Abstract
Objectives
To identify which MCH services delivered by local health departments (LHD) appear associated with reducing differences in Black-White mortality.
Methods
We used a time-trend design to investigate relationships between change in MCH activities provided by LHDs in 1993 and in 2005 and changes in 1993–2005 Black-White mortality disparities. Secondary data were analyzed for 558 U.S. counties and multi-county districts. Independent variables included the six MCH services provided by LHDs and captured in the 1993 and 2005 NACCHO Profile of Local Public Health Departments surveys. MCH service variables represented change in each service from 1993 to 2005. Control variables included selected LHD characteristics and county-level socioeconomic, demographic, and health provider resource data. Absolute change in Black and White mortality rates and changes in the mortality disparity “gap” between these rates in 1993 and 2005 were examined as dependent variables.
Results
Among the MCH service examined, prenatal care had a significant beneficial relationship with Black all-age mortality change and with reducing the mortality “gap.” Family planning services had a beneficial relationship with reducing the mortality “gap” for females in the jurisdictions in the study sample. WIC services indicated the most consistently beneficial relationship with both Black mortality and White mortality change, but these changes did not influence the mortality “gap” during the study period.
Conclusions
LHD delivery of family planning and prenatal care by LHDs appears related to reductions in Black-White mortality disparities. Implications of this study suggest the importance of certain MCH services for reducing Black-White mortality disparities.
Keywords: public health systems, mortality, health disparities, prenatal care, preventive services, prenatal care
Background
The publication of Healthy People 2000 in 1991 was the first coordinated attempt to focus national attention and specific efforts on addressing the need to equalize health status among racial and ethnic groups in the U.S. (1). Nonetheless, 20 years later health disparities persist (2). In terms of mortality disparities, 1993 is considered an unfortunate “high point in the life expectancy gap” between African American and White residents in the U.S. (3). Overall Black-White disparities in life expectancy have declined since 1993, but this decline is uneven relative to specific age groups (3), and Black-White disparities in mortality did not improve at all for U.S. infants from 1990 to 2005 (2).
Research indicates that focused prevention and primary care interventions intended to reach specific vulnerable populations can reduce mortality disparities and improve health outcomes, particularly among women and infants (4, 5, 6). Health promoting interventions for women and children include prenatal and obstetrical care (7), family planning (8), the federal Women Infants and Children (WIC) Supplementary Nutrition Program (5, 6), and Medicaid’s Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) (9). Local health departments (LHD) have been major providers of these basic, preventive maternal and child health (MCH) services to vulnerable populations (10).
The National Association of County and City Health Officials (NACCHO) has articulated the role of a “functional LHD” and states that “everyone, no matter where they live, should reasonably expect” the LHD in their jurisdiction to be addressing health disparities among other functions (11). The activities that LHDs undertake to improve health in their communities and address these disparities, however, have been changing dramatically in recent decades due to trends toward more population-focused services, budget cuts, and the growth of alternative service providers (8, 12, 13, 14). The long-held tradition of LHDs providing MCH services has been one of those areas that has undergone some of the most dramatic change (12).
While LHDs vary in the services they provide and how they are organized, over half of the nation’s LHDs provide certain MCH-related services such as immunizations, WIC, and family planning (15). Other services, such as obstetrical and prenatal care, were provided directly by only 16% and 42% of LHDs, respectively, in 2005, with these percentages decreasing in 2008 (15). These NACCHO reports suggest there are major differences in emphasis of MCH service provision across agencies and jurisdictions. Existing local variation in service delivery may be exacerbated by national public health practice shifts away from individually-oriented direct services (such as prenatal care) and toward more population-focused activities (such as community assessment, epidemiology and surveillance) (12, 16, 17).
In light of dramatic budget cuts currently being made by LHDs, it is particularly important to understand the nature of the MCH services provided by LHDs and which ones favorably impact population health and disparities (18). MCH services are among the LHD service areas receiving some of the biggest cuts in capacity and activity (12). As LHD leaders make difficult program decisions during this financial crisis, even as disparities continue and increase on some MCH-related indicators (2, 19, 20), they struggle to develop and make use of evidence in support of what specific practices do and do not impact the health of vulnerable populations in their communities and for what cost (21, 22). LHD leaders and policy makers need evidence for decision-making about what types of agencies and providers should perform certain preventive services--particularly those provided at the more intensive, individual level such as family planning and prenatal care--and what mechanisms related to specific systems and approaches to service provision drive population health improvements and the elimination of disparities.
In a related study to the one reported here, our research team examined the relationship of 11 different domains of LHD practice (e.g. Environmental Health, MCH, Epidemiology and Surveillance) and the relationship of these program domains to changes in Black-White mortality disparities over time (23). Findings indicate that the breadth of MCH services provided directly by LHDs had a significant relationship to reductions in the Black-White mortality gap from 1993 to 2005 (23). Given these findings, we then investigated, in this study, the individual MCH services provided by LHDs to identify specific MCH practices associated with reductions in this mortality disparity “gap.”
