Abstract
Little is known about the age of onset of sexual and drug risk and their association with complex patterns of recent drug use among male sex workers (MSW) in a developing country, such as Vietnam. The aim of this study was to determine whether latent class analysis (LCA) would aid in the detection of current individual and polydrug use combinations to predict how different trajectories of sexual and drug initiation contribute to different patterns of current illicit drug use. Data were collected from a cross-sectional survey administered to young male sex workers between 2010 and 2011 in Vietnam (N = 710). Latent class analysis (LCA) clustered participants into recent drug use groups, incorporating both the specific types and overall count of different drugs used. Men reported drug use within a one month period from an 11-item drug use list. LCA identified 3 distinct drug use classes: 1) alcohol use, 2) alcohol and tobacco use and 3) high polydrug use. The current drug use classes are associated with sex worker status, housing stability, income level, educational attainment, marital status, sexual identity and sexual preferences. High levels of drug use are strongly associated with being a recent sex worker, not having recent stable housing, higher than median income, more than a high school education, less likely to be currently in school and more likely to have non-homosexual preferences and heterosexual partners. An event history analysis approach (time-event displays) examined the timing of the age of onset of drug and sexual risks. Early ages of drug and sexual initiation are seen for all three classes. High current drug users show earlier onset of these risks, which are significantly delayed for moderate and low current drug users. LCA incorporating an overall count of different drugs detected 3 distinct current drug use classes. The data illustrates that the complexity of drug factors that must be accounted for, both in advancing our epidemiological understanding of the complexity of drug use and the use of drug and sexual risk initiation data to predict current drug use subtypes among high risk populations.
Keywords: Male sex work, Vietnam, latent class analysis, drug use, sexual initiation
INTRODUCTION
Men who have sex with men (MSM), particularly young men who have sex with men (YMSM), continue to figure prominently in the spread of HIV infection in Vietnam (VN), along with intravenous drug users (IDU) and female sex workers. Vietnam has seen a sharp increase in HIV cases, with an estimated 280,000 infections nationwide in 2012, with 40,000 new infections each year (Ministry of Health, 2009). Despite limited epidemiological data available on HIV in MSM in Vietnam, there is cause to be alarmed. The prevalence of HIV among MSM in Hanoi has nearly doubled from 2006 to 2009 from 11.0% to 19.8% and similarly for Ho Chi Minh City (HCMC), which is currently at 14.3% (Ministry of Health, 2011).
Among the factors contributing to the growth of HIV infection rates in MSM populations, drug abuse has emerged as a significant contributing factor, both in relation to sexual risk as well as in the context of injection mediated transmission risk (Go et al., 2011, Quan et al., 2010, Thanh et al., 2009, Clatts et al., 2007, Vu et al., 2012, Clatts et al., 2010). Male sex workers (MSW), notably a group that is represented within the YMSM population as a whole, are of particular concern in relation to risk for HIV infection because they may have high risk behavioral interactions with multiple populations with high background HIV seroprevalence, including adult MSM (clients that purchase sex as well as non-client partners), injection drug users (IDUs) and female sex workers (Baral et al., 2015). The complex partnership status includes multiple sources of initiation of different sexual encounters during the life course which along with drug initiation patterns may play a role in establishing risk trajectories and poor health outcomes among MSW (Clatts et al., 2015).
Relatively little is known about the relationship between age of onset of sexual and drug use risks and current patterns of combined complex drug use among MSW in Vietnam, as most research has focused on the use of specific individual drugs or classes of drugs (Yu et al., 2015a, Yu et al., 2015b). Based on data collected in a controlled comparison, epidemiological study of young MSW in Vietnam, this paper describes the prevalence of current use for a wide range of drugs. We also show the prevalence of selected high risk behaviors, including the onset of both drug use and sexual risk, with the overall goal of illuminating the role of drug and sexual onset on increasing risk for negative health outcomes, such as opiate and/or stimulant use, among MSW. Latent Class Analysis (LCA) is a statistical technique that can be used to determine subtypes of drug use that can impact current risk practices, and data on the onset of drug use can predict these drug use subtypes. The ultimate aim of this type of research and analysis is to identify individuals early on who would be at greatest risk for polydrug use, and therefore be at most behavioral risk in the future.
