Abstract
African American women report high rates of physical inactivity and related health disparities. In our previous formative research, we conducted a series of qualitative assessments to examine physical activity barriers and intervention preferences among African American women in the Deep South. These data were used to inform a 12-month Home-based, Individually-tailored Physical activity Print (HIPP) intervention, which is currently being evaluated against a wellness contact control condition among 84 post-menopausal African American women residing in the metropolitan area of Birmingham, Alabama. This paper reports the rationale, design and baseline findings of the HIPP trial. The accrued participants had an average age of 57 (SD= 4.7), a BMI of 32.1 kg/m2 (SD=5.16) with more than half (55%) having a college education and an annual household income under $50,000 (53.6%). At baseline, participants reported an average of 41.5 minutes/week (SD=49.7) of moderate intensity physical activity, and 94.1% were in the contemplation or preparation stages of readiness for physical activity. While social support for exercise from friends and family was low, baseline levels of self-efficacy, cognitive and behavioral processes of change, decisional balance, outcome expectations, and enjoyment appeared promising. Baseline data indicated high rates of obesity and low levels of physical activity, providing strong evidence of need for intervention. Moreover, scores on psychosocial measures suggested that such efforts may be well received. This line of research in technology-based approaches for promoting physical activity in African American women in the Deep South has great potential to address health disparities and impact public health.
Keywords: physical activity, health disparities, home-based interventions, African American women
Introduction
To date, African Americans have the highest death rate and shortest survival of any racial/ethnic group in the U.S. for most cancers.1 Among women, existing racial disparities are largely due to breast and colon cancers. According to the American Cancer Society (ACS), African American women have mortality rates that are 44% higher for colorectal cancer and 39% higher for breast cancer than White women.1 Disparities such as these necessitate intervention, and sedentary lifestyle is one of the few modifiable risk factors for breast and colon cancer.1 Numerous observational studies indicate that regular moderate-to-vigorous physical activity can reduce the risk of developing colon cancer by 25-40%2-7 and breast cancer by 20-80%8-11 in adults. Larger risk reductions (average 41%) were observed in three studies focused on African American women.9,11 While the exact mechanisms have yet to be determined, physical activity may influence breast and colon cancer risk indirectly by promoting weight control or directly by altering biologic pathways related to breast and/or colon cancer (e.g., concentrations of insulin, adipocytokines, sex steroid hormones; gene expression).3,4,10,12
Due to its cancer-protective effects, at least 30 minutes of moderate-to-vigorous physical activity on 5 or more days of the week is recommended by the ACS.13 Despite these recommendations, most Americans remain sedentary14 with national survey data indicating particularly low levels of regular leisure-time physical activity in African American women (19.8%).1 As sedentary behavior may contribute to existing cancer disparities, interventions aiming to increase physical activity among African American women are needed. Past efforts to promote physical activity in general (and as a strategy for reducing cancer risk) among African American women have typically involved center- or clinic-based programs,15-17 which have limited reach and may be difficult for many individuals to attend. Home-based interventions minimize many barriers to interventions commonly cited by African American women (e.g., childcare and monetary costs).18
Our research team has developed and tested a computer expert system19-22 that individually tailors self-help print materials based on constructs from the Social Cognitive Theory23 and Transtheoretical Model.24 This program can be mail-delivered and now specifically addresses the physical activity intervention needs and preferences of African American women, as identified by our formative research (11 focus groups with the target population in rural and urban counties across Alabama). 25 A one-month demonstration trial (N=10 African American women recruited in Birmingham, AL) was previously conducted to vet the resulting theory-based individually-tailored physical activity intervention. Results showed participant satisfaction and increased motivational readiness for physical activity in 70% of the participants, as well as 90% retention. Moreover, there was almost a doubling of moderate-to-vigorous physical activity from baseline (M=89.5 min/week, SD=61.17) to 1 month (M=155 min/week, SD=100.86; p=.056).25 Building on these promising findings, the current study will test the Home-based Individually tailored Physical activity Print (HIPP) intervention for African American women in the Birmingham, AL metropolitan area against a wellness contact control condition. The purpose of the current paper is to describe the rationale, design, and baseline findings of this study.
Methods
Design
The HIPP study is an ongoing randomized controlled trial (N=84) of a 12-month computer-tailored physical activity intervention for cancer risk reduction compared to a wellness contact control condition among African American women. Addressing key areas derived from Bowen and colleagues' framework for feasibility studies26 (see Table 1), we hypothesize that participant satisfaction questionnaire/interview data, recruitment, retention, and adherence will demonstrate the acceptability and demand for the HIPP intervention among African American women. As for limited efficacy testing, we expect increases in physical activity from baseline to six months (7-Day Physical Activity recall interviews, accelerometers) will be greater in the intervention arm as compared to the control arm. Moreover, we anticipate that arm differences at 6 months will be sustained at 12 months.
Table 1. Key areas of focus for feasibility studies and how they were addressed in the current study.
| Key area* | Definition | Outcomes of interest | Assessed in this study? |
|---|---|---|---|
| Acceptability | Is a new program suitable, satisfying, or attractive to participants? | Satisfaction, intent to continue use, perceived appropriateness | Yes. By participant satisfaction surveys, exit interviews, recruitment |
| Demand | Is a new program likely to be used? | Actual use, expressed interest or intention to use, perceived demand | Yes. By participant satisfaction surveys, exit interviews, adherence, retention |
| Implementation | Can a new program be successfully delivered to intended participants in some defined, but not fully controlled, context? | Degree of execution, success or failure of execution | No. This study was conducted in a rather controlled context. Please see discussion for future directions. |
| Practicality | Can a program be carried out with intended participants using existing means, resources, and circumstances and without outside intervention? | Amount/type of resources needed to implement; factors affecting ease or difficulty of implementation; efficiency, speed, or quality of implementation; positive/negative effects on target participants; ability of participants to carry out intervention activities; cost analysis | Somewhat. We will be able to comment on positive/negative effects on participants (improved physical activity). Future directions include cost analyses, which have already been conducted on similar programs in different populations and support practicality.69 See discussion for future directions. |
| Adaption | To what extent does an existing program perform when changes are made for a new format or with a different population? | Degree to which similar outcomes are obtained in new format, process outcomes comparison between intervention use in two populations | Somewhat. We will be able to compare findings with our participants to past studies using similar interventions in different populations. |
| Integration | To what extent can a new program be integrated within an existing system? | Perceived fit with infrastructure, perceived sustainability | No. Program was implemented by research staff in current study. Please see discussion for future directions. |
| Expansion | To what extent can a previously tested program, process, approach, or system be expanded to provide a new program or service? | Costs to organization and policy bodies, fit with organizational goals and culture, positive or negative effects on organization, disruption due to expansion component | No. Please see discussion for future directions. |
| Limited efficacy | Does the new program show promise of being successful with the intended population, even in a highly controlled setting? | Intended effects of program or process on key intermediate variables, effect-size estimation, maintenance of changes from initial change | Yes. We will examine group differences in changes in physical activity from baseline to 6 and 12 months. Data will be used to estimate effect sizes for future power analyses. |
Adapted from Bowen and colleagues26
Secondary aims include exploring differences between groups on changes in functional exercise capacity (6 minute walk test), body mass index (BMI), waist circumference, and percent body fat (estimated by bioelectrical impedance); associations between changes in physical activity and changes in these variables; and potential moderators (e.g., education) and mediators (Social Cognitive Theory and Transtheoretical Model constructs directly targeted by the physical activity intervention) that are associated with intervention efficacy. Blood draws at baseline, six months, and 12 months will allow for hormone assays (e.g, insulin, leptin, free estradiol, and other circulating biomarkers implicated in cancer pathways) and exploratory studies of gene expression.