Methods
We compiled a linked data set of national, county-level data to identify which MCH services delivered by LHDs were related to reduced mortality rates for Black and for White residents, respectively, and which MCH services appeared to mitigate health disparities by reducing 1993–2005 differences in Black-White mortality rates. Our study received an exemption by the University of Washington’s Institutional Review Board.
Data sources included the 1990 and the 2000 national U.S. Census, the CDC Wonder data base, Health Resources and Services Administration’s (HRSA) Area Resource File of local-level health resources, and the 1993 and the 2005 NACCHO Profile of Local Public Health Departments (Profile) surveys. The dependent variables were changes in mortality rates, measured as the absolute change in all-cause, age-adjusted mortality rates from 1993 to 2005 for Black residents and for White residents in a county (or multi-county) jurisdiction. Changes in mortality rates from 1993 to 2005 were included for Black and for White all-age groups, for 15–44 year olds, for females, and for infants (birth to 12 months). Infant mortality rates were constructed for 3 year periods (1992–94 and 2003–05) to accommodate for small sample sizes. The difference between the 2005 Black-White disparity in mortality and the 1993 Black-White disparity in mortality for each group depicted change in the Black-White disparity gap (24). This “difference in the annual differences” was used by the research team in a previous study (24) and is shown in the equation below, with negative scores indicating a narrowing of the disparity gap:
Difference in Black-White Mortality Gap = (2005 Black Mortality Rate – 2005 White Mortality Rate) – (1993 Black Mortality Rate – 1993 White Mortality Rate)
Independent variables included the five MCH services provided by LHDs that were comparable across the two 1993 and 2005 NACCHO Profile surveys. The MCH variables we ultimately used in our regression models were limited to 5 binary epidemiological measures of whether or not an LHD had ever or never directly provided Family Planning, Prenatal Care, Obstetrical Care, WIC, or EPSDT services in 1993 and/or 2005.
Control measures included selected community characteristics based on county-level socio-demographics that have been found to be related to health outcomes and differential risk (10, 25, 26, 27), general local health resources per capita that may be affecting local health outcomes and the services that LHDs chose to provide (28, 29), and basic LHD characteristics that have been shown to relate to LHD performance and the mix of provided services (30, 31, 32). A similar set of covariates, including the socioeconomic disadvantage index (SDI) developed by Robert and Reither (26), were used in our previous study of 11 LHD service domains (23). Robert and Reither’s SDI measured “community disadvantage” by summing county-level variables from the U.S. Census that represent percent of households on public assistance, percent of families below the local median family income, and percent unemployment. Except for variables specific to geography (i.e. rural/urban classification, federal region), our regression model used largely time-variant control variables, measuring change in these variables over two time points in time, 1990 and 2005. We included the following covariates in every regression model: change in each of percent foreign born residents, percent Black residents, percent residents with high school diploma, SDI, nurses and physicians per capita, LHD full time employees, existence of a LHD Board of Health, whether or not the LHD lead executive was a clinician.
Sample
Our national dataset of 558 “common local areas” represented mostly (82.4%, n=460) county jurisdictions with local-level data and an LHD serving a county-wide jurisdiction. Other “areas” contained data with multiple municipal LHDs aggregated to the county level (11.5%, n=64 areas) and multi-county LHD jurisdictions (4.8%, n=27) with data linked at the multi-county level. A few LHD cases (1.3%, n=7) were combined into small regions and aggregated to the county or multi-county level, when LHDs did not fit standard county or municipal designations (23). Since the focus of our study is on reductions in the Black-White disparity gap, we limited our sample to those “areas” with statistically measurable Black mortality that was greater than the measurable White mortality in 1993 or 2005. The few jurisdictions in which Black mortality was less than White mortality were, therefore, excluded.
Analysis
To compare our sample with the nation as a whole, descriptive statistics were calculated along with examining the distribution of the specific MCH services among LHD areas. We examined the change in the provision of each MCH service across LHDs by computing whether each MCH service was “discontinued”--conducted in 1993 but discontinued in 2005; “initiated”--not conducted in 1993 but conducted in 2005; “had no activity”-- not conducted in either 1993 or 2005); or was “maintained”--conducted by the LHD in both 1993 and 2005.
To examine the relationship between individual MCH services provided by LHDs and changes in mortality and disparities, we estimated separate linear regression models that defined each MCH service as a binary variable of a service ever or never provided in 1993 or 2005. Since the five binary MCH service variables ultimately included in the model were all significantly (and positively) correlated with each other (with coefficients ranging from 0.271 to 0.606), we estimated models for each MCH service separately rather than reduce power and interpretability by modeling the service items together. We used robust standard errors to adjust for within state clustering of LHDs.