METHODS
Sample and Study Design
Data collection was initiated in April 2010 and completed in July 2011. Community samples of MSW were recruited from three cities [Hanoi (North), Nha Trang (Central), Ho Chi Minh City (South)] using a combination of locally-tailored “targeted” and “time-location” sampling methods (Waters and Biernacki, 1989, Clatts et al., 1995). In each city, ethnographic methods (including observation, mapping, and informal interviews) were used to identify and map local venues and social groups in which MSW were present, including bus stations, public parks, tea stalls, internet cafes, massage parlors, and similar public settings. These data served as the basis for development of a targeted sampling plan oriented to maximizing theoretical sources of variability, including age, migration status, sexual identity, drug involvement and setting for client-recruitment.
Selection of subjects was facilitated through the use of a brief, field-based, conversationally-oriented intercept interview which included questions related to screening criteria. Eligible subjects were referred to a private research office where formal screening, written informed consent, behavioral survey interviews, and biological testing activities were conducted. Although the assessment measure included questions about a broad range of both monetary and non-material rewards in exchange for sex, questions in the initial field-based screening served to restrict eligibility to males between the ages of 16 and 35 who self-report having exchanged sex for some form of material remuneration (including money, food, clothing, or some other kind of material benefit) within 90 days prior to the interview. The interview also included several questions designed to mask eligibility criteria, including current drug use and migration status.
Written informed consent procedures included a formal assessment of capacity for consent. Subjects were paid the equivalent of $10 in local Vietnamese currency (Đồng) in compensation for their time. All study procedures and instruments were reviewed and approved by the collaborating research institutions, including the University of Puerto Rico, National Development and Research Institutes, Inc. and Hanoi Medical University.
MEASURES
The survey interview included five general domains: 1) Demographic Characteristics, 2) Substance Use, 3) Sexual History and Current Practices (including age of onset of first sex with different types of partners, current sexual practices and partner characteristics, and practices and partner types at last sexual exchange), 4) Knowledge of HIV/STI Transmission Risk and 5) Use of Health Services (including HIV/STI testing in the last year).
The main life-course outcome variables were: 1) age of first use of alcohol, tobacco and marijuana; 2) age of first sexual debut with the following sexual practices (insertive or receptive vaginal, oral and anal sex with elective female partners and elective male partners); 3) age of first migration to the host city; 4) age of first sex work with a male client and 5) age of first use of opiates and/or stimulants and injection heroin.
For the substance use domain, participants were asked if they had ever used any of the following 11 drugs (lifetime use) and within the past 30 days (current use): alcohol, tobacco, marijuana, opiates and/or stimulants (amphetamine/methamphetamine, MDMA, non-injection heroin, ketamine, opium, cocaine, Diazepam) and injection heroin. Each drug was coded dichotomously as having been used or not. All non-response and non-applicable answers were coded as missing data (i.e. self-reported age of first alcohol use at age 0).
STATISTICAL ANALYSIS
Latent Class Analysis
LCA (Rindskopf & Rindskopf, 1986) was used to empirically identify classes of individuals reporting similar patterns of drug use prior to or during sex within the past year. The 11 dichotomous drug use indicators, and an overall count of the number of different drugs used, were analyzed using LCA with varying number of classes, ranging from 1 to 7 (Yu et al., 2015a, Cheung et al., 2015). The optimal number of classes was determined using Bayesian information criterion (BIC), which balances model fit and parsimony (Fraley & Raftery, 1998, McLachlan & Peel, 2004). The parameters of the LCA model included: (1) the creation of a total drug count indicator as a simple sum of all drug items to reflect the cumulative exposure, (2) the probability of each specific drug being used within each latent class, (3) the overall proportion of the population in each of the latent classes, (4) the mean number of different drugs used in each latent class. The LCA model was fit using maximum likelihood in Mplus version 6.11 (Muthen & Muthen, 1998-2011), where the dichotomous drug use indicators were modeled with a binomial logit link and the overall count of different drugs used was modeled with a log Poisson link. Once the optimal number of classes was determined, the posterior probability that a certain individual belongs to a certain latent class was computed using Bayes’ Rule (Rindskopf & Rindskopf, 1986). Qualitative descriptions of the resulting drug profile classes are based on the prevalence of individual drugs and types of drugs and were labeled as high/low if the prevalence of use within the latent class was above or below the overall sample prevalence by at least 10%.
