Abstract
Aim:
We have shown that low-dose gadolinium chloride (GdCl3) abolishes arachidonic acid (AA)-induced increase of cytoplasmic Ca2+, which is known to play a crucial role in myocardial ischemia/reperfusion (I/R) injury. The present study sought to determine whether low-dose GdCl3 pretreatment protected rat myocardium against I/R injury in vitro and in vivo.
Methods:
Cultured neonatal rat ventricular myocytes (NRVMs) were treated with GdCl3 or nifedipine, followed by exposure to anoxia/reoxygenation (A/R). Cell apoptosis was detected; the levels of related signaling molecules were assessed. SD rats were intravenously injected with GdCl3 or nifedipine. Thirty min after the administration the rats were subjected to LAD coronary artery ligation followed by reperfusion. Infarction size, the release of serum myocardial injury markers and AA were measured; cell apoptosis and related molecules were assessed.
Results:
In A/R-treated NRVMs, pretreatment with GdCl3 (2.5, 5, 10 μmol/L) dose-dependently inhibited caspase-3 activation, death receptor-related molecules DR5/Fas/FADD/caspase-8 expression, cytochrome c release, AA release and sustained cytoplasmic Ca2+ increases induced by exogenous AA. In I/R-treated rats, pre-administration of GdCl3 (10 mg/kg) significantly reduced the infarct size, and the serum levels of CK-MB, cardiac troponin-I, LDH and AA. Pre-administration of GdCl3 also significantly decreased the number of apoptotic cells, caspase-3 activity, death receptor-related molecules (DR5/Fas/FADD) expression and cytochrome c release in heart tissues. The positive control drug nifedipine produced comparable cardioprotective effects in vitro and in vivo.
Conclusion:
Pretreatment with low-dose GdCl3 significantly attenuates I/R-induced myocardial apoptosis in rats by suppressing activation of both death receptor and mitochondria-mediated pathways.
Keywords: myocardium, ischemia/reperfusion, apoptosis, gadolinium chloride, nifedipine, arachidonic acid, death receptor, mitochondria, cardioprotection
Introduction
Myocardial infarction (MI) is a leading cause of death and a major health problem worldwide. The current most effective therapy after acute MI is the restoration of blood flow through the occluded coronary artery to limit infarct size and preserve cardiac function. However, this treatment causes additional injury during ischemia/reperfusion (I/R), which is a major risk factor for MI-induced arrhythmia, contractile dysfunction, and heart failure1,2,3. Mitochondrial oxidative phosphorylation returns to pre-ischemic levels within seconds of reperfusion, but contractile power lags behind, which is termed 'myocardial stunning'4. Stunned myocardium exhibits excess oxygen consumption for a given rate of contractile work, and it has reduced mechanical efficiency5. Abundant evidence has suggested that myocardial I/R is a main cause of apoptotic and necrotic cell death because of oxidative stress, inflammation, Ca2+ overload, and ATP depletion6,7,8,9. Several observations in human hearts have indicated that apoptotic cardiomyocytes contribute dramatically to overall cell loss during MI10,11. Notably, cardiomyocyte apoptosis contributes to left ventricle dysfunction following cardiac surgery12. Previous studies have demonstrated that mitochondrial-related pathways and death receptor-mediated pathways are involved in I/R-induced cardiomyocyte apoptosis13,14,15. Therefore, the exploration of the mechanisms of myocardial I/R-induced apoptosis and the identification of the potential target(s) to prevent or reverse cell apoptosis are important for the prevention and treatment of myocardial I/R and following cardiac surgery.
Several studies have suggested that a large concentration of arachidonic acid (AA) is released from cell membrane phospholipids under pathological conditions, such as stress, ischemia, hypoxia, and I/R, thus leading to multiple deleterious consequences, including abnormal excitation-contraction coupling due to alterations in ion channel kinetics, bioenergetic inefficiency, apoptosis, and accelerated necrosis, which collectively promote the development of heart dysfunction, heart failure, and sudden death16,17. Accumulating evidence has indicated that AA-induced cell apoptosis partially occurs through mitochondria-mediated pathways via an increase in mitochondrial membrane permeability, the release of cytochrome c, and caspase-3 activation, which induces apoptosis and cell death17. Our previous data have suggested that low-dose gadolinium chloride (GdCl3) is protective against AA-induced Ca2+ overload18,19 and cardiomyocyte apoptosis in primary cultured neonatal rat ventricular myocytes (NRVMs) via AA scavenging20. Therefore, whether GdCl3 can effectively prevent I/R-mediated cell apoptosis and myocardial injury in vivo and the potential involvement of AA as a candidate for the underlying mechanism (s) were investigated.
Previous studies have suggested that the effect of GdCl3 is dose dependent because high doses of GdCl3 (≥300 μmol/L) activate the calcium-sensing receptor, which may induce apoptosis in cardiomyocytes21. However, GdCl3 (≤10 μmol/L) completely blocks AA-mediated Ca2+ increase in HEK293 cells19,20. GdCl3 (10 mg/kg) has been demonstrated to exert a protective potential in I/R-induced brain injury and hepatic injury and to protect the myocardium against I/R-induced inflammation via the reduction of circulating monocytes and neutrophils and the infiltration of leukocytes. This dose also attenuated myocardial stunning when administered prior to the onset of ischemia or during ischemia, but it did not enhance the contractile function of normal myocardium21,22,23,24. However, the precise mechanism(s) underlying the effect of GdCl3 are not known. The present study used low-dose GdCl3 (10 mg/kg, iv), which is safe and effective in the treatment of hepatic I/R in rats25, to detect the protective effect and the mechanism against myocardial I/R-induced cell apoptosis and myocardial infarction in rats and cultured ventricular cardiomyocytes.
Materials and methods
Materials and reagents
GdCl3 and nifedipine were purchased from Sigma-Aldrich (St Louis, MO, USA). Fluo-4/AM was obtained from Molecular Probes (Invitrogen Inc, CA, USA). Antibodies for Fas, DR5, FADD, cytochrome c, casepase-8 and GAPDH were purchased from Santa Cruz Biotechnology, Inc (CA, USA). Cox IV was purchased from Cell Signaling Technology (CST, MA, USA).
Ethics statement
The Capital Medical University Animal Care and Use Committee approved this study, and all studies were conducted in accordance with the 'Guide for the Care and Use of Laboratory Animals' adopted by the Beijing government and 'Guide for the Care and Use of Laboratory Animals' published by the US National Institutes of Health (publication No 85-23, revised 1996).
Isolation and culture of neonatal rat ventricular myocytes (NRVMs)
NRVMs were isolated from 2-day-old Sprague-Dawley rats by enzymatic digestion with 0.05% trypsin and 0.015% collagenase, as described previously26. Cardiac fibroblasts were removed, and NRVMs were plated onto 35-mm dishes at a density of 1×106 cells/mL in Dulbecco's modified Eagle's medium containing 10% fetal bovine serum (FBS, Hyclone, Australian), 100 units/mL penicillin/streptomycin, and 0.1 mmol/L 5-bromo-2-deoxyuridine to inhibit fibroblast proliferation.