Setting and Sample
The study is being conducted at the Clinical Research Unit at the University of Alabama at Birmingham (UAB) Center for Clinical and Translational Science. Human subjects approval was obtained from the UAB Institutional Review Board and the trial is registered with ClinicalTrials.gov (NCT02574689). Participants are women between the ages of 50-69 from the Birmingham, AL metropolitan area who self-identified as African American and/or Black. Post-menopausal women were recruited for the current study to avoid problems associated with timing of the menstrual cycle when measuring hormones and because there is more evidence for an inverse association between physical activity and breast cancer risk in postmenopausal women.27 At the time of writing this publication, recruitment of study participants is completed. See Table 2 for demographic characteristics.
Table 2. Demographic characteristics of the HIPP study participants.
| Characteristics* | Intervention (n=43) (M and SD or %) | Control (n=41) (M and SD or %) | Overall (N=84) (M and SD or %) |
|---|---|---|---|
|
| |||
| African American women | 100% | 100% | 100% |
|
| |||
| Age (n=84) | 56.65 (4.78) | 57.29(4.69) | 56.96 (4.71) |
|
| |||
| Educational level | |||
| <High school degree | 4.7% | 4.9% | 4.8% |
| High school graduate | 2.3% | 2.4% | 2.4% |
| Some college | 41.9% | 31.7% | 36.9% |
| College graduate | 25.6% | 34.1% | 29.8 |
| Post-graduate work | 25.6% | 26.8% | 26.2% |
| Do not know | 0% | 0% | 0% |
|
| |||
| Employment | |||
| Unemployed | 2.3% | 7.3% | 4.8% |
| Retired | 20.9% | 24.4% | 22.6% |
| Full time | 65.1% | 56.1% | 60.7% |
| Part time | 9.3% | 12.2% | 10.7% |
| Do not know | 2.3% | 0% | 1.2% |
|
| |||
| Annual household income | |||
| < $10,000 | 2.3% | 9.8% | 6% |
| ≥$10,000 but <$20,000 | 7.0% | 9.8% | 8.3% |
| ≥ $20,000 but <$30,000 | 9.3% | 17.1% | 13.1% |
| ≥ $30,000 but <$40,000 | 9.3% | 7.3% | 8.3% |
| ≥$40,000 but <$50,000 | 20.9% | 14.6% | 17.9% |
| ≥$50,000 | 51.2% | 39% | 45.2% |
| Do not know | 0% | 2.4% | 1.2% |
|
| |||
| Marital status | |||
| Married/living with partner | 51.2% | 31.7% | 41.7% |
| Single | 14.0% | 12.2% | 13.1% |
| Divorced | 23.3% | 39% | 30% |
| Separated | 2.3% | 4.9% | 3.6% |
| Widowed | 9.3% | 9.8% | 9.5% |
| Do not know | 0% | 2.4% | 1.2% |
|
| |||
| BMI (n=84) | 32.42 (5.17) | 31.79 (5.19) | 32.11 (5.16) |
|
| |||
| Waist (cm, n=77) | 100.69(11.35) | 99.79(4.69) | 100.26(11.5) |
|
| |||
| Body Fat % (n=74) | 46.88. (6.59) | 47.21(6.48) | 47.03(6.50) |
There were no significant group differences in demographic characteristics.
Recruitment and Retention
Recruitment activities involved face-to-face recruiting and placing flyers in public areas in the Birmingham, AL metropolitan area, such as municipal buildings (city hall, county health department), community centers, and libraries. Other recruitment methods included advertising on local radio stations and attendance at local churches. Participants were given flyers and encouraged to consider referring friends, relatives, and coworkers, to facilitate “word of mouth” recruitment. These efforts were led by an experienced recruitment coordinator with extensive connections in the community and a broad network of contacts through the Deep South Network for Cancer Control.
To minimize obstacles to research participation (e.g., costs, transportation), the intervention is provided free of charge and through the mail. Participants are compensated for their time and receive $35 at the baseline, 6 months and 12 months assessments and $10 each month for completing the packet of psychosocial measures used to tailor feedback reports and mailing them back to the research center.
Screening and Eligibility Requirements
Interested individuals telephoned the research center and completed an eligibility screening interview, including items from the Physical Activity Readiness Questionnaire (PAR-Q) to assess cardiovascular/musculoskeletal risk factors.28,29 A history of heart disease, myocardial infarction, angina, stroke, BMI over 45, orthopedic conditions which limit mobility, or any serious medical condition that would make physical activity unsafe were grounds for ineligibility. The study physician (E.K.) provided guidance on medical questions that arose when screening for eligibility.
Eligibility criteria included post-menopausal status (defined as not having menstrual periods for at least 12 months), not taking medication that may impair physical activity tolerance or performance (e.g., beta blockers), not planning to move from the area within the next year, and scoring ≥19 on the Rapid Estimate of Adult Literacy in Medicine (REALM),30 as the intervention materials were written at a 4th grade reading level.20 Finally participants had to report being insufficiently active (e.g., engaging in moderate or vigorous physical activity < 60 minutes per week) at the point of screening and were encouraged to not make any changes to their exercise habits before starting the study. Once initial eligibility was confirmed by the phone screen interview, participants were scheduled for an orientation session to learn more about the study.
