cells, especially monocytes and macrophages37 whose role in scavenging talc in tissue is described.38 These observations provide a framework for talc carcinogenicity in EOC involving chronic inflammation.9
Biologic credibility of the talc/EOC association is enhanced by persuasive evidence that inert particles the size of talc, present in the vagina, can migrate to the upper genital tract. In a technique called hysterosalpingoscintigraphy, technetium-labeled albumen microspheres are placed in the vagina and their migration to the upper tract was confirmed using serial scintograms.39 The microspheres are 5 to 40 μm in diameter—a range which includes the size of sperm and talc. Migration from the vagina is the obvious explanation for why talc can be found in diseased (and some normal) ovaries.3 Unfortunately, no epidemiologic study of epithelial ovarian cancer and talc has taken the opportunity to determine whether talc can actually be found in tissues removed at surgery and correlated with exposure to talc. A clue to talc’s presence is birefringent particles found when slides are examined under polarized-light microscopy. Although confirmation that the material is actually talc requires scanning electron microscopy and X-ray dispersion spectroscopy, presence of birefringence is a practical screening technique as illustrated by a case report of a woman with ovarian cancer and long-term talc use who had talc in her pelvic lymph nodes first suggested by birefringence.40
There are inherent limitations quantifying a dose–response due to a lack of metrics for how much talc is in an “application,” how much enters the vagina, and how much reaches the upper genital tract where, presumably, any deleterious effect is mediated. This may account for the failure to identify a dose–response in many papers on talc and ovarian cancer. Our 1999 study7 suggested that adjusting total applications by whether the genital tract was “open” (i.e., excluding use after a tubal ligation or hysterectomy and examining use during times when ovulation was occurring) yielded significant dose–responses. Mills et al.10 found a dose–response by frequency of use. Wu et al.,12 looking at all types of body use, found a dose–response with estimated applications. Merritt et al.11 reported a significant trend in risk for invasive serous ovarian cancer with years of talc use. The recent OCAC analysis reported no trend with increasing lifetime applications when restricted to talc users.19 However, an increase in risk with increasing applications was found for nonmucinous epithelial ovarian cancer when nonusers were included. Virtually all papers that have looked at dose–response for talc and epithelial ovarian cancer risk have included nonusers in the trend analysis. In our article, we calculated talc-years and showed that, overall, there is a significant trend for epithelial ovarian cancer risk and talc-years when nonusers are included, and the trend is even more apparent in premenopausal women with certain epithelial ovarian cancer subtypes.
In summary, this study on talc and epithelial ovarian cancer has contributed the following perspectives, some new, regarding this association:
(1) Overall, there is an association between genital talc use and EOC and a significant trend with increasing “talc-years” of use.
(2) Among many epidemiologic variables, no confounders for the association were identified.
(3) Talc users, both cases and controls, were more likely to report a medical history of asthma.
(4) The talc/epithelial ovarian cancer association was largely confined to premenopausal women and postmenopausal women who used HT. Other potential effect modifiers in premenopausal women included BMI, breastfeeding, current smoking, or alcohol use. These observations may suggest a role for estrogen and/or prolactin, both known to affect macrophage function and inflammatory response.
(5) Histologic subtypes of epithelial ovarian cancer more likely to be associated with talc include serous and mucinous borderline tumors and invasive serous and endometrioid tumors.
(6) For epithelial ovarian cancer categories based on certain effect modifiers or histologic subtypes, stronger overall associations and dose–responses were observed.
(7) The association may be stronger in African Americans.
An editorial17 accompanying the WHI study16 noted that “several case–control studies have reported associations between talc use and ovarian cancer risk” and “no epidemiologic studies have demonstrated a dose–response” (page 2). We believe these appraisals understate the epidemiologic evidence. There have been dozens of case–control studies and several have, in fact, found a dose–response. The editorial further notes that “it does not seem likely that additional conventional epidemiologic studies will strengthen the evidence for or against talc carcinogenicity” (page 2). We believe the observations made here present a good case for talc carcinogenicity and that reanalyses of existing data from already published studies might provide confirmatory evidence. To encourage consolidation of data, we have provided a copy of the “raw” and derived variables examined in our study to NCI dbGaP (available here: http://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs001034.v1.p1) as well as the SAS and Stata programs used in this analysis (eAppendix 1; http://links.lww.com/EDE/B2).
