Abstract
Dislocation of the hip is a well-described event that occurs in conjunction with high-energy trauma or postoperatively after total hip arthroplasty. Bigelow first described closed treatment of a dislocated hip in 1870, and in the last decade many reduction techniques have been proposed. In this article, we review all described techniques for the reduction of hip dislocation while focusing on physician safety. Furthermore, we introduce a modified technique for the reduction of posterior hip dislocation that allows the physician to adhere to the back safety principles set for by the Occupational Safety and Health Administration.
Key words: Dislocation, safety, review, technique, maneuver
Introduction
Dislocation of the hip is a well-described event that occurs in conjunction with high-energy trauma or postoperatively after total hip arthroplasty. Hip dislocations are commonly classified according to the direction of the dislocation of the femoral head, either anterior or posterior. Generally, closed reduction is the initial method for treatment and usually occurs in the emergency department (ED). Native hip dislocation necessitates emergent reduction because of the concern for chondrolysis.1 Bigelow first described closed treatment of a dislocated hip in 1870,2-4 and in the last decade many reduction techniques have been proposed.5-25 Each method has unique advantages and disadvantages.
Anterior hip dislocation is commonly reduced by in-line traction and external rotation, with an assistant sometimes pushing on the femoral head or pulling the femur laterally to assist reduction.19 For the most common dislocation, the posterior dislocation, Allis described the commonly used method: applying longitudinal traction with internal rotation to the hip.18 In this article, we review all published techniques for reduction of hip dislocation and offer a new technique for posterior hip dislocation that offers increased compliance with back safety recommendation by the Occupational Safety and Health Administration (OSHA) and allows the physician to stay low and stable when entering the bed with the patient.
Methods
We conducted a systematic review of publications on the reduction of hip dislocations. An initial search of the MEDLINE database provided a basis for the articles on reduction of the hip. We also conducted extensive manual searches of major orthopedic journals, major orthopedic texts relating to hip dislocations, and bibliographies of the previously found orthopedic texts and books to find relevant articles. We reviewed each article to ensure it described detailed reduction maneuvers or introduced a novel maneuver. We then reproduced and evaluated the techniques and made each into a line drawing for display. We also systematically reviewed OSHA workplace safety articles and policies for incorporation into the discussion.
Maneuvers
While there are many details and particulars to reducing hips, this article provides a brief overview and illustration of the methods described in the literature. Prereduction roentgenograms are necessary to clearly diagnose the dislocation and look for concomitant injury. In each case, intravenous sedation is usually required for patient comfort and to relax the large muscles surrounding the hip.
Reduction of posterior dislocations
For posterior dislocations, the principles of reduction are flexion, internal rotation, and adduction of the hip. Each of the maneuvers described below uses these principles as the basis of their mechanics.
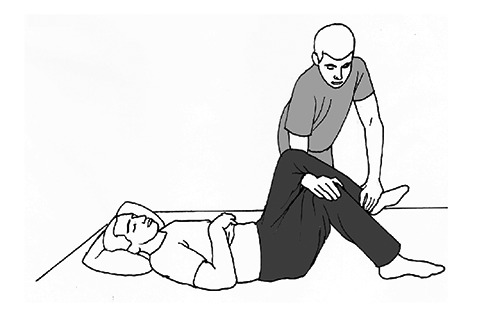
Allis maneuver
The patient is placed in the supine position, and the physician usually enters the bed with the patient; however, standing beside the bed is advised. The surgeon grasps the ipsilateral leg at the knee and flexes the knee to 90 degrees. While an assistant stabilizes the pelvis against the bed, the physician applies traction in line with the femur while flexing the hip up to 90 degrees by grasping the patient’s knee (Figure 1). According to Allis’s original description, no rotation is performed. As the hip reduces, the physician gently extends the hip and externally rotates the leg to allow the femoral head to enter the acetabulum.18
Figure 1.