Results
Table 1 displays the characteristics of our sample, which over-represented urban areas and regions in the southern U.S. The socio-demographics of these areas were similar at baseline to counties across the national as a whole, but had a higher proportion of Black residents and a slightly higher overall percentage of foreign born residents and of people on public assistance. Our sample also had a higher density of nurses and general practice physicians than the nation as a whole. The LHDs in the sample were less likely to have a physician as lead executive by 2005 than they were in 1993, and they were likely to be governed by a local Board of Health (BOH) in both years.
Table 1.
Characteristics of the local areas sampled and the related Local Health Departments (LHD).
| 10 Federal Regions |
N (%) | |
|---|---|---|
| Region 1 | Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont | 15(2.7) |
| Region 2 | New Jersey, New York | 36(6.5) |
| Region 3 | Delaware, District of Columbia, Maryland, Pennsylvania, Virginia, West Virginia | 52(9.3) |
| Region 4 | Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee | 258(46.2) |
| Region 5 | Illinois, Indiana, Michigan, Minnesota, Ohio, Wisconsin | 69(12.4) |
| Region 6 | Arkansas, Louisiana, New Mexico, Oklahoma, Texas | 68(12.2) |
| Region 7 | Iowa, Kansas, Missouri, Nebraska | 22(3.9) |
| Region 8 | Colorado, Montana, North Dakota, South Dakota, Utah, Wyoming | 5(0.9) |
| Region 9 | Arizona, California, Hawaii, Nevada | 25(4.5) |
| Region 10 | Alaska, Idaho, Oregon, Washington | 8(1.4) |
| Community Characteristics |
All U.S. Counties 1989 (N=3225) |
“Common Local Areas” in Sample (N=558) | ||
|---|---|---|---|---|
| Mean ± SD | 1990 Mean ± SD |
2000 Mean ± SD |
2000-1990 Change Mean ± SD |
|
| Rate of unemployment (age 16+) | 5.9 ± 3.0 | 6.0 ± 2.2 | 4.6 ± 2.2 | −1.4 ± 1.7 |
| % of families with incomes less than the 1989 (and 1999) median family income | 58.9 ± 12.6 | 52.6 ± 13.9 | 50.3 ± 12.7 | −2.3 ± 3.5 |
| % of households receiving public assistance | 8.5 ± 4.5 | 9.1 ± 4.7 | 3.5 ± 1.7 | −5.7 ± 3.6 |
| % foreign born | 2.3 ± 3.6 | 3.4 ± 4.5 | 5.6 ± 6.4 | 2.09 ± 2.3 |
| % Black | 8.6 ± 14.3 | 18.3 ± 15.6 | 19.0 ± 15.7 | 0.73 ± 4.2 |
| % persons age +25 with high school diploma or more | 69.6 ± 10.4 | 69.1 ± 12.1 | 77.0 ± 8.3 | 7.92 ± 7.1 |
| # of MDs per 100,000α | 52.7 ± 218.6 | 56.0 ± 30.1 | 70.8 ± 39.9 | 14.8 ± 24.6 |
| # of Nurses per 100,000β | 584.5 ± 1952.9 | 667.6 ± 280.2 | 557. 1 ± 525.3 | −110.9 ± 602.9 |
| LHD Agency Characteristics |
1993 | 2005 | 2005-1993 Change | ||||
|---|---|---|---|---|---|---|---|
| N (%) | Mean ± SD |
N (%) | Mean ± SD |
N (%) | Mean ± SD |
||
| Governed by a Board of Health | 403(72.2) | 393(70.4) | −10(−2.5) | ||||
| Profession of LHD Lead Executive | RN &/or BSN | 93(16.7) | 125(22.4) | 32(34.4) | |||
| Physician | 261(46.8) | 162(29.0) | −99(37.9) | ||||
| Non-clinician | 206(36.9) | 273(48.9) | 67(32.5) | ||||
| # staff FTEs | 134.0 ± 280.2 | 153.9 ± 384.3 | 19.9 ± 475.6 | ||||
Medical Doctors (MD) represents general and medical specialty physicians per 100,000 population
Nurses represents Registered Nurses physicians per 100,000 population
Overall mortality rates for our sample were consistently higher for Black residents than for White residents among all-ages, females, aged 15–44 residents, and infants (Table 2). Mortality rates, as well as the gap in Black-White mortality rates, declined from 1993 to 2005.
Table 2.
