Abstract
Total elbow arthroplasty (TEA) is utilized in the treatment of rheumatoid and post-traumatic elbow arthritis. TEA is a relatively low volume surgery in comparison to other types of arthroplasty and therefore little is known about current surgical utilization, patient demographics and complication rates in the United States. The purpose of our study is to evaluate the current practice trends and associated in-patient complications of TEA at academic centers in the United States. We queried the University Health Systems Consortium administrative database from 2007 to 2011 for patients who underwent an elective TEA. A descriptive analysis of demographics was performed which included patient age, sex, race, and insurance status. We also evaluated the following patient clinical benchmarks: hospital length of stay (LOS), hospital direct cost, in-hospital mortality, complications, and 30-day readmission rates. Our cohort consisted of 3146 adult patients (36.5% male and 63.5% female) with an average age of 58 years who underwent a total elbow arthroplasty (159 academic medical centers) in the United States. The racial demographics included 2334 (74%) Caucasian, 285 (9%) black, 236 (7.5%) Hispanic, 16 (0.5%) Asian, and 283 (9%) other patients. The mean LOS was 4.2±5 days and the mean total direct cost for the hospital was 16,300±4000 US Dollars per case. The overall inpatient complication rate was 3.1% and included mortality <1%, DVT (0.8%), re-operation (0.5%), and infection (0.4%). The 30-day readmission rate was 4.4%. TEA is a relatively uncommon surgery in comparison to other forms of arthroplasty but is associated with low in-patient and 30-day perioperative complication rate. Additionally, the 30-day readmission rate and overall hospital costs are comparable to the traditional total hip and knee arthroplasty surgeries.
Key words: Total elbow arthroplasty, United States, in-patient trend, complications, insurance, readmission
Introduction
Total elbow arthroplasty (TEA) is an effective procedure for the management of inflammatory and post-traumatic arthritis of the elbow as well as severely comminuted distal humerus fractures in low-demand individuals.1-4 TEA is a relatively uncommon arthroplasty procedure in comparison to other joints and therefore information regarding rates of utilization, costs, and complications from large nationwide databases are not widely available. Obtaining and understanding this information is important in an era of increasing cost conscious delivery of healthcare. A large, nationalized inpatient registry for TEA is on the rise. Several European registries exist for elbow arthroplasty.5,6 No large registry for TEA is available in the United States despite calls for such a registry. Previous analysis of TEA utilization and complication rates in the United States have been limited to sampling of either regional or national databases with limited information. Using the National Inpatient Sample database, Day et al.7 reported a 248% increase of the number of primary TEA from 1993 to 2007 which equates to a 6.4% annual procedure volume growth rate. However, their study did not report the associated costs, 30-day complication rates or the demographics of patients undergoing TEA. Gay et al.8 reported on the indications and reoperation rates for TEA in New York State. The largest previous cohort review occurred over a decade ago and included 3500 TEA’s between 1988 and 2005. Recent trends in the United States indicate an increase in the number of TEA procedures performed per year with a trend toward performing more procedures for trauma than for inflammatory arthritis.8,9 To our knowledge, there is no established national database studying the epidemiology and 30-day complication rates or outcomes of patients undergoing TEAs because majority of studies have been performed at single institutions with small numbers of patients. We isolated our study to TEA procedures performed at academic medical centers in United States between 2007-2011. Our study intends to evaluate the inpatient demographics, complications and readmission rate of patients after TEA in major academic centers across the United States.
Materials and Methods
A national administrative database of academic medical centers that tracks patients and hospital specific outcomes was used to characterize in-patient trends and complications. The University Health Systems Consortium (UHC) is an alliance of the nation’s leading nonprofit academic medical centers with 159 academic medical centers and 261 affiliated hospital members. UHC membership includes more than 90% of the non-profit academic medical centers in the United States. It provides patient, hospital, and financial outcomes across different centers. The data in the UHC database is primarily acquired from submitted UB-04 billing forms, similar to the forms submitted by hospitals for reimbursement on a variety of disease conditions and surgical treatments.