Anoxia and reoxygenation model
NRVMs were cultured for 12 h (FBS free) and exposed to A/R, as described previously27. Briefly, cardiomyocytes were exposed to anoxia by the addition of fresh anoxia medium (in mmol/L: NaCl 98.5, KCl 10, MgSO4 1.2, CaCl2 1.0, HEPES 20, sodium lactate 40, pH 6.8) with GdCl3 dissolved in water (2.5, 5, or 10 μmol/L) or nifedipine (1 μmol/L) and incubated in an anoxic chamber with an atmosphere of 95% N2 and 5% CO2 for 12 h. Cells were returned to reoxygenation medium (composition in mmol/L: NaH2PO4 0.9, NaHCO3 20.0, CaCl2 1.0, MgSO4 1.2, HEPES 20.0, NaCl 129.5, KCl 5.0, glucose 5.5, pH 7.4) and incubated in an incubator with an atmosphere of 95% O2 and 5% CO2 for 12 h. Cells in control normoxia experiments were incubated in fresh culture growth medium in an incubator with 95% O2 and 5% CO2 for 24 h (Supplementary Figure S1A).
Confocal Ca2+ transients
Myocytes were loaded with Fluo-4/AM and measurements of intracellular Ca2+ concentration ([Ca2+]i) were performed as previously described27. Experiments were performed at room temperature (22–24°C). All NRVMs at 70%-80% confluence were used after 48 h in culture. Cardiomyocytes were loaded with 4 μmol/L Fluo-4/AM for 30 min at 37°C followed by three washes with HEPES-buffered physiological saline solution (HBSS) (mmol/L: NaCl 135, KCl 5, MgCl2 1, CaCl2 1.8, HEPES 10, glucose 11, pH 7.4) to remove extracellular Fluo-4/AM for 20 min. These cells were visualized with a laser confocal microscope (Leica SP5) equipped with a 40× oil immersion objective (NA 1.35). The fluorescence of interested regions, which generally contained approximately 30 cells, was recorded at an excitation of 488 nm and emission detection at 515 nm. Cardiomyocytes for the AA stimulation protocol were pretreated with vehicle, GdCl3 (5 μmol/L) or nifedipine (1 μmol/L) for 2 min, which were then followed by AA (10 μmol/L) treatment for 2 min. Fluo-4 loaded cardiomyocytes for the A/R cells were recorded for 100 s and stimulated with 50 μmol/L phenylephrine (PE) to detect cellular responses to agonist27. Changes in the fluorescence intensity over time were collected using series image scanning, and the [Ca2+]i was expressed as F/F0, where F0 stands for the mean basal fluorescence obtained from 4 images with cell at resting state. The relative basal [Ca2+]i in A/R cells were calculated as F0(A/R) normalized with the F0(con) in normal cells from the same experiment.
Ischemia and reperfusion model
Sprague-Dawley rats (males, 10 weeks old) were obtained from the experimental animal center of Capital Medical University (Beijing, China). Myocardial ischemia and reperfusion was conducted as previously described28. Briefly, rats were anesthetized with urethane (5 mg/kg, ip). Rats were incubated, and mechanical ventilation was achieved by connecting the endotracheal tube to the ventilator. The left chest was opened to expose the heart. An 8-0 silk suture was passed underneath the left anterior descending (LAD) coronary artery, and a slipknot was tied. Sham-operated rats underwent the same surgical procedures except that the suture was placed beneath the LAD without ligation. I/R was induced by 30 min of ischemia followed by 2 h of reperfusion. Significant elevations of ST segment were detected using electrocardiography. Rats were treated with GdCl3 (10 mg/kg) via tail vein injection 30 min before LAD ischemia (Supplementary Figure 1B). Experimental groups included sham (no treatment, no ischemia), I/R (no treatment but subject to ischemia and reperfusion), GdCl3 (treated and subject to I/R) and nifedipine 10 mg/kg (treated and subject to ischemia and reperfusion).
Assessment of the area at risk and infarct size
The LAD was immediately religated at the end of the 2-h reperfusion, and 2 mL of 2% Evans blue dye (Sigma, USA) was injected into the left ventricular cavity. The heart was quickly removed, frozen at -20°C, and sliced horizontally to yield five slices. Slices were incubated in 1% triphenyl tetrazolium chloride (TTC) (Amresco, USA) prepared with phosphate buffer (pH=7.8) for 15 min at 37°C and photographed using a digital camera. The areas stained with Evans blue (blue staining, area not at risk) and TTC (red staining, ischemic but viable myocardium), the TTC-negative area (white area, infarct size) and the LV area were measured digitally using Image J.
Assessment of apoptosis
Apoptotic death of cultured cardiomyocytes was detected by a caspase-3 activity ELISA kit (Applygen, Beijing, China) and an FITC annexin V apoptosis detection kit (BD Pharmingen, USA) for flow cytometry. Myocardial apoptosis in hearts was detected by the terminal deoxyribonucleotide transferase-mediated dUTP nick end labeling (TUNEL) detection kit (Roche, Switzerland) and caspase-3 activity ELISA kit (Applygen, Beijing, China) according to the manufacturers' protocols.
Enzyme-linked immunosorbent assay (ELISA)
Blood was collected from the heart immediately after 2 h of reperfusion. Creatine kinase MB (CK-MB), cardiac troponin I (cTn-I), lactate dehydrogenase (LDH) and AA assay kits (CUSABIO, Shanghai, China) were used to detect the activities of these myocardial markers. Heart tissues were rinsed in ice-cold PBS to remove excess blood and minced into small pieces. Tissues (100 mg) were homogenized in 1000 mL ice-cold lysis buffer and centrifuged for 10 min at 12 000×g at 4°C. Supernatants were assayed immediately with a caspase-3 activity ELISA kit (Applygen, Beijing, China), caspase-8 activity ELISA kit (Applygen, Beijing, China), and Fas ELISA kit (CUSABIO, Shanghai, China). All procedures were performed according to the manufacturers' protocols.
Histological examination
Hearts were fixed in 10% formalin, embedded in paraffin, and cut into 6-μm sections. Sections were stained using hematoxylin and eosin (HE) for histochemical examination. An observer who was blinded to the experimental conditions of animals recorded the data. Two investigators evaluated all histopathological changes in a blinded fashion, and the main observation indexes, including intercellular space, heart tissue edema, and inflammatory cell infiltration, were assessed under a microscope.
Subcellular cytoplasmic and mitochondrial fractionation
Subcellular cytoplasmic and mitochondrial fractionations were obtained as previously described29. Isolation of mitochondrial and cytosolic proteins was performed using a mitochondria/cytosol fractionation kit (Beyotime Inst Biotech, Peking, China). Briefly, cells or tissue were collected and washed in PBS followed by the addition of mitochondrial isolation buffer. Lysates were centrifuged at 3500×g for 10 min at 4°C. The resulting pellets were used as the mitochondrial fraction. Supernatants were centrifuged further at 11000×g for 10 min at 4°C and used for the analysis of the cytosolic fraction.
Western blots
Samples were homogenized in RIPA lysis buffer and centrifuged at 15 000 r/min for 15 min at 4 °C. Protein concentrations were measured using a bicinchoninic acid (BCA) protein assay kit (Thermo, Rockford, IL, USA). Equal amounts of protein lysates were separated using 12% or 15% sodium dodecyl sulfate-polyacrylamide (SDS-PAGE) gel electrophoresis. Gels were blotted onto nitrocellulose membranes and incubated with the indicated antibodies. Blots were developed using ECL according to the manufacturer's instructions.
