Abstract
Diabetic retinopathy (DR) is a growing concern in India. The first step in management of DR is timely screening. With 10% prevalence in rural India, 11 million people are likely to have DR by the year 2030. With limited resources and skilled manpower, it will not be possible to have routine eye examination to identify and treat these patients on a regular basis. Telemedicine is a possible answer in these situations where patients could be remotely screened and appropriately advised. With the advent of several technological advances such as low cost hand-held nonmydriatic camera, increased capabilities of the smartphones to take external eye and retinal photographs coupled with improving broadband connectivity; teleophthalmology in the management of DR could be a reality in the not too distant future.
Keywords: Diabetic retinopathy, India, rural, screening, telemedicine
Telemedicine is exchange of medical data by electronic telecommunication technology that allows patients’ medical problems evaluated and monitored by a remotely located physician.[1] Electronic medical record system has not only allowed creating a paperless office and easy to analyze collected data but also has created a platform to seek opinion from a specialist for decision-making and in data sharing. In addition, ophthalmology, in general, being highly image sensitive is particularly suited for telemedicine.
Diabetic retinopathy (DR) is unique for several inherent reasons for telemedicine. The diabetics take a variable length of time to developing manifest retinopathy and all manifest retinopathies are not vision-threatening for treatment. The yearly incidence of developing sight-threatening DR (STDR) in the Liverpool Diabetic Eye Study was 0.3% in the 1st year, rising to 1.8% by the 5th year, and the cumulative incidence of STDR was 3.9%.[2] The current estimated prevalence of STDR globally is 10.2% among diabetics.[3] It has been stated that DR develops in 4–7 years after onset of noninsulin-dependent DM.[4] Development of DR depends on several factors such as type and duration of DM, status of blood pressure, and serum lipid. Hence, it is advised that all diabetic patients receive a comprehensive eye examination including a dilated fundus examination. From a pure ophthalmologist point of view, it is impractical to examine all people with DM with the current limited trained manpower of both ophthalmologist and optometrists. Hence, it is the value of telemedicine in diabetics where the basic physical data and the fundus photograph are collected closer to patients’ habitat and opinion on the presence/absence of retinopathy, and the need for treatment is sought from a remotely located expert ophthalmologist.
Diabetic Retinopathy Fits into Screening Criteria
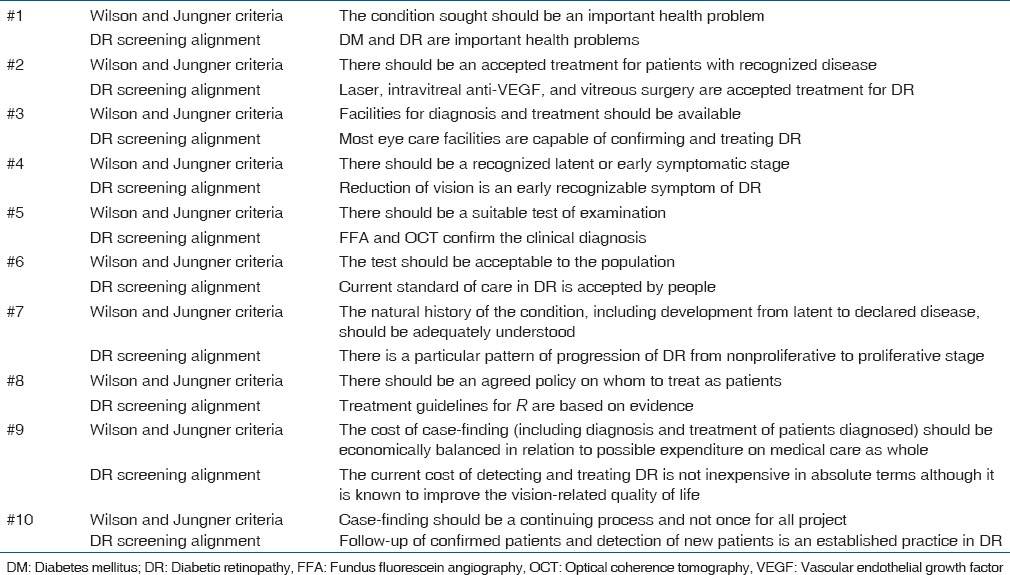
Wilson and Jungner[5] have defined 10 criteria for screening of chronic diseases such as DM and DR. These are listed in Table 1 along with the DR screening alignment.[6]
Table 1.