The UHC clinical data base resource manager (CDB/RM) provides the following information: synthetic hospital and surgeon identifiers, including specialty, unique patient visit identifiers, patient demographics, financials, procedurals, and diagnostic information. Morbidity and complication data are compiled from the UHC morbidity profiler. Both cost and charge information is reported in CDB/RM. Charges are reported by each center and costs are calculated using institution-specific cost-to-charge ratios obtained from the department-level Medicare cost reports. Federally reported area wage indices are used to account for regional- and center-specific cost variations that are not directly attributable to a center. The UHC severity of illness score is a validated measurement tool for both risk adjustment and predicted resource allocation. The UHC severity of illness score takes into account several health-related patient variables including medical comorbidities, age, and other relevant diagnoses.10 We queried the UHC administrative database from 2007 to 2011 for adult patients ≥18 who underwent an elective TEA. Elective total elbow arthroplasty was defined by the type of admission (elective) and International Classification of Diseases book 9, and clinical modification procedural codes (81.84). A descriptive analysis of demographics was performed which included patient age, sex, race, and insurance status (private, Medicaid, Medicare, government, and other). The outcomes of interest were perioperative morbidity, hospital length of stay (defined as the interval from the date of procedure to the date of discharge), hospital direct cost, index hospitalization survival, complications or inpatient mortality, and 30-day read-mission rate. Cost was defined as an expense that could be directly traced to the care of a patient, whether it was services or supplies rendered.
Results
Between 2007 and 2011, 3146 TEAs were performed and queried from the UHC administrative database from 159 different academic medical centers across the USA. The mean and standard deviation of surgical volume for individual surgeons was 7±5 TEA performed annually. The average patient age was 58 years old. 64% of patients were female (Figure 1A). Of the 3146 total elbow arthroplasties, the majority of the cohort 2334 patients (74%) were white, 285 (9%) were black, 236 (7.5%) were Hispanic, 16 (0.5%) were Asian, and 9% were other or unknown. Overall, 51% of the cohort had private insurance, 41% had Medicare, and 8% had Medicaid (Figure 1B). At least 70% of the cohort had one or more chronic medical condition. The average length of stay post-surgery was 4.23 days (Figure 2A). The mean total direct cost for the hospital was 16,300±4000$ per case (Figure 2B). In hospital mortality was less than 1% during the index hospitalization. The overall complication rate was 3.1% includes DVT (0.8%), re-operation (0.5%), and infection (0.4%) (Figure 2C). The 30-day readmission rate was 4.4%.
Figure 1.
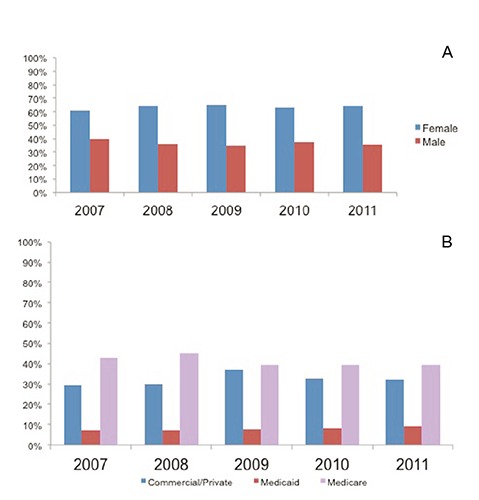
A) Gender demographics and B) insurance demographics of total elbow arthroplasty patients in the United States.
Figure 2.

Average length of stay (A), cost (B) and complication rates (C) of total elbow arthroplasty patients in the United States.
