Abstract
Introduction
Five hundred thousand maternal deaths occur each year worldwide, many of which are in developing countries. The maternal mortality rate is a measure that demonstrates the degree of adequacy of prenatal care and of economic and social conditions. The aim of this study was to determine the frequency and causes of pregnancy-related mortality rates in Yazd Province.
Methods
This cross-sectional study examined the maternal deaths related to pregnancy that were recorded in Yazd Province, Iran, from 2002 to 2011. All maternal deaths that occurred during pregnancy, during delivery, and 42 days after birth were analyzed in this study. The data were collected through a questionnaire, and both direct and indirect causes of maternal deaths were determined.
Results
Forty pregnancy-related deaths occurred in this period, and the maternal mortality rate was 20.8 deaths per 100,000 live births. The mean age of death in the mothers in this study was 29.17. Fifty-five percent of women of the women who died delivered their babies by cesarean section, and only 20% of them delivered their babies vaginally. Bleeding was the most common cause of maternal mortality (30%), and it was associated directly with maternal mortality. Furthermore 20% of the mothers died due to heart disease and cardiac complications, which were associated indirectly with maternal mortality.
Conclusion
Cesarean section and its complications were the main cause of death in many cases. Thus, providing a strategic plan to reduce the use of this procedure, educate mothers, and ensure adequate access to pre-maternal care and to care during pregnancy are the most important measures that can be taken to decrease the maternal mortality rate.
Keywords: maternal mortality, pregnancy-related
1. Introduction
Five hundred thousand maternal deaths occur worldwide each year, many of which are in developing countries (1). Even though maternal mortality rates have declined dramatically over the past 50 years (2), there are still high levels of maternal mortality in developing countries, and this an increasing public health concern (3). Maternal mortality is a vital index that drastically differs between developed and developing countries. The causes of maternal deaths in these countries are the same, but the distributions of these causes vary from region to region (4). According to the World Health Organization, the definition of death during pregnancy includes death during pregnancy or 42 days after its conclusion, regardless of the duration of the pregnancy or the site of embryo implantation, death for any reason related to pregnancy, death due to pregnancy, or death related to any of the procedures that are used (5). The maternal mortality rate is a measure that indicates the adequacy of the degree of parental care as well as social and economic conditions (6). So decreasing maternal mortality and improving maternal health is one of the eight Third Millennium Development Goals, which are conducted under the auspices of the United Nations in all countries. The aim of the Goals is to reduce maternal mortality by 75% in 2015 from the rate in 1990 (7). In 2013, a report issued by the World Health Organization estimated that 289,000 maternal deaths occurred worldwide that year, which was a 45% decrease from the number in 1990. According to this report, the ratio of maternal deaths in developing regions to maternal deaths in developed countries is about 14:1. The maternal mortality rate in Iran in 1990 was 83 per hundred thousand live births. This rate declined to 23 per hundred thousand live births in 2013. According to the Fifth Development Plan of Iran, this rate should be reduced to 15 deaths per hundred thousand live births (9). The persistence of maternal mortality in low-income countries highlights the need to identify the causes and to identify strategies that are effective reducing or eliminating those causes (10). About 80% of pregnancy-related deaths are associated directly with the complications of pregnancy, childbirth, the postpartum period, and improper interventions or treatments (5). According to numerous studies, bleeding disorders, hypertension, and infection are the triad of lethality that is responsible for much of the morbidity and mortality associated with pregnancy in the world (11). This is despite the fact that 25% of all pregnancy-related deaths are due to postpartum hemorrhage, which rapidly results in death unless immediate actions are taken to save the patient (5). Several studies have shown that bleeding is the most common cause of maternal death, e.g., Rajais et al.’s study (7) and Mohammad, Nia et al.’s study (12). More deaths related to complications of pregnancy can be prevented if pregnant women have access to good quality antenatal care, delivery care, and post-delivery care (5). The aim of this study was to determine the frequency and causes of pregnancy-related maternal mortality in Yazd Province, Iran.