Orientation
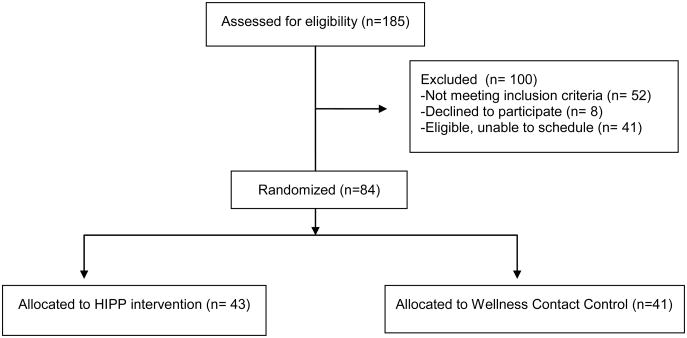
At orientation, research staff gave a PowerPoint© presentation describing the study and answered questions. Interested individuals then completed the informed consent process and demographic questionnaire, and received ActiGraph GT3X accelerometers, with instructions to wear the accelerometer during waking hours for 7 days and return them at the baseline assessment and randomization session. See Figure 1 for study schema.
Figure 1. Study Schema.
Baseline Assessments
Physical Activity
The 7-Day Physical Activity Recall (PAR) interview was administered,31,32 which estimates minutes per week of physical activity and uses several strategies for increasing accuracy of recall. For example, the interview breaks down the week into daily segments (i.e., morning, afternoon, and evening) and asks about many types of activities, including time spent sleeping and in moderate, hard, and very hard activity. This measure has demonstrated reliability, internal consistency, and congruent validity with objective physical activity measures.33-41 It is sensitive to changes in moderate intensity physical activity over time42,43 and has been used in several past studies with African Americans.44-48
The interviewer for the current study is blind to group status and prior to conducting these interviews for study purposes underwent rigorous training on the administration of the 7-Day PAR with a research staff member, who was professionally trained by the Cooper Institute and has completed over 3,000 7-Day PARs. The trainer conducted an intensive training session with the interviewer and demonstrated how to conduct the interview. Then the interviewer conducted two 7-Day PAR interviews under the trainer's direct supervision and received feedback from the trainer on five more audio-taped interviews conducted with volunteers. Finally, the interviewer conducted a 7-Day PAR on the trainer to complete the training. To encourage adherence to protocol, interviews are audio-taped and 10% will be reviewed for quality control.
To corroborate the self-report 7-Day PAR data, participants wore ActiGraph GT3X accelerometers for seven days prior to the baseline assessment (overlapping with the 7-Day PAR recall period). Accelerometers measure both movement and intensity of activity and have been validated with heart rate telemetry49 and total energy expenditure.50 These devices are lightweight, small, and worn on the waist. A 6 Minute Walk Test was also administered, which measures the distance that can be quickly walked on a flat, hard surface in 6 minutes.51,52,53
Psychosocial Variables
Participants completed a brief demographics questionnaire regarding age, education, income, occupation, race, ethnicity, history of residence, and marital status.
Social Cognitive Theory and Transtheoretical Model constructs were also measured at the research center at baseline and on a monthly basis by mail to generate the tailored expert system feedback reports for the intervention group. The 4-item Stages of Readiness Measure was used to categorize participants' stage of motivational readiness for physical activity and has shown reliability (Kappa = 0.78; intra-class correlation r = 0.84) and concurrent validity with measures of self-efficacy and physical activity.54 Self-efficacy or confidence regarding participation in physical activity in various situations (e.g., bad weather) was measured with 5 items (alpha= .82).54 Decisional balance, or the perceived advantages and disadvantages to physical activity participation, was examined by 16 items with acceptable internal consistencies (alphas: Cons = 0.79 and Pros = 0.95) and concurrent validity with stage of change measures.55 The 40-item processes of change measure included 10 sub-scales that address a variety of processes of activity behavior change, with alphas ranging from .62 to .96.56 Social support for exercise from family and friends was assessed by a 13 item-scale (alphas=.61-.91) with previously established criterion validity.57 Outcome expectations, or beliefs on the consequences of physical activity participation, was examined by 9 items with internal consistency (alpha=.89) and validity based on confirmatory factor analysis and positive correlations with physical activity and self-efficacy.58 Physical activity enjoyment was assessed with an 18-item scale with high internal consistency (alpha = 0.96) and test-retest reliability.59
Anthropometrics and Phlebotomy
Participants were measured (height, weight, waist circumference) in a private room wearing light indoor clothes and no shoes. Height was measured using a Digi-Kit stadiometer (Measurement Concepts, North Bend, WA) to the nearest 1/100th cm. Weight was measured on Scaletronix digital scale to nearest 1/10th kilogram. Waist circumference was measured using a Gulick II measuring tape (Country Technology, Gary Mills, WI) that was calibrated for accurate body measurements to ensure repeatable measurements by applying a constant tension. The tape was placed around the waist just above the iliac crest and the measurement was recorded to the nearest 0.1 cm at the end of the participant's normal expiration.
A Quantum II bioelectrical body composition analyzer (RJL Systems, Inc., Detroit, MI), a four-electrode system that determines resistance and reactance, along with the Lukaski equation,60 was used to assess percent body fat. The Lukaski equation was previously shown to provide the most precise and accurate estimates of percent body fat (vs. other available equations) in comparison with DXA among obese African-American women.61
When scheduling appointments, research staff carefully reviewed the protocol requirements for bioelectrical impedance analysis with participants (e.g., fast for 8 hours prior to testing; refrain from exercise, sauna, and alcohol for 12 hours prior to testing; arrive in a euvolemic state with no overt signs/symptoms of dehydration or edema) and prioritized the convenience and comfort of the participants (e.g., offered appointments first thing in the morning, provided light refreshments after testing).
Blood (10mL) was drawn, centrifuged, separated into plasma and white cells, and frozen at −80° C for future batch analysis, including hormone assays and exploratory studies of gene expression.
Randomization
After completing baseline study measures, participants were randomly assigned to one of two print-based, mail-delivered intervention conditions: HIPP intervention or wellness contact control. Treatment allocation was stratified by BMI (BMI<30 and BMI≥30), as this variable is related to activity levels.62,63 Randomization lists were pre-prepared by the study statistician and participants received their group assignment in a sealed envelope. Participants are currently receiving regular mailings of group-appropriate cancer prevention information over six months (i.e., three mailings in month 1, two mailings in months 2-3, and one mailing in months 4-6, with booster mailings in months 8, 10, 12; see Figure 1) and will return to the research center for assessments at 6 and 12 months.
HIPP intervention
The physical activity intervention is based on the Social Cognitive Theory23 and Transtheoretical Model24 and emphasizes behavioral strategies (i.e., goal-setting, self-monitoring with Accusplit AE120XLv3-xBX pedometers and logs, problem-solving barriers, increasing social support, rewarding oneself for meeting physical activity goals) for gradually increasing physical activity until the national guidelines are reached, and includes regular mailings (see Figure 1) of physical activity manuals that are matched to the participant's current level of motivational readiness and individually-tailored computer expert system feedback reports. The computer expert system reports provide feedback on each participants': 1) current stage of readiness for physical activity; 2) self-efficacy; 3) decisional balance; 4) social support; 5) outcome expectations; 6) perceived enjoyment; 7) how the participant compares to her prior responses (progress feedback); 8) how the participant compares to individuals who are physically active and with national guidelines (normative feedback); 9) self regulation (use of pedometers to self monitor physical activity behavior). Participant responses to the monthly update surveys are used by the computer expert system to generate appropriate messages for the feedback reports from a bank of 531 messages addressing different levels of psychosocial and environmental factors affecting physical activity.