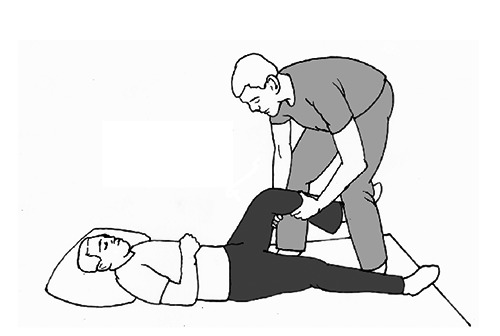
Allis maneuver.
Bigelow maneuver
The patient is placed in the supine position. The physician grasps the ankle of the affected leg with one hand and places his/her opposite forearm under the patient’s knee. The hip is flexed to 90 degrees, ensuring the affected leg is kept in an adducted and internally rotated position (Figure 2). While an assistant stabilizes the pelvis with downward pressure, the physician applies traction in line of the femur while abducting, externally rotating, and extending the affected hip.2-4 The preferred method for physician safety is to perform this maneuver while standing at the side of the bed; however, at times, entering the bed is a necessity.
Figure 2.
Bigelow maneuver.
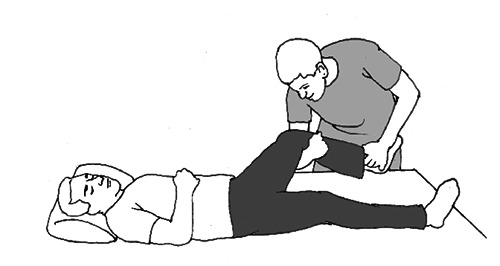
Lefkowitz maneuver
Described in 1993, this technique calls forthe patient to be placed in the supine position on the gurney. The physician stands on the affected side, placing his/her knee closest to the hip under the patient’s ipsilateral knee in the popliteal fossa and placing his/her foot on the gurney. The physician then flexes the patient’s leg over his/her knee by applying a downward force on the patient’s lower leg until the hip is reduced. One of the physician’s hands is on the patient’s lower anterior thigh and the other hand applies the downward force at the patient’s ankle (Figure 3).6
Figure 3.

Lefkowitz maneuver.
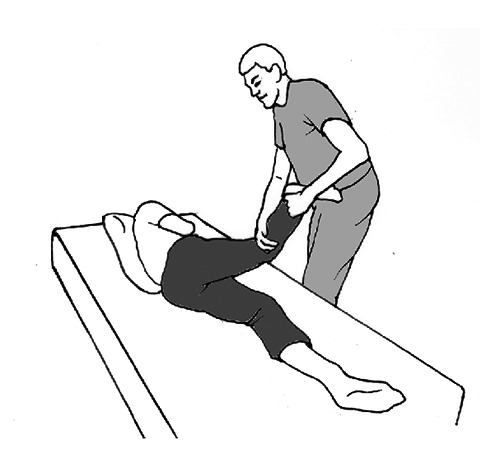
Captain Morgan maneuver
Described in 2011, this technique calls for the patient to behe patient is placed in the supine position on a backboard on a gurney with the pelvis strapped to the board. The physician stands on the side of the gurney of the affected hip and places his/her foot closest to the hip on the backboard and flexes the patient’s affected leg over his/her own thigh, close to popliteal fossa. The physician grasps the ankle of the affected leg with one hand and places the opposite hand underneath the patient’s affected knee. The physician then plantar flexes his/her own foot under the patient’s affected leg while applying upward traction with the hand behind the affected knee (Figure 4). Internal and external rotation, adduction, and abduction can be applied using the hand grasping the ankle until reduction is achieved. The differences between this maneuver and the Lefkowitz maneuver include use of a backboard and the hand being placed under the patient’s knee, not on the lower anterior thigh.20
Figure 4.
Captain Morgan maneuver.
