Abstract
At present, one of greatest concerns of medical personnel is Zika virus (ZIKV). Though it has been reported for quite a long time, its rapid emergence, new modes of transmission, and more importantly, the congenital anomalies associated with it have made the situation worse. It was first detected in 1947. After that, this infection was found in the countries of Africa as well as Asia. At present, interestingly it has been reported from Brazil. Microcephaly and intracranial calcification have been postulated to be related to maternal infection with this virus. Though it is asymptomatic in maximum number of cases, the serious complications of the infection should be prevented at the earliest. No specific treatment and vaccine are available till now. But research continues and hopefully, success is not far off. The right information about this infection should reach patients as well as physicians. It will prevent unnecessary panic. In August, Brazil is going to organize the Olympic and Paralympic Games and all eyes are now focused on this. In this review article, the authors have tried to focus on the important points about this infection. The data were gathered after searching for relevant articles published in PubMed, the World Health Organization's (WHO) website, Centers for Disease Control and Prevention's (CDC) website, and some other related websites on the Internet.
Keywords: Aedes mosquitoes, microcephaly, pregnancy, Zika virus (ZIKV)
Introduction
The World Health Organization (WHO) declared a public health emergency of international concern (PHEIC) on February 1, 2016 as there were more than 4,000 microcephaly cases and neurological disorders in some areas affected by Zika virus (ZIKV).[1] Due to the rapid emergence of the ZIKV infection it is naturally becoming a concern all over the world. The single-stranded RNA arbovirus of Flavivirus genus was first identified in the Zika forest of Uganda and named accordingly.[2] In May 2015, it was first reported from Brazil.[3] Since then, it has rapidly become a significant problem in the medical field. In 1968, it was reported from Nigeria. From 1951 to 1981, infection due to this virus was documented from various African countries. At that time, such cases were also found in different countries of Asia.[4] In April 2007, there was an outbreak of ZIKV on Yap Island in the Federated States of Micronesia.[5] In 2013, another outbreak was reported in French Polynesia. From 2012 to 2014 in Thailand, some cases were identified to be affected by ZIKV.[6] Introduction of ZIKV in Easter Island in 2014 has been suggested to originate from French Polynesia in the literature.[7]
Similarities were found between the strains isolated from Thailand and the Pacific regions. It was postulated that might be a similar type of ZIKV prevalent among a large portion of the globe.[6] In the USA, most cases are related to travel and the first case of microcephaly was reported from Hawaii in January 2016.[8] In the past 6 weeks from 11 Feb, 2016, four cases have been documented in the UK.[9]
Transmission
ZIKV has been transmitted mainly by the bite of female Aedes mosquitoes.[10] Favorable environmental factors for these vectors may play a role in the rapid emergence of the infection in countries in the Americas.[2] Some reports blame El Niño and global warming that cause hot winters and summers, which help in spreading this virus. At the time of drought local people usually store water in the container, which is the ideal environment to help in the breeding of Aedes mosquitoes.[11] But the infection can be spread through sexual intercourse,[12] blood transfusion,[13] and perinatal transmission.[2] Regarding blood transfusion during an outbreak in French Polynesia, a significant number of asymptomatic donors’ blood was positive for ZIKV. So it may be a potential way of transmitting the disease.[13] In February 2016, a case of sexually transmitted ZIKV infection was reported from Texas, USA.[14]