Discussion
Total elbow arthroplasty is an effective procedure for the treatment of patients with long standing rheumatoid arthritis and other degenerative conditions of the elbow and acute trauma. However, as the results of this study show, it is a relatively uncommon in surgery with only 3146 TEA’s performed over a 5 year period in comparison to higher volume arthroplasty such as total knee arthroplasty which is performed at a rate of 700,000 annually in the United States. As such, the information regarding TEA utilization, demographics, cost and complications are limited. Our study found a steady increase in the number of TEA procedures performed in the United States from 2007 to 2011 at around 600 to 700 TEA per year. Day et al.7 reported the number of TEAs performed in the United States increased at a rate of 6.4% in annual procedural volume and 7.6% in annual growth between 1993 to 2007. A recent study analyzing the Norwegian Arthroplasty Registry found a decreased number of TEAs performed per year in that particular country. The report indicated an increase in the number of TEAs performed for traumatic conditions, however the overall number of procedures decreased by 50% from 1994 to 2006.11 The overall decrease in TEA volume is thought to be related to the decreased number of symptomatic rheumatoid arthritis patients as a result of advances in medical management, specifically the introduction of immune modulating or suppression medications such as TNF (tumor necrosis factor) inhibitors. In 1994, Kraay et al.12 reported 80% of total elbow arthroplasties in their series were performed secondary to rheumatoid arthritis. In contrast to the above studies, Gay et al.8 using New York State Department of Health database, found a 44% increase in the number of total elbow arthroplasties performed per year. Their study showed a decreasing trend in the number of rheumatoid arthritis patients, but this decrease in number was offset by a 132% increase in the number of total elbow arthroplasty procedures performed for trauma or elbow fracture diagnosis.
In our study, the most common group of patients undergoing total elbow arthroplasty is primarily white females, which is consistent with previous epidemiological studies.9 This is likely related to increased number of osteoporotic traumatic elbow fractures seen in this patient population. The average age of 58 years old in our study is also similar to what is reported in the literature.8 Our database found the annual surgical volume for individual surgeons who performed total elbow arthroplasties was 7±5 procedures. Given the overall low volume of TEA surgery, we were unable to evaluate any correlation between surgeon experience and outcomes or complications. Though previous studies have found differences in complication rates at 6.8% for inexperienced surgeons compared to 2.8% for experienced surgeons.8 The average length of stay (LOS) was 4.23 days and did not vary significantly during the time period studied. The average LOS indicates that acute post-surgical recovery can be a difficult and lengthy process for these patients that include pain control, physical and occupational therapy, and rehab placement. In our study, approximately half of the patients had Medicare and/or Medicaid; the other half was comprised of private (32.3%), military (1%), worker’s compensation (6.7%), and self-pay (8.6%). The average cost of total elbow arthroplasty including hospital stay was 16,300±4000$. Day et al. reported the average hospital charges in 2007 for a TEA in the United States was $51,970 (range of $46,338 to $57,601) including a surgeon’s fee of $1524 (range of $1228 to $1842).7 The difference in cost between this database study and the above reported values is likely due to the location, type of charges reported and hospital systems.
Common complications of total elbow arthroplasty reported in clinical studies include ulnar neuropathy (up to 40%), aseptic loosening (7-15%), periprosthetic fracture (5-29%), implant failure, infection (3-8%), triceps insufficiency (2-8%) and instability.1,2,4,8,13-16 The Coonrad-Morrey total elbow prosthesis (Zimmer, Warsaw, IN, USA) is one of the most commonly used semi-constrained devices. Previous studies have reported >80% of the patients had good to excellent results, which was associated with good elbow function and pain relief. In our study, the overall inpatient and 30-days complication rate associated with TEA is 3.1%. The rate of deep vein thrombosis is 0.8%, re-operation is 0.5% and infection is 0.4%. The 30-day