Abstract
Sea drowning is a common cause of accidental death worldwide. Respiratory complications such as acute pulmonary oedema, which is often complicated by acute respiratory distress syndrome, is often seen. Noninvasive ventilation is already widely used as a first approach to treat acute respiratory failure resulting from multiple diseases. We report a case of a 45 year old man with a history of epilepsy, motor and mental handicap who developed acute respiratory failure secondary to sea water drowning after an epileptic crisis. We illustrate successful and rapid management of this case with noninvasive ventilation. We emphasize the advantages and limitations of using noninvasive ventilation to treat acute respiratory failure due to sea water drowning syndrome.
Keywords: Noninvasive ventilation, Drowning, Acute respiratory failure, Epilepsy
List of abbreviations: ARDS, Acure Respiratory Distress Syndrome; ARF, Acute Respiratory Failure; CRP, C-reactive protein; PEEP, Positive End Expiratory Pressure; PS, Pressure Support; MV, Mechanical ventilation; NIV, Noninvasive ventilation; RF, Respiratory Frequency; VES, Erythrocyte sedimentation rate
1. Introduction
Drowning is a global problem that affects all populations, and continues to be a leading cause of morbidity and mortality around the world [1], [2]. The World Health Organization (WHO) reports that every hour of every day, more than 40 people lose their lives to drowning; 372,000 deaths each year [3], more than 4000 alone in the United States [4]. Pulmonary oedema and acute respiratory failure (ARF), are the main components of drowning pathophysiology, frequently evolving to acute respiratory distress syndrome (ARDS), and sometimes causing circulatory dysfunction and cardiac arrest [5], [6]. Despite extensive literature on drowning, clinical data are still lacking on the best medical strategy to use [5]. Conventional mechanical ventilation is generally used in patients with severe ARDS after drowning. Recently, noninvasive ventilation (NIV) has been used to treat more severe cases of patients with acute respiratory failure [7]. We report the case of a 45 year old man with a history of epilepsy and mental handicap who developed acute respiratory failure secondary to salt-water drowning, who was successful treated with noninvasive ventilation.
2. Case presentation
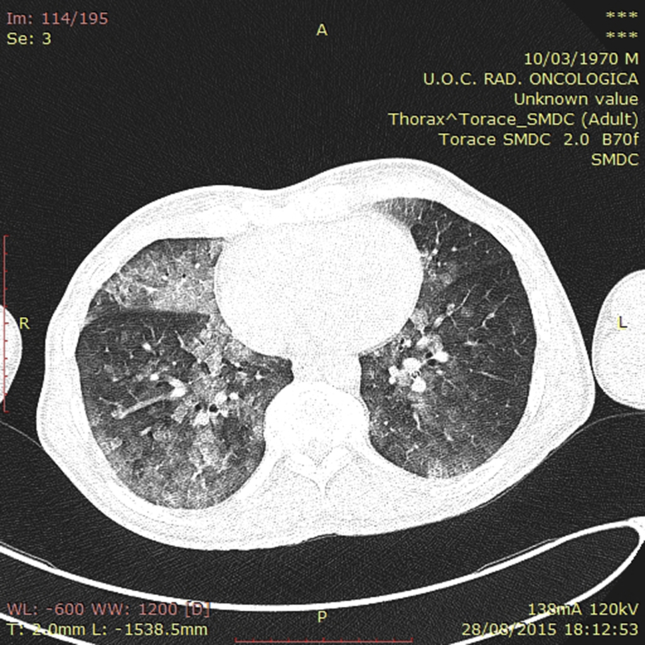
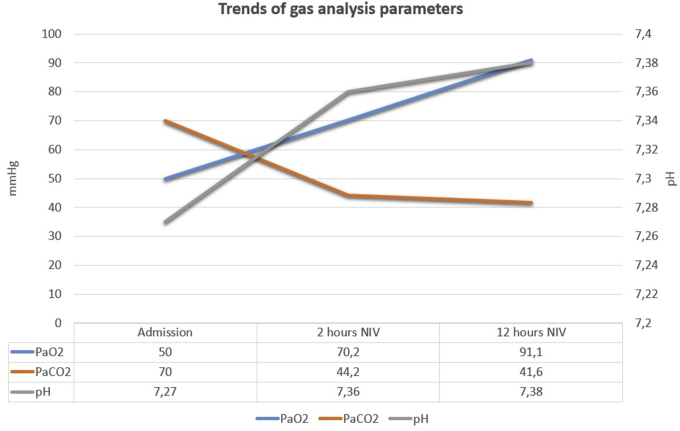