Intervention participants also receive tip sheets addressing physical activity barriers (e.g., time, negative outcome expectations, safety, costs, enjoyment, social support, fear of injury) specific to African American women that were informed by our previous formative research. 25 Moreover, efforts were made to enhance the appeal and relevance of this program for our target population by incorporating religiosity (including relevant scripture in intervention text), emphasizing physical activity health benefits other than weight loss (i.e., chronic disease prevention), highlighting preferred activities (walking, dance, aerobics), and working with a local African American female graphic designer to improve the appearance and appeal of intervention materials (e.g., add pictures of African American women of all sizes exercising, streamline text, include more color graphics). Further detail on the intervention needs and preferences of African American women in the Deep South have been reported previously by Pekmezi and colleagues.25
For intervention fidelity, participant satisfaction questionnaires will ask if women received and read the intervention materials. Late/unreturned monthly update surveys prompt staff to call and ask whether intervention materials were received in the mail. Research staff audit 10% of tailored reports for quality control. After hand-scoring original data and comparing results to normative scores and prior results obtained from that participant, auditors review reports and determine if the expert system selected correct content. This system allows for early detection and correction of errors in the programming.
Wellness Contact Control Condition
Cancer prevention information on topics other than physical activity (e.g., “Add Fruits and Veggies to Your Diet”; See Figure 1) from the American Cancer Society website (www.cancer.org) are mailed to control participants at identical time points that the HIPP Intervention participants receive their physical activity intervention materials, thus controlling for number of contacts (see Figure 1).
Six and Twelve Month Assessments
Six month and twelve month assessment sessions are ongoing. Participants are mailed ActiGraph accelerometers with instructions to wear them for 7 days prior to both visits. At these sessions, participants return the accelerometers and complete anthropometric and psychosocial measures, the 6 Minute Walk Test, and the 7-Day Physical Activity Recall interview again, along with blood draws. Participant satisfaction questionnaires will be administered and a subsample will be asked to undergo qualitative in-depth interviews to explore participants' overall perceptions and satisfaction with the intervention. Suggestions for program improvement are solicited.
Data Analyses and Sample Size Considerations
Baseline physical activity and psychosocial data are available and are summarized, along with demographic characteristics, in Tables 2 and 3 and compared across treatment arms (using t-tests for continuous measures and chi square analyses for categorical variables). There were no significant group differences in demographic, physical activity or psychosocial variables at baseline assessment.
Table 3. Baseline physical activity levels and related psychosocial variables (N=84).
| Variables* | Intervention Mean(SD) or % | Control Mean(SD) or % | Overall Mean(SD) or % |
|---|---|---|---|
|
| |||
| Self report physical activity (minutes/week, 7-Day PAR, N=82) | 35.10(47.80) | 48.23(51.33) | 41.50(49.69) |
|
| |||
| Accelerometer measured physical activity (minutes/week, N=80) | 12.81 (34.24) | 14.66 (35.23) | 13.69(34.51) |
|
| |||
| 6 Minute Walk Test (meters, N=84) | 377.73 (62.05) | 386.25 (54.48) | 381.89 (58.29) |
|
| |||
| Stage of Change for Physical Activity (N=84) | |||
| Precontemplation | 2.3% | 0% | 1.2% |
| Contemplation | 44.2% | 36.6% | 40.5% |
| Preparation | 51.2% | 56.1% | 53.6% |
| Action | 0% | 2.4% | 1.2% |
| Maintenance | 2.3% | 4.9% | 3.6% |
|
| |||
| Decisional Balance (scores >0 indicate more pros than cons to physical activity, N=81) | 2.02 (1.16) | 2.09 (1.14) | 2.06 (1.14) |
|
| |||
| Physical Activity Self-Efficacy (range = 1-5, N=84) | 3.11 (0.94) | 2.84(1.01) | 2.98(.98) |
|
| |||
| Physical Activity Enjoyment (range = 18-126, N=82) | 92.26 (23.78) | 99.46(21.51) | 95.68(22.88) |
|
| |||
| Behavioral Processes of Change for Physical Activity (range = 1-5, N=80) | 3.17 (.67) | 3.05 (0.71) | 3.12(.69) |
|
| |||
| Cognitive Processes of Change for Physical Activity (range = 1-5, N=81) | 3.40 (0.79) | 3.50 (0.86) | 3.45 (.82) |
|
| |||
| Social Support for Physical Activity | |||
| Friends (range =10-50, N=73) | 22.49 (11.63) | 24.19 (12.28) | 23.23 (11.87) |
| Family (range = 10-50, N=80) | 25.56 (11.47) | 26.41 (10.61) | 25.95 (11.02) |
| Reward & Punishment (range = 3-15, N=82) | 8.95 (3.58) | 10.03 (3.12) | 9.46 (3.39) |
|
| |||
| Outcome expectations for Physical Activity (range = 1-5, N=84) | 4.18 (1.08) | 4.26 (.90) | 4.22 (.99) |
There were no significant group differences in baseline physical activity levels and related psychosocial variables.
Once 6 and 12 months assessment data are available, we will address acceptability, demand, and limited efficacy testing (key areas of focus for feasibility studies in the framework provided by Bowen and colleagues26). Using a mixed methods approach to assessing the acceptability and demand for the HIPP intervention among African American women in the Deep South, we will describe both quantitative participant satisfaction questionnaire data and themes from qualitative exit interview data related to outcomes of interest (e.g., satisfaction, intention to continue use, perceived appropriateness, actual use, expressed interest/intention to use, as suggested by Bowen and colleagues). Moreover, recruitment, retention, and adherence will be examined. Recruitment goals being met and at least 80% retention at 6 and 12 months will be viewed as favorable indicators of acceptability and demand. To account for adherence, data on return of update surveys will also be collected and analyzed. We anticipate that participants will mail back to the research center at least 80% of the 6 completed update surveys required by the study protocol (Figure 1).
Limited efficacy testing for the current study will involve analyzing group differences in changes in physical activity. The analyses will include assessing the distribution of the self-report physical activity and, if necessary, making a normalizing transformation of this variable. Effectiveness of the randomization procedure across demographic and psychosocial variables will be assessed and a longitudinal regression model, implemented using Generalized Estimating Equations (GEE), will be used to model the effect of treatment assignment on mean minutes of physical activity at 6 and 12 months, while controlling for key baseline covariates. Data will be analyzed by intent-to-treat. Missing data will be imputed by carrying the last value forward. To corroborate these self-report findings, similar analyses will be conducted using accelerometer data.