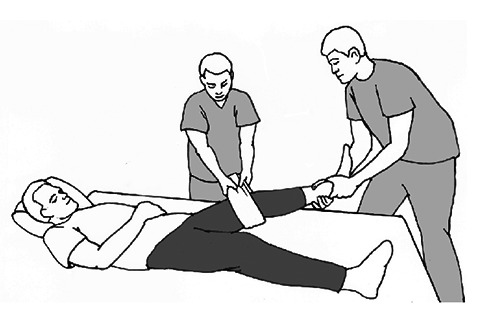
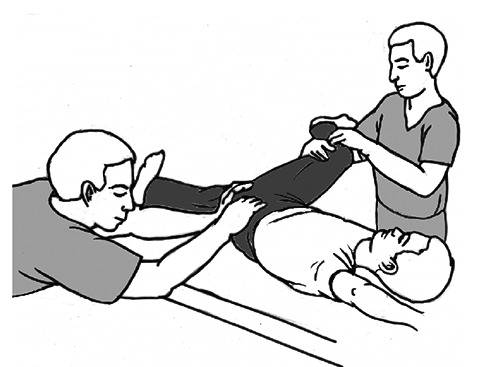
East Baltimore Lift maneuver
The patient is placed in the supine position on the gurney. The physician stands on the side of the affected hip, with the assistant on the opposite side of the patient. The physician and assistant, while slightly flexing their own knees, place their arms beneath the knee of the patient’s affected hip and rest their hands on each others’ shoulders. The physician or assistant uses his/her free hands to stabilize the pelvis. A second assistant at the foot of the gurney applies a downward leveraging force on the ankle while the physician and first assistant concomitantly apply an upward force in line with the femur by extending their knees (Figure 5). This action should lead to a reduction of the dislocated hip. The physician can also apply adduction, abduction, and internal and external rotation using the patient’s ankle until reduction is achieved. If no second assistant is available, the physician uses his/her arm closest to the affected hip as the fulcrum and places the arm farthest from the affected hip on the ankle of the patient’s affected leg. While the assistant stabilizes the pelvis, the physician and assistant then apply traction to the affected femur by extending their legs (not pictured).21
Figure 5.

East Baltimore lift maneuver.
Howard maneuver
The patient is placed in the supine position. The physician and assistant stand on the side of the affected hip. The affected hip is flexed to a 90-degree angle. The assistant applies a lateral traction force on the thigh of the affected side (Figure 6). If available, a second assistant can stabilize the pelvis against the bed (not pictured); however, if a second assistant is not available, the first assistant can help to stabilize the pelvis. The physician, while holding the lower leg by grasping the knee, then applies traction in line of the femur and uses internal and external rotation until reduction is achieved.9 Preferably, the physician stands on the side of the bed, rather than entering the bed. Entering the bed, however, is necessary at times.
Figure 6.

Howard maneuver.
Lateral traction method
The patient is placed in the supine position on the gurney. An assistant wraps a sheet around the inner thigh of the patient’s affected leg. The physician applies longitudinal force along the length of the femur, while the assistant using the sheet provides lateral traction until reduction is achieved (Figure 7). Internal rotation is used as necessary.5
Figure 7.
Lateral traction method.
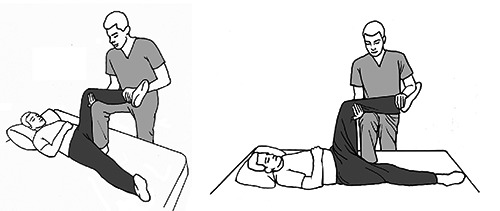
Piggyback method
The patient is placed in the supine position at the end of the gurney. The patient’s affected leg is flexed at the hip and the patient’s knee is placed over the physician’s preferred shoulder (Figure 8). Using the shoulder as fulcrum, the physician applies a downward force on the patient’s tibia until reduction is achieved. A variant of this maneuver is to place both of the patient’s legs on the physician’s shoulders.8
Figure 8.

Piggyback method.