The case concerns a 45-year-old (height 170 cm/weight 75 Kg, BMI 25) Caucasian man, never smoker, with history of epilepsy with mental retardation and behavioral problems. While he was lying on the foreshore, the patient developed an epileptic crisis with loss of consciousness and inhalation of sea water. Bystanders reported that submersion duration was less than 1 min, and cardiopulmonary resuscitation by emergency medical service was not necessary. The patient was transported to the accident and emergency department in acute respiratory failure, and initially treated with a high dose of oxygen (FiO2 60% Venturi Mask 12 L/m). On admission, the patient presented a moderate impaired sensorium (GCS 12). Physical examination revealed the presence of bilaterally inspiratory and expiratory coarse breath sounds. Chest x-ray revealed diffused patchy bilateral opacities. Chest CT confirmed mixed consolidation/ground glass opacifications (Fig. 1). Serum blood analysis revealed only mild elevation of CRP, VES and fibrinogen with normal leucocytes. Arterial blood gas-analysis during oxygen therapy (FiO2 60%) documented acute decompensated respiratory acidosis with severe hypoxemia and hypercapnia (pH 7.27; PaO2 50 mmHg; PaCO2 70 mmHg; Sat 80%; HC 25.2 mEq/L). The patient was admitted to the Respiratory Intermediate Care Unit (RICU) and an NIV trial session was decided and promptly started. A Viasys Healthcare Vela Ventilator (Carefusion, Savi Ranch Parkway Yorba Linda, CA, USA) was used with a Fisher & Paykel 431 NIV nasobuccal mask (medium) (Fisher & Paykel Healthcare, Panmure, Auckland, New Zeland). Ventilator setting was: pressure support (PS) 10 cmH2O; positive end-expiratory pressure (PEEP) 5 cmH2O; respiratory frequency (RF) 10; inspiratory trigger 1 L/min; inspiratory time (Tinsp) 0.8 s; FiO2 50%. The patient was administered intravenous moderate dosage corticosteroid (prednisone 80 mg) and antibiotic (Piperacillin/Tazobactam 4 g/0.5) therapy. At the beginning, the patient manifested good tolerance toward assisted ventilation procedure, with stabilization of oxygen saturation above 94%, so FiO2 was progressively decreased to 35%. A 10 ml/kg target expiratory tidal volume was set during the first hour of ventilation: it was achieved with a progressive increase of PS from 10 cmH2O to 15 cmH2O. No change in PEEP was adopted. After 2 h of assisted ventilation, a second arterial blood gas analysis was performed with evidence of significant improvement (pH 7.36, pO2 70.2 mmHg, pCO2 44.2 mmHg, HC 24.4 mmol/L, BE -1.2 mmol/L). After 12 h of assisted ventilation, a third blood gas analysis documented a complete resolution of acute respiratory failure (pH 7.38, pO2 91.1 mmHg, pCO2 41.6 mmHg, BE -0.9 mmol/L, HC 24.2 mmol/L) so NIV was stopped and patient was treated with low flow oxygen therapy (2 L/min by nasal cannule). Trends of gas analysis parameters were reported in Graph 1.
Fig. 1.
Chest computed tomography on admission shows mixed consolidation/ground glass opacifications.
Graph 1.
Trends of gas analysis parameters.