2. Material and Methods
This study was a cross-sectional study that examined all maternal deaths from 2002 to 2011 in order to determine the details of the deaths that were recorded in this period in health centers in Yazd. All maternal deaths that occurred during pregnancy, during delivery, and 42 days after birth were included in this study. The questionnaire was designed by the researchers, and it included questions about the demographic characteristics of mothers and their obstetrical history during pregnancy, childbirth, and after childbirth. The questionnaire was developed by a team to investigate the death of mothers using the 18-page questionnaire entitled Guidelines on Tracking Child and Maternal Mortality (according to the Countries Instructions of Maternal Death Affairs System) (13). This team consisted of two maternal experts, an expert from the Department of Family Health, and a professional in the field of midwifery. The numbers of live births during this period also were collected from Yazd Health Centers. The data were analyzed by SPSS software, version 16. The direct and indirect causes of maternal deaths were identified, and a report was presented indicating the percentages of births and maternal mortality in several provinces in Iran.
3. Results
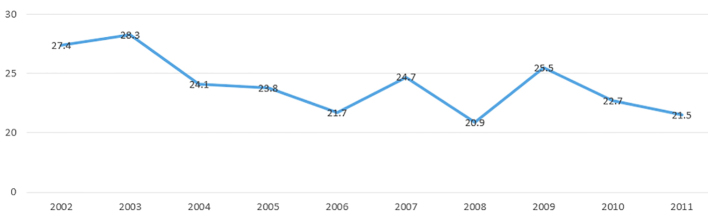
The mean age of the mothers in this study was 29.17 ± 5.6 years. The average gestation period for these mothers was 32.78 weeks, and the mean interval between their pregnancies was 5.68 ± 4.6 years. The mean rate of pregnancy among the mothers was 2.62 ± 2.3, with a mean parity rate of 2.52 ± 1.1. Most of the women were literate, but 17.5% of them were illiterate. Among the mothers, 92.5% of them gave birth in a hospital, and a specialist delivered 82.5% of the babies. Cesarean delivery was the most common method (55%), and only 20% gave birth vaginally. Prenatal care was received by 77.5 % of the mothers (Table 1). Bleeding was the most common cause of maternal mortality with the prevalence 30%. After that, heart disease, malignancies, amniotic fluid, embolism, and pulmonary diseases caused 20, 12.5, 10, 10, and 10% of the deaths, respectively. Also, preeclampsia and eclampsia were responsible for 7.5% of the deaths. During the study period, among the 192,217 births that occurred in Yazd, 40 maternal deaths occurred. Among the deaths, 47.5% occurred for reasons directly related to obstetrics, and 52.5% of deaths were due to indirect causes (Table 2). Figure 1 shows that the maternal mortality rate in the country had a downward trend from 2002 to 2011, decreasing from 27.4 per 100,000 live births in 2002 to 21.5 in 2011. Also, the mean rate of maternal deaths was 20.94 per 100,000 live births in Yazd, which was less than the mean of 23.99 for the entire country. The lowest maternal mortality rate was in 2007 and the highest rate was in 2010 (Figure 1). According to the World Health Organization and UNICEF (Table 3), the maternal mortality rate was 16 deaths per 100,000 live births in developed countries and 240 deaths per 100,000 live births in developing countries from 2005 to 2010. It was evident that Iran had a significant reduction in maternal mortality from 1990 to 2010 among the countries in the region (−81%).
Table 1.
Distribution of demographic and obstetric characteristics of pregnancy-related maternal mortality in Yazd (2002–2011)
| Characteristics | n | % | |
|---|---|---|---|
| Mother’s education | None | 7 | 17.5 |
| Elementary and secondary | 9 | 22.5 | |
| University | 24 | 60 | |
| Attendant | Doctor | 33 | 82.5 |
| Trained midwife | 5 | 12.5 | |
| Untrained midwife | 2 | 5 | |
| Place of delivery | Hospital | 37 | 92.5 |
| Home | 3 | 7.5 | |
| Pregnancy outcome | Cesarean | 22 | 55 |
| Abortion | 6 | 15 | |
| Normal vaginal delivery | 8 | 20 | |
| Death in pregnancy | 4 | 10 | |
| Prenatal care | Yes | 31 | 77.5 |
Table 2.