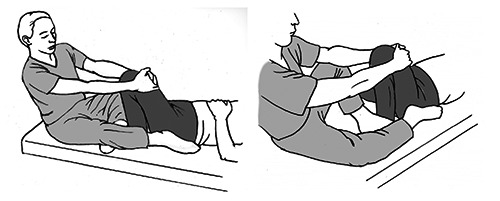
Tulsa technique/Rochester method/Whistler technique
The patient is placed supine on the gurney with both legs flexed. While standing on the side of the affected hip, the physician uses his/her arm closest to the head of the bed to hold the patient’s knee on the unaffected side so the patient’s leg on the affected side is flexed over the physician’s forearm. The physician places his/her other hand on the ankle of the patient’s affected leg. The physician applies downward traction using the ankle and a combination of internal and external rotation to reduce the hip (Figure 9).5,15,17,22
Figure 9.
Tulsa technique/Rochester method/Whistler technique.
Skoff maneuver
The patient is placed in the lateral decubitus position with the affected leg facing up. The assistant positions the affected leg into 90-100 degree hip flexion, 40-45 degree internal rotation, and 40-45 degree adduction and flexes the knee to 90 degrees. The assistant then leans back, providing a lateral traction in line of the femur (Figure 10). At the same time, the physician palpates the deformity in the gluteal region (not pictured) and pushes the femoral head until reduction into the acetabulum is achieved.7
Figure 10.
Skoff maneuver.
Stimson gravity maneuver
The patient is placed in the prone position with the lower limbs at 90 degrees flexion over the edge of the gurney. The physician flexes the knee to 90 degrees and applies a downward force on the lower leg while using the ankle to apply internal and external rotation until reduction in achieved (Figure 11).10 Alternatively, the physician can use his/her knee to apply the downward force in the popliteal fossa of the patient’s affected leg.13 While this technique uses gravity as a reduction aide, positioning the patient partially off the bed requires a great deal of caution because the patient must be sedated for a hip reduction. The patient must be protected from falling off the bed, and the patient’s airway must be monitored because s/he is in the prone position while sedated.
Figure 11.
Stimson gravity maneuver.
Traction counter maneuver
The patient is placed in the lateral decubitus position with the affected leg up. An assistant positions the affected leg into hip flexion, internal rotation, and adduction and flexes the knee to 90 degrees in a manner similar to the Skoff method. Standing within a looped strap, the assistant places the strap around the patient’s groin and over the iliac crest. The physician stands in a separate looped strap and places it around the patient’s knee. The physician then leans back against the looped strap, providing a lateral traction in line of the femur, while manipulating the affected leg with his/her free hands. At the same time, the assistant leans back against his/her looped strap, providing a lateral traction force, palpates the deformity in the gluteal region, and pushes the femoral head until reduction into the acetabulum is achieved (Figure 12).23
Figure 12.

Traction counter traction maneuver.
Flexion adduction method
The patient is placed in the supine position and is under general anesthesia. Standing on the unaffected side of the patient, the physician lifts the affected leg into flexion and maximum adduction while pulling traction in line with the femur. An assistant stabilizes the pelvis and provides manual pressure to the head of the femur toward the acetabulum (Figure 13).24
Figure 13.
Flexion adduction method.
Foot-fulcrum maneuver
The patient is placed supine on the bed, and the physician sits on the bed at the patient’s feet. The physician gently flexes the affected hip as much as possible, moving the femoral head more posteriorly and reducing the chance of the femoral head getting stuck on the acetabular rim. The physician places his/her inner foot against the anterior aspect of the patient’s affected ankle and his/her outer foot on the posterolateral aspect of the patient’s hip to attempt to palpate the femoral head (Figure 14). Next, the physician grasps the flexed knee on the patient’s affected side and leans backward, using his/her feet as the fulcrum and giving a longitudinal traction in line with the femur. If necessary, the physician can internally rotate as needed by leaning from side to side.25
Figures 14.
Foot-fulcrum maneuver.