Relationship between Age of Onset of Drug and Sexual Risk Factors and LCA Drug Use Classes
Demographic covariates (i.e. including age, study site, migration, educational attainment, current schooling, employment income, housing, marital status, sexual identity, sexual preference and recent sex work within the last month) were compared across the predicted LCA drug use classes using chi-square tests. We describe the onset and sequence of life event factors among each class followed by illustrating the trajectories of drug use (alcohol, tobacco and marijuana), sexual risk (with elective female and male partners), migration, sex work and illicit drugs (opiates and/or stimulants and injection heroin). Repeated measure ANOVAs were conducted to examine differences in the onset of events within classes and ANOVAs were conducted to examine differences in the onset of events between classes. SPSS (version 22.0) was used for all analyses.
RESULTS
Polydrug use patterns from the LCA Model
The LCA model resulted in an optimal three classs solution based on the BIC. The three latent classes were: alcohol use class (1) (mean 0.8 drugs) consisting primarily of alcohol use; alcohol and tobacco use class (2) (mean 2.4 drugs), with alcohol (83%) and higher than average use of tobacco (100%); high polydrug use class (3) (mean 3.6 drugs), with higher than average use of alcohol (96%), tobacco (87%), cannabis (31%), amphetamine/methamphetamine (54%) and ecstasy (59%). The LCA also estimated the proportion of the sample in each class. The moderate drug use class was the largest (60%), followed by the low drug use class (26%) and the high drug use class (14%). The overall prevalence of different drugs used and the results of prevalence within the classes identified by the hybrid LCA are shown in Table 1. Overall, men reported an average use of 2.1 drugs, 84% reported alcohol use, 73% reported tobacco use and 10% reported cannabis use all within the last 30 days.
Table 1.
LCA with Total Drug Count – 3 Cluster Solution
| Average Age of First Use (SD) | Recent Drug Use Within the Last 30 Days |
Alcohol and Low Drug Use (1) | Age of First Use (SD) |
Alcohol, Tobacco and Moderate
Drug Use (2) |
Age of First Use (SD) | High Polydrug Use (3) | Age of First Use (SD) | |
|---|---|---|---|---|---|---|---|---|
| Latent Class Percentages | % | % | % | % | ||||
| Alcohol | 15.86 (2.90)A |
83.9% | 76.1% |
16.71
(2.63) A |
83.5% |
15.68
(2.92) A |
95.7% |
15.08
(2.93) A |
| Tobacco | 15.89 (3.17)A |
72.7% | 0.0% | 16.76 (2.94)A |
100.0% | 15.91 (3.17)A |
87.3% | 15.41 (3.20)A |
| Cannabis | 18.72 (3.20)B |
10.0% | 0.0% | 19.60 (4.28) |
7.3% | 18.79 (3.00)B |
31.4% | 18.51 (3.53)B |
|
Opiates and/or
Stimulants |
20.02 (3.39)C |
20.29 (3.21)C |
19.99 (3.41)C |
19.97 (3.41)C |
||||
| Amphetamines/ | ||||||||
| Methamphetamines | 20.31 (3.19) |
16.9% | 4.6% | 20.60 (2.59) |
10.3% | 20.29 (3.25) |
53.3% | 20.24 (3.35) |
| MDMA | 19.96 (3.31) |
12.3% | 3.9% | 20.08 (3.83) |
0.0% | 20.06 (3.33) |
60.2% | 19.77 (3.04) |
| Heroin (Non-Injection) | 19.35 (3.71) |
2.8% | 0.0% | 21.50 (3.54) |
4.2% | 19.24 (3.54) |
0.2% | 19.50 (4.24) |
| Ketamine | 21.07 (3.53) |
3.0% | 0.0% | 20.25 (0.96) |