Descriptive Statistics of 1993, 2005 and 1993–2005 Change in Mortality Rates.
| Mortality Rate | 1993 U.S. Mortality |
Number of Areas |
1993 Ave (St Dev) |
2005 Ave (St Dev) |
2005-1993 Ave Change (St Dev) |
|
|---|---|---|---|---|---|---|
| All-Age, All-cause, age adjusted | 519 | |||||
| Black | 1216 | 1236 (193) | 1075 (216) | −161 (230) | ||
| White | 870 | 942 (107) | 863 (130) | −79 (96) | ||
| Gap | 346 | 294 (195) | 212 (183) | −82 (232) | ||
| Female, age adjusted | 386 | |||||
| Black | 948 | 982 (160) | 884 (153) | −98 (176) | ||
| White | 698 | 750 (82) | 715 (100) | −35 (89) | ||
| Gap | 250 | 232 (159) | 170 (138) | −63 (177) | ||
| Ages 15–44 | 166 | |||||
| Black | 323 | 318 (95) | 221 (62) | −96 (81) | ||
| White | 135 | 142 (37) | 129 (38) | −13 (40) | ||
| Gap | 188 | 175(81) | 92 (53) | −83 (67) | ||
| 1992–94 Ave (St Dev) |
2003–05 Ave (St Dev) |
(2003–05)-(1992–94) Ave Change (St Dev) |
||||
| Infant Mortality | 150 | |||||
| Black | 16.52 | 16.85(3.36) | 13.43 (3.66) | −3.42 (4.17) | ||
| White | 6.82 | 6.85(1.33) | 6.07 (1.49) | −7.9 (1.37) | ||
| Gap | 9.7 | 10.00 (3.21) | 7.36 (3.11) | −2.64 (4.08) | ||
Note: All-ages and Ages 15–44 are per 100,000 residents; Infants are per 1,000 residents
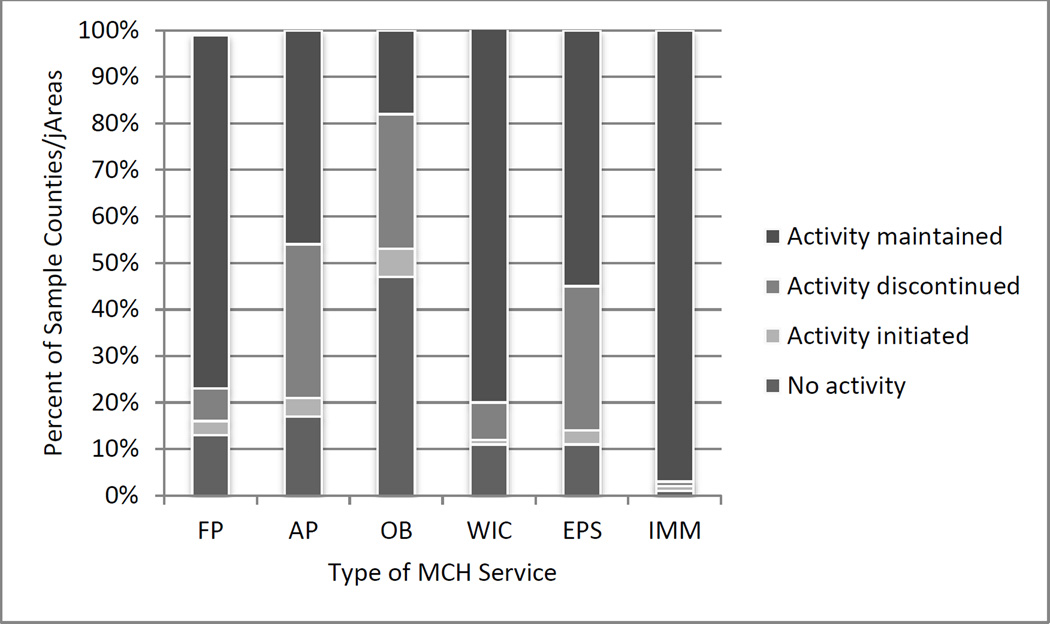
When change in the provision of MCH services was examined, Immunization services remained largely unchanged and were provided by nearly 100% of the LHDs in the sample (Figure 1). Obstetrical Care was by far the activity most likely to no longer be provided in 2005—both through discontinuation and with no service provided in both of years 1993 and 2005. The provision of Family Planning (76% of area cases in the sample, n=425) and WIC (81% of cases, n=451) remained relatively stable across in 1993–2005, while 33% (185 cases) discontinued Prenatal Care and 29% (163 cases) discontinued Obstetrical Care.
Figure 1.
Percent of counties or areas in sample with changes in MCH service delivery from 1993 to 2005 (n=558).
NOTE: FP = Family Planning, AP represents Antenatal (Prenatal) Care, OB represents Obstetrical Care, WIC represents Women Infants and Children Supplementary Nutrition Program, EPSDT represents Medicaid’s Early and Periodic Screening, Diagnosis, and Treatment, IMM represents Immunizations
Significant relationships existed between the maintenance of the provision of FP (43.78, p<0.001), WIC (13.49, p<0.001), Immunizations (6.28, p<0.05), and EPSDT (11.61, p<0.001) and jurisdiction size (urban, large town, or small town/rural). FP, WIC, and Immunizations were significantly more likely to have been provided in both survey years in smaller jurisdictions. EPSDT was more likely to have been provided in both years in larger jurisdictions. We also found significant relationships between some of our socio-economic variables and the maintenance of these MCH services over time. Greater1990 community socioeconomic disadvantage (SDI) and higher percentages of Black residents in a county were significantly (all at p<0.01) related to LHDs having maintained Family Planning, WIC, and EPSDT services in a jurisdiction, with coefficients ranging from 0.200 to 0.315.