Supplementary Material
Footnotes
Supported by the National Institutes of Health (Grant Numbers R01CA054419, P50CA105009, R01CA67272), the Department of Defense Congressionally Directed Medical Research Programs (W81XWH-10-1-0280), and the Department of Obstetrics and Gynecology, Brigham and Women’s Hospital.
Dr. Cramer reports being paid for expert testimony in litigation related to ovarian cancer. Ms. Vitonis reports being paid for programming work related to the same litigation. The other authors have no conflicts to report.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
REFERENCES
- 1.Cralley LJ, Key MM, Groth DH, Lainhart WS, Ligo RM. Fibrous and mineral content of cosmetic talcum products. Am Ind Hyg Assoc J. 1968;29:350–354. doi: 10.1080/00028896809343015. [DOI] [PubMed] [Google Scholar]
- 2.Graham J, Graham R. Ovarian cancer and asbestos. Environ Res. 1967;1:115–128. doi: 10.1016/0013-9351(67)90008-4. [DOI] [PubMed] [Google Scholar]
- 3.Henderson WJ, Joslin CA, Turnbull AC, Griffiths K. Talc and carcinoma of the ovary and cervix. J Obstet Gynaecol Br Commonw. 1971;78:266–272. doi: 10.1111/j.1471-0528.1971.tb00267.x. [DOI] [PubMed] [Google Scholar]
- 4.Cramer DW, Welch WR, Scully RE, Wojciechowski CA. Ovarian cancer and talc: a case-control study. Cancer. 1982;50:372–376. doi: 10.1002/1097-0142(19820715)50:2<372::aid-cncr2820500235>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 5.Purdie D, Green A, Bain C, et al. Reproductive and other factors and risk of epithelial ovarian cancer: an Australian case-control study. Survey of Women’s Health Study Group. Int J Cancer. 1995;62:678–684. doi: 10.1002/ijc.2910620606. [DOI] [PubMed] [Google Scholar]
- 6.Chang S, Risch HA. Perineal talc exposure and risk of ovarian carcinoma. Cancer. 1997;79:2396–2401. doi: 10.1002/(sici)1097-0142(19970615)79:12<2396::aid-cncr15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 7.Cramer DW, Liberman RF, Titus-Ernstoff L, et al. Genital talc exposure and risk of ovarian cancer. Int J Cancer. 1999;81:351–356. doi: 10.1002/(sici)1097-0215(19990505)81:3<351::aid-ijc7>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 8.Wong C, Hempling RE, Piver MS, Natarajan N, Mettlin CJ. Perineal talc exposure and subsequent epithelial ovarian cancer: a case-control study. Obstet Gynecol. 1999;93:372–376. doi: 10.1016/s0029-7844(98)00439-6. [DOI] [PubMed] [Google Scholar]
- 9.Ness RB, Grisso JA, Cottreau C, et al. Factors related to inflammation of the ovarian epithelium and risk of ovarian cancer. Epidemiology. 2000;11:111–117. doi: 10.1097/00001648-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Mills PK, Riordan DG, Cress RD, Young HA. Perineal talc exposure and epithelial ovarian cancer risk in the Central Valley of California. Int J Cancer. 2004;112:458–464. doi: 10.1002/ijc.20434. [DOI] [PubMed] [Google Scholar]
- 11.Merritt MA, Green AC, Nagle CM, Webb PM Australian Cancer Study (Ovarian Cancer); Australian Ovarian Cancer Study Group. Talcum powder, chronic pelvic inflammation and NSAIDs in relation to risk of epithelial ovarian cancer. Int J Cancer. 2008;122:170–176. doi: 10.1002/ijc.23017. [DOI] [PubMed] [Google Scholar]