1.7% | 21.36 (3.84) |
10.8% | 20.80 (3.35) |
| Opium | 18.89 (3.37) |
2.0% | 0.0% | 19.00 (0.00) |
2.6% | 18.79 (3.03) |
2.6% | 19.23 (4.66) |
| Cocaine | 19.75 (3.37) |
0.3% | 0.0% | --- | 0.5% | 21.00 (3.76) |
0.0% | 17.67 (1.53) |
| Diazepam | 21.50 (1.29) |
0.1% | 0.0% | --- | 0.0% | 21.00 (1.41) |
0.8% | 22.00 (1.41) |
| Heroin (Injection) | 20.81 (4.05) |
4.1% | 0.0% | 24.00 (--- ) |
3.7% | 20.47 (3.59) |
13.0% | 21.28 (4.92) |
| Avg Drug Use | 2.1 | 0.8 | 2.1 | 3.6 | ||||
| Proportion in Class | 100% | 25.6% | 60.3% | 14.1% | ||||
| Avg Current Age | 22.18 | 21.76 | 22.27 | 22.53 | ||||
| N | 710 | 182 | 428 | 100 |
Dark Grey Shows Greater than Average Prevalence of Drug Use > +10%
No shading indicates Average or Lower Than Average Prevalence of Drug Use ≤ +10%
Statistical Pairwise Differences Between Alcohol/Tobacco, Cannabis and Opiates and/or Stimulants with a Tukey correction for multiple comparisons at the 5% alpha level
Bolded values indicates differences in average age of first use by class at the 5% alpha level
Demographic Characteristics associated with the Three Latent Drug Use Classes
MSW in the sample ranged from 16 to 35 years of age as presented in Table 2 (Mean = 22.2, SD = 3.9). The three subgroups are relatively equally distributed in relation to age, which means that any differences in age of onset of drug use and sexual risk behaviors cannot be attributed to cohort effects between current drug classes. High current polydrug users and moderate drug users are more likely than low current drug users to report being a recent sex worker (defined as sex work within the past month) (p = 0.028). Differences are also seen in housing stability. High and moderate users are more likely than low users to report having unstable housing within the past month (p < 0.001). Similar differences are seen in relation to educational attainment. Around half of the high users have at least a high school education (56%), while two-thirds of low (65%) and moderate users (63%) completed high school (p < 0.001). Likewise, more than two-thirds of moderate (80%) and high users (68%) report currently not attending school while less than half of low users report likewise (46%) (p < 0.001). The average monthly income ranged from $0 to $3,840 with a median of $173 (Mean = $245, SD = $279). More than two thirds of high users (69%) make more than the median while less than half of moderate (48%) and low users (45%) make more than the median income (p = 0.001). This study was limited to a behaviorally defined population of males who self-reported a sexual exchange with a male client in the last 90 days. Overall, most identify in terms of sexual attraction as bisexual (46%) or heterosexual (31%), followed by homosexual (23%). Differences in sexual attraction and identity are statistically significant among the three drug groups (p < 0.001). Low users are sexually attracted to men (39%) at higher rates than moderate (19%) and high users (16%) while the self-reported bisexual identity remains constant throughout the three classes. Low users sexually identify as a man (50%) at lower rates than the moderate (69%) and high users (58%).
Table 2.