Linear regression models indicated that the provision of certain MCH services were associated significantly with changes in mortality rates and in reductions in the Black-White mortality gap (Table 3). LHDs that had ever provided Prenatal Care (−78.23, p <0.10) were related significantly with a greater decline in all-age/gender Black mortality rates. LHDs that had ever provided Family Planning (−43.95, p <0.10) and/or WIC (−47.48, p <0.10) were associated with reductions in female Black mortality rates. No significant relationships were found with Black mortality rates for the age 15–44 group and for infants.
Table 3.
Effects of MCH services provided by LHDs in 1993 and/or 2005 and change mortality rates for Black residents, White residents, and for the Black-White mortality gap.
| MCH | All ages | Ages 15–44 | Females | Infant | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Black | White | Gap | N | Black | White | Gap | N | Black | White | Gap | N | Black | White | Gap | |
| Family Planning | 434 | −21.045 | −16.495 | −4.550 | 140 | −12.896 | −16.094* | 3.199 | 320 | −43.952* | −7.447 | −36.505* | 124 | −103.009 | 5.330 | −108.339 |
| Prenatal Care | 428 | −78.231* | 29.024 | −102.254** | 144 | 16.454 | 4.763 | 11.691 | 319 | 11.500 | 22.750 | −11.250 | 129 | 9.890 | 73.078** | −63.187 |
| OB Care | 423 | −28.350 | −16.793** | −11.557 | 139 | −6.863 | −4.332 | −2.530 | 310 | 25.081 | −11.468 | 36.549* | 123 | 64.620 | 29.406 | 35.214 |
| WIC | 445 | −54.634 | −32.389** | −22.245 | 144 | −4.680 | −1.031 | −3.649 | 327 | −47.482* | −19.475* | −28.007 | 128 | −6.158 | 46.792 | −52.950 |
| EPSDT | 435 | −25.677 | −6.709 | −18.968 | 142 | −12.456 | −1.009 | −11.447 | 320 | −16.311 | 4.728 | −21.038 | 126 | 21.225 | 36.398 | −15.172 |
p-value: * <0.1
<0.05,
<0.01
Note that Immunizations was not included among the regression analyses due to lack of variation in LHD provision of immunization activities.
For White populations, greater declines in mortality rates were found to be significantly associated with Family Planning, WIC, and Obstetrical Care. These significant associations were found for White mortality rates in the 15–44 year old age group, in terms of Family Planning; and for White females, in terms of WIC, and Obstetrical Care. The only apparent significant relationship with infant mortality rates existed between Prenatal Care (73.08, p <0.05) and an increase in White infant mortality.
Prenatal Care (−102.25, p <0.05) had a strong relationship with all-age/gender reductions in the Black-White gap, and Family Planning (−36. 50, p <0.10) was also significantly associated with a decline in the Black-White gap for females. Conversely, Obstetrical Care (36.55, p <0.10) was associated unexpectedly with a widening gap for females.
No significant relationships were apparent between maintaining the provision of EPSDT service delivery and any mortality changes in the sample.
Discussion
Family Planning, Prenatal Care, and WIC appear to be those services most consistently related to favorable reductions in Black mortality and/or White mortality and, for Family Planning and Prenatal Care, favorable reductions in the Black-White mortality gap. For both Family Planning (for females) and Prenatal Care (for all-ages/genders), these favorable changes in the mortality gap appear driven by a significant decrease in Black mortality that is associated with these services and that was significantly different from the corresponding White mortality rates. At the same time, WIC is the one MCH service we examined that was significantly associated with decreases in Black and in White mortality rates for females, but these decreases did not narrow the Black-White mortality gap for females.
None of these MCH services appeared to favorably and significantly impact the Black-White infant mortality gap during the time period of this study, while for White infants there was an association with Prenatal Care and an increase in mortality. Orsi’s (2) national study of 15 health indicators and change over time from 1990–2005, showed only modest improvement on many Black-White health disparity indicators during the period she studied. For infants, she found that both White residents and Black residents had an increase in rate of low birth weight. Our results regarding infants, therefore, could reflect a response by public health officials to initiate or maintain services in the presence of detected increases in negative health outcomes for infants.
Our findings reflect a more favorable impact on mortality disparities for adult populations and no significant favorable impact on mortality for infants. This finding may reflect MCH services provided for children well before the 1993 baseline year of our study, and the ability of these prevention-oriented services, focused toward populations at risk, to have a bigger impact on health and illness over the life course, than during the isolated period of infancy. This is supported by the proliferation of epigenetic studies linking high maternal stress, poor nutrition, and other preventable in-utero risk factors with higher adult levels of cancer and chronic disease (33, 34).