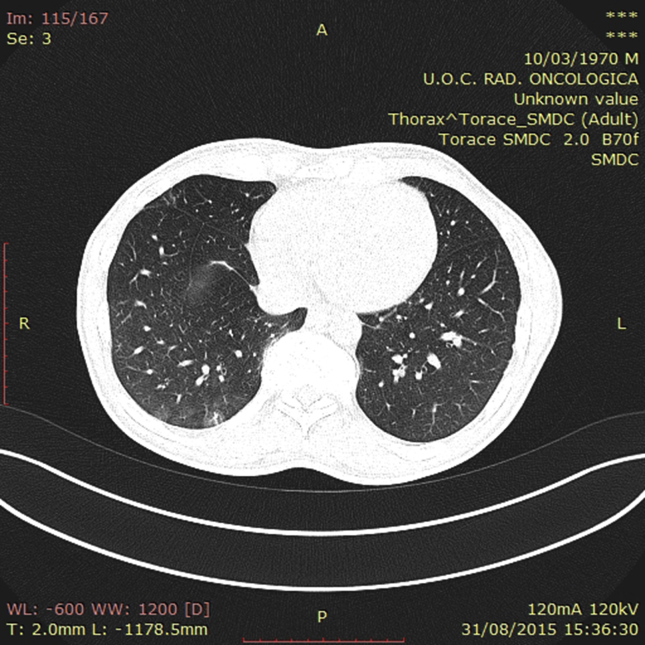
Vital signs were stable over the successive 48 h with valid diuresis and progressive improvement of consciousness (GCS 14). After 72 h from admission, a control chest CT revealed a significant reduction of alveolar and ground glass opacities (Fig. 2). After 96 h, the patient was discharged in a stable condition.
Fig. 2.
After 72 h from admission, a control chest CT revealed a significant reduction of mixed consolidation/ground glass opacifications.
3. Discussion
Drowning comprises a heterogeneous group of conditions with a wide spectrum of severity [8]. Although the outcome of patients after accidental submersion in a liquid medium is related mainly to the presence or absence of anoxic encephalopathy, acute respiratory failure (ARF) is very common in these patients [6]. Pulmonary oedema is commonly encountered after initial resuscitation. The first 12 h after an accident are crucial as a patient's condition may deteriorate suddenly due to development of ARDS [9]. People with epilepsy have increased risk of injury from submersion especially if they are unaccompanied during swimming but also when they stay on the foreshore, as in the case described [10]. As stated above, the sequelae from a drowning incident vary greatly based on numerous factors, but the primary physiologic insult is always hypoxia. This is the starting point for all morbidity and mortality, and it must remain the focus of treatment [1]. Thus, correction of hypoxemia by ventilation-only resuscitation is critical [3], and medical ventilation is the milestone treatment [4].
Clinical data are still lacking on the best medical ventilation strategy to be used [5]. Despite the absence of recommendations for NIV use in the case of drowning-related ARF, this technique has been previously used, with safety and efficacy [5].
In a retrospective cohort study, among 126 patients, 38 patients with cardiac arrest at the scene were not analyzed, 26 received mechanical ventilation (MV), and 48 patients received noninvasive ventilation (NIV). Compared with patients placed under MV, the NIV patients presented a better initial neurological (Glasgow Coma Scale of 7 ± 4 vs. 12 ± 3, P < 0.05) and hemodynamic status from the pre-hospital stage (mean arterial pressure of 77 ± 18 vs. 96 ± 18, P < 0.001). With comparable ARF-related hypoxemia to MV, NIV was maintained with success in 92% (44/48) of cases. Both MV and NIV were associated with rapid improvement of oxygenation and short ICU length of stay 3 (1–14) and 2 (1–7) days, respectively [5].
In the last twenty years, NIV has profoundly changed the approach to patients with ARF, reducing length of stay and avoiding the complications of endotracheal intubation [7]. Many studies support new and unusual applications of NIV [11]. Although loss of consciousness could be a limiting factor in applying NIV, several patients with hypercapnic encephalopathy syndrome have been successfully treated with this technique [12]. Only in awake patients who are breathing spontaneously has nasal continuous positive airway pressure been reported to be beneficial in fresh-water drowning [13]. In this case, a non-invasive positive-pressure ventilation (NPPV) modality of ventilation was chosen to support respiratory muscles and a PEEP was applied to recruitment of atelectatic regions and reducing shunt. In our case, we believe that NIV played a role in preventing ARDS development. We feel that well designed, randomized trials examining the use of NIV in acute respiratory failure secondary to drowning are warranted.