Demographic Characteristics of 710 Vietnamese Male Sex Workers by the 3 Drug Use Classes
| Drug Use | Low (N = 182) |
Moderate (N = 428) |
High (N = 100) |
|
|---|---|---|---|---|
| N (%) | N (%) | N (%) | p-value | |
| Hanoi | 60 (33.0%) | 161 (37.6%) | 29 (29.0%) | 0.308 |
| Nha Trang | 39 (21.4%) | 95 (22.2%) | 20 (20.0%) | |
| Ho Chi Minh City | 83 (45.6%) | 172 (40.2%) | 51 (51.0%) | |
| Recent Sex Work in Last 30 Days | 162 (89.0%) | 394 (92.1%) | 98 (98.0%) | 0.028 |
| No Recent Sex Work in Last 30 Days | 20 (11.0%) | 34 (7.9%) | 2 (2.0%) | |
| Stable Housing in Last 30 Days | 179 (98.4%) | 360 (84.1%) | 91 (88.7%) | <0.001 |
| No Stable Housing in Last 30 Days | 3 (1.6%) | 68 (15.9%) | 9 (9.0%) | |
| Income >= $173 (Median) | 82 (45.1%) | 207 (48.4%) | 69 (69.0%) | 0.001 |
| Income < $173 (Median) | 100 (54.9%) | 221 (51.6%) | 31 (31.0%) | |
| >= HS | 68 (37.4%) | 277 (35.3%) | 44 (44.0%) | <0.001 |
| < HS | 114 (62.6%) | 151 (64.7%) | 56 (56.0%) | |
| Single, Never Married | 179 (98.4%) | 417 (97.4%) | 97 (97.0%) | 0.024 |
| Married/Separated/Divorced | 3 (1.6%) | 11 (2.6%) | 3 (3.0%) | |
| Age < 21 | 77 (42.3%) | 170 (39.7%) | 35 (35.0%) | 0.487 |
| Age > 21 | 105 (57.7%) | 258 (60.3%) | 65 (65.0%) | |
| In School Now | 66 (53.7%) | 56 (20.4%) | 18 (31.6%) | < 0.001 |
| Not In School Now | 57 (46.3%) | 218 (79.6%) | 39 (68.4%) | |
| Migrant to the Host City | 98 (53.8%) | 231 (54.0%) | 50 (50.0%) | 0.765 |
| Born or Raised in the Host City | 84 (46.2%) | 197 (46.0%) | 50 (50.0%) | |
| Sexual Identity | ||||
| Man | 90 (49.5%) | 293 (68.6%) | 58 (58.0%) | < 0.001 |
| Woman | 17 (9.3%) | 23 (5.4%) | 4 (4.0%) | |
| Transgender | 11 (6.0%) | 27 (6.3%) | 6 (6.0%) | |
| Other | 25 (13.7%) | 23 (5.4%) | 8 (8.0%) | |
| Not Sure | 39 (21.4%) | 61 (14.3%) | 24 (24.0%) | |
| Sexual Preferences | ||||
| Men | 70 (38.5%) | 80 (18.8%) | 16 (16.0%) | < 0.001 |
| Both Men and Women | 79 (43.3%) | 191 (44.8%) | 56 (56.0%) | |
| Women | 33 (18.1%) | 155 (36.4%) | 28 (28.0%) |
Timing and order of onset of drug use and sexual risk behaviors in relation to current drug use classes
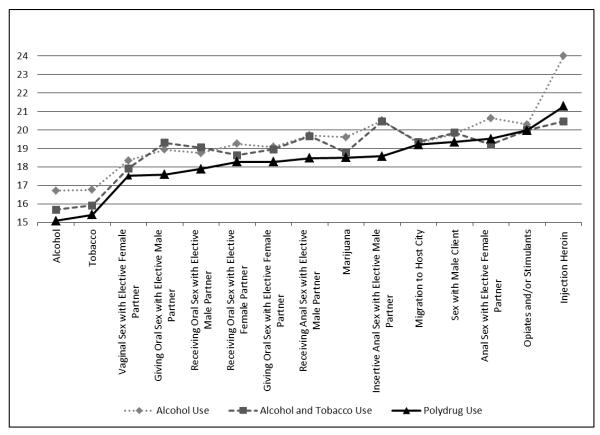
The high current drug use class illustrates that drug use is prevalent among MSW. We examined the timing and the onset of first drug use relative to the timing of first sexual behaviors across these three groups. Here we use age of onset data to provide three types of comparisons: First, we show the order in which each life event occurs in relation to chronological age; second, we show the order in which these events occur relative to one another; and third, we show how these events are distributed across the three current drug use classes. Events included in the trajectory include first age of alcohol use, first age of tobacco use, first age of vaginal sex with a female partner, first age of oral sex with a male partner, first age of marijuana, first age of sex with a male client, first age of opiate and/or stimulant use, and first age of injection heroin use. We also examined the trajectory of onset of each different type of sexual behavior, including: first receiving oral sex with a female partner, first giving oral sex with a female partner, first vaginal sex with a female partner, first anal sex with a female partner, first receiving oral sex with male partner, first giving oral sex with a male partner, first receiving anal sex with a male partner, first insertive anal sex with a male partner and first sex with a male client.