Our findings and related research indicate that preventive interventions such as prenatal care, family planning, and WIC can also produce differential effects on racial and ethnic populations in local areas. LHDs tend to provide particularly targeted “safety net” services (13). The Prenatal Care and Family Planning services provided by the LHDs in our study were located in areas with high populations of African American residents and where services may have been specifically focused on African American residents and other populations at disproportionate risk for poor birth and long term health outcomes. In counties depicted in our study, where populations were perhaps equally dependent on these services, but did not have these MCH services provided by the LHD in their jurisdiction in 1993 and/or 2005, mortality disparities were not similarly narrowed. The positive effect related to LHD-provided MCH services could be indicative of wider community support for comprehensive services to women and children that is met through other community services existing along side of those provided by some LHDs and representing a general protective effect of a community-wide investment in early childhood. As public health officials also have a role in monitoring health status within their communities, the community assessment function of LHDs and detection of specific MCH needs may also have resulted in broader community support among local providers (15).
The significant beneficial relationships between LHD delivery of Family Planning and Prenatal Care services and reductions in mortality disparities are also interesting given the increase in provision of these services from other community providers during some of the same years examined in this study. The number of federally qualified health centers (FQHC) grew by 60% (from 750 to 1,200) across the U.S. between 2001 and 2007 (14). These centers often provide prenatal care along with other primary care services and are typically stand-alone community-based health centers that are usually separate from LHDs. As FQHCs serve a “safety net” role in providing care for the underserved, they serve many women and children who may have otherwise been impacted by the discontinuation of an MCH service provided by an LHD. Also, during much of the time period of this study, there was dramatic change occurring in the distribution of publicly funded family planning services. Between 1994 and 2001 many LHDs remained the primary providers of family planning services but some discontinued the provision of these services in their communities as the numbers of community health centers and other agencies providing publicly funded family planning services grew by as much as 16% (8). The growth of these alternate care providers during this time period likely helped to maintain (and perhaps grow) the level of family planning and related services in communities, perhaps contributing to the significant association that family planning services had with reducing mortality disparities. In any case, the apparent relationships between Family Planning and Prenatal Care services and reductions in Black mortality Black-White mortality disparities suggest the importance of maintaining (and, indeed, consider expanding) these services in communities with high populations of African American residents—perhaps regardless of the type of publicly-funded community agency providing the service.
Our finding that the provision of EPSDT services has no relationship to mortality change is supported by a similar finding related to other screening services focused on secondary prevention and delivered by LHDs (23). EPSDT, a Medicaid service established by the federal government in 1967, is predominately a screening activity provided by many LHDs in which assurance of regular screening for health and developmental issues among children and appropriate referrals are made, as needed (9). The focus on secondary prevention via these screening services may provide a less direct and detectable effect in relation to reducing mortality or the mortality gap.
LHD involvement in Obstetrical Care had no apparent relationship to mortality change for Black residents and was the only service associated with an increase in the Black-White mortality gap (females). These services, however, are also less comprehensive and prevention-focused than Prenatal Care, Family Planning, and WIC which indicated high positive effects in our study.
While changes over time in the number of county-wide per capita physicians and nurses was controlled for in this study, our investigation is limited by the focus on services provided by LHDs only and not other MCH services provided in a community. Our study is also limited by the services depicted in the 1993 and 2005 NACCHO Profile data as only representing little more than availability of a service, but providing no information about service volume, quality, or reach or information regarding additional services such as MCH home visiting. The two points in time (1993 and 2005) with comparable MCH service items, lends strength to our findings, but precludes causal inferences about the outcomes of specific services, since reverse or reciprocal effects may be present. The finding of race-specific differences in outcomes also suggests that other complex factors, not fully controlled for in this study, interact with mortality change differently for African American and for White residents in a county. Contributing factors, such as racism and segregation, that differentially impact Black mortality changes and birth outcomes likely played a part in mortality differences and, while we control for some features of the local area that may be associated with such unmeasured detrimental health factors, we are not able to fully control for such factors in the models examined (20).
Further research is needed with richer data and a longer time trajectory that can be used to compare the outcomes of the delivery of MCH services by a variety of public and private service providers, with data detailing variation in reach, quality, and approach to service delivery. Research is also needed to explicate the mechanisms that are seemingly at work in those MCH services and/or community-wide approaches that are most effective in reducing mortality disparities.
Conclusions/Implications
LHD delivery of family planning and prenatal care by LHDs appears related to reductions in Black-White mortality disparities. The focusing of these services on specific populations of need and through ongoing assessment and comprehensive community services may, at least in part, be the mechanisms that underlie these disparity reductions. Targeted MCH programs are needed that specifically focus on Black mortality rates and that can assure a reduction in disparities and not just overall mortality (35, 36).