Wilson and Jungner screening criteria and diabetic retinopathy screening alignment
India has a Large Burden of Diabetic Retinopathy
DR is the leading cause of visual disability in diabetics. The reported prevalence of DR in India ranges from 17.6% to 28.2%.[7,8,9,10] With this prevalence, the number of people with DM is likely to increase to 79.4 million and people with DR is likely to increase to 22.4 million by the year 2030.[11] Both DM and DR are relatively less, between 10% and 12%, in rural India compared to urban India[12,13,14] but not small enough to ignore. Considering that prevalence of DR at a moderate level of 20% in urban India and at a lower level of 10% in rural India and assuming that 70% of Indians live in rural areas, the incidence of DR in rural India could rise to 10.97 million by the year 2030. In addition, there is an acute shortage of skilled manpower to screen DR in rural India. Traditionally, the two popular methods of DR screening are either ophthalmologist led or optometrist led. Both methods are effective and are used both in India and globally. However, with the large emerging burden, it may no longer be the cost effective method of DR screening. This is truer in rural India. Hence, a cost-effective DR screening is required in rural India, and this is possible with the existing and emerging technology of telemedicine.
Categories of Telemedicine
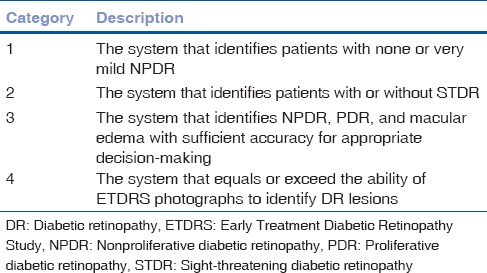
The American Telemedicine Association has described four categories of DR screening from identification of mild NPDR (Category 1) to the one that exceeds the ability of Early Treatment Diabetic Retinopathy Study photographs (Category 4) [Table 2].[15]
Table 2.
American Telemedicine Association diabetic retinopathy telescreening categories
DR screening is done by direct and indirect ophthalmoscopy and fundus photography. Fundus photography is more popular than ophthalmoscopy because it is more objective. It is also convenient because it does not need the ophthalmologist to be always present in the screening site; the stored photographs could be examined later, and when in doubt, could be confirmed with another expert. The technological improvements in fundus photography– from analog to digital, from 30° to 45° to 60° field in most digital cameras, and from mydriatic to nonmydriatic retinal cameras – have made the fundus photography as the most accepted form and standard of care in DR telescreening. In past, satellite connection has been used for transmission of the fundus photographs for teleconsultation. With improvement in internet and wire-free connection, the current generation of cameras is capable of transmitting the fundus images at fraction of cost incurred in the past.
Our Experience
We have established such a system of receiving the fundus photographs obtained in a hand-held nonmydriatic fundus camera placed at centers managing diabetes, and the images are both qualified and quantified for DR in the image reading center, L. V. Prasad Eye Institute Imaging Laboratory and Analysis Center (LILAC). Certified technicians grade the images and the specialist's opinion is sought in difficult ones. This has further reduced the ophthalmologist's time required to screen these patients. In a pilot study, the LILAC received fundus photographs of 229 diabetic subjects over 6 months; images of 32 subjects were ungradable (small pupil, lens opacities, etc.,) and 94 were diagnosed to having treatable DR (unpublished data). With increasing and powerful internet services planned in India, this method could be the most cost-effective method of DR telescreening in rural areas.
A few Indian studies have confirmed the superiority of fundus photography in teleophthalmology of DR care and good patient satisfaction.[16,17] Some Indian investigators have used the services of the Indian Space Research Organization designed teleophthalmology vehicles to transmit images from outreach locations to the DR reading and grading center at the base eye care facilities. While this facility may not be available to everyone and everywhere, the internet or cloud-based facility will be cost effective that delivers equally reliable information.
The current lacunae in telescreening of DR in India are lack of enough broadband capacity in India. A satellite transmission is preferred over an internet system.[6] As India is progressing in digital technology, we hope that this deficiency will be effectively addressed.
Future Direction
We foresee two important future developments; one, further miniaturization of fundus camera, superior picture quality, and reduced cost of the cameras; two, autodetection of fundus lesions in DR. This will empower and enable the patients for informed decision-making. Smartphones are increasingly used in ophthalmic screening.[18] There are many attempts currently made for autodetection of retinal lesions.[19] While we are on the threshold of witnessing a revolution in DR screening, the knowledge, attitude, and practice (KAP) toward diabetes and retinopathy needs considerable improvement (authors’ unpublished data). We are less likely to benefit from these disruptive technological unless the KAP also improves.
Conclusion
Prevalence of DR in rural India (or the world) is not too different than the urban people. However, the rural population is disadvantaged for not having a similar access to skilled personnel, particularly a specialist ophthalmologist similar to their urban counterpart. The modern technology of digital nonmydriatic photography, particularly the smartphones, fast expanding broadband transmission of these fundus pictures, and smarter autodetection of the retinal lesions will make the rural diabetic patients no more remain disadvantaged. The success of these new developments partly rests on similar improvement in the KAP of the rural folk.