Pathogenesis
The detailed pathogenesis is still unknown. Emerging evidence suggests that ZIKV after being injected through the skin, gains access initially to immature dendritic cells, dermal fibroblast, and epidermal keratinocytes. Adhesion factors such as DC-SIGN, AXL, Tyro3, and TIM-1 help entry in these cells.[15] With the help of envelope protein (E-protein), the virion attaches to the targeted cells. Then by the process of endocytosis with assistance from clathrin-coated pits, the virion enters the cytoplasm of the cells.[16] Replication occurs primarily in the cellular cytoplasm though ZIKV RNA has been isolated from the nucleus.[17] Then the cells undergo apoptosis and autophagy causing the release of virus particles, which ultimately spread to the lymphatics and blood stream leading to the florid manifestation of the disease. The host innate immune system produces type 1 and type 2 interferons to which ZIKV is susceptible.[15]
Clinical Feature
The incubation period of ZIKV infection is not known precisely. Most of the cases occur 3-12 days after mosquito bites.[18] A majority of ZIKV infections are asymptomatic. Mild fever, skin rashes, conjunctivitis (nonpurulent), muscle pain and joint pain (small joints of hands and feet), back pain, malaise, or a headache lasting for 2-7 days are seen only in 20% of infected individuals. Other possible manifestations include anorexia, retro-orbital pain, edema, diarrhea, constipation, abdominal pain, dizziness, and pruritus. It is indistinguishable from the symptoms of other arboviral diseases such as dengue and chikungunya.[16,19] Patients rarely become sick enough to get hospitalized, and mortality is rare.[20]
Diagnosis
At present, there is no commercial test to diagnose ZIKV. Viral RNA can be detected by reverse transcription-polymerase chain reaction (RT-PCR), and the antiviral antibodies can be detected by either immunoglobulin M (IgM) enzyme-linked immunosorbent assay (ELISA) or plaque reduction neutralization test (PRNT). IgM antibody appears in the blood toward the end of the first week of illness. Cross reaction with another Flavivirus is common. This cross-reaction effect can be attenuated by using PRNT.[21] Till date, there is no consensus about the superiority of one test over the other; so the Centers for Disease Control and Prevention (CDC) recommends performing both RT-PCR and serological test to diagnose congenital ZIKV infection. Serum from the umbilical cord or the infant within 2 days of birth is used for RT-PCR testing. Cerebrospinal fluid (CSF), placental tissue, and amniotic fluid can also be used for RT-PCR. The period of viremia is just about 3-5 days after onset of illness. ZIKV has been isolated from the saliva but did not help to extend the period of detection of the virus.[12] On the other hand, RNA can be isolated from urine even up to 3 weeks after the onset of symptoms, which is extremely advantageous in a practical scenario.[2] RT-PCR is positive only for 3-7 days. A negative result does not exclude the disease. Neutralizing antibody titers that are more than or equal to fourfold higher than dengue neutralizing antibody in the serum may be used in pregnant women (with or without symptoms). Other infections causing arthritis should be kept in mind. They are dengue, chikungunya, parvovirus, Rubella, measles, Leptospira, malaria, rickettsial infection, and Group A Streptococcus.[22]
ZIKV diagnosis can be performed by isolating it from mosquitoes and animals.[23]
Travelers returning from ZIKV-affected areas who are positive for dengue IgM antibody but negative dengue for IgG antibody on convalescent sera should be tested for ZIKV infection.[24] Recently, an individual with ZIKV infection was found to have false positive NS 1 dengue antigen.[25] So clinicians must be suspicious of the correct diagnosis of ZIKV infection.