For sample size considerations, power analysis was designed to test the hypothesis that the intent-to-treat effect was 0 versus the 2-sided alternative that the effect was different for those randomized to HIPP Intervention vs. Wellness Contact Control. In a similar past study,22 mean weekly minutes of physical activity at 6 months were 129.5 (SD=156.46) for those randomized to tailored print intervention, and 77.7 (SD=101.79) for those randomized to wellness contact control. With 40 participants randomized to each arm at baseline and a significance level α=0.05, we have 42% power to detect a similar difference in minutes of physical activity at 6 months. However, these calculations are provided as a formality as this is a feasibility study and such analyses are exploratory. The sample size will allow us to explore whether this new program shows promise of being successful with the intended population and estimate effect sizes for future power analyses.
Secondary aims include exploring potential intervention effects on functional exercise capacity, BMI, % body fat, waist circumference, and hormone levels at 6 and 12 months using repeated measures multivariate analyses of covariance. Regression analyses will be conducted to explore associations between changes in physical activity with changes in the outcomes noted above, as well as potential mediators (theoretical constructs directly targeted by the intervention) and moderators (e.g., education) of physical activity outcomes.
To examine potential molecular alterations that occur in the process of becoming physically active, analysis of differential gene expression from baseline to 6 months will be performed for all participants using GeneSpring software. We will focus our analysis on identifying genes whose expression has been significantly altered (either induced or repressed) consequent to physical activity change. Genes identified using this strategy will be further examined for gene ontology and/or coordinated regulation by the same or similar transcription mechanisms. Gene expression over time (up to 12 months) will also be analyzed using linear mixed model approaches, controlling for response category (“responders” and “non-responders”) and appropriate moderators, as described above. These exploratory analyses are designed to provide insight into the molecular alterations associated with physical activity that may ultimately impact cancer risk.
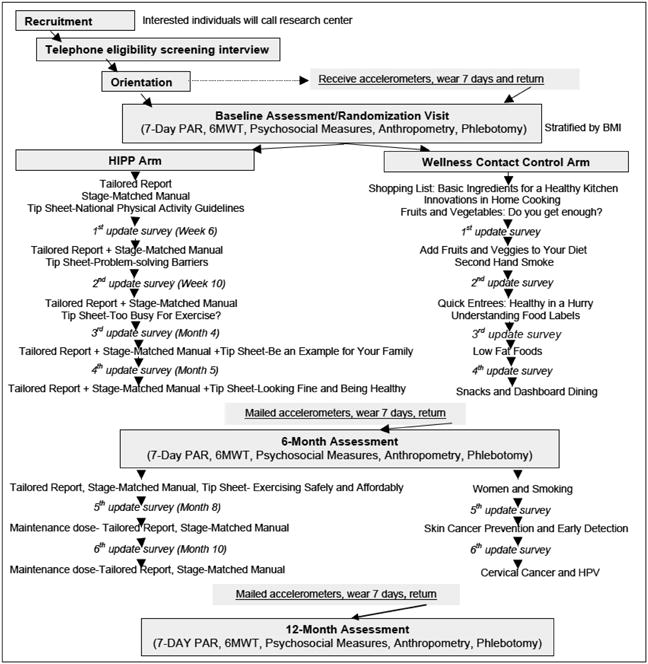
Results
Recruitment was completed in 12 months. A total of 185 individuals expressed interest in participation. Of these, 101 were not included in the study: 52 did not meet inclusion criteria, 8 declined to participate, and 41 were unable to be scheduled for an appointment. The remaining 84 participants were randomized: 43 to the HIPP intervention and 41 to the Wellness Contact Control arm. Figure 2 illustrates the CONSORT diagram. Participants are mostly obese, post-menopausal African American women living in Birmingham, AL area. The average age was 57 years old. Most reported full-time employment (60.7%) and at least some college level education (92.9%), with 53.6% of participants reporting household income under $50,000 per year. Please see Table 2 for demographic characteristics.
Figure 2. Consort Diagram.
Participants reported low levels of moderate intensity physical activity (M=41.5 minutes/week, SD=49.7) at baseline assessment, which was moderately correlated with accelerometer measured physical activity (Spearman's rho =.30, p=.068). As for psychosocial variables, most participants were in the contemplation and preparation stages of readiness for physical activity (94.1%) at baseline. While social support for exercise was low, perhaps even more so among friends (M=23.23, SD=11.87) than from family (M=25.95, SD=11.02, ranges for both subscales= 10-50, with higher scores indicating more support), participants described more pros than cons to participating in physical activity (based on decisional balance scores >0, M=2.06, SD=1.14). Moreover baseline levels of physical activity self-efficacy (M=2.98, SD=.98), cognitive (M= 3.45, SD= .82) and behavioral (M=3.12, SD= .69) processes of change related to physical activity, outcome expectations for physical activity participation (M=4.22, SD=.99, ranges= 1-5 for all 3 scales with high scores indicating better self-efficacy, processes of change and outcome expectations), and physical activity enjoyment (M=95.68, SD=22.88, range=18-126, higher scores indicating more enjoyment) appear promising. See Table 3 for baseline physical activity and related psychosocial variables.
Discussion
The HIPP study tests a home-based physical activity intervention for African American women residing in the Deep South. African American women report low levels of physical activity and are disproportionately burdened by associated cancers, particularly cancers of the breast and colon.1 The present study represents a low-cost, high-reach intervention to increase physical activity levels and reduce cancer risk among a traditionally underserved and difficult to reach population. Given the strong theoretical underpinnings and extensive formative research involved in the intervention design, we anticipate that the HIPP intervention will have a positive impact on the physical activity behaviors of the women participating in this study.