Distribution of causes of maternal deaths in Yazd (2002–2011)
| Causes of pregnancy-related maternal deaths | % | Maternal mortality ratio (MMR) | |
|---|---|---|---|
| Direct obstetric | Hemorrhage | 30 | 6.24 |
| Eclampsia-Preeclampsia | 7.5 | 1.56 | |
| Amniotic fluid embolism | 10 | 2.08 | |
| Total | 47.5 | ||
| Indirect obstetric | Heart disease | 20 | 4.16 |
| Malignancy | 12.5 | 2.6 | |
| Pulmonary diseases | 10 | 2.08 | |
| Other obstetric | 10 | 2.08 | |
| Total | 52.5 | 4.16 | |
Figure 1.
Trend of maternal mortality rate in Iran from 2002 to 2011
Table 3.
Trends in estimates of maternal mortality ratio in Iran’s neighboring countries as classified by the World Health Organization and UNICEF (1990–2010)
| Country/region | MMR | % Change in MMR (1990–2010) | ||||
|---|---|---|---|---|---|---|
| 1990 | 1995 | 2000 | 2005 | 2010 | ||
| Developed Regions | 26 | 20 | 17 | 15 | 16 | −39 |
| Developing Regions | 440 | 400 | 350 | 290 | 240 | −47 |
| Afghanistan | 1300 | 1300 | 1000 | 710 | 460 | −65 |
| Azerbaijan | 56 | 81 | 65 | 52 | 43 | −23 |
| Bahrain | 23 | 21 | 22 | 21 | 20 | −13 |
| Iran | 120 | 72 | 48 | 30 | 21 | −81 |
| Iraq | 89 | 84 | 78 | 74 | 63 | −29 |
| Kuwait | 11 | 10 | 9 | 8 | 14 | 24 |
| Saudi Arabia | 44 | 33 | 27 | 25 | 26 | −45 |
| Pakistan | 490 | 440 | 380 | 310 | 260 | −46 |
| Oman | 110 | 74 | 51 | 39 | 32 | −72 |
| Qatar | 15 | 13 | 11 | 9 | 7 | −53 |
4. Discussion
The maternal mortality rate is the most important development indicator because it shows the status of each country’s development by taking into account the number of maternal deaths per 100,000 live births. This index is in compliance with the status of women’s education, the status of communication routes, access to health services and emergency obstetrical care, health care costs, the amount of family income, and many other factors (9). The results show that the average age of maternal death was 29.17. In Heyl et al.’s study (14), it also was reported that the highest rates of maternal mortality were in the 25–34 age group. Fauveau et al. (15) also obtained similar results. And this age range is exactly the peak ages at which women have the most family responsibilities. In this study, the mean interval between pregnancies was 6.5 years. After gathering obstetrical information on 456,889 women, Conde-Agudelo and Belizan (16) reported that the highest rates of maternal mortality occurred when the interval between delivery and next pregnancy was less than 14 months. Most studies also have shown that the less time between pregnancies increases the risk of maternal mortality. The differences in these results may be due to the increased interval between births in recent years in Iran. In this study, the average number of pregnancies was 2.6 and parity was 2.5. Hochon et al. (17) conducted a study to determine the causes of maternal mortality in rural Bangladesh. They reported the highest maternal mortality rate in women who had five or more deliveries (43.2% of all deaths). The contrast between these results and the results of this study could be due to high birthrate in the area noted. Heyl et al. (14) performed a study on 46 cases of maternal deaths due to amniotic fluid embolism in America, and the mean parity was 2.4, and the findings of our study were consistent with that finding. In this study, the highest mortality was related to mothers with higher education (60%).
