Abstract
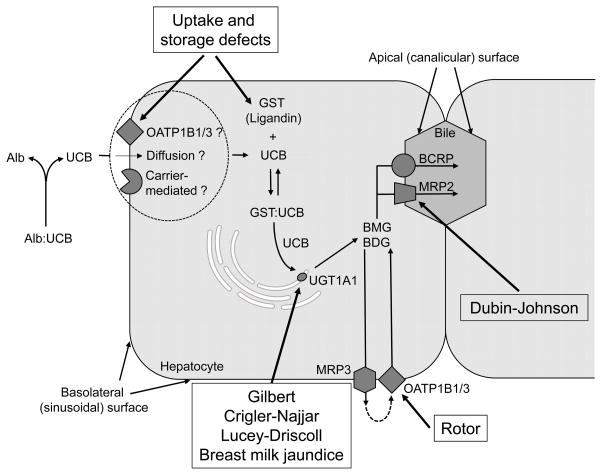
Inherited disorders of hyperbilirubinemia may be caused by increased bilirubin production or decreased bilirubin clearance. Reduced hepatic bilirubin clearance can be due to defective 1) unconjugated bilirubin uptake and intrahepatic storage, 2) conjugation of glucuronic acid to bilirubin (e.g. Gilbert syndrome, Crigler-Najjar syndrome, Lucey-Driscoll syndrome, breast milk jaundice), 3) bilirubin excretion into bile (Dubin-Johnson syndrome), or 4) conjugated bilirubin re-uptake (Rotor syndrome). In this review, the molecular mechanisms and clinical manifestations of these conditions are described, as well as current approaches to diagnosis and therapy.
Introduction
Bilirubin is the end product of heme catabolism and originates primarily from the breakdown of erythrocyte hemoglobin in the reticuloendothelial system. A smaller, yet significant proportion is derived from the breakdown of other heme proteins and ineffective erythropoiesis in the bone marrow (1). Bilirubin is poorly soluble in water and when circulating in blood, is mostly bound to serum albumin. Small amounts of unbound, unconjugated bilirubin exist in equilibrium with bound, unconjugated bilirubin in the circulation. This unbound, circulating bilirubin is neurotoxic and associated with acute bilirubin encephalopathy, which can progress to the more permanent and devastating chronic bilirubin encephalopathy, also known as kernicterus (2). Under normal conditions, unconjugated bilirubin is rapidly and selectively taken up by hepatocytes, conjugated to water-soluble bilirubin glucuronide conjugates, and ultimately secreted into bile.
Disorders that produce hyperbilirubinemia can be divided into those in which excessive bilirubin is produced (hemolysis), those in which there is decreased clearance of bilirubin (hepatic or intestinal), and combinations of the two. Newborns are particularly susceptible to developing hyperbilirubinemia as they have increased bilirubin synthesis (secondary to elevated hemoglobin concentrations and shorter red blood cell lifespan) and inefficient hepatic uptake, conjugation, and excretion of bilirubin. The aim of this review is to describe hepatic clearance of bilirubin and focus on inherited disorders of hepatic uptake, conjugation, and excretion of bilirubin.
Bilirubin Clearance by the Liver
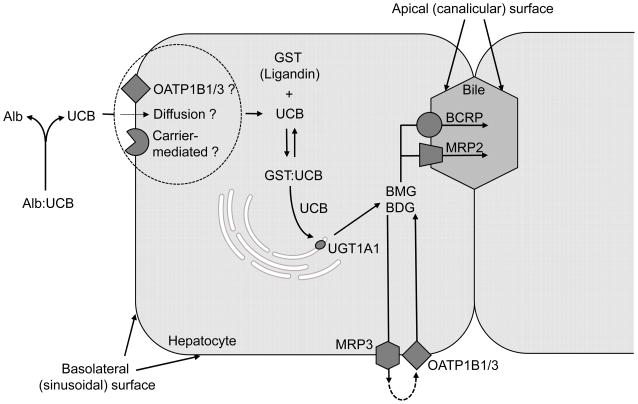
There are four major steps in hepatic clearance of bilirubin: 1) uptake and storage of unconjugated bilirubin by hepatocytes, 2) conjugation of bilirubin to bilirubin glucuronides, 3) excretion of conjugated bilirubin into bile, and 4) reuptake of conjugated bilirubin by hepatocytes.
Uptake and Intrahepatic Storage
Bilirubin dissociates from albumin before entering hepatocytes. It is not clear whether the initial uptake of free bilirubin is carrier-mediated or by passive diffusion (3). Recent studies have described a role for membrane-associated organic anion transport proteins (OATPs) in bilirubin uptake by hepatocytes. OATPs belong to the OATP superfamily, which is also known as the solute carrier organic anion transporter (SLCO) superfamily (4). Bilirubin is a known substrate for the human SLCO1B1/OATP1B1 and SLCO1B3/OATP1B3 proteins (5), but most studies have shown that it is conjugated (as opposed to unconjugated) bilirubin that is the major substrate for these transporters (5,6). OATPs therefore play an important role in the reuptake of conjugated bilirubin (see Secretion into Plasma and Reuptake and Rotor Syndrome). However, there is evidence from genome-wide association studies that polymorphisms resulting in decreased SLCO1B1/OATP1B1 or SLCO1B3/OATP1B3 activity are associated with higher serum levels of both conjugated and unconjugated bilirubin (7,8), suggesting a role for OATPs in the initial uptake of unconjugated bilirubin into hepatocytes as well.
Once inside the hepatocyte, bilirubin binds to the cytoplasmic transport protein ligandin, which belongs to the glutathione-S-transferases (GST) family. Ligandin has a much higher affinity for bilirubin than albumin, and therefore facilitates intrahepatocyte bilirubin accumulation and storage (9).
Conjugation
After binding to ligandin, bilirubin is transported to the smooth endoplasmic reticulum, the site at which the conjugating enzyme, uridine diphosphate glucuronosyl transferase 1A1 (UGT1A1) is localized. UGT1A1 is a transmembrane protein that has a binding site for bilirubin and another one for uridine diphosphate glucuronic acid. Conjugation is a two-step process; in the first step, the UGT1A1 enzyme catalyzes the transfer of one glucuronic acid molecule to one of the carboxyl groups on bilirubin forming bilirubin monoglucuronide. Addition of another molecule of glucuronic acid to the second carboxyl group forms bilirubin diglucuronide. Both bilirubin mono- and diglucuronide are water-soluble and can readily be excreted in bile.