Baseline data from the HIPP study suggest that the participants are in need of intervention due to high rates of obesity and low levels of physical activity. The mean baseline 6 Minute Walk Distance for participants in the current study was 382 meters, whereas past studies found mean 6 Minute Walk Distances of 580 meters for 117 healthy men and 500 meters for 173 healthy women64 and 630 meters for 51 healthy older adults.65 Moreover, the high percent body fat and waist circumferences are concerning, given that larger waist sizes [>/=99.1 cm (39 in) and 101.6 cm (40 in) for women and men, respectively, similar to the mean found in the current study] have been associated with a two-fold increased risk of colon cancer.66
Scores on psychosocial measures indicate that most participants are in the pre-action phases of physical activity adoption (according to the Transtheoretical Model) and have low levels of social support for exercise. Given the HIPP intervention is designed to facilitate forward progression through the processes of change (i.e., from pre-action to action and maintenance stages) and enhance social support for physical activity, we hypothesize that improvements in these concepts will coincide with increased physical activity. Moreover, decisional balance, enjoyment, and outcome expectations scores indicate that the participants anticipate positive results from engaging in physical activity and will likely be receptive to this intervention. In fact, baseline scores on several psychosocial variables were higher than those found in similar past physical activity intervention studies among sedentary Latinas [mean self-efficacy= 2.34 (.079), enjoyment=87.17 (20.22), cognitive processes=2.45 (0.82), behavioral processes= 1.99 (0.61), social support from friends=14.93 (6.52), social support from family= 17.77 (7.60)]67 and mostly white participants [mean decisional balance= 0.25(12.69), self-efficacy=2.64 (0.76), behavioral processes=2.39 (0.58), cognitive processes= 2.90 (0.71)].68
While the study is still on-going, a wealth of information has already been collected regarding the feasibility of the program. Participant recruitment was completed in timely fashion; however, we note that the early stages of recruitment were not as prolific. Feedback from research staff indicated that exclusion criteria associated with weight status (i.e., BMI<40) and the presence of chronic diseases (i.e., high blood pressure, diabetes) were resulting in a substantial number of potential participants being deemed ineligible. After discussing these issues with the study physician, the research team concluded that it was safe to relax the eligibility criteria and allow individuals with a BMI of < 45 and controlled high blood pressure and/or diabetes (but not taking insulin) to enroll in the study. This avoided the unnecessary exclusion of potential participants given the frequency of these conditions among our target population (African American women between the ages of 50-69 years old in the Deep South). Moreover, it allowed women who were perhaps in the greatest need of physical activity intervention to enroll in the study and will increase the generalizability of our findings.
We have also learned that some recruitment channels were clearly better investments than others. Paid advertising on local radio stations produced disappointing results. In contrast, involving local churches in our recruitment efforts was instrumental. Once study flyers were distributed at local church services and health fairs and the study information was included in church announcements, websites, and bulletins, our accrual increased dramatically. Numerous other factors could have influenced the slow start for recruitment. For example, the protocol required multiple blood draws. Given past issues surrounding mistrust of research (i.e., “Tuskegee Incident”) in this region, researchers conducting future studies in this area should be mindful that endorsement from key opinion leaders might be necessary to facilitate participant enrollment.
A strength of the current study is the randomized controlled trial design. Other unique aspects include the at-risk population, automated system that provides the tailoring, along with the repeated assessments to ensure tailoring throughout the intervention period, and the collection of cancer-related biomarkers. As for limitations, our participants were community volunteers with relatively high education levels, which may limit the generalizability of the findings.
The current study is well positioned to examine acceptability, demand, and limited efficacy and will allow for comment on practicality and adaption. Future studies will be needed to address the other key areas of focus for feasibility studies highlighted by Bowen and colleagues (see Table 1). We may observe positive (and negative) effects on participants (e.g., improved physical activity) in the current study, and cost analyses of such individually tailored print-based physical activity interventions in mostly white populations69 already provide support for practicality. Moreover, comparing physical activity outcomes from past studies using similar interventions in different populations to findings with our participants will allow us to speak to adaption. If proven efficacious for increasing physical activity, long term goals of this line of research include implementation, integration, and potentially even expansion through public health departments, and healthcare-based networks, at which point the RE-AIM framework will be considered given its strengths for translating research into practice in real world settings. Moreover, mail-delivered intervention strategies may be well-suited to supplement and extend the ongoing community health worker efforts of the Deep South Network for Cancer Control, especially in hard to reach rural counties.
Transferring the delivery channel of the HIPP intervention to an even more cost-effective, interactive technology-based platform may also represent an important potential future direction. Formative research for the current study indicated that print was the preferred delivery channel in this target population. African Americans trail the national average in ownership of computers and broadband access at home and Internet use and is lowest in the South.70 Moreover, the research team frequently encountered no cell phone service while in the field conducting focus groups. However, the digital divide is shrinking, mostly due to a rapid uptake and adoption of smartphones and tablets among African Americans in recent years. 71 Recent physical activity studies using text messaging, social media, and websites were well-received by African American women. 72-75 While these studies are few in number and preliminary in nature, such findings bode well for the m-health future directions of this line of research.
Acknowledgments
This research was supported by the American Cancer Society (MRSG-13-156-01-CPPB) and the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR001417). We would like to thank collaborators Drs. David Allison and Mona Fouad for earlier contributions to this study. We thank Michelle Constant-Jones, Ashley Sineath, Amanda Burnside, Claudia Hardy, Tara Bowman, Jolene Lewis, and the staff at the Clinical Research Unit of the University of Alabama at Birmingham, as well as Rachelle Edgar of the University of California, San Diego for their valuable assistance with this project. Most importantly we thank our study participants for their time.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cancer Facts & Figures for African Americans 2009-2010. Atlanta: American Cancer Society; 2009. [Google Scholar]