Potential Complications
Recently, ZIKV infection has become a well-discussed topic for not only its rapidity of spread but also its effect on the neurological system that has been documented. Guillain–Barré syndrome has been found to be associated with ZIKV infection.[26]
Around 10,000 ZIKV cases were registered in October 2013. Among them, there were cases of meningoencephalitis and autoimmune thrombocytopenia-like complications.[27]
Recently, ZIKV infection in pregnant mothers was identified to be associated with microcephaly of newborn children.[28] This finding has no doubt stolen the focus to a significant extent. In Brazil, a cohort of 35 infants with microcephaly was investigated. They were born during from August 2015 to October 2015. In all cases, the mothers had lived in or had paid a visit to ZIKV-affected areas during pregnancy. A task force has already been developed in Brazil to study antenatal cases thoroughly. Data from one study in Brazil suggested that first-trimester ZIKV infection in pregnant women carries more risk of microcephaly.[28]
There are several causes of microcephaly. More data are required to provide any conclusive data.[29]
Apart from these, ophthalmological involvement is a less discussed topic regarding ZIKV. Infants from Brazil were found to have macular pigment mottling and loss of foveal reflex. One of them manifested well-defined macular atrophy as well.[30] Chorioretinal scarring and other ocular abnormalities in infants have been reported recently.[31] Also, recently ZIKV has been detected by the RT-PCR method by performing autopsy in the fetal brain with microcephaly. The mother had a history of living in the state of Reo Grande do Norte, and she left the place at 28 weeks of gestation. The neurotropic character of the virus was suggested as the virus was not found in other organs of the fetus.[32]
Treatment
There is no particular treatment for ZIKV infection. Supportive management is the only way. Taking rest, maintaining adequate hydration, and appropriate nutrition may help patients in early recovery. But patients must be kept under observation, and any signs of multiorgan involvement should be monitored. Acetaminophen may be used for relieving fever. Nonsteroidal anti-inflammatory drugs (NSAIDs) and aspirin should be used cautiously and after dengue infection (to avoid hemorrhagic complications) and pregnancy are ruled out. Till date, no vaccine is available.[19,20]
Prevention
The Pan American Health Organization (PAHO) has pointed out reasons for rapid spread of the virus:
The population of the Americas had no previous exposure to ZIKV and they have lack immunity, and
Aedes mosquitoes — The principle vector for ZIKV transmission — Are present in all of the region's countries except Canada and continental Chile.[33]
Its recommendations are as follows:[33]
Necessary reduction of the mosquito population.
Removal of potential breeding sites of mosquitoes.
Use of necessary personal protection.
People who live in or are going to visit susceptible areas have to use insect repellents and wear clothes covering the maximum body surface area.
Till date, there is no restriction in breastfeeding for the prevention of ZIKV transmission even though ZIKV RNA has been isolated from breast milk.[22]
The CDC has laid down guidelines for pregnant ladies [Figure 1].[34]
Figure 1.
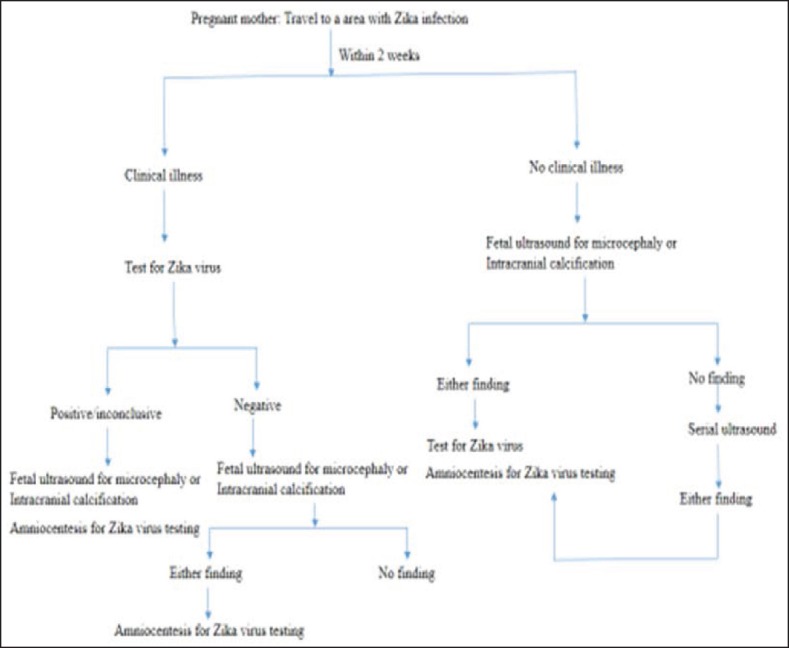
CDC recommendation for pregnant lady for ZIKV infection
All pregnant women who visit the ZIKV-affected regions should consult their doctors for further suggestions. All symptomatic women including those who develop symptoms within 2 weeks of their travel in a ZIKV-endemic zone should positively consult the health care provider. ZIKV remains in the blood of an infected person for 1 week and in the semen for 2 weeks. There is currently no evidence of birth defects in babies conceived after the clearance of the virus from the blood or semen.[35]
The CDC has also provided detailed guidelines for infants with and without microcephaly or other clinical features whose mothers have lived in or paid a visit to ZIKV-infected areas. Infants with congenital anomaly should be tested for ZIKV and reported accordingly. If no congenital anomaly is present, mothers should be evaluated. It is to be found out whether she has been screened during the antenatal period. If the mother is tested to be positive, then the infant is also tested for the virus.[21]
To reduce sexual transmission, the following have been recommended:[36]
Men who live in or have to visit a ZIKV-infected area should use condoms during sex with their pregnant partners.