Excretion into Bile
Once bilirubin glucuronide leaves the endoplasmic reticulum and is transported into the cytoplasm, it can diffuse toward either the apical surface of the hepatocyte (canalicular surface) or the basolateral surface (sinusoidal surface). At the canalicular surface, it is efficiently secreted into bile via ATP-binding cassette (ABC) transporters. The predominant ABC transporter responsible for bilirubin excretion is the multidrug resistance-associated protein ABCC2/MRP2 transporter (10). Recently, another ABC transporter, the breast cancer resistance protein ABCG2/BCRP has also been identified to play a role in bilirubin excretion, albeit to a lesser degree (11).
Secretion into Plasma and Reuptake
Interestingly, a substantial fraction of bilirubin glucuronide is secreted back into sinusoidal blood and subsequently taken up again by the hepatocytes for biliary excretion. The process of conjugated bilirubin excretion at the basolateral surface is mediated by the transporter ABCC3/MRP3 and reuptake is via the SLCO1B1/OATP1B1 and SLCO1B3/OATP1B3 carriers (12). Since the expression of OATP1B1 and OATP1B3 is higher in downstream hepatocytes (hepatocytes located near the central vein), it is postulated that this reuptake protects upstream hepatocytes (those located near the portal tracts) from saturating their biliary secretory capacity (9,13).
Figure 1 summarizes the transporters and enzymes involved in hepatic uptake, conjugation, secretion, and reuptake of bilirubin
Figure 1.
Schematic view of transporters and enzymes involved in hepatic bilirubin clearance. (Alb, albumin; BCRP, breast cancer resistance protein; BMG, bilirubin monoglucuronide; BDG, bilirubin diglucuronide; GST, glutathione-S-transferase; MRP, multidrug resistance-associated protein; OATP, organic anion transport protein; UCB, unconjugated bilirubin; UGT, uridine diphosphate glucuronosyl transferase).
Developmental Regulation of Transporters and Enzymes Involved in Bilirubin Clearance
All components of hepatic clearance of bilirubin are developmentally regulated and newborns have significantly reduced expression and/or activity of the transporters and enzymes involved in uptake, conjugation, and excretion of bilirubin. SLCO1B1/OATP1B1 and SLCO1B3/OATP1B3 mRNA expression is approximately 500-fold lower in neonates and 100-fold lower in infants up to the 12 months of age than in adults (14). GST has multiple classes, with proteins belonging to class alpha (GST-A) having the highest affinity to bilirubin (15). GST-A protein expression is 1.5 to 4-fold lower in newborns and reach adult levels after the first 1–2 years of life (16). UGT1A1 enzyme activity is absent from fetal livers, and is triggered in newborns by parturition (17). However, newborn UGT1A1 enzyme activity remains less than 1% of adult activity, and does not reach adult activity until 3 months of age (18). Hepatic ABCC2/MRP2 mRNA expression is 200-fold lower in neonates and 100-fold lower in infants up to 12 months of age than in adults (14). Given the reduced ability of the liver for bilirubin uptake, conjugation, and excretion, newborns are particularly susceptible to developing hyperbilirubinemia, which can improve as enzyme activities and liver function mature.
Inherited Disorders of Bilirubin Clearance
Inherited disorders involving defects in each of the four steps of hepatic bilirubin clearance have been described. Many of these disorders present in the newborn period and range in presentation from clinically insignificant to neurologically devastating and lethal.
Disorders of Uptake and Intrahepatic Storage
Disorders of bilirubin uptake and intrahepatic storage are only infrequently described in the literature (19), and the clinical significance of these disorders remains to be confirmed. Recent studies have demonstrated polymorphisms in GST genes that are associated with increased risk of neonatal hyperbilirubinemia (15,20). The most important polymorphism associated with neonatal hyperbilirubinemia is one that encodes for a partial gene deletion in the GST mu (GST-M) gene class. This GSTM1 null mutation results in complete absence of GSTM1 enzyme activity. Also, as noted above, polymorphisms in SLCO1B1/OATP1B1 and SLCO1B3/OATP1B3 may modestly contribute to unconjugated hyperbilirubinemia (7,8).
Disorders of Conjugation
Inherited disorders of conjugation are primarily due to alterations in the UGT1A1 gene, resulting in decreased or absent enzyme expression and function.
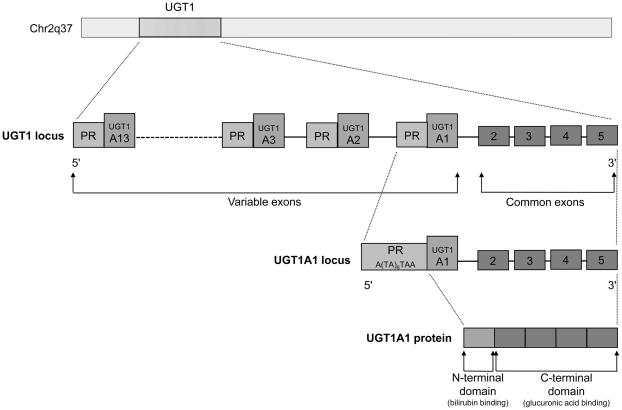
UGT Gene
The UGT gene is a superfamily of genes that encode enzymes catalyzing glucuronidation of various substrates to facilitate their excretion (21). The gene that governs bilirubin conjugation, UGT1 was cloned by Ritter et al in 1991 (22) and is located on chromosome 2, at 2q37 (23). This gene consists of four common exons (exons 2, 3, 4, and 5) and 13 unique promoter and first exons (variable exons) (Figure 2). A single variable first exon and its promoter are spliced to the four common exons prior to transcription. Of the 13 possible genes that can be encoded, only that containing the variable exon A1 is involved in bilirubin conjugation (13).
Figure 2.
Schematic representation of the UGT1 gene locus and the UGT1A1 protein. (Chr, chromosome; PR, promoter regions; UGT, uridine diphosphate glucuronosyl transferase).
UGT1A1 is the only enzyme catalyzing the generation of water-soluble bilirubin glucuronides in hepatocytes, thus mutations in this gene lead to deficiencies in bilirubin conjugation and excretion. To date, 130 UGT1A1 mutations, in both coding and non-coding regions of the gene, have been identified that decrease or abrogate enzymatic function (24). Conversely, UGT1A1 activity can be increased by phenobarbital administration, which induces UGT1A1 gene expression by activating the distal phenobarbital response enhancer element (25).