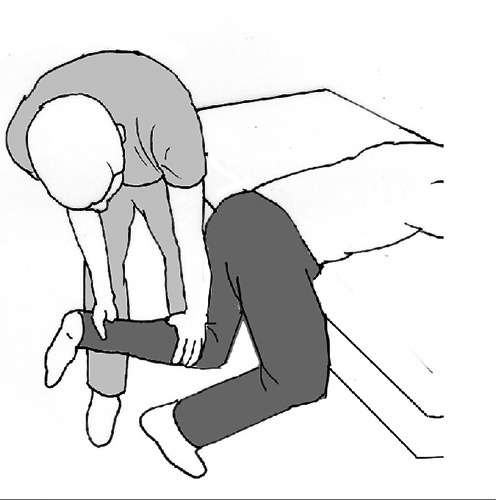
The Waddell technique
This maneuver uses the principles of the Allis and Bigelow maneuvers, with a modification that relieves the strain normally placed on the back. The reduction is performed with an assistant holding the patient’s pelvis down on the bed. The physician hovers over the patient and bends into position with the patient’s affected leg between his/her legs. The physician places his/her forearm behind the knee of the affected hip so the patient’s lower leg and foot are draped over the forearm and rest between his/her legs. The physician rests his/her forearm across his/her knees so the elbow is on one knee and the hand/wrist is on the other. Keeping the back straight, the physician hugs the patients’ knee close to the chest. The patient’s hip is flexed between 60 to 90 degrees and the knee is flexed to 90 degrees. This position places the physician at a mechanical advantage by holding the leg of the patient’s affected hip steadily from behind the knee with the forearm locked across the knees and the patient’s knee tucked close to the physician’s chest (Figures 15). The surgeon then gently leans backward using only his/her feet to pivot, pulling traction through the patient’s knee with the force exerted by the surgeon’s forearm that is locked on his knees. This gives a steady and gentle, yet forceful, traction on the patient’s femur. Minimal strain is placed on the physician’s back, and the physician stays low and stable while on the bed with the patient. The physician then can adduct and internally rotate by leaning and rotating, as necessary. We advise using the lateral forearm to wrap under the patient’s knee when attempting reduction. The opposite arm can be used to add traction by pushing off the assistant holding the pelvis or by pulling on the end of the bed behind the physician. A palpable clunk alerts the physician that the hip has been reduced. The leg is then rested in extension, and postreduction roentgenograms are taken to confirm reduction.
Figure 15.
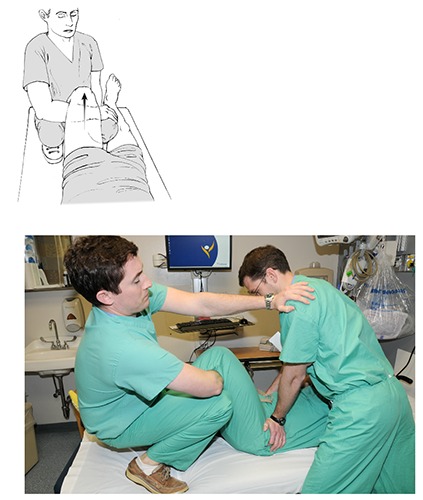
The Waddell technique.
Reduction of anterior dislocations
Anterior dislocations require the same inline traction on the femur; however, flexion of the hip is not usually possible because the femoral head is resting on the anterior surface of the pelvis in most cases. Two types of anterior dislocation are described: obturator dislocation26 and pubic dislocation.27 Each require slight variations in technique but usually require hip extension, in-line traction, and external rotation for reduction. For the pubic dislocation, flexion of the hip is not usually possible and hyper-extension and in-line traction is required.27 The obturator dislocation is usually reduced with hip flexion, adduction and external rotation. Once the head is unlocked from the obturator foramen, axial traction is applied.28 All the methods described below use these basic principles. Again, as in posterior hip dislocations, roentgenograms are necessary to confirm dislocation and position. Furthermore, as stated in the posterior section, physicians should be wary of and look for concomitant injury, as anterior dislocations are usually high-energy injuries. Department-specific sedation is required for patient comfort and to overcome the strong surrounding hip muscles. Pictures of the reductions for anterior dislocations are not included as they are performed in a similar manner as posterior dislocations.