They should also use condoms during sex with nonpregnant partners.
Both the partners should discuss the possibility of transmission of the infection, and they should consult experts when needed.
ZIKV can be detected in the semen when viremia is not present in blood even after 2 weeks.[12] So it is important to make more conclusive guidelines and provide sexual safety to people at risk.
Travelers returning from an area with ZIKV infection should be kept under surveillance for ZIKV infection.[37]
The CDC has also developed travel notifications so that more stringent follow-ups can be done.[38]
The Assistant Director General, World Health Organization (WHO) has recently (28 January, 2016) stated that countries in the dengue belt with Aedes aegypti should look for ZIKV and take measures to detect neurological conditions.[26]
Ongoing Researches on Zika
The National Institute of Allergy and Infectious Diseases is trying to find out antiviral drugs with actions against ZIKV. It is also working on Zika vaccine. A DNA-based vaccine with the same principle used for West Nile virus, a live attenuated ZIKV vaccine, and a genetically engineered vesicular stomatitis virus vaccine is being researched on. Hopefully, in 2016 we will be informed about the success in this field.[39] Animal models may be helpful for more information about the disease's course as well as treatment of ZIKV infection.[40] As the preventive methods such as removing the breeding areas and insecticide use are now proving insufficient, new approaches of genetically engineered mosquitoes are gaining importance.[41] A US scientist has predicted that it may take 2 years to develop a vaccine to be ready for testing and will take a decade to be available commercially.[42] One of the Indian biotechnology companies, Bharat Biotech, has reportedly claimed to develop two possible vaccines (recombinant and inactivated), which will be tested further in animal trials within a few weeks, (The article was accessed last on Feb 8, 2016).[43]
There are still some unknown facts about this virus. It is present in several body fluids such as the saliva and urine. But whether it can be transmitted by these is not known precisely. For this reason, countries have a ban on blood donations for 1 month after a visit to the affected countries. The ban may be longer if the individual develops symptoms.[44] Other unknown factors about pregnancy and Zika are whether there is any safe period during pregnancy when the infection will not affect the fetus. Another point is the clear-cut chance of transmission of the disease after the mosquito bite in pregnant lady, and the chance of occurrence of congenital anomaly is also not known precisely. We are waiting for the answers.[45]
2016 Olympic
Brazil is going to organize the Olympic and Paralympic Games in 2016 in Rio de Janeiro. The organizing committee has confirmed that it is following the guidelines of WHO for prevention of Zika infection. The International Olympic Committee (IOC) has provided athletes and national olympic committees with guidance about the prevention and symptoms of ZIKV.[46] But as the events are in August (cooler and drier weather), there are less chance of transmission through mosquitoes.[44] We are hopeful that the great event will be a huge success without any medical problem.
Current scenario regarding Zika in the USA (as of February 10, 2016):[45]
In the US states: Travel-related ZIKV disease cases-52, locally acquired mosquito-borne cases-0.