Gilbert syndrome (GS)
First described in 1901 by Gilbert and Lereboulet (26), GS is the most common hereditary hyperbilirubinemia syndrome, occurring in 3–13% of the population (27,28). It is typically associated with at least 50% decrease in hepatic bilirubin UGT activity (29). GS is now regarded as an autosomal recessive disorder, with affected patients being either homozygotes or compound heterozygotes (i.e. two different recessive alleles at a particular locus) (30). More than 100 different mutations have been implicated in GS and their frequencies differ among different ethnic groups (31). The most common genotype among Caucasians with GS is the homozygous polymorphism of two extra bases (TA) in the TATAA box sequence of the promoter region of the UGT1A1 gene, resulting in a sequence of A(TA)7TAA (also known as UGT1A1*28) instead of the normal A(TA)6TAA(32,33). The extra TA repeat lessens the affinity of TATAA-binding protein to the TATAA box, resulting in decreased gene expression. This A(TA)7TAA variant is highly prevalent in the Western population, with an allelic frequency of 0.4 ((30,34). Various other mutations, including missense mutations in the coding region are more prevalent in non-Western populations. For example, in East Asians from Japan, Korea, and China, GS most commonly results from the Gly71Arg mutation (G71R; UGT1A1*6) in exon 1 (35). The allelic frequency of the G71R mutation in this population is 0.16–0.21 (36,37), whereas the A(TA)7TAA allelic frequency is only 0.11–0.15 (36).
Clinical manifestation
Although GS is an inherited disorder, it typically first presents as mild, intermittent unconjugated hyperbilirubinemia in otherwise asymptomatic young adults without evidence of hemolysis or liver injury. GS can present in the newborn period, especially if there is concurrent hemolytic disease such as ABO incompatibility or glucose-6-phophatate dehydrogenase (G6PD) deficiency (38). Such infants are at high risk for developing severe hyperbilirubinemia and even kernicterus. GS can also contribute to neonatal hyperbilirubinemia in the absence of hemolytic disease as several authors have shown that the A(TA)7TAA homozygous genotype is associated with higher serum bilirubin levels, when compared to heterozygous and wild type controls (39–41). However, the clinical significance of this finding remains unclear as the infants in these studies had either subclinical or only mild/moderate hyperbilirubinemia (27). GS has also been associated with the jaundice of inadequate breastfeeding with weight loss (“breastfeeding jaundice”) (42,43) and with breast milk jaundice (see Breast milk jaundice) (44,45).
Diagnosis and management
In older children and adults, the diagnosis of GS can be made by administering intravenous nicotinic acid (niacin) or oral rifampin and monitoring the subsequent rise in bilirubin concentrations (46). Liver biopsy is not indicated and is usually normal. Genetic testing can be useful in the work-up of prolonged neonatal jaundice, with genotyping of the A(TA)7TAA variant in non-Asians and Gly71Arg mutation analysis in Asian patients.
Crigler-Najjar syndrome type I (CN syndrome type I)
In 1952, Crigler and Najjar (47) described the most lethal form of hereditary hyperbilirubinemia, CN syndrome type I, which is characterized by absent or nearly absent UGT1A1 enzyme activity (48). CN syndromes are inherited in an autosomal recessive manner and patients are homozygotes or compound heterozygotes. Mutations in CN syndrome type I are deleterious and consist of either premature truncation or deletion of key amino acid sequences on any of the five exons of the UGT1A1 gene (24). Additionally, intronic mutations resulting in frameshifts and premature stop codons have been described (49). The majority of the mutations found in CN syndrome type I are found in the common exons 2–5 and thus affect many UGT1 enzymes (50).
Clinical manifestation
CN syndrome type I presents shortly after birth with serum bilirubin levels greater than 20 to 50 mg/dL. Consequently, it is associated with bilirubin encephalopathy and death unless managed by aggressive phototherapy and exchange transfusions in the immediate newborn period (51). The risk for kernicterus persists into adult life (52).
Diagnosis and management
There is currently no simple test to confirm the diagnosis of CN syndrome type I. Definitive diagnosis is by gene analysis and sequencing the coding region for known mutations. Management in the newborn period consists of aggressive phototherapy and exchange transfusions to keep bilirubin levels below the threshold for kernicterus. Phototherapy for 8–12 hours daily is continued throughout the early years of life, though its effectiveness decreases with time (53). The nonsense or stop codons that cause CN syndrome type I preclude the use of phenobarbital to upregulate gene expression (54). Liver transplantation remains the only definitive treatment for this disease (55). Gene therapy may be a promising therapeutic option for these patients in the near future (56).
Crigler-Najjar syndrome type II (CN syndrome type II, aka Arias syndrome)
Described by Arias in 1962 (57), CN syndrome type II is characterized by reduced (but not abolished) UGT1A1 enzyme activity (< 10% of normal) (58). Unlike CN syndrome type I, which is caused by various types of deleterious mutations, the genetic defect in CN syndrome type II is usually a point mutation, causing a substitution of a single amino acid residue, thereby reducing but not eliminating enzyme activity (24).
Clinical manifestation
Unconjugated hyperbilirubinemia occurs in the first days of life, but total bilirubin levels usually do not exceed 20 mg/dL (51). CN syndrome type II rarely results in kernicterus. In older children and adults, illness and stress may cause temporary increases in bilirubin levels.
Diagnosis and management
CN syndrome type II can be clinically distinguished from CN syndrome type I by lower levels of bilirubin (usually less than 20 mg/dL) and a decrease in serum bilirubin levels by more than 30% after treatment with phenobarbital (58). Analysis of bile pigments for bilirubin conjugates can also differentiate the two CN syndromes, with only trace amounts of conjugated bilirubin present in type I and significant amounts of monoconjugated bilirubin present in type II (59). Treatment includes aggressive phototherapy in the newborn period and occasionally phenobarbital therapy. These patients generally have a good prognosis.
Are GS and CN syndrome type I ends of a continuous spectrum?
Historically GS, CN syndrome type I, and CN syndrome type II have been characterized as distinct clinical syndromes, distinguished by the degree of unconjugated hyperbilirubinemia. However, intermediate phenotypes have been well described, suggesting that there is a continuous spectrum of altered bilirubin conjugation (60,61). Due to the high frequency of the Gilbert-type promoter in the general population (up to 40% of the Western population has at least one Gilbert type allele), heterozygous carriers of mutations that cause CN syndromes can also carry the Gilbert-type promoter on their normal allele, resulting in compound heterozygosity and intermediate levels of hyperbilirubinemia. Therefore, the variability of the UGT1A1 gene locus most likely leads to a continuous spectrum of altered bilirubin conjugation, with GS and CN syndrome type 1 representing the two ends of the spectrum (31).
Lucey-Driscoll syndrome (aka Transient Familial Neonatal Hyperbilirubinemia)
In 1960, Lucey et al. (62) described a rare familial disorder that caused severe unconjugated hyperbilirubinemia is the first few days of life. In vitro testing demonstrated that sera of affected infants and their mothers contained an unidentified inhibitor of UGT1A1 activity. Since its original description in 1960, additional cases of Lucey-Driscoll syndrome have not been reported in the literature and its existence has been questioned.