Allis leg extension method
With the patient in the supine position, the physician either enters the bed or stands beside it. While an assistant stabilizes the pelvis against the bed, the surgeon grasps the ipsilateral leg at the knee and applies traction in line with the deformity.18 With this maneuver, the additions noted by Toms, Dawson and Dingley can be applied.26-28 These include adduction, external rotation and hip flexion. If the patient has a pubic dislocation, hip hyper-extension will be necessary.
Bigelow leg extension method
The patient is placed in the supine position. The physician grasps the ankle of the affected leg with one hand and places the opposite forearm under the patient’s knee. While an assistant stabilizes the pelvis with downward pressure, the physician applies traction in line of the femur while adducting, externally rotating, and extending the affected hip.2-4 Again, the additional techniques described by Toms, Dawson and Dingley can be applied.26-28 The preferred method for physician safety is to perform this maneuver while standing at the side of the bed; however, at times, entering the bed is a necessity.
Lateral traction method
The patient is placed in the supine position on the gurney. An assistant wraps a sheet around the inner thigh of the patient’s affected leg. The physician applies longitudinal force along the length of the femur, while the assistant uses the sheet to provide lateral traction until reduction is achieved. External rotation is used as necessary.5
Stimson gravity method
The patient is placed in the prone position, with the lower limbs at 90 degrees flexion over the edge of the gurney. The physician flexes the knee to 90 degrees and applies a downward force on the lower leg while using the ankle to apply internal and external rotation until reduction is achieved.10 Alternatively, the physician uses his/her knee to apply the downward force in the popliteal fossa of the patient’s affected leg.13 While this technique uses gravity as a reduction aide, positioning the patient partially off the bed requires a great deal of caution because the patient must be sedated for a hip reduction. The patient must be protected from falling off the bed, and the patient’s airway must be monitored because s/he is in the prone position while sedated. As noted by Dawson, the pubic anterior dislocation usually cannot achieve hip flexion and may not be reducible with this technique.26
Experience with the Waddell technique
After IRB approval, 20 consecutive posterior dislocations were reduced using the Waddell technique described above. Patients were met in the ED after consultation by the ED physician. The ED physician provided conscious sedation. All hips were confirmed as posterior dislocations with X-rays and all hips were status post total hip arthroplasty. Once the patient was sedated, the dislocated hip was reduced in the manner described above. Patients were placed in a knee immobilizer or hip abduction brace after reduction. Each reduction attempt was successful on the initial attempt. No periprosthetic fractures or other complications occurred during the reduction attempts. Furthermore, no injuries occurred in the physician performing the reductions.
Discussion
While relatively uncommon in native hips, dislocation is a complication of total hip arthroplasty, seen in approximately 1% of all hip arthroplasties.29 During the next 15 years, the number of total hip arthroplasties is expected to increase to 572,000 cases per year.30 With this rapid increase in the number of total hip arthroplasties being performed, the number of dislocations will also increase. Attention to the direction of the dislocation is paramount because both the complications associated with the dislocation and the reduction maneuvers required to reduce it differ.
When a patient presents with suspected dislocation, standard workup should include a history, physical examination, and radiographs. History should include any prior surgical procedures and inciting events for the dislocation. Specific hip movements can help determine the direction of location: anterior dislocations are usually caused by abduction, extension, and external rotation, while posterior dislocations are usually the result of adduction, internal rotation, and flexion of the hip. The physical examination should not only include a neurovascular exam but also an examination of the hip for scars and acute injuries. The scar location can help determine the approach used and may give an indication for the dislocation direction. After the history and physical examination, radiographs will further help determine the presence of dislocation and its direction. When evaluating the radiograph, subtle clues can help determine the location of dislocation. When an anterior dislocation is present, the femoral head is closer to the generator and further from the x-ray film in an anterior to posterior film. This will lead to a magnification of the femoral head. In the opposite manner, a posterior dislocation will lead to a femoral head that is closer to the film and further from the generator, leading to the head appearing smaller.31
Once the diagnosis and direction of dislocation have been established, reduction should be performed emergently. Depending on the direction of the dislocation, one of the reduction techniques described above can be used. Physician and worksite safety must be taken into account for the reduction. Many of the reduction maneuvers require the physician to enter the bed with the patient. Anytime this occurs, the potential for physician harm increases because standing on the mattress is unstable, and performing a high-intensity maneuver from a height has the potential of causing the physician to fall.