In US territories: Travel-related cases-1, locally acquired cases-9.[45]
Conclusion
Though there are several unknown facts about the pathogenesis, transmission, complications, and treatment of ZIKV, physicians should guide patients regarding prevention of the disease as much as possible. Particular care should be taken of pregnant women. The disease is asymptomatic in a majority of the cases. Affected patients should be kept under close observation. They should be counseled about the use of condoms and the risk of blood donations. Mosquito control measures should also be implemented stringently. Proper preventive methods will break the chain of transmission. Countries where other Aedes mosquito-borne diseases are endemic should be extremely cautious and have a thorough surveillance. In 2016, the vaccine of Zika is expected to arrive. If the current guidelines are followed properly, this infection can be combated successfully.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Public Health Emergency of International Concern (PHEIC) declared for Zika and clusters of microcephaly and neurological disorders. [Accessed February 11, 2016]; at: http://ecdc.europa.eu/en/activities/sciadvice/_layouts/forms/Review_DispForm.aspx?List=a3216f4c-f040-4f51-9f77-a96046dbfd72&ID=790#sthash.qs56bU0i.WCbWDCmx.dpuf . [Google Scholar]
- 2.Petersen E, Wilson ME, Touch S, McCloskey B, Mwaba P, Bates M, et al. Rapid spread of zika virus in the Americas-implications for public health preparedness for mass gatherings at the 2016 Brazil olympic games. Int J Infect Dis. 2016;44:11–5. doi: 10.1016/j.ijid.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Zanluca C, de Melo VC, Mosimann AL, Dos Santos GI, Dos Santos CN, Luz K. First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz. 2015;110:569–72. doi: 10.1590/0074-02760150192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayes EB. Zika virus outside Africa. Emerg Infect Dis. 2009;15:1347–50. doi: 10.3201/eid1509.090442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ioos S, Mallet HP, Leparc Goffart I, Gauthier V, Cardoso T, Herida M. Current Zika virus epidemiology and recent epidemics. Med Mal Infect. 2014;44:302–7. doi: 10.1016/j.medmal.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Buathong R, Hermann L, Thaisomboonsuk B, Rutvisuttinunt W, Klungthong C, Chinnawirotpisan P, et al. Detection of Zika virus infection in Thailand, 2012-2014. Am J Trop Med Hyg. 2015;93:380–3. doi: 10.4269/ajtmh.15-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tognarelli J, Ulloa S, Villagra E, Lagos J, Aguayo C, Fasce R, et al. A report on the outbreak of Zika virus on easter island, South Pacific, 2014. Arch Virol. 2015 doi: 10.1007/s00705-015-2695-5. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 8.State of Hawaii. DOH News Release: Hawaii Department of Health Receives Confirmation of Zika Infection in Baby Born with Microcephaly. [Accessed January 27, 2016]. at: http://governor.hawaii.gov/newsroom/doh-news-releasehawaii-department-of-health-receives-confirmation-ofzika-infection-in-baby-born-with-microcephaly/
- 9.O’Dowd A. UK records four cases of Zika virus in past six weeks. BMJ. 2016;352:i875. doi: 10.1136/bmj.i875. [DOI] [PubMed] [Google Scholar]
- 10.Zika virus transmission, Centers for disease control and prevention. [Accessed February 13, 2016]. at: http://www.cdc.gov/zika/transmission/index.html .
- 11.Parry L. ‘El Niño is to blame for the Zika outbreak’: Exceptionally hot and dry winter in Brazil triggered the crisis, say experts. [Accessed February 5, 2016]; at: http://www.dailymail.co.uk/health/article-3433996/El-Ni-o-blame-Zikaoutbreak-Exceptionally . [Google Scholar]
- 12.Musso D, Roche C, Nhan TX, Robin E, Teissier A, Cao-Lormeau VM. Detection of Zika virus in saliva. J Clin Virol. 2015;68:53–5. doi: 10.1016/j.jcv.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 13.Marano G, Pupella S, Vaglio S, Liumbruno GM, Grazzini G. Zika virus and the never-ending story of emerging pathogens and transfusion medicine. Blood Transfus. 2015:1–6. doi: 10.2450/2015.0066-15. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dallas County Health and Human Services. DCHHS Reports First Zika Virus Case in Dallas County Acquired Through Sexual Transmission. [Accessed February 3, 2016]. at: http://www.dallascounty.org/department/hhs/press/documents/PR2-2-16DCHHSReportsFirstCaseofZikaVirusThroughSexualTransmission.pdf .