Clinical manifestation
Based on the original description, this syndrome presents with severe hyperbilirubinemia in the immediate newborn period and can result in kernicterus and death. Children who survive the neonatal period have no recurrence of hyperbilirubinemia (62).
Diagnosis and management
The serum inhibitory effects gradually decline after delivery and therefore this is a self-resolving condition. However, given the risk of severe hyperbilirubinemia, these infants need to be monitored closely in the first two weeks of life and may need treatment with aggressive phototherapy and possibly exchange transfusion if threshold bilirubin levels are reached.
Breast milk jaundice
First described by Newman and Gross in 1963 (63), breast milk jaundice refers to a common and relatively benign cause of unconjugated hyperbilirubinemia in healthy newborns who are primarily breastfed. Its etiology remains unknown, and several components of breast milk such as pregnane-3β,20α-diol (pregnanediol) (64), other steroids (cortisol and estriol), nonesterified fatty acids (65), β-glucoronidase (66), and epidermal growth factor (67) have been implicated in its pathogenesis. Interestingly, polymorphic mutations of UGT1A1 (especially mutations seen in GS) are associated with breast milk jaundice. Specifically, studies in East Asian infants have shown a causal relationship between infants with breast milk jaundice and the G71R mutation (36,45). A recent in vitro study using transfected HepG2 cells demonstrated that pregnanediol did not alter UGT1A1 transcriptional and enzyme activity in wild-type or A(TA)7TAA variant expression vectors, but reduced enzyme activity in G71R variant vectors by 51% (68). These studies suggest that breast milk jaundice is caused by a combination of genetic and environmental factors (i.e. breast milk components).
Clinical manifestations
Breast milk jaundice develops after 4–7 days of life and can persist for as long as 3–4 months before spontaneous resolution. It is distinguished from “breastfeeding jaundice”, which occurs with mild dehydration and weight loss in the first few days of life because of insufficient intake or production of breast milk. Infants with breast milk jaundice are otherwise healthy, with normal weight gain, normal stool and urine output, and a normal physical examination. Total serum bilirubin levels usually do not exceed 12 mg/dL (69), though higher bilirubin levels and rare cases of kernicterus have been reported (70).
Diagnosis and management
Discontinuation of breast milk and substitution with formula results in rapid improvement in hyperbilirubinemia, which is both a diagnostic and therapeutic option for breast milk jaundice. However, since breast milk jaundice is a benign and self-limiting condition, current recommendations do not support discontinuation of breastfeeding in these infants (69).
Disorders of Excretion into Bile
Dubin-Johnson syndrome (DJS)
DJS was first described in 1954 by Dubin et al and Sprinz et al who reported several cases of healthy young adults with chronic low-grade jaundice (mostly conjugated hyperbilirubinemia) and black livers, with no other features of hepatobiliary disease (71,72). It is an autosomal recessive disorder and genomic studies have shown that DJS results from homozygous or compound heterozygous mutations in ABCC2/MRP2 resulting in either absent or deficient expression of this transporter (73). Several different mutations have been described in DJS patients, including exon skipping, missense, nonsense and base deletion. Most mutations result in stop codons and failure of MRP2 transcription. Less frequently, they can result in endoplasmic reticulum retention of MRP2 and failure of translocation to the canalicular membrane (9).
Clinical manifestation
DJS usually presents in young adulthood with predominantly conjugated hyperbilirubinemia and otherwise normal liver studies. The conjugated hyperbilirubinemia is mild because of urinary excretion of bilirubin glucuronides. Most patients are asymptomatic except for occasional abdominal pain (13). There is no risk of fibrosis or cirrhosis. Rarely, DJS can present in the neonatal period. Neonatal DJS differs from adult-onset DJS in that it presents with severe cholestasis and hepatomegaly. Bilirubin levels can reach > 20 mg/dL. Increased severity in neonates has been attributed to immature bile physiology combined with the MRP2 defect. As the liver matures, infants become asymptomatic until later in life, when they can present with intermittent hyperbilirubinemia (74).
Diagnosis and management
DJS in a benign disease and in adolescents and adults it does not require treatment. Diagnosis, however, is important to eliminate the possibility of other hepatobiliary disorders that may lead to hepatic injury. In addition to elevated conjugated bilirubin levels in the setting of normal liver function tests, urine tests are diagnostic. Urine tests reveal normal total coproporphyrin levels but the characterization of the coproporphyrin reveals 80% coproporphyrin I in affected individuals, compared to 75% coproporphyrin III in healthy controls (31). Coproporphyrin I is a metabolic byproduct of heme synthesis and also an endogenous substrate of MRP2; therefore serum and urinary levels are increased in the presence of defective MRP2 (73). Hepatobiliary iminodiacetic acid (HIDA) scan will show either normal or slightly delayed visualization of the liver, with absent or delayed gallbladder filling (75). Liver histology, though not necessary in establishing the diagnosis, characteristically shows the presence of dark lysosomal melanin-like pigment deposits (12). Genotyping of ABCC2 gene is possible, but typically not part of the routine clinical work up (31).
DJS should be suspected in any neonate with unexplained prolonged moderate to severe conjugated hyperbilirubinemia. Similar to adults, diagnosis is made by elevated urine coproporphyrin I levels. Computerized tomography (CT) of the abdomen can also be done and will show attenuation of the liver (75). Therefore, characterization of urinary coproporphyrins and abdominal CT should confirm the diagnosis without additional invasive means. Given the significant cholestasis that occurs in this age group, treatment with phenobarbital and ursodeoxycholic acid is recommended (74).
Disorders of Reuptake
Rotor syndrome (RS)
RS was first described by Rotor et al in 1948 and was initially considered a variant of DJS (76). Subsequently, a number of functional studies confirmed that patients with RS do not have defective biliary excretion, but rather a defect in hepatic uptake and storage. RS is an autosomal recessive disorder. Animal experiments and studies of patients with RS suggest that there are homozygous mutations of both SLCO1B1/OATP1B1 and SLCO1B3/OATP1B3 resulting in simultaneous absence of OATP1B1 and OATP1B3 transporters (12). Of note, SLCO1B1 and SLCO1B3 lie very close together on chromosome 12.
Clinical manifestation
Clinically, the disorder is indistinguishable from DJS, and presents with predominantly a mixed conjugated and unconjugated hyperbilirubinemia in otherwise asymptomatic individuals. It can present in the neonatal period or in childhood. Serum total bilirubin levels are usually between 2 and 5 mg/dL, but can be higher.