Financial support and sponsorship
Hyderabad Research Foundation, Hyderabad, Telangana, India.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zimmer-Galler IE, Zeimer R. Telemedicine in diabetic retinopathy screening. Int Ophthalmol Clin. 2009;49:75–86. doi: 10.1097/IIO.0b013e31819fd60f. [DOI] [PubMed] [Google Scholar]
- 2.Younis N, Broadbent DM, Vora JP, Harding SP. Liverpool Diabetic Eye Study. Incidence of sight-threatening retinopathy in patients with type 2 diabetes in the Liverpool Diabetic Eye Study: A cohort study. Lancet. 2003;361:195–200. doi: 10.1016/s0140-6736(03)12267-2. [DOI] [PubMed] [Google Scholar]
- 3.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris MI, Klein R, Welborn TA, Knuiman MW. Onset of NIDDM occurs at least 4-7 yr before clinical diagnosis. Diabetes Care. 1992;15:815–9. doi: 10.2337/diacare.15.7.815. [DOI] [PubMed] [Google Scholar]
- 5.Wilson JM, Jungner G. Geneva: WHO; 1968. Principles and Practice of Screening for Disease. [Google Scholar]
- 6.Das T, Raman R, Ramasamy K, Rani PK. Telemedicine in diabetic retinopathy: Current status and future directions. Middle East Afr J Ophthalmol. 2015;22:174–8. doi: 10.4103/0974-9233.154391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dandona L, Dandona R, Naduvilath TJ, McCarty CA, Rao GN. Population based assessment of diabetic retinopathy in an urban population in Southern India. Br J Ophthalmol. 1999;83:937–40. doi: 10.1136/bjo.83.8.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V. Prevalence of diabetic retinopathy in urban India: The Chennai urban rural epidemiology study (CURES) eye study, I. Invest Ophthalmol Vis Sci. 2005;46:2328–33. doi: 10.1167/iovs.05-0019. [DOI] [PubMed] [Google Scholar]
- 9.Narendran V, John RK, Raghuram A, Ravindran RD, Nirmalan PK, Thulasiraj RD. Diabetic retinopathy among self reported diabetics in Southern India: A population based assessment. Br J Ophthalmol. 2002;86:1014–8. doi: 10.1136/bjo.86.9.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agarwal RP, Ranka M, Beniwal R, Gothwal SR, Jain GC, Kochar DK, et al. Prevalence of diabetic retinopathy in type 2 diabetics in relation to risk factors: Hospital based study. Int J Diabetes Dev Countries. 2003;23:16–9. [Google Scholar]
- 11.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Namperumalsamy P, Kim R, Vignesh TP, Nithya N, Royes J, Gijo T, et al. Prevalence and risk factors for diabetic retinopathy: A population-based assessment from Theni district, South India. Br J Ophthalmol. 2009;93:429–34. doi: 10.1136/bjo.2008.147934. [DOI] [PubMed] [Google Scholar]
- 13.Jonas JB, Nangia V, Khare A, Matin A, Bhojwani K, Kulkarni M, et al. Prevalence and associated factors of diabetic retinopathy in rural central India. Diabetes Care. 2013;36:e69. doi: 10.2337/dc12-2377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raman R, Ganesan S, Pal SS, Kulothungan V, Sharma T. Prevalence and risk factors for diabetic retinopathy in rural India. Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study III (SN-DREAMS III), report no 2. BMJ Open Diabetes Res Care. 2014;2:e000005. doi: 10.1136/bmjdrc-2013-000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Washington, DC, USA: American Telemedicine Association; 2011. American Telemedicine Association. Telehealth practice recommendations for diabetic retinopathy. [DOI] [PubMed] [Google Scholar]
- 16.Raman R, Rani PK, Mahajan S, Paul P, Gnanamoorthy P, Krishna MS, et al. The tele-screening model for diabetic retinopathy: Evaluating the influence of mydriasis on the gradability of a single-field 45 degrees digital fundus image. Telemed J E Health. 2007;13:597–602. doi: 10.1089/tmj.2006.0084. [DOI] [PubMed] [Google Scholar]
- 17.Kumari Rani P, Raman R, Manikandan M, Mahajan S, Paul PG, Sharma T. Patient satisfaction with tele-ophthalmology versus ophthalmologist-based screening in diabetic retinopathy. J Telemed Telecare. 2006;12:159–60. doi: 10.1258/135763306776738639. [DOI] [PubMed] [Google Scholar]
- 18.Bastawrous A, Rono HK, Livingstone IA, Weiss HA, Jordan S, Kuper H, et al. Development and validation of a smartphone-based visual acuity test (Peek Acuity) for clinical practice and community-based fieldwork. JAMA Ophthalmol. 2015;133:930–7. doi: 10.1001/jamaophthalmol.2015.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abràmoff MD, Niemeijer M, Suttorp-Schulten MS, Viergever MA, Russell SR, van Ginneken B. Evaluation of a system for automatic detection of diabetic retinopathy from color fundus photographs in a large population of patients with diabetes. Diabetes Care. 2008;31:193–8. doi: 10.2337/dc08-0952. [DOI] [PMC free article] [PubMed] [Google Scholar]