Implications of this study suggest the importance of certain MCH services for reducing Black-White mortality disparities. As particularly significant cuts are being made to MCH programs and service delivery by LHDs (12), our findings underscore the need for research with a long-term trajectory to effectively measure more specific outcomes of these services and to determine what mechanisms in the provision of these MCH services provided by LHDs are the elements that appear to have the greatest relationship to disparities. In addition, more detailed information regarding the provision of service, besides presence or absence, will help further understand the relation of these mechanisms to desired outcomes. Sweeping changes to MCH services that impact these services without preserving or transitioning these seemingly important elements of service could further negatively impact disparities.
Acknowledgments
Funding support was provided from Pfizer Scholars Grants in Public Health and the University of Washington School of Nursing’s Van Hooser Gift Fund.
Contributor Information
Betty Bekemeier, University of Washington School of Nursing, Department of Psychosocial and Community Health and University of Washington School of Public Health, Department of Health Services.
David Grembowski, University of Washington School of Public Health, Department of Health Services and University of Washington School of Nursing, Department of Psychosocial and Community Health.
Young Ran Yang, University of Washington School of Nursing, doctoral student.
Jerald R. Herting, University of Washington School of Nursing, Department of Psychosocial and Community Health and University of Washington School of Arts and Sciences, Department of Sociology.
References
- 1.Brown DW. The dawn of Healthy People 2020: a brief look back at its beginnings. Prev Med. 2009;48(1):94–95. doi: 10.1016/j.ypmed.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Orsi J, Margellos-Anast H, Whitman S. Black-White health disparities in the United States and Chicago: A 15-year progress analysis. Am J of Public Health. 2010;100(2):349–356. doi: 10.2105/AJPH.2009.165407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harper S, Lunch J, Burris S, Davey Smith G. Trends in the black-white life expectancy gap in the United States, 1983–2003. JAMA. 2007;297(11):1224–1232. doi: 10.1001/jama.297.11.1224. [DOI] [PubMed] [Google Scholar]
- 4.Shin P, Jones K, Rosenbaum S. Reducing racial and ethnic health disparities: Estimating the impact of high health center penetration in low-income communities. National Association of Community Health Centers; 2003. Sep, [Accessed 01/15/08]. www.gwhealthpolicy.org/downloads/GWU_Disparities_Report.pdf. [Google Scholar]
- 5.Khanani I, Elam J, Hearn R, Jones C, Maseru N. The impact of prenatal WIC participation on infant mortality and racial disparities. Am J Public Health. 2007;100(Suppl 1):S204–S209. doi: 10.2105/AJPH.2009.168922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghosh TS, Patnaik JL, Bennett A, Trefren L, Vogt RL. Assessment of missing immunizations and immunization-related barriers among WIC populations at the local level. Public Health Rep. 2007;122(5):602–606. doi: 10.1177/003335490712200507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wightkin J, Magnus JH, Farley TA, Boris NW, Kotelchuck M. Psychosocial predictors of being an underweight infant differ by racial group: a prospective study of Louisiana WIC program participants. Matern Child Health J. 2007;11(1):49–55. doi: 10.1007/s10995-006-0129-4. [DOI] [PubMed] [Google Scholar]
- 8.Frost JJ, Frohwirth L, Purcell A. The availability and use of publicly funded family planning clinics: U.S. trends, 1994–2001. Perspect Sex Reprod Health. 2004;36(5):206–215. doi: 10.1363/psrh.36.206.04. [DOI] [PubMed] [Google Scholar]
- 9.Selby-Harrington ML, Riportella-Muller R. Easing the burden on health departments: A cost-effective method for public health nurses to increase private sector participation in the early and periodic screening, diagnosis, and treatment program. Public Health Nurs. 1993;10(2):114–121. doi: 10.1111/j.1525-1446.1993.tb00034.x. [DOI] [PubMed] [Google Scholar]
- 10.Mete C, Cioffi JP, Lichtveld MY. Are public health services available where they are most needed? An examination of local health department services. J Public Health Manag Pract. 2003;9(3):214–223. doi: 10.1097/00124784-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 11.NACCHO. Operational definition of a functional local health department. National Association of County and City Health Officials; 2005. [Accessed 01/7/08]. http://www.naccho.org/topics/infrastructure/documents/OperationalDefinitionBrochure.pdf. [Google Scholar]
- 12.NACCHO. Trends in local health department finances, workforce, and activities: Findings from the 2005 and 2008 National Profile of Local Health Departments Studies. National Association of County and City Health Officials; 2010. [Google Scholar]
- 13.Keene C, Marx J, Ricci E. Local health departments' mission to the uninsured. J of Public Health Policy. 2003;24(2):130–149. [PubMed] [Google Scholar]