Diagnosis and management
RS is benign and does not require any therapy. Again, diagnosis is important to differentiate from other causes of hepatobiliary disorders. Urine tests are diagnostic and can differentiate RS from DJS. In RS, total coproporphyrin excretion in urine is elevated 2–5 fold, with 65% constituting coproporphyrin I (31). Further diagnostic or invasive testing is usually not indicated. If performed, a HIDA scan will reveal slow liver uptake and prominent kidney excretion (12) and histology will show normal liver tissue with absent pigment (9).
The main characteristics of these disorders are summarized in Table 1 and the defective transporters/enzymes are shown in Figure 3.
Table 1.
Characteristics of inherited disorders of bilirubin clearance.
| Disorder | Molecular Defect |
Inheritance | Age of Presentation |
Type and Degree of Hyperbilirubinemia |
Urine Studies | Liver Histology |
Treatment | Prognosis | |
|---|---|---|---|---|---|---|---|---|---|
| Uptake defect | - | ? GST ? OATP1B1/3 |
? | Neonatal | Unconjugated, low to moderate | Normal (75% coproporphyrin III) | Normal | Possible phototherapy in newborn period | Good |
| Conjugation defect | GS | UGT1A1 | Autosomal recessive | Early adulthood; neonatal presentation especially if co-existing hemolytic disorder | Unconjugated, low to moderate | Normal | Normal | Usually none; phototherapy in newborn period especially if hemolytic disorder; rarely phenobarbital | Good |
| CN type I | UGT1A1 | Autosomal recessive | Neonatal | Unconjugated, severe | Normal | Normal | Aggressive phototherapy; exchange transfusions; liver transplant | Poor | |
| CN type II | UGT1A1 | Autosomal recessive | Neonatal | Unconjugated, moderate to severe | Normal | Normal | Phototherapy in newborn period; phenobarbital | Good with treatment | |
| Lucey-Driscoll | Placental transfer of maternal serum inhibitor of UGT1A1 | - | Neonatal | Unconjugated, moderate to severe | Normal | Normal | Phototherapy and possible exchange transfusion in newborn period | Good with treatment | |
| Breast milk jaundice | ? UGT1A1 polymorphism ? Inhibitor of UGT1A1 in breast milk |
- | Neonatal | Unconjugated, low to moderate | Normal | Normal | Usually none | Good | |
| Excretion defect | DJS | MRP2 | Autosomal recessive | Early adulthood; rarely neonatal presentation | Conjugated, low to moderate | Normal total coproporphyrin (80% coproporphyrin I) | Pigment deposit | Usually none; possible need for phenobarbital or ursodiol in cases of severe neonatal cholestasis | Good |
| Reuptake defect | RS | OATP1B1/3 | Autosomal recessive | Newborn to early adulthood | Conjugated, low to moderate | 3–5 fold increase in coproporphyrin (65% coproporphyrin I) | Normal | None | Good |
Figure 3.
Schematic view of transporters and enzymes involved in inherited disorders of bilirubin clearance. (Alb, albumin; BCRP, breast cancer resistance protein; BMG, bilirubin monoglucuronide; BDG, bilirubin diglucuronide; CN, Crigler-Najjar; DJS, Dubin-Johnson syndrome; GS, Gilbert syndrome; GST, glutathione-S-transferase; MRP, multidrug resistance-associated protein; OATP, organic anion transport protein; RS, Rotor syndrome; UCB, unconjugated bilirubin; UGT, uridine diphosphate glucuronosyl transferase).
Summary
Inherited disorders of bilirubin clearance can present with either unconjugated or conjugated hyperbilirubinemia in the newborn period. Understanding the molecular basis and clinical presentation of these syndromes is critical for differentiating those that are benign from those that can be lethal and associated with kernicterus.
Acknowledgments
Financial support: This work was supported by the National Institute of Environmental Health Sciences [Grant P30ES002022].
Footnotes
Disclosure/Conflict of interest: Authors have no conflict of interest to disclose.
References
- 1.London IM, West R, Shemin D, Rittenberg D. On the origin of bile pigment in normal man. J Biol Chem. 1950;184:351–8. [PubMed] [Google Scholar]
- 2.Watchko JF, Tiribelli C. Bilirubin-induced neurologic damage--mechanisms and management approaches. N Engl J Med. 2013;369:2021–30. doi: 10.1056/NEJMra1308124. [DOI] [PubMed] [Google Scholar]
- 3.Sorrentino D, Berk PD. Mechanistic aspects of hepatic bilirubin uptake. Semin Liver Dis. 1988;8:119–36. doi: 10.1055/s-2008-1040533. [DOI] [PubMed] [Google Scholar]
- 4.Hagenbuch B, Meier PJ. Organic anion transporting polypeptides of the OATP/SLC21 family: phylogenetic classification as OATP/SLCO superfamily, new nomenclature and molecular/functional properties. Pflugers Arch. 2004;447:653–65. doi: 10.1007/s00424-003-1168-y. [DOI] [PubMed] [Google Scholar]
- 5.Briz O, Serrano MA, MacIas RI, Gonzalez-Gallego J, Marin JJ. Role of organic anion-transporting polypeptides, OATP-A, OATP-C and OATP-8, in the human placenta-maternal liver tandem excretory pathway for foetal bilirubin. Biochem J. 2003;371:897–905. doi: 10.1042/BJ20030034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cui Y, Konig J, Leier I, Buchholz U, Keppler D. Hepatic uptake of bilirubin and its conjugates by the human organic anion transporter SLC21A6. J Biol Chem. 2001;276:9626–30. doi: 10.1074/jbc.M004968200. [DOI] [PubMed] [Google Scholar]
- 7.Zhang W, He YJ, Gan Z, et al. OATP1B1 polymorphism is a major determinant of serum bilirubin level but not associated with rifampicin-mediated bilirubin elevation. Clin Exp Pharmacol Physiol. 2007;34:1240–4. doi: 10.1111/j.1440-1681.2007.04798.x. [DOI] [PubMed] [Google Scholar]