- 15.Hamel R, Dejarnac O, Wichit S, Ekchariyawat P, Neyret A, Luplertlop N, et al. Biology of Zika virus infection in human skin cells. J Virol. 2015;89:8880–96. doi: 10.1128/JVI.00354-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sikka V, Chattu VK, Popli RK, Galwankar SC, Kelkar D, Sawicki SG, et al. The emergence of zika virus as a global health security threat: A review and a consensus statement of the INDUSEM Joint working Group (JWG) J Global Infect Dis. 2016;8:3–15. doi: 10.4103/0974-777X.176140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buckley A, Gould EA. Detection of virus-specific antigen in the nuclei or nucleoli of cells infected with Zika or Langat virus. J Gen Virol. 1988;69:1913–20. doi: 10.1099/0022-1317-69-8-1913. [DOI] [PubMed] [Google Scholar]
- 18.Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, Lanciotti RS, et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med. 2009;360:2536–43. doi: 10.1056/NEJMoa0805715. [DOI] [PubMed] [Google Scholar]
- 19.Zika virus, World health organization. [Accessed February 13, 2016]. at: http://www.who.int/mediacentre/factsheets/zika/en .
- 20.Zika virus: Symptoms, Diagnosis, and Treatment, Centers for disease control and prevention. [Accessed February 3, 2016]. at: http://www.cdc.symptoms/index.gov/zika/html .
- 21.Staples JE, Dziuban EJ, Fischer M, Cragan JD, Rasmussen SA, Cannon MJ, et al. Interim guidelines for the evaluation and testing of infants with possible congenital Zika virus infection-United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:63–7. doi: 10.15585/mmwr.mm6503e3. [DOI] [PubMed] [Google Scholar]
- 22.Sexton DJ. Zika virus infection. In: Hirsch MS, Lockwood CJ, Edwards MS, editors. UpToDate. 2016. [Accessed February 13, 2016]. at: http://www.uptodate.com/contents/zika-virusinfection . [Google Scholar]
- 23.Faye O, Faye O, Diallo D, Diallo M, Weidmann M, Sall AA. Quantitative real-time PCR detection of Zika virus and evaluation with field-caught mosquitoes. Virol J. 2013;10:311. doi: 10.1186/1743-422X-10-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.European Centre for Disease Prevention and Control. Rapid risk assessment: Zika virus infection outbreak, Brazil and the Pacific region – 25 May 2015. Stockholm: ECDC. 2015 Doi:10.1001/jamaophthalmol.2016.0284. [Google Scholar]
- 25.Gyurech D, Schilling J, Schmidt-Chanasit J, Cassinotti P, Kaeppeli F, Dobec M. False positive dengue NS1 antigen test in a traveller with an acute Zika virus infection imported into Switzerland. Swiss Med Wkly. 2016;146:w14296. doi: 10.4414/smw.2016.14296. [DOI] [PubMed] [Google Scholar]
- 26.Gatherer D, Kohl A. Zika virus: A previously slow pandemic spreads rapidly through the Americas. J Gen Virol. 2015 doi: 10.1099/jgv.0.000381. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 27.Samarasekera U, Triunfol M. Concern over Zika virus grips the world. Lancet. 2016;387:521–4. doi: 10.1016/S0140-6736(16)00257-9. [DOI] [PubMed] [Google Scholar]
- 28.Schuler-Faccini L, Ribeiro EM, Feitosa IM, Horovitz DD, Cavalcanti DP, Pessoa A, et al. Brazilian Medical Genetics Society-Zika Embryopathy Task Force. Possible association between Zika virus infection and microcephaly-Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:59–62. doi: 10.15585/mmwr.mm6503e2. [DOI] [PubMed] [Google Scholar]
- 29.Jampol LM, Goldstein DA. Zika virus infection and the Eye. JAMA Ophthalmol. 2016:1–8. doi: 10.1001/jamaophthalmol.2016.0284. [DOI] [PubMed] [Google Scholar]
- 30.Ventura CV, Maia M, Bravo-Filho V, Góis AL, Belfort R., Jr Zika virus in Brazil and macular atrophy in a child with microcephaly. Lancet. 2016;387:228. doi: 10.1016/S0140-6736(16)00006-4. [DOI] [PubMed] [Google Scholar]
- 31.de Paula Freitas B, de Oliveira Dias JR, Prazeres J, Sacramento GA, Ko AI, Maia M. Ocular findings in infants with microcephaly associated with presumed Zika virus congenital infection in Salvador, Brazil. JAMA Ophthalmol. 2016 doi: 10.1001/jamaophthalmol.2016.0267. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mlakar J, Korva M, Tul N, Popović M, Poljšak-Prijatelj M, Mraz J, et al. Zika virus associated with microcephaly. N Engl J Med. 2016 doi: 10.1056/NEJMoa1600651. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 33.Pan American Health Organization (PAHO), World Health Organization (WHO). PAHO Statement on Zika virus transmission and prevention. [Accessed February 13, 2016]. at: http://www.paho.org/hq/index.php?option=com_content&view=article&id=11605&Itemid=0&lang=en .