According to the Arifeen study (18), raising the educational level of women of reproductive age is an important factor in reducing mortality and morbidity. In a study by Conde-Agudelo (16), it was reported that the highest mortality rate occurred in mothers with only a primary education. The difference in results could be due to the low number of samples. In the current study, 92% of the mothers gave birth in hospitals. In 2011, throughout Iran, 94% of the mothers who died had given birth in a hospital (19). Jokhio et al. (1) in Pakistan reported different results, showing that 82.8% of pregnant women who died were giving birth at home. (The maternal mortality rate was 268 deaths per 100,000 live births.) In West Africa, the study of Ronsmans et al. (20) showed that 55% of women who died in urban areas had given birth in a hospital, whereas, in rural areas, only 11% who died had given birth in hospitals. The results show that social and economic conditions and access to healthcare services are important factors in maternal mortality. In urban areas in which most of the deliveries were in a hospital, more attention should be diverted to potential negligence and delayed treatment in the hospitals. Also, in the present study, 82.5% of deliveries were performed by physicians. In Iran (2011), 96% of deliveries were performed by physicians and midwives (18). However, the study conducted in Pakistan showed that only 10.8% of deliveries were performed by doctors, and 76.2% were performed by untrained midwives (13). Ronsmans et al. (19) showed that, in West Africa, only 3% of deliveries were performed by physicians. These differences could be due to the increase in cesarean rates in Iran and low levels of healthcare services in countries such as Pakistan and South Africa. In this study, 77/5% of mothers had benefited from prenatal care. Montgomery et al. (20) showed that maternal mortality in India was significantly higher in rural women due to poor access to healthcare. A study by Mackay et al. (21) also indicated that women who did not receive prenatal care had the highest mortality rate; the results of our study were inconsistent with their finding, and this discrepancy may have resulted from our low number of samples. The method of delivery produced one of the most noticeable results obtained from this study in that 55% of the mothers who died had a cesarean section. According to the national instructions of the Maternal Death System, 63% of deaths occurred in women who had cesarean section (18). Most studies in this field also have shown similar results. Heyl et al. (13) reported that the highest death rate occurred in women who had cesarean delivery. (The ratio of pregnancy-related deaths in women who had cesarean sections was 2.8 compared with 0.2 in women who had vaginal deliveries). Ronsmans’ study (19) also showed that there was a significant association between cesarean delivery and maternal mortality rate (p = 0.027). Huchon et al. (16) performed a study on the prediction of maternal deaths in Senegal and Mali, and they concluded that the maternal mortality rate was higher in hospitals where more caesarean deliveries were performed. In our study, most of the deaths were due to bleeding, which was directly responsible for 30% of the maternal deaths. In a study conducted in India, bleeding during delivery and after delivery was identified as one of the main factors that affected maternal mortality (22). Souza et al. (23) showed in their study that the highest proportion of maternal deaths (26.7%) was due to postpartum hemorrhage. In the study of Atrash et al. (2), it was displayed that 30.2% of maternal deaths in America occurred because of bleeding. In the study of Rajai et al. (7), hemorrhage was reported as the most common cause of maternal mortality (34.1%) in Hormozgan. The results of these studies are consistent with the results of Fauveau’s and Huchon’s studies (14, 16). It is hoped that it may be possible to reduce maternal deaths caused by cesarean by the country’s healthcare system offering to increase the birth rate by vaginal delivery in first parity and to offer free of vaginal delivery. Specialists’ efforts to increase awareness and early diagnosis of heart and lung problems and cancer can reduce maternal mortality considerably, albeit indirectly. Finally, it was calculated that the average maternal mortality rate in this study during 10 years was 20.94 deaths per 100000 live births. At the same time, in Iran, it was 23.99 deaths per 100,000 live births. Rajai et al. (7) reported that the maternal mortality rate was 39.7 deaths per 100,000 live births for 2005–2011. It was reported that in 2010, the worldwide maternal mortality rate was 16 deaths per 100,000 live births in developed countries and 240 deaths per 100,000 live births in developing countries. In America, in the years 1979–1986, the maternal mortality rate was 1.9 deaths per 100,000 live births, and it was 1.6 deaths per 100,000 live births during the period of 1999–2007 (2, 13). According to the World Health Organization and UNICEF, in 2010, the maternal mortality rates in Afghanistan, Pakistan, and Iraq were 460, 260, and 63 per 100,000 live births, respectively. Iran had a significant reduction of maternal deaths in 2010 compared to 1990. Iran has improved its healthcare system in the past three decades, and the maternal mortality rate has been reduced considerably. This accomplishment can be presented as a useful example for other developing countries (24, 25).