Another potential area for physician injury is lumbar strain when applying in-line traction for the reduction. During many reduction maneuvers, the first author noted the significant force and strain upon the back when using the classic Allis and Bigelow maneuvers. Occupational safety literature describes using one’s legs to lift heavy loads, while keeping the back straight and hugging the object close to one’s body.32 The newly described Waddell technique shifts the lifting agent from the back to the strong leg muscles and also employs the lever force when pivoting backwards with the physician’s feet. As seen in most illustrations and videos of the Allis or Bigelow technique, most physicians performing reductions by leaning over the patient’s leg and use their backs to lift. This was the case of the first author; however, in attempting to mitigate the force through the back, the first author began draping the arm used for reduction across his knee and pivoting backward through his feet. This modification allowed the spine to stay straight and hugged the load close to the reducer’s chest. Pivoting backward through the feet provides the required force for the reduction. In doing this, strain on the back was significantly reduced and proper ergonomics for heavy lifting were followed. The other authors began using the technique and described a similar reduction in back strain. While it is possible to use the legs to lift using the Allis and Bigelow maneuvers, standing up in the bed should be avoided because of the instability associated with standing on a cushioned bed. This modified technique allows the physician to stay low and stable when required to enter the bed for reduction.
Conclusions
While all of the described techniques are viable for the reduction of dislocated hips, we suggest using this modified technique for posterior hip dislocation to decrease the strain on the reducing physician’s back. Furthermore, this maneuver allows the physician to adhere to the back safety principles set forth by OSHA that have been shown to prevent back injury.
Acknowledgments
The authors would like to thank Barbara Siede for her expert illustration support and Kathleen McFadden for her expert editorial support. The first author thanks Doug Padgett for his sound advice and mentorship.
References
- 1.Hougaard K, Thomsen PB. Traumatic dislocation of the hip - prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Trauma Surg 1986;106:32-5. [DOI] [PubMed] [Google Scholar]
- 2.Bigelow HJ. Luxations of the hip joint. Boston Med Surg J 1870;5:65-7. [Google Scholar]
- 3.Bigelow HJ. On the dislocated hip. Lancet 1878;1:860-2. [Google Scholar]
- 4.Bigelow HJ. On the dislocated hip. Lancet 1878;1:894-5. [Google Scholar]
- 5.Nordt WE., 3rd Maneuvers for reducing dislocated hips: a new technique and literature review. Clin Orthop Relat Res 1999: 260-4. [PubMed] [Google Scholar]
- 6.Lefkowitz M. A new method for reduction of hip dislocations. Orthop Rev 1993;22: 253-6. [PubMed] [Google Scholar]
- 7.Skoff HD. Posterior hip dislocation, a new technique for reduction. Orthop Rev 1986;15:405-9. [PubMed] [Google Scholar]
- 8.Marya SK, Samuel AW. Piggyback technique for relocation of posterior dislocation of the hip. Injury 1994;25:483-4. [DOI] [PubMed] [Google Scholar]
- 9.Howard CB. A gentle method of reducing traumatic dislocations of the hip. Injury 1992;23:481-2. [DOI] [PubMed] [Google Scholar]
- 10.Stimson LA. Treatise on Fractures. Philadelphia, PA: Lea Brothers & Co.; 1883. [Google Scholar]
- 11.Stimson LA. Five cases of dislocation of the hip. NY Med J 1889;50:118-21. [Google Scholar]