- 8.Sanna S, Busonero F, Maschio A, et al. Common variants in the SLCO1B3 locus are associated with bilirubin levels and unconjugated hyperbilirubinemia. Hum Mol Genet. 2009;18:2711–8. doi: 10.1093/hmg/ddp203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erlinger S, Arias IM, Dhumeaux D. Inherited disorders of bilirubin transport and conjugation: new insights into molecular mechanisms and consequences. Gastroenterology. 2014;146:1625–38. doi: 10.1053/j.gastro.2014.03.047. [DOI] [PubMed] [Google Scholar]
- 10.Jemnitz K, Heredi-Szabo K, Janossy J, Ioja E, Vereczkey L, Krajcsi P. ABCC2/Abcc2: a multispecific transporter with dominant excretory functions. Drug Metab Rev. 2010;42:402–36. doi: 10.3109/03602530903491741. [DOI] [PubMed] [Google Scholar]
- 11.Vlaming ML, Pala Z, van Esch A, et al. Functionally overlapping roles of Abcg2 (Bcrp1) and Abcc2 (Mrp2) in the elimination of methotrexate and its main toxic metabolite 7-hydroxymethotrexate in vivo. Clin Cancer Res. 2009;15:3084–93. doi: 10.1158/1078-0432.CCR-08-2940. [DOI] [PubMed] [Google Scholar]
- 12.van de Steeg E, Stranecky V, Hartmannova H, et al. Complete OATP1B1 and OATP1B3 deficiency causes human Rotor syndrome by interrupting conjugated bilirubin reuptake into the liver. J Clin Invest. 2012;122:519–28. doi: 10.1172/JCI59526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sticova E, Jirsa M. New insights in bilirubin metabolism and their clinical implications. World J Gastroenterol. 2013;19:6398–407. doi: 10.3748/wjg.v19.i38.6398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mooij MG, Schwarz UI, de Koning BA, et al. Ontogeny of human hepatic and intestinal transporter gene expression during childhood: age matters. Drug Metab Dispos. 2014;42:1268–74. doi: 10.1124/dmd.114.056929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muslu N, Dogruer ZN, Eskandari G, Atici A, Kul S, Atik U. Are glutathione S-transferase gene polymorphisms linked to neonatal jaundice? Eur J Pediatr. 2008;167:57–61. doi: 10.1007/s00431-007-0425-z. [DOI] [PubMed] [Google Scholar]
- 16.McCarver DG, Hines RN. The ontogeny of human drug-metabolizing enzymes: phase II conjugation enzymes and regulatory mechanisms. J Pharmacol Exp Ther. 2002;300:361–6. doi: 10.1124/jpet.300.2.361. [DOI] [PubMed] [Google Scholar]
- 17.Burchell B, Coughtrie M, Jackson M, et al. Development of human liver UDP-glucuronosyltransferases. Dev Pharmacol Ther. 1989;13:70–7. doi: 10.1159/000457587. [DOI] [PubMed] [Google Scholar]
- 18.Onishi S, Kawade N, Itoh S, Isobe K, Sugiyama S. Postnatal development of uridine diphosphate glucuronyltransferase activity towards bilirubin and 2-aminophenol in human liver. Biochem J. 1979;184:705–7. doi: 10.1042/bj1840705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Metreau JM, Dhumeaux D, Gisselbrecht C, Preaux AM, Berthelot P. Constitutional unconjugated hyperbilirubinaemia. Lancet. 1977;1:1319. doi: 10.1016/s0140-6736(77)91359-9. [DOI] [PubMed] [Google Scholar]
- 20.Abdel Ghany EA, Hussain NF, Botros SK. Glutathione S-transferase gene polymorphisms in neonatal hyperbilirubinemia. J Investig Med. 2012;60:18–22. doi: 10.2310/JIM.0b013e318235479a. [DOI] [PubMed] [Google Scholar]
- 21.Owens IS, Basu NK, Banerjee R. UDP-glucuronosyltransferases: gene structures of UGT1 and UGT2 families. Methods Enzymol. 2005;400:1–22. doi: 10.1016/S0076-6879(05)00001-7. [DOI] [PubMed] [Google Scholar]
- 22.Ritter JK, Crawford JM, Owens IS. Cloning of two human liver bilirubin UDP-glucuronosyltransferase cDNAs with expression in COS-1 cells. J Biol Chem. 1991;266:1043–7. [PubMed] [Google Scholar]
- 23.van Es HH, Bout A, Liu J, et al. Assignment of the human UDP glucuronosyltransferase gene (UGT1A1) to chromosome region 2q37. Cytogenet Cell Genet. 1993;63:114–6. doi: 10.1159/000133513. [DOI] [PubMed] [Google Scholar]
- 24.Canu G, Minucci A, Zuppi C, Capoluongo E. Gilbert and Crigler Najjar syndromes: an update of the UDP-glucuronosyltransferase 1A1 (UGT1A1) gene mutation database. Blood Cells Mol Dis. 2013;50:273–80. doi: 10.1016/j.bcmd.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Sugatani J, Kojima H, Ueda A, et al. The phenobarbital response enhancer module in the human bilirubin UDP-glucuronosyltransferase UGT1A1 gene and regulation by the nuclear receptor CAR. Hepatology. 2001;33:1232–8. doi: 10.1053/jhep.2001.24172. [DOI] [PubMed] [Google Scholar]
- 26.Gilbert A, Lereboullet P. La cholemie simple familiale. Semaine Medicale. 1901;21:241–3. [Google Scholar]
- 27.Travan L, Lega S, Crovella S, Montico M, Panontin E, Demarini S. Severe neonatal hyperbilirubinemia and UGT1A1 promoter polymorphism. J Pediatr. 2014;165:42–5. doi: 10.1016/j.jpeds.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 28.Owens D, Evans J. Population studies on Gilbert’s syndrome. J Med Genet. 1975;12:152–6. doi: 10.1136/jmg.12.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Auclair C, Hakim J, Boivin P, Troube H, Boucherot J. Bilirubin and paranitrophenol glucuronyl transferase activities of the liver in patients with Gilbert’s syndrome An attempt at a biochemical breakdown of the Gilbert’s syndrome. Enzyme. 1976;21:97–107. doi: 10.1159/000458848. [DOI] [PubMed] [Google Scholar]
- 30.Bosma PJ. Inherited disorders of bilirubin metabolism. J Hepatol. 2003;38:107–17. doi: 10.1016/s0168-8278(02)00359-8. [DOI] [PubMed] [Google Scholar]
