Abstract
The course of depressive disorders can vary considerable, with some individuals exhibiting a chronic course and poor outcomes, while others have a more episodic course and better outcomes. However it is unclear whether degree of chronicity is continuous or reflects qualitatively distinct subgroups. Using data from a 5-wave, 10-year, naturalistic study of 127 depressed outpatients, we examined whether depression chronicity lies on a continuum or manifests natural boundaries. Spline regression was used to test 7 continuous and discontinuous models of the relationship between depression during the first follow-up interval and multiple outcomes at subsequent follow-ups. In order to further validate the findings, we also created empirically-derived subgroups based on the results of the spline regression analyses and compared them on baseline clinical characteristics and long-term outcomes. There was a clear and consistent discontinuity indicating that for higher levels of chronicity during the first 30 month period, depression was linearly related to outcome; in contrast, for lower levels of chronicity, depression in the initial interval was unrelated to subsequent outcomes. The findings were strikingly consistent across the 4 follow-up evaluations using multiple outcomes and goodness-of-fit indices. In addition, the chronic group--as defined by the first follow-up period--exhibited more baseline chronic depression, anxiety and personality disorders, family history of dysthymia, and childhood adversity, and was more likely to attempt suicide and be hospitalized during follow-up, than the non-chronic group. Results suggest that there are qualitatively distinct classes of patients with more and less chronic depressions, and support the utility of longitudinal course as a means of parsing depression into more homogeneous subgroups.
Keywords: depression, chronic, persistent, subtypes, classification
Historically, depression was viewed as having a relatively favorable course characterized by recovery between episodes. However, in the late 1970s and early 1980s, it was recognized that some individuals with depression experience a chronic course and poor outcomes (Akiskal et al., 1981; Keller & Shapiro, 1982; Kocsis & Frances, 1983; Weissman & Klerman, 1977). The lifetime prevalence of chronic depression in community samples of adults is 4–5% (Blanco et al., 2010; Murphy & Byrne, 2012), accounting for 30% of cases of depressive disorders in the general population (Murphy & Byrne, 2012). Chronic depression is more common in clinical settings, with a prevalence of approximately 36% in outpatient mental health clinics (Markowitz, Moran, Kocsis, & Frances, 1992), comprising about half the cases of depression (Benazzi, 1998; Rounsaville, Sholomskas, & Prusoff, 1980).
Chronic depression can take a number of forms that differ in course pattern and severity (Keller et al., 1995). For example, it can present with a pattern of mild chronic-intermittent symptoms (dysthymic disorder), moderate-severe and very persistent symptoms (chronic major depression), or mild chronic-intermittent symptoms punctuated by periods of moderate-severe symptoms (“double depression”; Keller & Shapiro, 1982). Interestingly, there are few differences between the various forms of chronic depression on clinical, family history, course, and treatment response variables (Blanco et al., 2010; Klein et al., 1995; Klein, Shankman, Lewinsohn, Rohde, & Seeley, 2004; McCullough et al., 2000, 2003; Yang & Dunner, 2001), although chronic depressions presenting with major depression are associated with greater impairment in functioning than those with dysthymic disorder alone (Evans et al., 1995; Goodman, Schwab-Stone, Lahey, Shaffer, & Jensen, 2000; Leader & Klein, 1996). In addition, patients who eventually recover from one form of chronic depression often relapse into a different form of chronic depression, suggesting that they are heterotypic expressions of the same condition (Klein et al., 2006). Given these similarities, the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5; American Psychiatric Association, 2013) recently subsumed the various forms of chronic depression under a single category - Persistent Depressive Disorder - although their differences in symptom severity continue to be recognized through specifiers.
In contrast to the relative similarity of the various forms of chronic depression, there are striking differences between episodic and chronic depressions. Although studies have defined the groups in a variety of ways (e.g., chronicity has been defined as a duration of 1 year or 2 years; non-chronic depression has been limited to major depression or also included minor depression), the results have been fairly consistent. Compared to non-chronic depression, chronic depression is characterized by higher rates of comorbid anxiety (Angst, Gamma, Rössler, Ajdacic, & Klein, 2009; Murphy & Byrne, 2012; Sang et al., 2011; Shankman et al., 2004) and personality disorders (Garyfallos et al., 1999; Markowitz et al., 1992; Pepper et al., 1995), higher levels of depressotypic cognitions (Blanco et al., 2010; Riso et al., 2003), greater suicidality (Gilmer et al., 2005; Holm-Denoma, Berlim, Fleck, & Joiner, 2006; Klein et al., 2006), and more childhood adversity and maltreatment (Angst, Gamma, Rössler, Ajdacic, & Klein, 2011; Horwitz, Widom, McLaughlin, & White, 2001; Lizardi et al., 1995; Wiersma et al., 2009). In addition, chronic depression aggregates in families of probands with chronic, but not non-chronic, depression (Klein et al., 1995, 2004; Mondimore et al., 2006) and the distinction between chronic and episodic depression is stable over time (Klein, Shankman & Rose, 2006).