- 12.Thompson VP, Epstein HC. Traumatic dislocation of the hip; a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am 1951;33A:746-78. [PubMed] [Google Scholar]
- 13.Herwig-Kempers A, Veraart BE. Reduction of posterior dislocations of the hip in the prone position. J Bone Joint Surg Br 1993;75:328. [DOI] [PubMed] [Google Scholar]
- 14.O’Hara JP, 3rd, Whitted G. A controlled method of closed reduction of total hip dislocation. Orthopedics 1993;16:489-92. [DOI] [PubMed] [Google Scholar]
- 15.Vosburgh CL, Vosburgh JB. Closed reduction for total arthroplasty dislocation. The Tulsa technique. J Arthroplasty 1995;10: 693-4. [DOI] [PubMed] [Google Scholar]
- 16.McMurtry IA, Quaile A. Closed reduction of the traumatically dislocated hip: a new technique. Injury 2001;32:162-4. [DOI] [PubMed] [Google Scholar]
- 17.Stefanich RJ. Closed reduction of posterior hip dislocation: the Rochester method. Am J Orthop (Belle Mead NJ) 1999;28:64-5. [PubMed] [Google Scholar]
- 18.Allis OH. The Hip. Philadelphia: Dorman; 1895. pp 14-26. [Google Scholar]
- 19.Epstein HC, Harvey JP., Jr Traumatic anterior dislocations of the hip: management and results. An analysis of fifty-five cases [abstract]. J Bone Joint Surg Am 1972;54:1561-2. [Google Scholar]
- 20.Hendey GW, Avila A. The Captain Morgan technique for the reduction of the dislocated hip. Ann Emerg Med 2011;58:536-40. [DOI] [PubMed] [Google Scholar]
- 21.Schafer SJ, Anglen JO. The East Baltimore lift: a simple and effective method for reduction of posterior hip dislocations. J Orthop Trauma 1999;13:56-7. [DOI] [PubMed] [Google Scholar]
- 22.Walden PD, Hamer JR. Whistler technique used to reduce traumatic dislocation of the hip in the emergency department setting. J Emerg Med 1999;17:441-4. [DOI] [PubMed] [Google Scholar]
- 23.Dahners LE, Hundley JD. Reduction of posterior hip dislocations in the lateral position using traction-countertraction: safer for the surgeon? J Orthop Trauma 1999;13:373-4. [DOI] [PubMed] [Google Scholar]
- 24.Bassi JL, Ahuja Singh H. A flexion adduction method for the reduction of posterior dislocation of the hip. J Bone Joint Surg Br 1992;74:157-8. [DOI] [PubMed] [Google Scholar]
- 25.Yin TC, Wang JW, Lao ML, Chung HY. A simple technique for reducing posterior hip dislocation: the foot-fulcrum manoevre. Injury 2010;41:665-7. [DOI] [PubMed] [Google Scholar]
- 26.Dawson I, van Rijn ABB. Traumatic anterior dislocation of the hip. Arch Orthop Trauma Surg 1989;108:55-7. [DOI] [PubMed] [Google Scholar]
- 27.Poelsky PE, Poelsky FA. Intrapelvic dislocation of the femoral head following anterior dislocation of the hip: a case report. J Bone Joint Surg Am 1972;54:1097-8. [PubMed] [Google Scholar]
- 28.Toms AD, Williams S, White SH. Obturator dislocation of the hip. J Bone Joint Surg Br 2001;83:113-5. [DOI] [PubMed] [Google Scholar]
- 29.Kwon MS, Kuskowski M, Mulhall KJ, et al. Does surgical approach affect total hip arthroplasty? Clin Orthop Relat Res 2006;447:34-8. [DOI] [PubMed] [Google Scholar]
- 30.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the united states from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [DOI] [PubMed] [Google Scholar]
- 31.Rockwood CA, Green DP. Rockwood and Green’s fractures in adults. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 32.U.S. Department of Labor Occupational Safety & Health Administration. Ergonomics eTool: solutions for electrical contractors - materials handling: heavy lifting. Available from: https://www.osha.gov/SLTC/etools/electricalcontractors/materials/heavy.html#awkward. Accessed on: August 6, 2015.