The trajectory data show that the timing of negative events occurs in a relatively consistent order of first alcohol and tobacco use followed by first sexual encounters with female and male partners, then first cannabis use before initiation of sexual activity with male clients (Yu et al., 2015b). Across all three groups, the data show a consistent temporal pattern (Fig 1) in which a constellation of life events occur, such as drug use and sexual encounters with male and female elective partners and migration to the host city before initiation of sex work. Moreover, event outcomes occur earlier for the high drug users relative to the moderate and low drug users. For high drug users, first age of alcohol use, first age of vaginal sex with a female partner, first age of giving oral sex with a male partner and first age of insertive anal sex with a male partner, on average, all occur at the earliest chronological ages (mean ages of 15.1, 17.5, 17.6, 18.6, respectively) compared to later ages for the moderate and low drug users (p < 0.05).
Figure 1.
Life Trajectory of Onset of Events
Recent alcohol use is the most prevalent in high users (Table 1) and also first age of alcohol use occurs, on average, earlier in this group (age 15.1 vs. age 15.7 for moderate users and age 16.7 for low users (p < 0.05)). First age of vaginal sex is the next statistically significant event in the trajectory, as indicated by the onset age of vaginal sex at a mean age of 17.1 for high users, and 17.9 and 18.4, respectively, for the moderate and low drug use classes (p < 0.05). The general trend follows that exposure to vaginal sex leads to the onset age of giving oral sex with male partners, and on average, the high users reported earlier exposure to giving oral sex with male partners than moderate and low users (17.6, 19.3, 18.9, respectively; p < 0.05). Finally, onset age of insertive anal sex with male partners follows the events described above with high users again reporting earlier exposure (18.6, 20.5, 20.5, respectively; p < 0.05). Following the trajectory towards first age of sex work using only the significant events, the events are chronologically listed as: first age of alcohol use, first age of vaginal sex, first age of giving oral sex with male partners and first age of insertive anal sex with male partners.
DISCUSSION
Limitations can be attributed to this particular study design. Collecting data using a community based, targeted sampling approach may not be a formal representation of the underlying MSW population. We did not disentangle the range and variety of exchange and transactional sex within our sample, including but not limited to sex-for-cash payments, drug-sex encounters, survival sex exchanges to more emotional and romantic benefits (such as dinner dates, escort services and travel companionship) (Baral et al., 2015, Tyler, 2014). Interval differences between the age of onset of negative behaviors are in some cases negligible and statistically insignificant. For example, the onset of both drug abuse and sex work occur in tandem, implying that they may be intertwined in crucial ways that are not easily partitioned in the context of cross-sectional, retrospective data. Additional insightful and in depth assessment, ideally in the context of a prospective, mixed-method study design, is needed to further illustrate these processes.
The protective factors that serve this population have failed to exert influence despite these limitations in the data. At the institutional level, there is the expectation that the presence of key social stakeholders – notably families, schools, hospitals and public health clinics – will serve as resources of support and as a protective influence in preventing exposure and accumulation of sexual and drug risks within the early life trajectories of youth and young adults (Clatts et al., 2005, Baral et al., 2015). For example, consistent with earlier studies of MSW in Vietnam, these data show a majority of men that report non-homosexual tendencies and sexual attraction, indicative of the fact that many of these young men may turn to drug use to deal with the untreated psychological distress of male sex work (Clatts et al., 2005, Yu et al., 2015b, Goldsamt et al., 2015). Similarly, interactions with elective female and male sexual partners and exposure to female sex workers also occur frequently and early among MSW, and yet have failed to deter the progressive involvement in the street economy of sex work.
While onset of drug use is complex, the data show that among high, moderate and low level drug using MSW, the onset of opiate and/or stimulant use is deferred or delayed until after initiation of sex work. Thus, these data support the assumption that high rates of current drug use among MSW may be substantially attributable to a prior and underlying problem of psychologically coping with sex work (Clatts et al., 2005, Goldsamt et al., 2015, Yu et al., 2015b). Similarly, these data challenge the assumption that high rates of involvement in illegal activities, such as injection drug use, and the street economy, including sex work, can be causally attributed to an underlying and pre-existing problem with opiates and/or stimulants. In short, outcomes of opiate and/or stimulant and injection drug use are better understood as adaptations to sex work, rather than causes of it.