re-admission rate is4.4%. In comparison to other cohorts of hip fracture and arthroplasty patients, previous studies on post-operative hip fracture patients, the 28 day re-admission rate was 11.8% and the most common causes were pneumonia (27.3%), dehydration and renal dysfunction (18.2%) and deteriorating mobility (18.2%).17 In the total hip arthroplasty population, previous studies have shown the 28 day readmission rate to be 8.5% and the main reasons for re-admission to include thromboembolic disease (2.5%), atraumatic dislocation (1.4%), wound complications (1.2%) and post operative swelling (1.8%)18. Frankle et al. reported of a 12% readmission rate in patients who had a total elbow arthroplasty for comminuted distal humerus fractures.19 Our reported 0.8% rate of deep venous thrombosis is consistent with previous reports of 0.3% rate of pulmonary emboli in patients who have undergone a total elbow arthroplasty.8 We found an in-hospital infection rate of 0.4% which likely only accounts for acute post-operative infections. Reported long-term infection rates range from 0 to 8.3% with higher rates in patients with inflammatory arthritis.2-4,8,12,20-23 The causes of readmission should be identified and addressed in future studies to improve total elbow arthroplasty outcomes. Overall, there are many inconsistencies in the literature for total elbow arthroplasty with a lack of standardization in outcome measures.24 Commonly cited functional outcomes include the Mayo Elbow Performance Score, the Dash score, SF-36 score, and the HSS scoring system for total elbow arthroplasty. We were unable to gather any long-term data including functional outcomes and pain scores from the University Health Systems Consortium database. Reported long-term complication rates in the existing literature range from <1-41.7%.1,2,4,8,13-16 Our inpatient short-term 30-day complication rate of 3.1% is similar to a report of <1% perioperative complications in a study of 3617 patients by Cook et al.9 These low complication rates may reflect technical improvements of implants or of improved surgical experience in surgeons who work at academic centers. According to a review of a New York State registry, Gay et al.8 reported that less than 10% of TEAs were performed by experienced surgeons. Given the paucity of outcomes data for TEA in the literature, the authors feel that there is a need for a national total elbow registry to collect uniform indications for surgery, functional outcomes and complication data.
There are several limitations of our study inherent to a retrospective review of an inpatient multicenter database. Our data is subject to reporting bias and we do not have information regarding indications for surgery or reasons for readmission. Additionally, we are unable to gather outcomes data or report the rate of certain pertinent complications related to TEA such as post-operative ulnar neuropathy and instability.20,25 Additionally, there is no data present from the UHC that describes the type of implants utilized (type of constraint or manufacturer) or the level of experience of the attending surgeon performing the procedure. Riedel et al.24 stated that there is a lack of consensus among published total elbow arthroplasty papers that makes it difficult to compare long term outcomes. In order for comparison across current studies that exist and for future data gathering purposes, it is important to report a universally accepted outcome score that focuses on epidemiology, pain, function, and complication rates.
Conclusions
Total elbow arthroplasty performed in United States university medical centers is associated with low in patient complication rates that include DVT 0.8%, re-operation 0.5%, and infection 0.4%. 4.4% of patients were readmitted to the hospital within 30 days of the index procedure. The overall 30-day complication rate is 3%. The average hospital stay is 4 days with a total cost of 16,300±4000$ per case. White females represent the vast majority of patients undergoing total elbow arthroplasty and private insurance or Medicare typically pays for the procedures. Future studies should focus on indications for total elbow arthroplasty with specific outcome scores reported in order to universally apply data to future cases.
References
- 1.Shi LL, Zurakowski D, Jones DG, et al. Semiconstrained primary and revision total elbow arthroplasty with use of the Coonrad-Morrey prosthesis. J Bone Joint Surg Am 2007;89:1467-75. [DOI] [PubMed] [Google Scholar]