5. Conclusions
Most maternal deaths are preventable, and the maternal mortality rate is one of the most important indicators of general health and the quality of healthcare in a community. The most common cause of maternal death in Iran is hemorrhage, but death rates from cardiovascular disease and increasing gestational age are approaching the maternal death rates due to hemorrhage. So, many deaths can be prevented by establishing control teams for bleeding in the Province, early referral, and having a presence at the patient’s bedside in an equipped health center. Also, deaths due to heart disease can be prevented by quick referral, especially in the third trimester and the postpartum period. Also providing strategies to reduce the use of cesarean section; to increase access to care before, during, and after pregnancy; and to enhance the mother’s education are the most important measures that can be taken to reduce maternal mortality.
Acknowledgments
We thank Dr. Aflatoonian, Dr. Karimzade, and Dr. Dehghani Firoozabadi who helped us collect the data for this study.
Footnotes
iThenticate screening: September 24, 2015, English editing: October 03, 2015, Quality control: Jan 05, 2016
Conflict of Interest: There is no conflict of interest to be declared.
Authors’ contributions: All authors contributed to this project and article equally. All authors read and approved the final manuscript.
References
- 1.Jokhio AH, Winter HR, Cheng KK. An Intervention Involving Traditional Birth Attendants and Perinatal and Maternal Mortality in Pakistan. N Engl J Med. 2005;325(20):2091–9. doi: 10.1056/NEJMsa042830. [DOI] [PubMed] [Google Scholar]
- 2.Atrash HK, Koonin LM, Lawson HW, Franks AL, Smith JC. Maternal Mortality in the United States, 1979–1986. Obstet Gynecol. 1990;76(6):1055–60. [PubMed] [Google Scholar]
- 3.Stanton C, Hobcraft J, Hill K, Kodjogbé N, Mapeta WT, Munene F. Every Death Counts: Measurement of Maternal Mortality Via a Census. Bulletin of the World Health Organization. 2001;79(7):657–664. [PMC free article] [PubMed] [Google Scholar]
- 4.Cham M, Sundby J, Vangen S. Maternal Mortality in the Rural Gambia, A Qualitative Study on Access to Emergency Obstetric Care. Reproductive Health. 2005;2(3) doi: 10.1186/1742-4755-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shodjai Tehrani H. In: In translation Text Book of Preventive and Social Medicine. 17th ed. Park JE, Park K, editors. Tehran: samat publication; 2005. pp. 276–80. [Google Scholar]
- 6.Baghiani Moghadam MH, Ehramposh H, Mazlomi S. Principles and Methods of Epidemiology. Tehran: Cheragheh Danesh & Albab; 2003. pp. 50–1. [Google Scholar]
- 7.Rajai M, Zaree SH, Dadipor S, et al. Determining the Frequency and Causes of Maternal Mortality in Hormozgan Province, Iran during 2005 – 2011. Iranina Journal of Obstetrics Gynecology and Infertility. 2014;16(87):9–14. [Google Scholar]
- 8.Worlds Health Organization. Trends in Maternal Mortality 1990 to 2013. pp. 1–8. [Google Scholar]
- 9.Ahmadi A, Eshrati B, Nowrozi M, et al. Root Cause Analysis(RCA) of a Maternal Death in Markazi Province: a Methodological Research in Clinical Epidemiology & Health Journal. 2013;5(1):18–28. [Google Scholar]
- 10.Bullough C, Meda N, Makowiecka K, et al. Current Strategies for the Reduction of Maternal Mortality. An International Journal of Obstetrics and Gynaecology. 2005;112:1180–8. doi: 10.1111/j.1471-0528.2005.00718.x. [DOI] [PubMed] [Google Scholar]