Statistical analysis
All data are presented as the mean±SD. Statistical analysis was performed using one-way ANOVA and Student's t-test, as appropriate. A value of P<0.05 was considered statistically significant.
Results
GdCl3 inhibited A/R-induced cardiomyocyte apoptosis in vitro
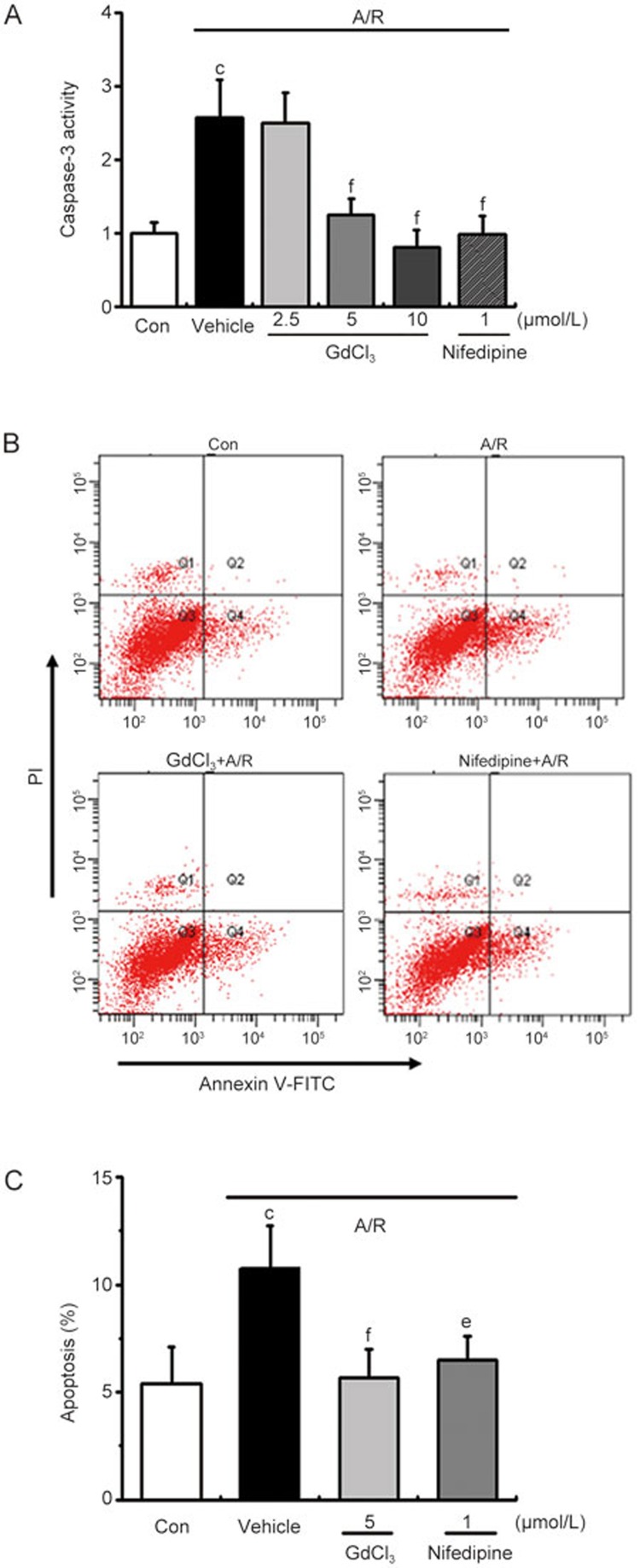
We investigated whether GdCl3 inhibited caspase-3 activity, which is a final common pathway in caspase-dependent apoptosis, to characterize the inhibitory effect of GdCl3 in myocardial cell apoptosis. The effects of GdCl3 were compared with the effect of the Ca2+ channel blocker nifedipine, which reduces intracellular Ca2+ overload in cardiomyocytes and dilates coronary arteries for the treatment of variant angina. Cells were treated with different concentrations of GdCl3 (2.5–10 μmol/L) and subjected to apoptosis analysis on the basis of caspase-3 activity and annexin-V-FITC/PI staining. We found that caspase-3 activity was triggered by A/R and inhibited by GdCl3 treatment in a dose-dependent manner (Figure 1A). GdCl3 at the concentration of 2.5 μmol/L did not affect caspase-3 activity, but 5 and 10 μmol/L exerted significant changes compared to the A/R group. The 5 μmol/L concentration was selected for the following experiments. Flow cytometric analysis of myocardial cells also demonstrated that A/R induced early stage cell apoptosis, and GdCl3 significantly decreased the extent of cardiomyocyte apoptosis with a similar potency as nifedipine (Figure 1B, 1C). These results indicated that GdCl3 inhibited A/R-induced apoptosis in NRVMs.
Figure 1.
GdCl3 attenuated A/R-induced cell apoptosis in NRVMs. (A) Vehicle or GdCl3 (2.5, 5, and 10 μmol/L) was incubated with A/R-treated cardiomyocytes as indicated for 24 h, and cell apoptosis was assessed on the basis of caspase-3 activity; (B) Apoptosis was also determined on the basis of annexin V-FITC/PI staining; (Q1: Necrotic cells; Q2: Early apoptotic cells; Q3: Viable cells; Q4: Late apoptotic cells). (C) Statistical analysis of flow cytometric data. All values are presented as the mean±SD. n=3. cP<0.01 vs control. eP<0.05, fP<0.01 vs A/R.
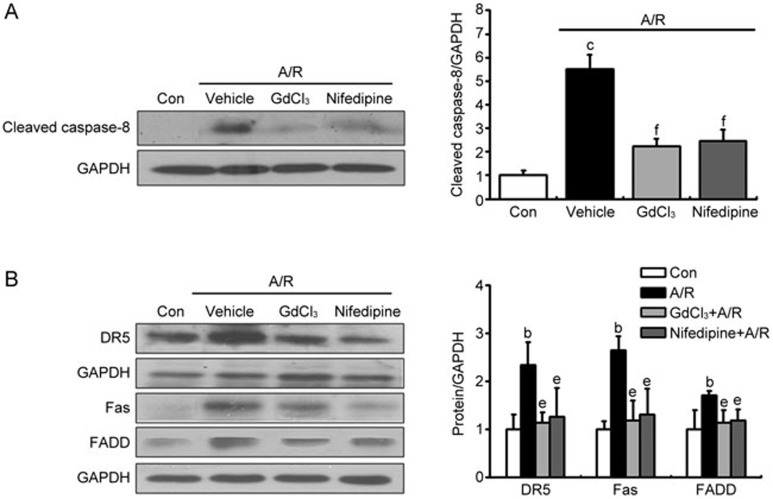
GdCl3 inhibited A/R-induced cardiomyocyte apoptosis via death receptor and mitochondrial signaling pathways
The expression levels of cleaved caspase-8, DR5, Fas, FADD and cytochrome c were evaluated by Western blotting to identify the molecular mechanisms underlying the protective effect of GdCl3 treatment against apoptosis. A/R treatment potently promoted the expression of these proteins compared to the control group, and GdCl3 (5 μmol/L) reversed all these activations (Figure 2). These results suggest that GdCl3 prevents cell apoptosis likely via the inhibition of the A/R-induced death receptor signaling pathway.