- 2.Aldridge JM, 3rd, Lightdale NR, Mallon WJ, Coonrad RW. Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis. A 10- to 31-year survival analysis. J Bone Joint Surg Br 2006;88B:509-14. [DOI] [PubMed] [Google Scholar]
- 3.Hildebrand KA, Patterson SD, Regan WD, et al. Functional outcome of semicon-strained total elbow arthroplasty. J Bone Joint Surg Am 2000;82A:1379-86. [DOI] [PubMed] [Google Scholar]
- 4.Schneeberger AG, Meyer DC, Yian EH. Coonrad-Morrey total elbow replacement for primary and revision surgery: a 2- to 7.5-year follow-up study. J Shoulder Elbow Surg 2007;16:S47-54. [DOI] [PubMed] [Google Scholar]
- 5.Rahme H, Jacobsen MB, Salomonsson B. The Swedish Elbow Arthroplasty Register and the Swedish Shoulder Arthroplasty Register: two new Swedish arthroplasty registers. Acta Orthop Scand 2001;72:107-12. [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen JV, Olsen BS, Fevang BT, et al. A review of national shoulder and elbow joint replacement registries. J Shoulder Elbow Surg 2012;21:1328-35. [DOI] [PubMed] [Google Scholar]
- 7.Day JS, Lau E, Ong KL, et al. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg 2010;19:1115-20. [DOI] [PubMed] [Google Scholar]
- 8.Gay DM, Lyman S, Do H, et al. Indications and reoperation rates for total elbow arthroplasty: an analysis of trends in New York State. J Bone Joint Surg Am 2012;94:110-7. [DOI] [PubMed] [Google Scholar]
- 9.Cook C, Hawkins R, Aldridge JM, 3rd, et al. Comparison of perioperative complications in patients with and without rheumatoid arthritis who receive total elbow replacement. J Shoulder Elbow Surg 2009;18:21-6. [DOI] [PubMed] [Google Scholar]
- 10.Shaw JJ, Santry HP, Shah SA. Specialization and utilization after hepatectomy in academic medical centers. J Surg Res 2013;185:433-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fevang BT, Lie SA, Havelin LI, et al. Results after 562 total elbow replacements: a report from the Norwegian Arthroplasty Register. J Shoulder Elbow Surg 2009;18:449-56. [DOI] [PubMed] [Google Scholar]
- 12.Kraay MJ, Figgie MP, Inglis AE, et al. Primary semiconstrained total elbow arthroplasty. Survival analysis of 113 consecutive cases. J Bone Joint Surg Br 1994;76B:636-40. [PubMed] [Google Scholar]
- 13.Little CP, Graham AJ, Karatzas G, et al. Outcomes of total elbow arthroplasty for rheumatoid arthritis: comparative study of three implants. J Bone Joint Surg Am 2005;87A:2439-48. [DOI] [PubMed] [Google Scholar]
- 14.Morrey BF, Adams RA. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J Bone Joint Surg Am 1992;74A:479-90. [PubMed] [Google Scholar]
- 15.Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J Bone Joint Surg Am 1998;80:1327-35. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg SH, Urban RM, Jacobs JJ, et al. Modes of wear after semiconstrained total elbow arthroplasty. J Bone Joint Surg Am 2008;90:609-19. [DOI] [PubMed] [Google Scholar]
- 17.Khan MA, Hossain FS, Dashti Z, Muthukumar N. Causes and predictors of early re-admission after surgery for a fracture of the hip. J Bone Joint Surg Br 2012;94A:690-7. [DOI] [PubMed] [Google Scholar]
- 18.Cullen C, Johnson DS, Cook G. Re-admission rates within 28 days of total hip replacement. Ann R Coll Surg Engl 2006;88:475-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frankle MA, Herscovici D, Jr., DiPasquale TG, et al. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. J Orthop Trauma 2003;17:473-80. [DOI] [PubMed] [Google Scholar]
- 20.Cesar M, Roussanne Y, Bonnel F, Canovas F. GSB III total elbow replacement in rheumatoid arthritis. J Bone Joint Surg Br 2007;89:330-4. [DOI] [PubMed] [Google Scholar]
- 21.Gschwend N, Simmen BR, Matejovsky Z. Late complications in elbow arthroplasty. J Shoulder Elbow Surg 1996;5:86-96. [DOI] [PubMed] [Google Scholar]
- 22.Jeon IH, Morrey BF, Anakwenze OA, Tran NV. Incidence and implications of early postoperative wound complications after total elbow arthroplasty. J Shoulder Elbow Surg 2011;20:857-65. [DOI] [PubMed] [Google Scholar]
- 23.Wolfe SW, Figgie MP, Inglis AE, et al. Management of infection about total elbow prostheses. J Bone Joint Surg Am 1990;72:198-212. [PubMed] [Google Scholar]
- 24.Riedel K, Beaton DE. Update on the state of outcome measurement in total elbow arthroplasty research: identifying a need for consensus. J Bone Joint Surg Am 2013;95A:e97 1-8. [DOI] [PubMed] [Google Scholar]
- 25.McKee MD, Veillette CJ, Hall JA, et al. A multicenter, prospective, randomized, controlled trial of open reduction—internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elbow Surg 2009;18:3-12. [DOI] [PubMed] [Google Scholar]