- 31.Strassburg CP. Hyperbilirubinemia syndromes (Gilbert-Meulengracht, Crigler-Najjar, Dubin-Johnson, and Rotor syndrome) Best Pract Res Clin Gastroenterol. 2010;24:555–71. doi: 10.1016/j.bpg.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 32.Bosma PJ, Chowdhury JR, Bakker C, et al. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert’s syndrome. N Engl J Med. 1995;333:1171–5. doi: 10.1056/NEJM199511023331802. [DOI] [PubMed] [Google Scholar]
- 33.Beutler E, Gelbart T, Demina A. Racial variability in the UDP-glucuronosyltransferase 1 (UGT1A1) promoter: a balanced polymorphism for regulation of bilirubin metabolism? Proc Natl Acad Sci U S A. 1998;95:8170–4. doi: 10.1073/pnas.95.14.8170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Monaghan G, Ryan M, Seddon R, Hume R, Burchell B. Genetic variation in bilirubin UPD-glucuronosyltransferase gene promoter and Gilbert’s syndrome. Lancet. 1996;347:578–81. doi: 10.1016/s0140-6736(96)91273-8. [DOI] [PubMed] [Google Scholar]
- 35.Akaba K, Kimura T, Sasaki A, et al. Neonatal hyperbilirubinemia and a common mutation of the bilirubin uridine diphosphate-glucuronosyltransferase gene in Japanese. J Hum Genet. 1999;44:22–5. doi: 10.1007/s100380050100. [DOI] [PubMed] [Google Scholar]
- 36.Maruo Y, Nishizawa K, Sato H, Sawa H, Shimada M. Prolonged unconjugated hyperbilirubinemia associated with breast milk and mutations of the bilirubin uridine diphosphate-glucuronosyltransferase gene. Pediatrics. 2000;106:E59. doi: 10.1542/peds.106.5.e59. [DOI] [PubMed] [Google Scholar]
- 37.Skierka JM, Kotzer KE, Lagerstedt SA, O’Kane DJ, Baudhuin LM. UGT1A1 genetic analysis as a diagnostic aid for individuals with unconjugated hyperbilirubinemia. J Pediatr. 2013;162:1146–52. 52 e1–2. doi: 10.1016/j.jpeds.2012.11.042. [DOI] [PubMed] [Google Scholar]
- 38.Kaplan M, Renbaum P, Levy-Lahad E, Hammerman C, Lahad A, Beutler E. Gilbert syndrome and glucose-6-phosphate dehydrogenase deficiency: a dose-dependent genetic interaction crucial to neonatal hyperbilirubinemia. Proc Natl Acad Sci U S A. 1997;94:12128–32. doi: 10.1073/pnas.94.22.12128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaplan M, Hammerman C, Renbaum P, Klein G, Levy-Lahad E. Gilbert’s syndrome and hyperbilirubinaemia in ABO-incompatible neonates. Lancet. 2000;356:652–3. doi: 10.1016/S0140-6736(00)02610-6. [DOI] [PubMed] [Google Scholar]
- 40.Roy-Chowdhury N, Deocharan B, Bejjanki HR, et al. Presence of the genetic marker for Gilbert syndrome is associated with increased level and duration of neonatal jaundice. Acta Paediatr. 2002;91:100–1. doi: 10.1080/080352502753458058. [DOI] [PubMed] [Google Scholar]
- 41.Laforgia N, Faienza MF, Rinaldi A, D’Amato G, Rinaldi G, Iolascon A. Neonatal hyperbilirubinemia and Gilbert’s syndrome. J Perinat Med. 2002;30:166–9. doi: 10.1515/JPM.2002.021. [DOI] [PubMed] [Google Scholar]
- 42.Chang PF, Lin YC, Liu K, Yeh SJ, Ni YH. Identifying term breast-fed infants at risk of significant hyperbilirubinemia. Pediatr Res. 2013;74:408–12. doi: 10.1038/pr.2013.120. [DOI] [PubMed] [Google Scholar]
- 43.Sato H, Uchida T, Toyota K, et al. Association of neonatal hyperbilirubinemia in breast-fed infants with UGT1A1 or SLCOs polymorphisms. J Hum Genet. 2015;60:35–40. doi: 10.1038/jhg.2014.98. [DOI] [PubMed] [Google Scholar]
- 44.Zaja O, Tiljak MK, Stefanovic M, Tumbri J, Jurcic Z. Correlation of UGT1A1 TATA-box polymorphism and jaundice in breastfed newborns-early presentation of Gilbert’s syndrome. J Matern Fetal Neonatal Med. 2014;27:844–50. doi: 10.3109/14767058.2013.837879. [DOI] [PubMed] [Google Scholar]
- 45.Maruo Y, Morioka Y, Fujito H, et al. Bilirubin uridine diphosphate-glucuronosyltransferase variation is a genetic basis of breast milk jaundice. J Pediatr. 2014;165:36–41. e1. doi: 10.1016/j.jpeds.2014.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bartlett MG, Gourley GR. Assessment of UGT polymorphisms and neonatal jaundice. Semin Perinatol. 2011;35:127–33. doi: 10.1053/j.semperi.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 47.Crigler JF, Jr, Najjar VA. Congenital familial nonhemolytic jaundice with kernicterus. Pediatrics. 1952;10:169–80. [PubMed] [Google Scholar]
- 48.Ritter JK, Yeatman MT, Ferreira P, Owens IS. Identification of a genetic alteration in the code for bilirubin UDP-glucuronosyltransferase in the UGT1 gene complex of a Crigler-Najjar type I patient. J Clin Invest. 1992;90:150–5. doi: 10.1172/JCI115829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gantla S, Bakker CT, Deocharan B, et al. Splice-site mutations: a novel genetic mechanism of Crigler-Najjar syndrome type 1. Am J Hum Genet. 1998;62:585–92. doi: 10.1086/301756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Clarke DJ, Moghrabi N, Monaghan G, et al. Genetic defects of the UDP-glucuronosyltransferase-1 (UGT1) gene that cause familial non-haemolytic unconjugated hyperbilirubinaemias. Clin Chim Acta. 1997;266:63–74. doi: 10.1016/s0009-8981(97)00167-8. [DOI] [PubMed] [Google Scholar]
- 51.Kadakol A, Ghosh SS, Sappal BS, Sharma G, Chowdhury JR, Chowdhury NR. Genetic lesions of bilirubin uridine-diphosphoglucuronate glucuronosyltransferase (UGT1A1) causing Crigler-Najjar and Gilbert syndromes: correlation of genotype to phenotype. Hum Mutat. 2000;16:297–306. doi: 10.1002/1098-1004(200010)16:4<297::AID-HUMU2>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 52.Blaschke TF, Berk PD, Scharschmidt BF, Guyther JR, Vergalla JM, Waggoner JG. Crigler-Najjar syndrome: an unusual course with development of neurologic damage at age eighteen. Pediatr Res. 1974;8:573–90. doi: 10.1203/00006450-197405000-00006. [DOI] [PubMed] [Google Scholar]
- 53.Jansen PL. Diagnosis and management of Crigler-Najjar syndrome. Eur J Pediatr. 1999;158(Suppl 2):S89–94. doi: 10.1007/pl00014330. [DOI] [PubMed] [Google Scholar]