In addition, the underlying patterns of drug use show that not all young male sex workers show equal burdens of drug use nor are equally vulnerable nor resistant to drug use. The high drug use class shows a polydrug group that has a tendency towards the need to use opiates and/or stimulants. The moderate use class shows vulnerability and a potential for developing future opiate and/or stimulant consumption patterns as their length of duration in sex work increases. The low use class shows relative resiliency (resistance towards drug use) despite an environment in which opiate and/or stimulant use is common and might even be normative.
Clearly drug use is a critical issue for MSW, and once established as a central behavioral adaptation, it may well become a critical factor in determining subsequent risk trajectory outcomes. Of particular concern is the onset of heterosexual encounters both before and after initiation of sex work which may serve as an important bridge population for the diffusion of HIV and STI across sexual risk networks (Clatts et al., 2007, Yu et al., 2015b, Clatts et al., 2015). As to the question of the origins of drug use, however, these data offer a compelling argument for understanding these behavioral risks not as artifacts of individual pathology, but rather as unintended medical consequences of the adaptation to male sex work, including the unmet internal and external needs (Clatts et al., 2005, Yu et al., 2015b). While the sources of risk are many, and their relationship with one another are increasingly complex, current drug use along with sex work clearly plays a pivotal role in MSW’s risk for exposure to drug and sexual risk as well as a formidable challenge to their management of risks.
CONCLUSIONS
Young MSW, in particular those under 18 years of age, are highly vulnerable and there is reluctance among medical providers to deal with young people at risk and likewise, among youth to actively seek out health care services. The need to target young people in structural intervention programs is of utmost importance given that drug and sexual risk behaviors are established early on in late adolescence. The trajectory data illustrate the earliest initiation of risk and negative event life factors affiliated with polydrug use, the class with the most complex interplay of drug use. It logically follows then, that structural interventions – systematic approaches to more effective means of reaching, engaging, and retaining MSW in primary preventive care and delaying the onset of drug and sexual risks – should be central considerations in formulating HIV and other public health interventions targeted to this population.
Acknowledgments
First and foremost, we would like to thank the many young men who participated in the study. This research was supported by Grant DA022170 (Diffusion of HIV-1 among Drug Using Men in SE Asia) from the U.S. National Institute on Drug Abuse, U.S. National Institutes of Health. Data collection was led by our research team at Hanoi Medical University. Additionally, we would like to thank the Hanoi Provincial AIDS Center, Ho Chi Minh City’s Office of Committee for AIDS Prevention and Control, and Khanh Hoa’s Center for Health Education and Communication. Professor Nguyen Tran Hien, M.D., Ph.D., provided valuable guidance and support in planning and implementation of the study.
References
- Baral SD, Friedman MR, Geibel S, Bozhinov B, Diouf D, Sabin K, et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet. 2015;385:260–268. doi: 10.1016/S0140-6736(14)60801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung YK, Yu G, Wall MW, Sacco RL, Elkind MSV, Willey JZ. Patterns of leisure-time physical activity using multivariate finite mixture modeling and cardiovascular risk factors in the Northern Manhattan Study. Annals of Epidemiology. 2015 Mar 23; doi: 10.1016/j.annepidem.2015.03.003. 2015. pii: S1047-2797(15)00092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Davis WR, Atillasoy A. Hitting a Moving Target: The Use of Ethnographic Methods in the Evaluation of AIDS Outreach Programs for Homeless Youth in NYC. Qualitative Methods in Drug Abuse and HIV Research: NIDA Res. Monograph. 1995;157:117–135. [PubMed] [Google Scholar]