- 2.Lee IM, Oguma Y. Physical Activity. In: Schottenfeld D, Fraumeni JF, editors. Cancer Epidemiology and Prevention. 3rd. New York: Oxford University Press; 2006. pp. 449–467. [Google Scholar]
- 3.Samad AK, Taylor RS, Marshall T, Chapman MA. A meta-analysis of the association of physical activity with reduced risk of colorectal cancer. Colorectal Dis. 2005;7(3):204–213. doi: 10.1111/j.1463-1318.2005.00747.x. [DOI] [PubMed] [Google Scholar]
- 4.Wolin KY, Yan Y, Colditz GA, Lee IM. Physical activity and colon cancer prevention: a meta-analysis. Br J Cancer. 2009;100(4):611–616. doi: 10.1038/sj.bjc.6604917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slattery ML. Physical activity and colorectal cancer. Sports Med. 2004;34(4):239–252. doi: 10.2165/00007256-200434040-00004. [DOI] [PubMed] [Google Scholar]
- 6.Ballard-Barbash R, Slattery ML, Thune L, Friedenreich CM. Obesity and body composition. In: Schottenfeld D, Fraumeni JF, editors. Cancer Epidemiology and Prevention. 3rd. New York: Oxford University Press; 2006. [Google Scholar]
- 7.Vainio H, Bianchini F. Weight control and physical activity. Lyon: IARC Press; 2002. [DOI] [PubMed] [Google Scholar]
- 8.Lynch BM, Neilson HK, Friedenreich CM. Physical Activity and Breast Cancer Prevention. In: Courneya KS, Friedenreich CM, editors. Physical Activity and Cancer: Recent Results in Cancer Research. New York: Springer; 2011. [DOI] [PubMed] [Google Scholar]
- 9.Friedenreich CM, Cust AE. Physical activity and breast cancer risk: impact of timing, type and dose of activity and population subgroup effects. Br J Sports Med. 2008;42(8):636–647. doi: 10.1136/bjsm.2006.029132. [DOI] [PubMed] [Google Scholar]
- 10.Friedenreich CM, Orenstein MR. Physical activity and cancer prevention: etiologic evidence and biological mechanisms. J Nutr. 2002;132(11 Suppl):3456S–3464S. doi: 10.1093/jn/132.11.3456S. [DOI] [PubMed] [Google Scholar]
- 11.Friedenreich CM. The role of physical activity in breast cancer etiology. Semin Oncol. 2010;37(3):297–302. doi: 10.1053/j.seminoncol.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Winzer BM, Whiteman DC, Reeves MM, Paratz JD. Physical activity and cancer prevention: a systematic review of clinical trials. Cancer Causes Control. 2011;22(6):811–826. doi: 10.1007/s10552-011-9761-4. [DOI] [PubMed] [Google Scholar]
- 13.Kushi LH, Byers T, Doyle C, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2006;56(5):254–281. doi: 10.3322/canjclin.56.5.254. quiz 313-254. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 15.Pekmezi D, Jennings EG. Interventions to promote physical activity among African Americans. American Journal of Lifestyle Medicine. 2009;3:173–184. [Google Scholar]
- 16.Banks-Wallace J, Conn V. Interventions to promote physical activity among African American women. Public Health Nurs. 2002;19(5):321–335. doi: 10.1046/j.1525-1446.2002.19502.x. [DOI] [PubMed] [Google Scholar]
- 17.Yancey AK, McCarthy WJ, Harrison GG, Wong WK, Siegel JM, Leslie J. Challenges in improving fitness: results of a community-based, randomized, controlled lifestyle change intervention. J Womens Health (Larchmt) 2006;15(4):412–429. doi: 10.1089/jwh.2006.15.412. [DOI] [PubMed] [Google Scholar]
- 18.Richter DL, Wilcox S, Greaney ML, Henderson KA, Ainsworth BE. Environmental, policy, and cultural factors related to physical activity in African American women. Women Health. 2002;36(2):91–109. doi: 10.1300/j013v36n02_07. [DOI] [PubMed] [Google Scholar]
- 19.Demark-Wahnefried W, Morey MC, Clipp EC, et al. Results of Project LEAD (Leading the Way in Exercise and Diet) - A trial testing an intervention of telephone-counseling and mailed materials in improving physical functioning among older breast and prostate cancer survivors. Journal of Clinical Oncology. 2005;23(16):763s–763s. [Google Scholar]
- 20.Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, Abrams DB. Using the stages of change model to increase the adoption of physical activity among community participants. Am J Health Promot. 1992;6(6):424–429. doi: 10.4278/0890-1171-6.6.424. [DOI] [PubMed] [Google Scholar]
- 21.Marcus BH, Lewis BA, Williams DM, et al. A comparison of Internet and print-based physical activity interventions. Arch Intern Med. 2007;167(9):944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- 22.Marcus BH, Napolitano MA, King AC, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychol. 2007;26(4):401–409. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 24.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 25.Pekmezi D, Marcus B, Meneses K, et al. Developing an intervention to address physical activity barriers for African-American women in the deep south (USA) Womens Health (Lond Engl) 2013;9(3):301–312. doi: 10.2217/whe.13.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Monninkhof EM, Velthuis MJ, Peeters PH, Twisk JW, Schuit AJ. Effect of exercise on postmenopausal sex hormone levels and role of body fat: a randomized controlled trial. J Clin Oncol. 2009;27(27):4492–4499. doi: 10.1200/JCO.2008.19.7459. [DOI] [PubMed] [Google Scholar]
- 28.Canadian Society for Exercise Physiology. PAR-Q and You. Gloucester, Ontario: Canadian Society for Exercise Physiology; 1994. [Google Scholar]
- 29.American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 30.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Family medicine. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 31.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121(1):91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 32.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122(5):794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 33.Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sloane R, Snyder DC, Demark-Wahnefried W, Lobach D, Kraus WE. Comparing the 7-day physical activity recall with a triaxial accelerometer for measuring time in exercise. Med Sci Sports Exerc. 2009;41(6):1334–1340. doi: 10.1249/MSS.0b013e3181984fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sports Exerc. 2003;35(5):801–809. doi: 10.1249/01.MSS.0000064941.43869.4E. [DOI] [PubMed] [Google Scholar]
- 36.Irwin ML, Ainsworth BE, Conway JM. Estimation of energy expenditure from physical activity measures: Determinants of accuracy. Obesity Research. 2001;9(9):517–525. doi: 10.1038/oby.2001.68. [DOI] [PubMed] [Google Scholar]
- 37.Johnson-Kozlow M, Sallis JF, Gilpin EA, Rock CL, Pierce JP. Comparative validation of the IPAQ and the 7-Day PAR among women diagnosed with breast cancer. Int J Behav Nutr Phys Act. 2006;3:7. doi: 10.1186/1479-5868-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leenders NYJM, Sherman WM, Nagaraja HN, Kien CL. Evaluation of methods to assess physical activity in free-living conditions. Med Sci Sport Exer. 2001;33(7):1233–1240. doi: 10.1097/00005768-200107000-00024. [DOI] [PubMed] [Google Scholar]
- 39.Leenders NYJM, Sherman WM, Nagaraja HN. Comparisons of four methods of estimating physical activity in adult women. Med Sci Sport Exer. 2000;32(7):1320–1326. doi: 10.1097/00005768-200007000-00021. [DOI] [PubMed] [Google Scholar]
- 40.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 Suppl):S1–205. [PubMed] [Google Scholar]