Figure 2.
GdCl3 5 μmol/L and nifedipine 1 μmol/L inhibited A/R-induced cardiomyocytes apoptosis via the inhibition of the death receptor-related signaling pathway. (A) Representative images of Western blots and quantitative analyses of cleaved caspase-8; (B) Representative images of Western blots and quantitative analyses of DR5, Fas, and FADD. Mean±SD. n=3. bP<0.05, cP<0.01 vs control. eP<0.05, fP<0.01 vs A/R.
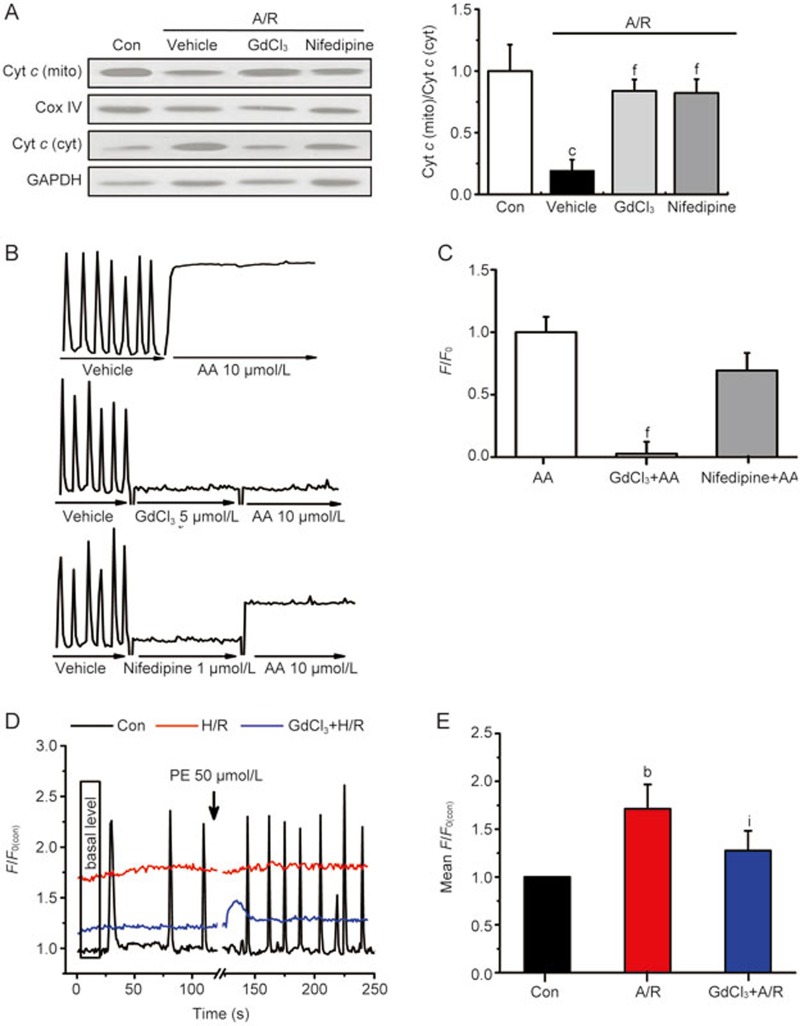
We also evaluated the level of cytochrome c in mitochondrial fractions/cytosol fractions and found that cytochrome c was normally localized in the mitochondria, as shown in the control group. However, the ratio of mitochondria cytochrome c to cytosol cytochrome c was reduced in A/R-injured NRVMs compared to the control group. Notably, treatment with GdCl3 significantly increased the ratio of mitochondria cytochrome c to cytosol cytochrome c compared to the A/R group (Figure 3A). These results indicated that GdCl3 reversed A/R-induced cell apoptosis via inhibition of the mitochondrial-related signaling pathway.
Figure 3.
GdCl3 inhibited A/R-induced cardiomyocyte apoptosis via inhibition of the mitochondria-related signaling pathway. (A) Representative images of Western blots and quantitative analyses of cytochrome c in mitochondrial/cytosol fractions; (B) Typical traces represent the spontaneous Ca2+ transients in NRVMs before and after AA (10 μmol/L) treatment for 2 min in the presence or absence of GdCl3 (5 μmol/L) or nifedipine (1 μmol/L) for 2 min as indicated. (C) GdCl3 (5 μmol/L) inhibited AA-induced increase in [Ca2+]i in NRVMs. (D) Representative traces illustrate global Ca2+ transients before and after 50 μmol/L PE treatment in normal cells (Con) and the disability of spontaneous pacing in NRVMs with A/R or GdCl3+A/R treatment. (E) Basal [Ca2+]i levels, the mean fluorescence from 4 images at the beginning of recording normalized by the control F0, were significantly enhanced as a result of A/R, which was partially prevented by 5 μmol/L GdCl3. All values are presented as the mean±SD. n=3 for each bar in A. n=4–6 for each bar in B–E. bP<0.05, cP<0.01 vs control (A, E). fP<0.01 vs AA (C). iP<0.01 vs A/R.
Accumulating evidence has indicated that AA is involved in cell apoptosis via the induction of Ca2+ overload, increase in mitochondrial membrane permeability, release of cytochrome c and activation of caspase-3, which eventually leads to cell apoptosis and death16,17. We monitored Ca2+ signals in NRVMs in response to AA to investigate the effect of GdCl3 on AA-induced Ca2+ overload and found that AA caused a marked increase in [Ca2+]i. GdCl3 pretreatment significantly inhibited the AA-induced increase in [Ca2+]i, but nifedipine did not exhibit this effect (Figure 3B and C). These results suggest that the AA-induced the Ca2+ signal is independent of potential-dependent Ca2+ channels. We also assessed internal Ca2+ activities in NRVMs treated with A/R or GdCl3 plus the A/R procedure and compared the results with NRVMs cultured in normal O2 as a control. Figure 3D and 3E shows that spontaneous oscillations were observed only in normal cells, and PE treatment significantly potentiated these oscillations, as reported previously26. In contrast, A/R cells lost their spontaneous oscillations and response to PE. Basal Ca2+ levels were also different between groups. A/R NRVMs exhibited much higher resting [Ca2+]i than normal cells. These abnormal changes in Ca2+ signaling reflect damaged cellular function because of A/R. GdCl3 treatment partially prevented these cells from A/R injury via lowering basal Ca2+ levels and responding to PE, but the spontaneous Ca2+ transients also disappeared in GdCl3+A/R cells (Figure 3D) and GdCl3-treated normal cells (data not shown). These data suggest that GdCl3 reversed A/R-induced cell apoptosis partially through its inhibition of exaggerated Ca2+ activities.