Taken together, these data suggest that there may be fundamental differences between depressions with more and less chronic courses. However, we are unaware of any studies that directly tested whether degree of chronicity is continuous or reflects qualitatively distinct subgroups. This has significant implications for classification (i.e., whether a categorical or dimensional approach is more appropriate) and developing more accurate and powerful assessment instruments (Ruscio & Ruscio, 2002). Moreover, it could provide important clues and constrain theories regarding etiological and developmental processes (Beauchaine, 2003). Finally, if there is a qualitative distinction between different levels of chronicity, combining them to create a single group of depressed participants, a ubiquitous practice in the depression literature, or using dimensional measures based on cross-sectional symptoms, are likely to obscure research on mechanisms and interventions.
Most studies of the natural boundaries of depression and depressive subtypes have examined patterns of cross-sectional symptoms (see Haslam, Holland, & Kuppens, 2012; Solomon, Haaga, & Arnow, 2001 for reviews). However, chronic and non-chronic depressions have similar symptom profiles (Klein et al., 1996), and are distinguished primarily on the basis of course. Hence, course may be the most appropriate domain in which to search for discontinuities. Unfortunately, existing outcome studies have not been designed to examine the natural structure of depressive disorders (Klein & Allmann, 2014). They have typically compared chronic and non-chronic groups, defined a priori, and found worse outcomes in chronic depression (e.g., Keller & Shapiro, 1982; Klein et al., 2006; Kovacs, Akiskal, Gatsonis & Parrone, 1994; Rhebergen, Beekman, & de Graaf, 2009). However, these results are consistent with both qualitative and quantitative differences. An alternative approach is to examine associations between a spectrum of depression courses and long-term outcomes. A natural boundary would manifest as a sharp change in the course-outcome association at some point along the range, whereas a continuum would result in a linear association throughout (Klein & Riso, 1993).
A recent study (Kotov et al., 2013) applied this approach to examine the associations between symptom course over 4 years and 10-year outcome in psychotic disorders. They used spline regression analysis (Marsh & Cormier, 2001; Muggeo, 2003), a piecewise regression technique that can model a wide range of functional relationships between predictors and outcomes, including linear, non-linear but continuous (e.g., quadratic), and discontinuous associations, as well as combinations of these functions. Comparison of fit among these models can reveal whether participants belong to a single population or to multiple subgroups characterized by different relationships between studied variables. Kotov and colleagues found a sharp discontinuity demarcating affective and non-affective psychosis during the first 4 years of the study and global functioning at the 10-year assessment, indicating a qualitatively worse outcome in the latter group.
Current Study
In this paper, we applied spline regression to data from a 5-wave 10-year prospective study to test whether course of depression in the 30 months following admission to an outpatient clinic is associated with qualitative versus quantitative differences in long-term outcomes. We reasoned that 30 months should be enough time to provide a relatively reliable measure of course, and would still allow us to predict 3 waves of outcomes over the course of the subsequent 90 months.
We hypothesized that there would be a single boundary demarcating two subgroups with qualitatively different relationships between initial course and subsequent symptom, functional, and global outcomes. In contrast, we hypothesized that models specifying linear or curvilinear relationships, or two distinct boundary points would not fit the data. As Haslam (2002) has noted, the existence of a discrete boundary between classes does not preclude the existence of dimensionality within classes. Indeed, data indicating that among individuals with chronic depression, major depression is associated with greater impairment than dysthymic disorder (Evans et al., 1995; Goodman et al., 2000; Leader & Klein, 1996) raises the possibility that there may be a relationship between course and long-term outcome within the more chronic group. Hence, we examined several types of discontinuous models, including models positing linear relationships between initial course and outcome in one or both classes in addition to discontinuity between them, as well as a step function, in which there is no relationship between initial course and outcome in either class.