- 12.Wu AH, Pearce CL, Tseng CC, Templeman C, Pike MC. Markers of inflammation and risk of ovarian cancer in Los Angeles County. Int J Cancer. 2009;124:1409–1415. doi: 10.1002/ijc.24091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenblatt KA, Weiss NS, Cushing-Haugen KL, Wicklund KG, Rossing MA. Genital powder exposure and the risk of epithelial ovarian cancer. Cancer Causes Control. 2011;22:737–742. doi: 10.1007/s10552-011-9746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Langseth H, Hankinson SE, Siemiatycki J, Weiderpass E. Perineal use of talc and risk of ovarian cancer. J Epidemiol Community Health. 2008;62:358–360. doi: 10.1136/jech.2006.047894. [DOI] [PubMed] [Google Scholar]
- 15.Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Cogliano V WHO International Agency for Research on Cancer Monograph Working Group. Carcinogenicity of carbon black, titanium dioxide, and talc. Lancet Oncol. 2006;7:295–296. doi: 10.1016/s1470-2045(06)70651-9. [DOI] [PubMed] [Google Scholar]
- 16.Houghton SC, Reeves KW, Hankinson SE, et al. Perineal powder use and risk of ovarian cancer. J Natl Cancer Inst. 2014;106:1–6. doi: 10.1093/jnci/dju208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wentzensen N, Wacholder S. Talc use and ovarian cancer: epidemiology between a rock and a hard place. J Natl Cancer Inst. 2014;106:1–2. doi: 10.1093/jnci/dju260. [DOI] [PubMed] [Google Scholar]
- 18.Gates MA, Tworoger SS, Terry KL, et al. Talc use, variants of the GSTM1, GSTT1, and NAT2 genes, and risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2008;17:2436–2444. doi: 10.1158/1055-9965.EPI-08-0399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Terry KL, Karageorgi S, Shvetsov YB, et al. Australian Cancer Study (Ovarian Cancer); Australian Ovarian Cancer Study Group; Ovarian Cancer Association Consortium. Genital powder use and risk of ovarian cancer: a pooled analysis of 8,525 cases and 9,859 controls. Cancer Prev Res (Phila) 2013;6:811–821. doi: 10.1158/1940-6207.CAPR-13-0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vitonis AF, Titus-Ernstoff L, Cramer DW. Assessing ovarian cancer risk when considering elective oophorectomy at the time of hysterectomy. Obstet Gynecol. 2011;117:1042–1050. doi: 10.1097/AOG.0b013e318212fcb7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCluggage WG. My approach to and thoughts on the typing of ovarian carcinomas. J Clin Pathol. 2008;61:152–163. doi: 10.1136/jcp.2007.049478. [DOI] [PubMed] [Google Scholar]
- 22.Willett WC, Reynolds RD, Cottrell-Hoehner S, Sampson L, Browne ML. Validation of a semi-quantitative food frequency questionnaire: comparison with a 1-year diet record. J Am Diet Assoc. 1987;87:43–47. [PubMed] [Google Scholar]
- 23.Glynn RJ, Rosner B. Multiple imputation to estimate the association between eyes in disease progression with interval-censored data. Stat Med. 2004;23:3307–3318. doi: 10.1002/sim.1770. [DOI] [PubMed] [Google Scholar]
- 24.Lash TL, Fox MP, Fink AK. Applying Quantitative Bias Analysis to Epidemiologic Data. New York, NY: Springer; 2009. [Google Scholar]
- 25.Giovannucci E, Stampfer MJ, Colditz GA, et al. Recall and selection bias in reporting past alcohol consumption among breast cancer cases. Cancer Causes Control. 1993;4:441–448. doi: 10.1007/BF00050863. [DOI] [PubMed] [Google Scholar]
- 26.Rosenblatt KA, Mathews WA, Daling JR, Voigt LF, Malone K. Characteristics of women who use perineal powders. Obstet Gynecol. 1998;92:753–756. doi: 10.1016/s0029-7844(98)00252-x. [DOI] [PubMed] [Google Scholar]
- 27.Chan-Yeung M. Occupational asthma. Clin Rev Allergy. 1986;4:251–266. doi: 10.1007/BF02993160. [DOI] [PubMed] [Google Scholar]