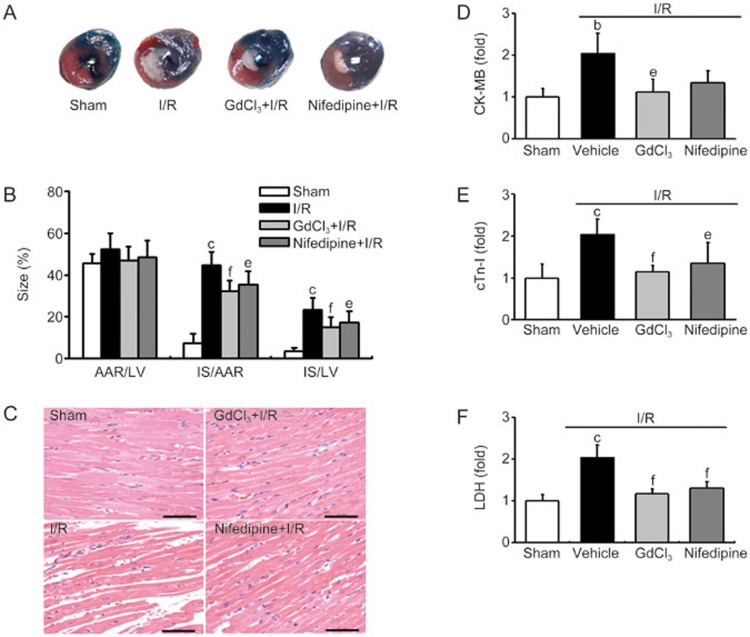
GdCl3 protected against myocardial I/R injury in rats
The induction and evaluations in cardiac I/R injury of rats were performed as described in the Methods (supplementary Figure 1), and nifedipine was used as the positive control drug. Figure 4A and B shows that the infarct areas were smaller in GdCl3 and nifedipine groups compared to the I/R group (15.0%±4.6% and 17.1%±5.5% in GdCl3 and nifedipine, respectively, versus 23.2%±5.8% in I/R), but the area-at-risk (AAR) area between these three groups were similar. HE staining in the sham group revealed the normal architecture of the myocardium with cardiomyocytes of normal size, clear boundaries and regular arrangement. However, cardiomyocytes in the I/R group were arranged irregularly, and intercellular spaces were enlarged, which indicates serious damage. However, GdCl3 and nifedipine pretreatment significantly alleviated the I/R-induced injury of the myocardium (Figure 4C). The release of CK-MB, cTn-I and LDH, which are markers of cardiomyocyte I/R injury, were higher in the I/R group than the sham group, and GdCl3 or nifedipine pretreatment significantly reduced the release of these factors as compared with the I/R group (Figure 4D–F). These results demonstrated that GdCl3 effectively protected the heart against I/R injury.
Figure 4.
GdCl3 reduced I/R-induced myocardial injury in a rat model. (A) The panel shows representative photomicrographs of LV sections from different groups after 30-min occlusion of the left anterior descending artery followed by 2 h of reperfusion. Blue-stained portion: non-ischemic normal region; red-stained portion: ischemic/reperfused but not infarcted region; unstained portion (white area): ischemic/reperfused, infarcted region; (B) Analysis of the percentage of myocardial infarct size in each group. Area-at-risk (AAR), infarct size (IS), left ventricle (LV); (C) Representative photomicrographs of H&E staining in myocardial tissues from sham-operated rats or rats with different pretreatments before I/R, bar = 50 μm; (D) Levels of CK-MB in rat sera; (E) Levels of cTn-I in rat sera; (F) LDH levels in rat sera. All values are presented as the mean±SD. n=8. bP<0.05, cP<0.01 vs sham. eP<0.05, fP<0.01 vs I/R.
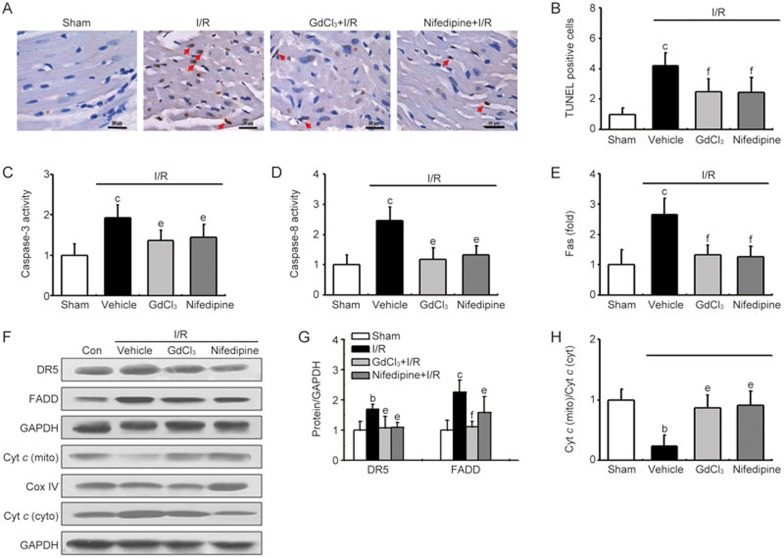
GdCl3 inhibited I/R-induced myocardial myocyte apoptosis in rats
Substantial evidence has suggested that apoptosis plays a critical role in I/R injury30,31. Therefore, the effect of GdCl3 on I/R-induced cardiomyocytes apoptosis in vivo was examined. A significant increase in the number of TUNEL-positive cells was detected in cardiac tissues in the I/R group after 2 h of reperfusion compared with that of the sham group. GdCl3 treatment exerted a remarkable anti-apoptotic effect, which was evidenced by reduced TUNEL-positive staining (Figure 5A and B). Similarly, I/R increased caspase-3 activity, and GdCl3 treatment significantly reduced caspase-3 activity compared with that in the I/R group (Figure 5C). These results provide direct evidence for GdCl3-mediated alleviation of I/R-induced cell apoptosis in vivo.
Figure 5.
GdCl3 attenuated I/R-induced myocardial apoptosis in vivo. (A) Representative photomicrographs of TUNEL staining in myocardial tissues from sham-operated rats or rats with different pretreatments before I/R as indicated. Scale bar=30 μm; arrows in each panel indicate cells positive for apoptosis; (B) Bar graph shows the percentages of TUNEL-positive nuclei in the sham, I/R and drug-treated groups; (C) Cardiomyocyte apoptosis was assessed on the basis of caspase-3 activity; (D) Cardiomyocyte apoptosis was assessed on the basis of caspase-8 activity; (E) Cardiomyocyte apoptosis was assessed on the basis of Fas levels; (F–H) Representative images of Western blots and quantitative analyses of apoptosis-related signaling molecules (DR5, FADD, and cytochrome c). All values are presented as the means±SD. n=6–8. bP<0.05, cP<0.01 vs sham. eP<0.05, fP<0.01 vs I/R.
GdCl3 alleviated I/R-induced cardiomyocyte apoptosis via the death receptor and mitochondrial signaling pathways
The activity of caspase-3 and caspase-8, the levels of Fas and the expression levels of DR5, FADD and cytochrome c were evaluated using ELISA and Western blotting to examine the molecular mechanisms underlying the protective effect of GdCl3 against I/R-induced apoptosis. Rats subjected to I/R injury exhibited significantly increased caspase-8 activity and Fas levels (Figure 5D and E). Rats in the GdCl3- or nifedipine-treated groups exhibited decreased caspase-8 activity and Fas levels (Figure 5D and E) compared to the I/R group. We evaluated the expression levels of DR5 and FADD in total tissues and cytochrome c in the mitochondrial fraction. I/R treatment potently promoted the expression of DR5 and FADD in whole cells and reduced cytochrome c in mitochondria, and GdCl3 reversed the effect of I/R-induced upregulation of these apoptosis-related signaling proteins (Figure 5F–H). GdCl3 inhibited cell apoptosis via death receptor-related and mitochondrial-related signaling pathways, a result consistent with the in vitro data (Figures 2 and 3).