- 34.Petersen EE, Staples JE, Meaney-Delman D, Fischer M, Ellington SR, Callaghan WM, et al. Interim guidelines for pregnant women during a Zika virus outbreak-United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:30–3. doi: 10.15585/mmwr.mm6502e1. [DOI] [PubMed] [Google Scholar]
- 35.Question and Answers: Zika virus infection (Zika) and pregnancy. [Accessed February 13, 2016]. at: http://www.cdc.gov/zika/pregnancy/question-answers.html .
- 36.Oster AM, Brooks JT, Stryker JE, Kachur RE, Mead P, Pesik NT, et al. Interim guidelines for prevention of sexual transmission of Zika virus-United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:120–1. doi: 10.15585/mmwr.mm6505e1. [DOI] [PubMed] [Google Scholar]
- 37.Recognizing, Managing, and Reporting Zika Virus Infections in Travelers Returning from Central America, South America, the Caribbean, and Mexico. [Accessed February 13, 2016]. at: http://emergency.cdc.gov/han/han00385.asp .
- 38.Travel Health Notices. [Accessed February 13, 2016]. at: http://wwwnc.cdc.gov/travel/notices .
- 39.Zika virus. National Institute of Allergy and Infectious Disease. [Accessed February 13, 2016]. at: https://www.niaid.nih.gov/topics/zika/Pages/default.aspx .
- 40.Animal Models Helping to Combat Zika Virus by NABR (national association for biomedical research) [Accessed February 13, 2016]. at: http://www.nabr.org/animal-modelshelping-to-combat-zika-virus/
- 41.Pollackjan A. Jan 30, 2016. New Weapon to Fight Zika: The Mosquitohttp. [Accessed February 10, 2016]. at: http://www.nytimes.com/2016/01/31/business/new-weapon-to-fightzika-the-mosquito.html?_r=0 .
- 42.Cook J. (27 January 2016). “Zika virus: US scientists say vaccine ‘10 years away’-BBC News”. [Accessed January 28, 2016];BBC News. at: http://www.bbc.com/news/world-uscanada-35423288 . [Google Scholar]
- 43.Siddiqi Z. (3 February 2016). “Bharat Biotech says working on two possible Zika vaccines”. Reuters. [Accessed February 8, 2016]; at: http://in.reuters.com/article/health-zika-vaccineidINKCN0VC12U . [Google Scholar]
- 44.Gallagher J. Zika outbreak: What you need to know. 4 February 2016. [Accessed February 10, 2016]; at: http://www.bbc.com/news/health-35370848 . [Google Scholar]
- 45.Zika virus, Centers for disease control and prevention. [Accessed February 13, 2016]. at: http://www.cdc.gov/zika/index.html .
- 46.Rio 2016 following World Health Organisation advice on zica alert. [Accessed February 13, 2016]. at: http://www.rio2016.com/en/news/rio-2016-following-world-healthorganisation-advice-on-zica-alert .