- 14.Lo Sasso AT, Byck GR. Funding growth drives community health center services. Health Affairs. 2010;29(2):289–296. doi: 10.1377/hlthaff.2008.0265. [DOI] [PubMed] [Google Scholar]
- 15.NACCHO. National Profile of Local Health Departments. Washington, DC: NACCHO; 2005. [Google Scholar]
- 16.Mays G, Scutchfield F, Bhandari M, Smith S. Understanding the organization of public health delivery systems: an empirical typology. Milbank Quarterly. 2010;88(1):81–111. doi: 10.1111/j.1468-0009.2010.00590.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zahner SJ, Gredig QN. Public health nursing practice change and recommendations for improvement. Public Health Nurs. 2005;22(5):422–428. doi: 10.1111/j.0737-1209.2005.220507.x. [DOI] [PubMed] [Google Scholar]
- 18.NACCHO. Local health department job losses and program cuts: Findings from January/February 2010 survey. National Association of County and City Health Officials; 2010. May, 2010 Research Brief. [Google Scholar]
- 19.Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98(2):216–221. doi: 10.2105/AJPH.2007.114777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alio A, Richman A, Clayton H, Jeffers D, Wathington D, Salihu H. An ecological approach to understanding Black-White disparities in perinatal mortality. Mat and Child Health J. 2009;14(4):557–566. doi: 10.1007/s10995-009-0495-9. [DOI] [PubMed] [Google Scholar]
- 21.Green LW. Public health asks of systems science: To advance our evidence-based practice, can you help us get more practice-based evidence? Am J Public Health. 2006;96(3):406–409. doi: 10.2105/AJPH.2005.066035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iton AB. The ethics of the medical model in addressing the root causes of health disparities in local public health practice. J Public Health Manag Pract. 2008;14(4):335–339. doi: 10.1097/01.PHH.0000324560.42039.0e. [DOI] [PubMed] [Google Scholar]
- 23.Bekemeier B, Grembowski D, Yang Y, Herting J. Local health department changes in service: Relationships to health disparities. 2010 under review. [Google Scholar]
- 24.Grembowski D, Bekemeier B, Conrad D, Kreuter W. Are local health department expenditures related to racial disparities in mortality? Soc Sci Med. 2010;71(12):2057–2065. doi: 10.1016/j.socscimed.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 25.Rajaratnam JK, Burke JG, O'Campo P. Maternal and child health and neighborhood context: the selection and construction of area-level variables. Health Place. 2006;12(4):547–556. doi: 10.1016/j.healthplace.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 26.Robert SA, Reither E. A multilevel analysis of race, community disadvantage, and body mass index among adults in the U.S. Soc Sci Med. 2004;59(12):2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 27.Hajat A, Cilenti D, Harrison LM, D MP, Pavletic D, Mays GP, et al. What predicts local public health agency performance improvement? A pilot study in North Carolina. J Public Health Manag Pract. 2009;15(2):E22–E33. doi: 10.1097/01.PHH.0000346022.14426.84. [DOI] [PubMed] [Google Scholar]
- 28.Bigbee J. Relationships between nurse- and physician-to-population ratios and state health rankings. Public Health Nurs. 2008;25(3):244–252. doi: 10.1111/j.1525-1446.2008.00701.x. [DOI] [PubMed] [Google Scholar]
- 29.Shi L, Starfield B. The effect of primary care physician supply and income inequality on mortality among blacks and whites in US metropolitan areas. Am J Public Health. 2001;91(8):1246–1250. doi: 10.2105/ajph.91.8.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Plough A. Understanding the financing and functions of metropolitan health departments: a key to improved public health response. J Public Health Manag Pract. 2004;10(5):421–427. doi: 10.1097/00124784-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Mays GP, McHugh MC, Shim K, Perry N, Lenaway D, Halverson PK, et al. Institutional and economic determinants of public health system performance. Am J of Public Health. 2006;96(3):523–531. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mays GP, Smith SA. Effects of local public health spending on population health: Does more money matter? Health Serv Res. 2010 in press. [Google Scholar]
- 33.Thornburg KL, Shannon J, Thuillier P, Turker MS. In utero life and epigenetic predisposition for disease. Adv Genet. 2010;71:57–78. doi: 10.1016/B978-0-12-380864-6.00003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chmurzynska A. Fetal programming: link between early nutrition, DNA methylation, and complex diseases. Nutrition Reviews. 2010;68(2):87–98. doi: 10.1111/j.1753-4887.2009.00265.x. [DOI] [PubMed] [Google Scholar]
- 35.Roberts C, Algert C, Mueller L, Hadler J. Trends in infant mortality in Connecticut, 1981–1992. J Public Health Manag Pract. 1997;3(5):50–57. doi: 10.1097/00124784-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Pestronk R, Franks M REACH Team, Healthy Start Team, & PRIDE Team. A partnership to reduce African American infant mortality in Genesee County, Michigan. Public Health Rep. 2003;118(4):324–335. doi: 10.1093/phr/118.4.324. [DOI] [PMC free article] [PubMed] [Google Scholar]