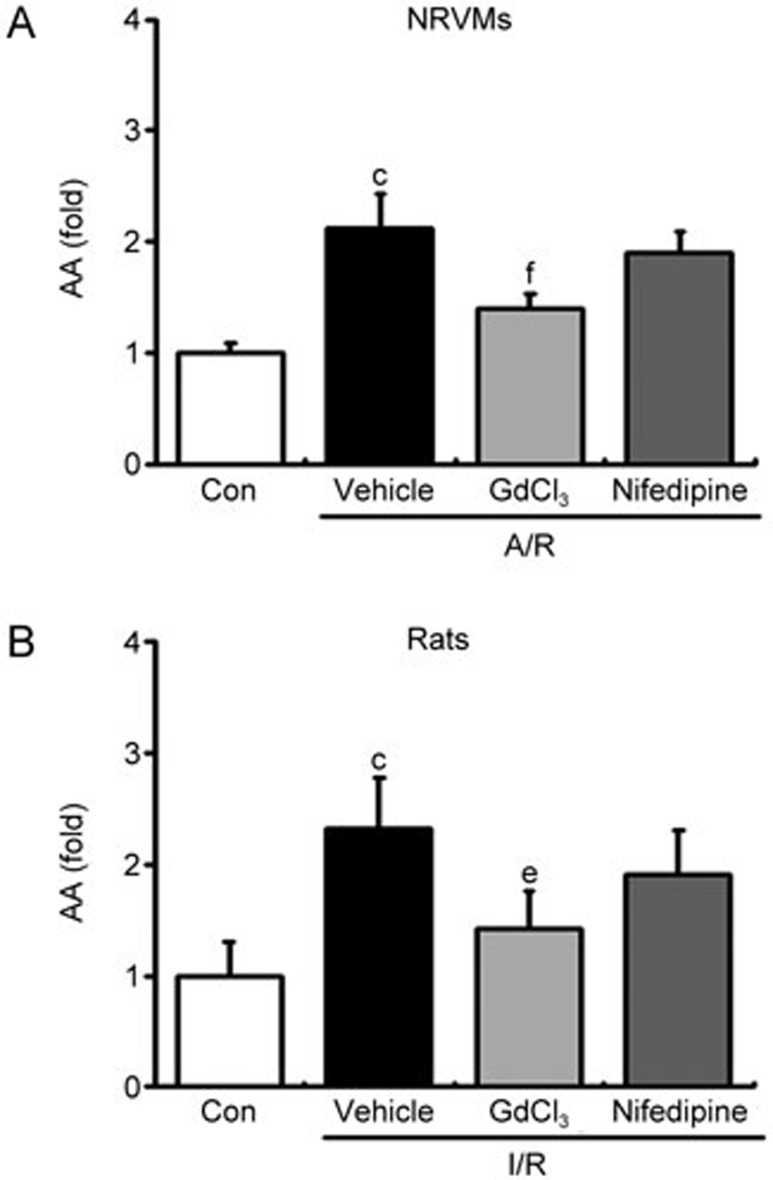
Pretreatment with GdCl3 reduced AA levels in in vitro and in vivo cardiomyocyte injury
Figure 6 shows that A/R- and I/R-treated cardiomyocytes and rats exhibited a dramatic upregulation of AA release compared to the control and sham groups, respectively. In contrast, GdCl3 pretreatment significantly reduced A/R- and I/R-induced AA levels compared to the vehicle-treated A/R and I/R group, respectively. However, nifedipine did not exert a significant inhibitory effect on AA release. These results suggest that GdCl3 abolished the induced AA augmentation due to the A/R or I/R process, which is a crucial factor in the induction of myocardial injury during I/R in vitro and in vivo32,33.
Figure 6.
GdCl3 decreased AA levels in the A/R and I/R models. (A) AA levels in NRVM A/R model with different treatments. All values are presented as the mean±SD. n=8. cP<0.01 vs Control. fP<0.01 vs A/R. (B) Serum AA levels in the I/R rat model with different treatments. All values are presented as the mean±SD. n=8. cP<0.01 vs sham. eP<0.05 vs I/R.
Discussion
Recent studies have indicated that low-dose GdCl3 minimizes hepatic I/R injury and prevents primary graft dysfunction after liver transplantation. The present myocardial I/R rat model demonstrated a lower extent of myocardial injury with decreased infarction size and reduced levels of myocardial injury markers (eg, CK-MB, cTnI, and LDH) in GdCl3 (10 mg/kg) and nifedipine groups compared with the I/R group (Figure 4). The dose of GdCl3 used in the current study was the same as that used in other studies20,34. The increased infarction area of the heart after reperfusion is most likely the result of cell apoptosis35,36. Our study demonstrated that GdCl3 administration reduced the number of TUNEL-positive cells, the death receptor expression, the cytochrome c release and the caspase-3 activation, suggesting an improved cell viability (Figure 5).
Previous studies have demonstrated the involvement of the mitochondrial and death receptor mediated pathways in cardiomyocyte apoptosis13,14. We investigated the regulators of apoptosis in intrinsic (mitochondria) and extrinsic (death receptor) pathways in isolated NRVMs to further elucidate the precise mechanism of GdCl3 against myocardial injury. Mitochondria in a pro-apoptotic state release pro-apoptotic triggers, such as cytochrome c and apoptosis-inducing factor, from the intermembrane space37. Ca2+ is one of the common secondary messengers that is likely involved in mitochondria-mediated apoptosis pathways directly or indirectly. [Ca2+]i and [Ca2+]m overload directly causes post-I/R oxidative stress and myocardial apoptosis. In this study, we found that low-dose GdCl3 dramatically inhibited AA-induced Ca2+ overload and elevated resting [Ca2+]i in A/R NRVMs (Figure 3B–E). We also demonstrated that low-dose GdCl3 significantly ameliorates I/R-induced cytochrome c release in vivo (Figure 5H) and in vitro (Figure 3A) and inhibits cell apoptosis via regulation of a mitochondrial-dependent cell apoptosis pathway.
Previous studies have demonstrated that pathophysiological responses triggered after reperfusion include the release of activation factors and free radicals, which activate phospholipase A2 and increase AA release24. The accumulated AA in the myocardium may play an important role in post-I/R injury because a time-dependent degradation of membrane phospholipids associated with an increase in membrane permeability was observed in the ischemic myocardium17,38. The [Ca2+]m overload may be an upstream signal for AA-induced mitochondrial-mediated apoptosis39. Our previous studies have suggested that GdCl3 at a molar ratio of 1/3 AA, which is different from other Ca2+ antagonists, almost completely inhibits AA-induced intracellular Ca2+ release and extracellular Ca2+ inflow18,19. Another study of ours20 has found that a fixed ratio of GdCl3/AA (1: 3) is required to satisfactorily inhibit Ca2+ signal responses in NRVMs. GdCl3 eliminates AA-induced cardiomyocyte apoptosis, probably through a direct chemical interaction with AA because mass and UV-Vis spectra measurements suggested that a new complex formed when GdCl3 was proportionally mixed with AA (GdCl3:AA=1:3). Therefore, GdCl3 may act as a scavenger of AA and block the properties and effects of AA. In the present study, we observed that low-dose GdCl3 pretreatment inhibited cell apoptosis in A/R and I/R models, and it dramatically decreased the level of AA in in vitro and in vivo measurements (Figure 6). Therefore, this study provides further evidence for the association of enhanced AA accumulation following ischemic damage in vitro in cardiomyocytes and an in vivo animal model heart. This study also suggests a possible mechanism in which GdCl3 acts as an AA scavenger to protect against cell apoptosis during I/R.