- 11.Ghazijahani B. In: In translation Williams Obstetrics. 21st ed. Gary Cunningham F, Gant NF, Leveno KJ, et al., editors. Tehran: Golban; 2001. p. 572. [Google Scholar]
- 12.Mohamadinia N, Samiye Zadye Tosy T, Rezay MA, Rostay F. The Frequency and Effective Factors on Maternal Mortality in Sistan and Baluchistan Province, Iran 2002–2009. Iranina Journal of Obstetrics Gynecology and Infertility. 2013;16(44):28–34. [Google Scholar]
- 13.Heyl PS, Sappenfield WM, Burch D, et al. Pregnancy-Related Deaths Due to Pulmonary Embolism:Findings from Two State-Based Mortality Reviews. Matern Child Health J. 2012 doi: 10.1007/s10995-012-1117-5. [DOI] [PubMed] [Google Scholar]
- 14.Fauveau V, Koenig MA, Chakraborty J, Chowdhury AI. Causes of Maternal Mortality in Rural Bangladesh, 1976–85. Bulletin of the World Health Organization. 1988;66(5):643–651. [PMC free article] [PubMed] [Google Scholar]
- 15.Conde-Agudelo A, Belizan JM. Maternal Morbidity and Mortality Associated with Interpregnancy Interval:Cross Sectional Study. BMJ. 2000;321:1255–1259. doi: 10.1136/bmj.321.7271.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huchon C, Dumont A, Traoré M, Abrahamowicz M, Fauconnier A, Fraser W, et al. A Prediction Score for Maternal Mortality in Senegal and Mali. Obstetrics & Gynecology. 2013;121(5):1049–1056. doi: 10.1097/AOG.0b013e31828b33a4. [DOI] [PubMed] [Google Scholar]
- 17.Arifeen SEL, Kenneth Hill, Ahsan KZ, et al. Maternal Mortality in Bangladesh: a Countdown to 2015 Country Case Study. The Lancet. 2014;(14):60955–7. doi: 10.1016/s0140-6736. [DOI] [PubMed] [Google Scholar]
- 18.Report on performance and achievements of maternal mortality care system in 2011. Health Office of Population, Family and School, Department of Maternal Health; [Google Scholar]
- 19.Ronsmans C, Etard JF, Walraven G, Høj L, Dumont A, de Bernis L. Maternal Mortality and Access to Obstetric Services in West Africa. Tropical Medicine and International Health. 2003;8(10):940–8. doi: 10.1046/j.1365-3156.2003.01111.x. [DOI] [PubMed] [Google Scholar]
- 20.Montgomery AL, Ram U, Kumar R, et al. Maternal Mortality in India: Causes and Healthcare Service Use Based on Nationally Representative Survey. PLOS ONE. 2014;9(1) doi: 10.1371/journal.pone.0083331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackay AP, Berg CJ, Atrash H. Pregnancy-Related Mortality from Preeclampsia and Eclampsia. Obstetrics & Gynecology. 2001;97(4):533–537. doi: 10.1016/S0029-7844(00)01223-0. [DOI] [PubMed] [Google Scholar]
- 22.Datta D, Datta PP. Maternal Mortality in India:Problems and Challenges. Asian JMed Res. 2013;2(1):33–5. [Google Scholar]
- 23.Souza JP, Gulmezoglo AM, Vogel J, et al. Moving Beyond Essential Interventions for Reduction of Maternal Mortality(the who multicountry survey on maternal and newborn health):a CROSS-SECTIONAL STUDY. The Lancet. 2013;381(9879):1747–1755. doi: 10.1016/S0140-6736(13)60686-8. [DOI] [PubMed] [Google Scholar]
- 24.Karimi-Zarchi M1, Ezabadi MG, Hekmatimoghaddam S, Mortazavizade M, Taghipour S, Vahidfar M, et al. cancer in pregnancy: a 10-year experience in shahid sadoughi hospital, yazd, iran. Int J Biomed Sci. 2013 Sep;9(3):168–73. [PMC free article] [PubMed] [Google Scholar]
- 25.Behtash N, Karimi Zarchi M, Modares Gilani M, Ghaemmaghami F, Mousavi A, Ghotbizadeh F. Ovarian carcinoma associated with pregnancy: a clinicopathologic analysis of 23 cases and review of the literature. BMC Pregnancy Childbirth. 2008 Jan 20;8:3. doi: 10.1186/1471-2393-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]