4. Conclusion
Acute respiratory failure secondary to submersion injury is a frequent condition with high morbidity and mortality. NIV represents an effective approach avoiding more severe complications due to conventional ventilation.
Consent
Written informed consent was obtained from patient's guardian (sister) for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Conflict of interest
The authors declare that they have no competing interests.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not for-profit sectors.
Author's contribution
P.R. contributed substantially to conception, design and drafting of case report manuscript.
S.C. was involved in data acquisition.
A.B. was involved in imaging acquisition.
G.G. and V.F. have been equally involved in critically revising the manuscript.
References
- 1.Schmidt A., Sempsrott J., Havryliuk T., Semple-Hess J. Drowning in the adult population: emergency department resuscitation and treatment. Emerg. Med. Pract. 2015;17(5):1–20. [PubMed] [Google Scholar]
- 2.Buggia M., Canham L., Tibbles C., Landry A. Near drowning and adult respiratory distress syndrome. J. Emerg. Med. 2014;46(6):821–825. doi: 10.1016/j.jemermed.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Truhlar A., Deakin C.D., Soar J., Khalifa G.E., Alfonzo A., Bierens J.J. European resuscitation council guidelines for resuscitation 2015: section 4. Cardiac arrest in special circumstances. Resuscitation. 2015;95:148–201. doi: 10.1016/j.resuscitation.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 4.Kleinman M.E., Brennan E.E., Goldberger Z.D., Swor R.A., Terry M., Bobrow B.J. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl. 2):S414–S435. doi: 10.1161/CIR.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 5.Michelet P., Bouzana F., Charmensat O., Tiger F., Durand-Gasselin J., Hraiech S. Acute respiratory failure after drowning: a retrospective multicenter survey. Eur. J. Emerg. Med. off. J. Eur. Soc. Emerg. Med. 2015 doi: 10.1097/MEJ.0000000000000362. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Salomez F., Vincent J.L. Drowning: a review of epidemiology, pathophysiology, treatment and prevention. Resuscitation. 2004;63(3):261–268. doi: 10.1016/j.resuscitation.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Nava S., Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374(9685):250–259. doi: 10.1016/S0140-6736(09)60496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Szpilman D. Near-drowning and drowning classification: a proposal to stratify mortality based on the analysis of 1,831 cases. Chest. 1997;112(3):660–665. doi: 10.1378/chest.112.3.660. [DOI] [PubMed] [Google Scholar]
- 9.Pratt F.D., Haynes B.E. Incidence of “secondary drowning” after saltwater submersion. Ann. Emerg. Med. 1986;15(9):1084–1087. doi: 10.1016/s0196-0644(86)80133-0. [DOI] [PubMed] [Google Scholar]
- 10.Beghi E. Accidents and injuries in patients with epilepsy. Expert Rev. Neurother. 2009;9(2):291–298. doi: 10.1586/14737175.9.2.291. [DOI] [PubMed] [Google Scholar]
- 11.Ambrosino N., Guarracino F. Unusual applications of noninvasive ventilation. Eur. Respir. J. 2011;38(2):440–449. doi: 10.1183/09031936.00192810. [DOI] [PubMed] [Google Scholar]
- 12.Scala R. Hypercapnic encephalopathy syndrome: a new frontier for non-invasive ventilation? Respir. Med. 2011;105(8):1109–1117. doi: 10.1016/j.rmed.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Dottorini M., Eslami A., Baglioni S., Fiorenzano G., Todisco T. Nasal-continuous positive airway pressure in the treatment of near-drowning in freshwater. Chest. 1996;110(4):1122–1124. doi: 10.1378/chest.110.4.1122. [DOI] [PubMed] [Google Scholar]