Death receptor-related signaling is another important pathway associated with cardiomyocyte apoptosis during I/R. Fas-mediated apoptosis is an important effector process in the progressive loss of cardiomyocytes40. The binding of Fas to its ligand (FasL) results in receptor cross-linking and apoptosis via receptor oligomerization and recruitment of the Fas-associated death domain protein (FADD), which regulates the proteolytic activity of caspase-8 and caspase-3 activation41. Our data indicated that A/R and I/R treatment activated death receptor pathways, and GdCl3 pretreatment clearly decreased the levels of death receptors and related downstream signal molecules, such as Fas/DR5/FADD (Figures 2 and 5), caspase-8 and caspase-3 activity in both models (Figures 1, 2 and 5).
Notably, GdCl3 was less potent than nifedipine in the inhibition of KCl-induced Ca2+ increases (an indication of L-type Ca2+ channel activation), but GdCl3 was much more potent in suppressing AA-induced Ca2+ signaling: 5 μmol/L GdCl3 caused a complete abolishment of such signaling in NRVMs (Figure 3 and Supplementary Figure S2). These data suggest that GdCl3 exerts a weaker inhibitory effect on myocardial contraction and rhythm than nifedipine, which is a common and dangerous side effect of Ca2+ channel blockers in clinical practice, especially in ischemic hearts. This difference in their effects may represent an advantage of GdCl3 over Ca2+ channel blockers for the clinical application of inhibiting cell apoptosis without affecting myocardial contraction and rhythm. In addition, a previous study has suggested that stretch-activated ion channels also play a key role in cardiac pathophysiology42, and GdCl3 is the most widely used antagonist of this channel. Abnormal tissue stretch is a classical feature of myocardial I/R21,43. Therefore, the antagonism effect of GdCl3 on stretch-activated ion channels may also reflect another advantage of GdCl3 over other drugs.
In summary, the current data demonstrated for the first time that low-dose GdCl3 significantly ameliorates I/R-induced myocardial infarction via the reduction of cardiomyocyte apoptosis through the inhibition of death receptor and mitochondrial-mediated apoptosis pathway activation, thus providing a potential candidate for therapies of acute coronary syndrome, thrombolysis, or extracorporeal circulation-induced myocardial injury.
Author contribution
Yuan-yuan ZHENG and Da-Li LUO conceived and designed the experiments; Min CHEN, Jing-yi XUE, Yun-tao SONG, Zheng-yang LIANG, Xin-xin YAN and Yuan-yuan ZHENG performed the experiments and analyzed the data; Min CHEN and Yuan-yuan ZHENG wrote the manuscript; Da-Li LUO revised the manuscript. All the authors read and approved the final paper.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (No 81302777 and 81370339) and the Beijing Key Laboratory of Cardiovascular Diseases Related to Metabolic Disturbance (No Z13111000280000).
Supplementary Information
References
- Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarction. Cardiovasc Res 2002; 53: 31–47. [DOI] [PubMed] [Google Scholar]
- Sutton MG, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation 2000; 101: 2981–8. [DOI] [PubMed] [Google Scholar]
- Mersmann J, Latsch K, Habeck K, Zacharowski K. Measure for ameasure-determination of infarct size in murine models of myocardial ischemia and reperfusion: a systematic review. Shock 2011; 35: 449–55. [DOI] [PubMed] [Google Scholar]
- Yellon DM, Hausenloy DJ. Myocardial reperfusion injury. N Engl J Med 2007; 357: 1121–35. [DOI] [PubMed] [Google Scholar]
- Frank A, Bonney M, Bonney S, Weitzel L, Koeppen M, Eckle T. Myocardial ischemia reperfusion injury: from basic science to clinical bedside. Semin Cardiothorac Vasc Anesth 2012; 16: 123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson AB, Gottlieb RA. Mechanisms of apoptosis in the heart. J Clin Immunol 2003; 23: 447–59. [DOI] [PubMed] [Google Scholar]
- Liu H, Guo X, Chu Y, Lu S. Heart protective effects and mechanism of quercetin preconditioning on anti-myocardial ischemia reperfusion (IR) injuries in rats. Gene 2014; 545: 149–55. [DOI] [PubMed] [Google Scholar]
- Lu C, Ren D, Wang X, Ha T, Liu L, Lee EJ, et al. Toll-like receptor 3 plays a role in myocardial infarction and ischemia/reperfusion injury. Biochim Biophys Acta 2014; 1842: 22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrashekhar Y, Sen S, Anway R, Shuros A, Anand I. Long-term caspase inhibition ameliorates apoptosis, reduces myocardial troponin-I cleavage, protects left ventricular function, and attenuates remodeling in rats with myocardial infarction. J Am Coll Cardiol 2004; 43: 295–301. [DOI] [PubMed] [Google Scholar]
- Boisguerin P, Giorgi JM, Barrère-Lemaire S. CPP-conjugated anti-apoptotic peptides as therapeutic tools of ischemia-reperfusion injuries. Curr Pharm Des 2013; 19: 2970–8. [DOI] [PubMed] [Google Scholar]
- Dorn GW 2nd. Apoptotic and non-apoptotic programmed cardiomyocyte death in ventricular remodelling. Cardiovasc Res 2009; 81: 465–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamura T, Hasegawa K, Morimoto T, Iwakura A, Nishina T, Nomoto T, et al. Down-regulation of endothelin-1 and alteration of apoptosis signaling following left ventricular volume reduction surgery in heart failure of adult rats. J Cardiovasc Pharmacol 2004; 44: S366–71. [DOI] [PubMed] [Google Scholar]
- Li D, Liu M, Tao TQ, Song DD, Liu XH, Shi DZ. Panax quinquefolium saponin attenuates cardiomyocyte apoptosis and opening of the mitochondrial permeability transition pore in a rat model of ischemia/reperfusion. Cell Physiol Biochem 2014; 34: 1413–26. [DOI] [PubMed] [Google Scholar]
- Stephanou A, Scarabelli TM, Brar BK, Nakanishi Y, Matsumura M, Knight RA, et al. Induction of apoptosis and Fas receptor/Fas ligand expression by ischemia/reperfusion in cardiac myocytes requires serine 727 of the STAT-1 transcription factor but not tyrosine 701. J Biol Chem 2001; 276: 28340–7. [DOI] [PubMed] [Google Scholar]
- Czerski L, Nunez G. Apoptosome formation and caspase activation: is it different in the heart. J Mol Cell Cardiol 2004; 37: 643–52. [DOI] [PubMed] [Google Scholar]
- Fang KM, Lee AS, Su MJ, Lin CL, Chien CL, Wu ML. Free fatty acids act as endogenous ionophores, resulting in Na+ and Ca2+ influx and myocyte apoptosis. Cardiovasc Res 2008; 78: 533–45 [DOI] [PubMed] [Google Scholar]