- 54.Arias IM, Gartner LM, Cohen M, Ezzer JB, Levi AJ. Chronic nonhemolytic unconjugated hyperbilirubinemia with glucuronyl transferase deficiency. Clinical, biochemical, pharmacologic and genetic evidence for heterogeneity. Am J Med. 1969;47:395–409. doi: 10.1016/0002-9343(69)90224-1. [DOI] [PubMed] [Google Scholar]
- 55.van der Veere CN, Sinaasappel M, McDonagh AF, et al. Current therapy for Crigler-Najjar syndrome type 1: report of a world registry. Hepatology. 1996;24:311–5. doi: 10.1002/hep.510240205. [DOI] [PubMed] [Google Scholar]
- 56.Bortolussi G, Zentilin L, Baj G, et al. Rescue of bilirubin-induced neonatal lethality in a mouse model of Crigler-Najjar syndrome type I by AAV9-mediated gene transfer. FASEB J. 2012;26:1052–63. doi: 10.1096/fj.11-195461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arias IM. Chronic unconjugated hyperbilirubinemia without overt signs of hemolysis in adolescents and adults. J Clin Invest. 1962;41:2233–45. doi: 10.1172/JCI104682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seppen J, Bosma PJ, Goldhoorn BG, et al. Discrimination between Crigler-Najjar type I and II by expression of mutant bilirubin uridine diphosphate-glucuronosyltransferase. J Clin Invest. 1994;94:2385–91. doi: 10.1172/JCI117604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee WS, McKiernan PJ, Beath SV, et al. Bile bilirubin pigment analysis in disorders of bilirubin metabolism in early infancy. Arch Dis Child. 2001;85:38–42. doi: 10.1136/adc.85.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chalasani N, Chowdhury NR, Chowdhury JR, Boyer TD. Kernicterus in an adult who is heterozygous for Crigler-Najjar syndrome and homozygous for Gilbert-type genetic defect. Gastroenterology. 1997;112:2099–103. doi: 10.1053/gast.1997.v112.pm9178703. [DOI] [PubMed] [Google Scholar]
- 61.Kadakol A, Sappal BS, Ghosh SS, et al. Interaction of coding region mutations and the Gilbert-type promoter abnormality of the UGT1A1 gene causes moderate degrees of unconjugated hyperbilirubinaemia and may lead to neonatal kernicterus. J Med Genet. 2001;38:244–9. doi: 10.1136/jmg.38.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Arias IM, Wolfson S, Lucey JF, McKay RJ., Jr Transient Familial Neonatal Hyperbilirubinemia. J Clin Invest. 1965;44:1442–50. doi: 10.1172/JCI105250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Newman AJ, Gross S. Hyperbilirubinemia in Breast-Fed Infants. Pediatrics. 1963;32:995–1001. [PubMed] [Google Scholar]
- 64.Arias IM, Gartner LM, Seifter S, Furman M. Prolonged Neonatal Unconjugated Hyperbilirubinemia Associated with Breast Feeding and a Steroid, Pregnane-3(Alpha), 20(Beta)-Diol, in Maternal Milk That Inhibits Glucuronide Formation in Vitro. J Clin Invest. 1964;43:2037–47. doi: 10.1172/JCI105078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bevan BR, Holton JB. Inhibition of bilirubin conjugation in rat liver slices by free fatty acids, with relevance to the problem of breast milk jaundice. Clin Chim Acta. 1972;41:101–7. doi: 10.1016/0009-8981(72)90501-3. [DOI] [PubMed] [Google Scholar]
- 66.Gourley GR, Arend RA. beta-Glucuronidase and hyperbilirubinaemia in breast-fed and formula-fed babies. Lancet. 1986;1:644–6. doi: 10.1016/s0140-6736(86)91724-1. [DOI] [PubMed] [Google Scholar]
- 67.Kumral A, Ozkan H, Duman N, Yesilirmak DC, Islekel H, Ozalp Y. Breast milk jaundice correlates with high levels of epidermal growth factor. Pediatr Res. 2009;66:218–21. doi: 10.1203/PDR.0b013e3181ac4a30. [DOI] [PubMed] [Google Scholar]
- 68.Ota Y, Maruo Y, Matsui K, Mimura Y, Sato H, Takeuchi Y. Inhibitory effect of 5beta-pregnane-3alpha,20beta-diol on transcriptional activity and enzyme activity of human bilirubin UDP-glucuronosyltransferase. Pediatr Res. 2011;70:453–7. doi: 10.1203/PDR.0b013e31822f242e. [DOI] [PubMed] [Google Scholar]
- 69.Preer GL, Philipp BL. Understanding and managing breast milk jaundice. Arch Dis Child Fetal Neonatal Ed. 2011;96:F461–6. doi: 10.1136/adc.2010.184416. [DOI] [PubMed] [Google Scholar]
- 70.Maisels MJ, Newman TB. Kernicterus in otherwise healthy, breast-fed term newborns. Pediatrics. 1995;96:730–3. [PubMed] [Google Scholar]
- 71.Dubin IN, Johnson FB. Chronic idiopathic jaundice with unidentified pigment in liver cells; a new clinicopathologic entity with a report of 12 cases. Medicine (Baltimore) 1954;33:155–97. doi: 10.1097/00005792-195409000-00001. [DOI] [PubMed] [Google Scholar]
- 72.Sprinz H, Nelson RS. Persistent non-hemolytic hyperbilirubinemia associated with lipochrome-like pigment in liver cells: report of four cases. Ann Intern Med. 1954;41:952–62. doi: 10.7326/0003-4819-41-5-952. [DOI] [PubMed] [Google Scholar]
- 73.Paulusma CC, Kool M, Bosma PJ, et al. A mutation in the human canalicular multispecific organic anion transporter gene causes the Dubin-Johnson syndrome. Hepatology. 1997;25:1539–42. doi: 10.1002/hep.510250635. [DOI] [PubMed] [Google Scholar]
- 74.Lee JH, Chen HL, Chen HL, Ni YH, Hsu HY, Chang MH. Neonatal Dubin-Johnson syndrome: long-term follow-up and MRP2 mutations study. Pediatr Res. 2006;59:584–9. doi: 10.1203/01.pdr.0000203093.10908.bb. [DOI] [PubMed] [Google Scholar]
- 75.Haimi-Cohen Y, Amir J, Merlob P. Neonatal and infantile Dubin-Johnson syndrome. Pediatr Radiol. 1998;28:900. doi: 10.1007/s002470050494. [DOI] [PubMed] [Google Scholar]
- 76.Rotor ABML, Florentin A. Familial nonhemolytic jaundice with direct van den Bergh reaction. Acta Med Phil. 1948;5:37–49. [Google Scholar]