- 41.Wilkinson S, Huang CM, Walker LO, Sterling BS, Kim M. Physical activity in low-income postpartum women. J Nurs Scholarship. 2004;36(2):109–114. doi: 10.1111/j.1547-5069.2004.04022.x. [DOI] [PubMed] [Google Scholar]
- 42.Dunn AL, Garcia ME, Marcus BH, Kampert JB, Kohl HW, Blair SN. Six-month physical activity and fitness changes in Project Active, a randomized trial. Med Sci Sports Exerc. 1998;30(7):1076–1083. doi: 10.1097/00005768-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, 3rd, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. Jama. 1999;281(4):327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 44.Pekmezi DW, Williams DM, Dunsiger S, et al. Feasibility of using computer-tailored and internet-based interventions to promote physical activity in underserved populations. Telemed J E Health. 2010;16(4):498–503. doi: 10.1089/tmj.2009.0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Young DR, Stewart KJ. A church-based physical activity intervention for African American women. Fam Community Health. 2006;29(2):103–117. doi: 10.1097/00003727-200604000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Newton RL, Jr, Perri MG. A randomized pilot trial of exercise promotion in sedentary African-American adults. Ethn Dis. 2004;14(4):548–557. [PubMed] [Google Scholar]
- 47.Fitzgibbon ML, Stolley MR, Ganschow P, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc. 2005;97(10):1393–1402. [PMC free article] [PubMed] [Google Scholar]
- 48.Racette SB, Weiss EP, Obert KA, Kohrt WM, Holloszy JO. Modest lifestyle intervention and glucose tolerance in obese African Americans. Obes Res. 2001;9(6):348–355. doi: 10.1038/oby.2001.45. [DOI] [PubMed] [Google Scholar]
- 49.Janz KF. Validation of the CSA accelerometer for assessing children's physical activity. Med Sci Sports Exerc. 1994;26(3):369–375. [PubMed] [Google Scholar]
- 50.Melanson EL, Jr, Freedson PS. Validity of the Computer Science and Applications, Inc. (CSA) activity monitor. Med Sci Sports Exerc. 1995;27(6):934–940. [PubMed] [Google Scholar]
- 51.Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed) 1982;284(6329):1607–1608. doi: 10.1136/bmj.284.6329.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Solway S, Brooks D, Lacasse Y, Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 2001;119(1):256–270. doi: 10.1378/chest.119.1.256. [DOI] [PubMed] [Google Scholar]
- 53.Cahalin L, Pappagianopoulos P, Prevost S, Wain J, Ginns L. The Relationship of the 6-Min Walk Test to Maximal Oxygen-Consumption in Transplant Candidates with End-Stage Lung-Disease. Chest. 1995;108(2):452–459. doi: 10.1378/chest.108.2.452. [DOI] [PubMed] [Google Scholar]
- 54.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 55.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992;11(4):257–261. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 56.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992;11(6):386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 57.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 58.Resnick B, Zimmerman SI, Orwig D, Furstenberg AL, Magaziner J. Outcome expectations for exercise scale: utility and psychometrics. J Gerontol B Psychol Sci Soc Sci. 2000;55(6):S352–356. doi: 10.1093/geronb/55.6.s352. [DOI] [PubMed] [Google Scholar]
- 59.Kendzierski D, DeCarlo KJ. Physical Activity Enjoyment Scale: two validation studies. J Sport Exercise Psy. 1991;13(1):50–64. [Google Scholar]
- 60.Lukaski HC, Bolonchuk WW, Hall CB, Siders WA. Validation of tetrapolar bioelectrical impedance method to assess human body composition. J Appl Physiol (1985) 1986;60(4):1327–1332. doi: 10.1152/jappl.1986.60.4.1327. [DOI] [PubMed] [Google Scholar]
- 61.Newton RL, Jr, Alfonso A, York-Crowe E, et al. Comparison of body composition methods in obese African-American women. Obesity (Silver Spring) 2006;14(3):415–422. doi: 10.1038/oby.2006.55. [DOI] [PubMed] [Google Scholar]
- 62.Lahti-Koski M, Pietinen P, Heliovaara M, Vartiainen E. Associations of body mass index and obesity with physical activity, food choices, alcohol intake, and smoking in the 1982-1997 FINRISK Studies. Am J Clin Nutr. 2002;75(5):809–817. doi: 10.1093/ajcn/75.5.809. [DOI] [PubMed] [Google Scholar]
- 63.Riebe D, Blissmer BJ, Greaney ML, Garber CE, Lees FD, Clark PG. The relationship between obesity, physical activity, and physical function in older adults. J Aging Health. 2009;21(8):1159–1178. doi: 10.1177/0898264309350076. [DOI] [PubMed] [Google Scholar]
- 64.Miyamoto S, Nagaya N, Satoh T, et al. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. Comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2000;161(2 Pt 1):487–492. doi: 10.1164/ajrccm.161.2.9906015. [DOI] [PubMed] [Google Scholar]
- 65.Stevens D, Elpern E, Sharma K, Szidon P, Ankin M, Kesten S. Comparison of hallway and treadmill six-minute walk tests. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1540–1543. doi: 10.1164/ajrccm.160.5.9808139. [DOI] [PubMed] [Google Scholar]
- 66.Moore LL, Bradlee ML, Singer MR, et al. BMI and waist circumference as predictors of lifetime colon cancer risk in Framingham Study adults. Int J Obes Relat Metab Disord. 2004;28(4):559–567. doi: 10.1038/sj.ijo.0802606. [DOI] [PubMed] [Google Scholar]
- 67.Marcus BH, Hartman SJ, Pekmezi D, et al. Using interactive Internet technology to promote physical activity in Latinas: Rationale, design, and baseline findings of Pasos Hacia La Salud. Contemp Clin Trials. 2015 doi: 10.1016/j.cct.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Marcus BH, Napolitano MA, King AC, et al. Examination of print and telephone channels for physical activity promotion: Rationale, design, and baseline data from Project STRIDE. Contemp Clin Trials. 2007;28(1):90–104. doi: 10.1016/j.cct.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sevick MA, Napolitano MA, Papandonatos GD, Gordon AJ, Reiser LM, Marcus BH. Cost-effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Prev Med. 2007;45(1):54–61. doi: 10.1016/j.ypmed.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Spooner T. [Accessed October 6, 2011];Internet Use by Region in the United States. 2003 http://www.pewinternet.org/∼/media//Files/Reports/2003/PIP_Regional_Report_Aug_2003.pdf.pdf.
- 71.Pew Internet and American Life Project. Demographics of Internet Users. 2013. [Accessed January 5, 2013]. [Google Scholar]
- 72.Joseph RP, Casazza K, Durant NH. The effect of a 3-month moderate-intensity physical activity program on body composition in overweight and obese African American college females. Osteoporos Int. 2014 doi: 10.1007/s00198-014-2825-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Joseph RP, Keller C, Adams MA, Ainsworth BE. Print versus a Culturally-Relevant Facebook and Text Message Delivered Intervention to Promote Physical Activity in African American Women: A Randomized Pilot Trial. BMC Women's Health. 2015;15:30. doi: 10.1186/s12905-015-0186-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Joseph RP, Pekmezi DW, Lewis T, Dutton G, Turner LW, Durant NH. Physical activity and Social Cognitive Theory outcomes of an Internet-enhanced physical activity intervention for African American female college students. Journal of Health Disparities Research and Practice. 2013;6(2):18. [PMC free article] [PubMed] [Google Scholar]
- 75.Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informatics J. 2009;15(1):17–25. doi: 10.1177/1460458208099865. [DOI] [PMC free article] [PubMed] [Google Scholar]