- Maia RC, Culver CA, Laster SM. Evidence against calcium as a mediator of mitochondrial dysfunction during apoptosis induced by arachidonic acid and other free fatty acids. J Immunol 2006; 177: 6398–404. [DOI] [PubMed] [Google Scholar]
- Luo D, Broad LM, Bird GJ, Putney JW Jr. Mutual antagonism of calcium entry by capacitative and arachidonic acid-mediated Ca2+ entry pathways. J Biol Chem 2001; 276: 20186–9. [DOI] [PubMed] [Google Scholar]
- Luo D, Sun H, Lan X, Xiao R, Han Q. Direct coupling between AA-induced Ca2+ release and Ca2+ entry in HEK293 cells. Prostgland Other Mediat 2005; 75: 141–51. [DOI] [PubMed] [Google Scholar]
- Zheng Y, Zhang H, Yan X, Chen M, Qi T, Zhang L, et al. Protective effect of low dose gadolinium chloride against isoproterenol-induced myocardial injury in rat. Apoptosis 2015; 20: 1164–75. [DOI] [PubMed] [Google Scholar]
- Yan L, Zhu TB, Wang LS, Pan SY, Tao ZX, Yang Z, et al. Inhibitory effect of hepatocyte growth factor on cardiomyocytes apoptosis is partly related to reduced calcium sensing receptor expression during a model of simulated ischemia/reperfusion. Mol Biol Rep 2011; 38: 2695–701. [DOI] [PubMed] [Google Scholar]
- Gulati P, Muthuraman A, Jaggi AS, Singh N. Neuroprotective effect of gadolinium: a stretch-activated calcium channel blocker in mouse model of ischemia-reperfusion injury. Naunyn Schmiedebergs Arch Pharmacol 2013; 386: 255–64 [DOI] [PubMed] [Google Scholar]
- Wang B, Zhang Q, Zhu B, Cui Z, Zhou J. Protective effect of gadolinium chloride on early warm ischemia/reperfusion injury in rat bile duct during liver transplantation. PLoS One 2013; 8: e52743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strande JL, Routhu KV, Hsu A, Nicolosi AC, Baker JE. Gadolinium decreases inflammation related to myocardial ischemia and reperfusion injury. J Inflamm 2009; 6: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider L, Hackert T, Longerich T, Hartwig W, Fritz S, Krych R, et al. Effects of gadolinium chloride and glycine on hepatic and pancreatic tissue damage in alcoholic pancreatitis. Pancreas 2010; 39: 502–9. [DOI] [PubMed] [Google Scholar]
- Duan JL, Wang JW, Guan Y, Yin Y, Wei G, Cui J, et al. Safflor yellow A protects neonatal rat cardiomyocytes against anoxia/reoxygenation injury in vitro. Acta Pharmacol Sin 2013; 34: 487–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo D, Yang D, Lan X, Li K, Li X, Chen J, et al. Nuclear Ca2+ sparks and waves mediated by inositol 1,4,5-trisphosphate receptors in neonatal rat cardiomyocytes. Cell Calcium 2008; 43: 165–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang R, Li Y, Yang X, Yue Y, Dou L, Wang Y, et al. Protective role of deoxyschizandrin and schisantherin A against myocardial ischemia–reperfusion injury in rats. PloS One 2013; 8: e61590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang MQ, Zhang YL, Chen H, Tu JF, Shen Y, Guo JP, et al. Sodium tanshinone IIA sulfonate protects rat myocardium against ischemia-reperfusion injury via activation of PI3K/Akt/FOXO3A/Bim pathway. Acta Pharmacol Sin 2013; 34: 1386–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsässer A, Suzuki K, Schaper J. Unresolved issues regarding the role of apoptosis of ischemic injury and heart failure. J Mol Cell Cardiol 2000; 32: 711–24. [DOI] [PubMed] [Google Scholar]
- Yousif MH, Benter IF, Roman RJ. Cytochrome P450 metabolites of arachidonic acid play a role in the enhanced cardiac dysfunction in diabetic rats following ischaemic reperfusion injury. Auton Autacoid Pharmacol 2009; 29: 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross GJ, Falck JR, Cross ER, Isbell M, Moore J, Nithipatikom K. Cytochrome P450 and arachidonic acid metabolites: role in myocardial ischemia/reperfusion injury revisited. Cardiovasc Res 2005; 68: 18–25. [DOI] [PubMed] [Google Scholar]
- Liang Z, Liu LF, Yao TM, Huo Y, Han YL. Cardioprotective effects of Guanxinshutong (GXST) against myocardial ischemia/reperfusion injury in rats. J Geriatr Cardiol 2012; 9: 130–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giakoustidis D, Papageorgiou G, Iliadis S, Giakoustidis A, Kostopoulou E, Kontos N, et al. The protective effect of alpha-tocopherol and GdCl3 against hepatic ischemia/reperfusion injury. Surg Today 2006; 36: 450–6. [DOI] [PubMed] [Google Scholar]
- Kim SJ, Kuklov A, Crystal GJ. In vivo gene delivery of XIAP protects against myocardial apoptosis and infarction following ischemia/reperfusion conscious rabbits. Life Sci 2011; 88: 572–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarabelli TM, Knight R, Stephanou A, Townsend P, Chen-Scarabelli C, Lawrence K, et al. Clinical implications of apoptosis in ischemic myocardium. Curr Probl Cardiol 2006; 31: 181–264. [DOI] [PubMed] [Google Scholar]
- Kristen AV, Ackermann K, Buss S, Lehmann L, Schnabel PA, Haunstetter A, et al. Inhibition of apoptosis by the intrinsic but not the extrinsic apoptotic pathway in myocardial ischemia-reperfusion. Cardiovasc Pathol 2013; 22: 280–6. [DOI] [PubMed] [Google Scholar]
- Voora D, Ortel TL, Lucas JE, Chi JT, Becker RC, Ginsburg GS. Time-dependent changes in non-COX-1-dependent platelet function with daily aspirin therapy. J Thromb Thrombolysis 2012; 33: 246–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang KM, Chang WL, Wang SM, Su MJ, Wu ML. Arachidonic acid induces both Na+ and Ca2+ entry resulting in apoptosis. J Neurochem 2008; 104: 1177–89. [DOI] [PubMed] [Google Scholar]
- Peter ME, Krammer PH. The CD95 (APO-1/Fas) DISC and beyond. Cell Death Differ 2003; 10: 26–35. [DOI] [PubMed] [Google Scholar]
- Nicolosi AC, Kwok CS, Logan B. Effects of gadolinium on regionally stunned myocardium: temporal considerations. J Surg Res 2007; 139: 286–91. [DOI] [PubMed] [Google Scholar]
- Bhuiyan MS, Fukunaga K. Inhibition of HtrA2/Omi ameliorates heart dysfunction following ischemia/reperfusion injury in rat heart in vivo. Eur J Pharmacol 2007; 557: 168–77. [DOI] [PubMed] [Google Scholar]
- Hao J, Kim HS, Choi W, Ha TS, Ahn HY, Kim CH. Mechanical stretch-induced protection against myocardial ischemia-reperfusion injury involves AMP-activated protein kinase. Korean J Physiol Pharmacol 2010; 14: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.