- Clatts MC, Giang LM, Goldsamt LA, Cólon-López V. Nonmedical use of promethazine hydrochloride among heroin injectors in Vietnam: unrecognized risks and unintended consequences. Subst Use Misuse. 2010;45:515–527. doi: 10.3109/10826080903452520. [DOI] [PubMed] [Google Scholar]
- Clatts MC, Giang LM, Goldsamt LA, Yi H. Male sex work and HIV risk among young heroin users in Hanoi, Vietnam. Sexual Health. 2007;4:261–267. doi: 10.1071/sh07018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Giang LM, Goldsamt LA, Yu G. Sexual Practices, Partner Concurrency and Prevalence of STIs and HIV Among Male Sex Workers in Three Cities in Vietnam. Sexual Health. 2015 doi: 10.1071/SH14101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Goldsamt LA, Yi H, Gwadz MV. Homelessness and drug abuse among young men who have sex with men in New York City: A preliminary epidemiological trajectory. Journal of Adolescence. 2005;28:201–214. doi: 10.1016/j.adolescence.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley C, Raftery AE. How many clusters? Which clustering method? Answers via model-based cluster analysis. The Computer Journal. 1998;41:578–588. [Google Scholar]
- Go VF, Frangakis C, Van Nam L, Sripaipan T, Bergenstrom A, Li F, et al. Characteristics of High-Risk HIV-Positive IDUs in Vietnam: Implications for Future Interventions. Substance Use Misuse. 2011;46:381–389. doi: 10.3109/10826084.2010.505147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsamt LA, Clatts MC, Le MG, Yu G. Prevalence and Behavioral Correlates of Depression and Anxiety Among Male Sex Workers in Vietnam. International Journal of Sexual Health. 2015;27:145–155. doi: 10.1080/19317611.2014.947055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLachlan G, Peel D. Finite Mixture Models. Wiley; Hoboken, NJ: 2004. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Author; Los Angeles, CA: 1998-2011. [Google Scholar]
- Ministry of Health of Vietnam . Vietnam HIV/AIDS Estimates and Projections 2007-2012. Vietnam Administration of HIV/AIDS Control and Family Health International; Hanoi, Vietnam: 2009. [Google Scholar]
- Ministry of Health of Vietnam . Vietnam AIDS Response Progress Report: HIV/AIDS Estimates and Projection 2012. Vietnam National Committee for AIDS, Drugs, and Prostitution Prevention and Control; Hanoi, Viet Nam: 2011. [Google Scholar]
- Quan VM, Minh NL, Ha TV, Ngoc NP, Vu PT, Celentano DD, et al. Mortality and HIV transmission among male Vietnamese injection drug users. Addiction. 2011;106:583–589. doi: 10.1111/j.1360-0443.2010.03175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rindskopf D, Rindskopf W. The value of latent class analysis in medical diagnosis. Statistical Medicine. 1986;5:21–27. doi: 10.1002/sim.4780050105. [DOI] [PubMed] [Google Scholar]
- Thanh DC, Hien NT, Tuan NA, Thang BD, Long NT, Fylkesnes K. HIV Risk Behaviors and Determinants Among People Living with HIV/AIDS in Vietnam. AIDS Behavior. 2009;13:1151–1159. doi: 10.1007/s10461-008-9451-8. [DOI] [PubMed] [Google Scholar]
- Tyler A. Male Sex Work and Society: Advertising Male Sexual Services. Harrington Park Press; New York, NY: 2014. [Google Scholar]
- Vu BN, Mulvey KP, Baldwin S, Nguyen ST. HIV risk among drug-using men who have sex with men, men selling sex, and transgender individuals in Vietnam. Culture Health Sex. 2012;14:167–180. doi: 10.1080/13691058.2011.630756. [DOI] [PubMed] [Google Scholar]
- Waters JK, Biernacki P. Targeted sampling: Options for the study of hidden populations. Soc Probl. 1989;36:416–430. [Google Scholar]
- Yu G, Clatts MC, Goldsamt LA, Giang LM. Substance Use Among Male Sex Workers in Vietnam: Prevalence, Onset, and Interactions with Sexual Risk. International Journal of Drug Policy. 2015b;26:516–521. doi: 10.1016/j.drugpo.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu G, Wall MM, Hirshfield S, Chiasson MA. Complex Drug Use Patterns and Associated HIV Transmission Risk Behaviors in an Internet Sample of US Men Who Have Sex with Men. Archives of Sexual Behavior. 2015a;44:421–8. doi: 10.1007/s10508-014-0337-8. [DOI] [PMC free article] [PubMed] [Google Scholar]