- 28.Gould SR, Barnardo DE. Respiratory distress after talc inhalation. Br J Dis Chest. 1972;66:230–233. doi: 10.1016/s0007-0971(72)80021-4. [DOI] [PubMed] [Google Scholar]
- 29.Moorman PG, Calingaert B, Palmieri RT, et al. Hormonal risk factors for ovarian cancer in premenopausal and postmenopausal women. Am J Epidemiol. 2008;167:1059–1069. doi: 10.1093/aje/kwn006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Toxicology P. NTP toxicology and carcinogenesis studies of talc (CAS No. 14807-96-6)(Non-Asbestiform) in F344/N rats and B6C3F1 mice (inhalation studies). Natl Toxicol Program Tech Rep Ser. 1993;421:1–287. [PubMed] [Google Scholar]
- 31.Zhang Y, Mikhaylova L, Kobzik L, Fedulov AV. Estrogen-mediated impairment of macrophageal uptake of environmental TiO2 particles to explain inflammatory effect of TiO2 on airways during pregnancy. J Immunotoxicol. 2015;12:81–91. doi: 10.3109/1547691X.2014.899411. [DOI] [PubMed] [Google Scholar]
- 32.Roelfsema F, Pijl H, Keenan DM, Veldhuis JD. Prolactin secretion in healthy adults is determined by gender, age and body mass index. PLoS One. 2012;7:e31305. doi: 10.1371/journal.pone.0031305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Delvoye P, Demaegd M, Uwayitu-Nyampeta, Robyn C. Serum prolactin, gonadotropins, and estradiol in menstruating and amenorrheic mothers during two years’ lactation. Am J Obstet Gynecol. 1978;130:635–639. doi: 10.1016/0002-9378(78)90319-8. [DOI] [PubMed] [Google Scholar]
- 34.Berta L, Fortunati N, Gennari P, Appendino M, Casella A, Frairia R. Influence of cigarette smoking on pituitary and sex hormone balance in healthy premenopausal women. Fertil Steril. 1991;56:788–789. doi: 10.1016/s0015-0282(16)54620-2. [DOI] [PubMed] [Google Scholar]
- 35.Sarkola T, Mäkisalo H, Fukunaga T, Eriksson CJ. Acute effect of alcohol on estradiol, estrone, progesterone, prolactin, cortisol, and luteinizing hormone in premenopausal women. Alcohol Clin Exp Res. 1999;23:976–982. [PubMed] [Google Scholar]
- 36.Kalleinen N, Polo-Kantola P, Irjala K, et al. 24-hour serum levels of growth hormone, prolactin, and cortisol in pre- and postmenopausal women: the effect of combined estrogen and progestin treatment. J Clin Endocrinol Metab. 2008;93:1655–1661. doi: 10.1210/jc.2007-2677. [DOI] [PubMed] [Google Scholar]
- 37.Malaguarnera L, Imbesi R, Di Rosa M, et al. Action of prolactin, IFN-gamma, TNF-alpha and LPS on heme oxygenase-1 expression and VEGF release in human monocytes/macrophages. Int Immunopharmacol. 2005;5:1458–1469. doi: 10.1016/j.intimp.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 38.Goldner RD, Adams DO. The structure of mononuclear phagocytes differentiating in vivo. III. The effect of particulate foreign substances. Am J Pathol. 1977;89:335–350. [PMC free article] [PubMed] [Google Scholar]
- 39.Kunz G, Beil D, Deininger H, Wildt L, Leyendecker G. The dynamics of rapid sperm transport through the female genital tract: evidence from vaginal sonography of uterine peristalsis and hysterosalpingoscintigraphy. Hum Reprod. 1996;11:627–632. doi: 10.1093/humrep/11.3.627. [DOI] [PubMed] [Google Scholar]
- 40.Cramer DW, Welch WR, Berkowitz RS, Godleski JJ. Presence of talc in pelvic lymph nodes of a woman with ovarian cancer and long-term genital exposure to cosmetic talc. Obstet Gynecol. 2007;110(2 Pt 2):498–501. doi: 10.1097/01.AOG.0000262902.80861.a0. [DOI] [PubMed] [Google Scholar]