Finally, we tested the validity of observed discontinuities by using the results of the spline regressions to assign participants to groups. We then compared these empirically defined course classes, which were based on first 30 months of prospective follow-up, on baseline characteristics that have been shown to distinguish chronic and episodic forms of depression in the literature (Klein & Allmann, 2014; Klein & Black, in press) and outcome at each follow-up assessment. Specifically, we hypothesized that the more chronic class would have higher rates of chronic depression diagnoses at baseline and family history of chronic depression, poorer early home environments, and greater comorbidity with anxiety and personality disorders than the less chronic class. In addition, we hypothesized that they would have poorer outcomes at follow-up, with more severe depressive symptoms, poorer social and global functioning, and more suicide attempts and hospitalizations.
Method
Subjects
The sample and methods have been described previously (Klein et al., 1995, 2006). The sample included 142 outpatients aged 18–60 years in a current episode of major depressive disorder (MDD) and/or dysthymic disorder (DD) selected from consecutive admissions to clinics at Stony Brook University. Diagnoses were based on DSM-III-R (American Psychiatric Association, 1987); the symptom and duration criteria for MDD and DD have remained virtually unchanged in DSM-IV (American Psychiatric Association, 1994) and DSM-5. The project began as a family study; to include more familial cases, we required that DD patients have the early-onset (< 21 years) subtype and MDD patients have an onset before age 35.
Patients were 70.9% female and 89.8% Caucasian. Their mean age was 31.4 years (SD=9.07) and they averaged 13.6 (SD=2.27) years of education. At study entry, 47.2% had never married, 29.9% were married or cohabiting, 21.3% were divorced or separated, and 1.6% were widowed. Baseline depressive diagnoses were non-chronic MDD with no DD (31.5%), DD with no major depressive episode (28.3%), or a chronic form of MDD (primarily double depression; 40.2%); 31.5% also had a current anxiety disorder and 45.7% had a personality disorder.
We conducted four follow-up assessments at 30-month intervals over 10 years. The 127 patients (89.4%) who completed at least one follow-up comprise the analysis sample. Of the 127 participants, 10 (7.9%), 7 (5.5%), 22 (17.3%), and 88 (69.3%) patients completed one, two, three, and four follow-ups, respectively. Patients with (n = 127) and without (n = 15) at least one follow-up assessment did not differ significantly on any of the demographic, baseline, or risk factor variables in Table 1.
Table 1.
Comparison of Spline Regression Models
| Outcome/Model | Social Functioning
|
GAF
|
HAM-D
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GCV | AICC1 | AIC | BIC | GCV | AICC1 | AIC | BIC | GCV | AICC1 | AIC | BIC | |
| 30-month outcome | ||||||||||||
| 1 Linear | 0.0121 | 150.1 | 34.9 | 40.4 | 1.1585 | 666.0 | 550.8 | 556.2 | 0.5711 | 586.1 | 470.9 | 476.3 |
| 1 Quadratic | 0.0114 | 143.5 | 28.2 | 36.4 | 1.1451 | 664.8 | 549.4 | 557.6 | 0.5449 | 580.9 | 465.5 | 473.7 |
| 1 Cubic | 0.0116 | 145.7 | 30.2 | 41.1 | 1.1590 | 666.3 | 550.7 | 561.6 | 0.5520 | 582.5 | 466.9 | 477.8 |
| 2 Linear | 0.0112 | 141.9 | 26.6 | 34.7 | 1.1272 | 663.0 | 547.6 | 555.8 | 0.5353 | 578.9 | 463.5 | 471.7 |
| Flat + Linear | 0.0113 | 142.6 | 27.4 | 32.8 | 1.1440 | 664.6 | 549.4 | 554.8 | 0.5458 | 581.0 | 465.7 | 471.2 |
| 2 Flat | 0.0121 | 150.8 | 35.6 | 41.0 | 1.2849 | 677.7 | 562.5 | 567.9 | 0.6168 | 594.8 | 479.6 | 485.0 |
| 3 Linear | 0.0111 | 141.2 | 25.6 | 36.6 | 1.1233 | 662.7 | 547.2 | 558.1 | 0.5370 | 579.3 | 463.8 | 474.7 |
| 60-month outcome | ||||||||||||
| 1 Linear | 0.0162 | 180.6 | 66.4 | 71.8 | 1.5039 | 688.4 | 574.1 | 579.6 | 0.9175 | 633.0 | 518.8 | 524.2 |
| 1 Quadratic | 0.0158 | 178.5 | 64.2 | 72.3 | 1.3800 | 678.8 | 564.5 | 572.6 | 0.8463 | 624.1 | 509.7 | 517.8 |
| 1 Cubic | 0.0161 | 180.7 | 66.1 | 77.0 | 1.4056 | 681.0 | 566.5 | 577.3 | 0.8612 | 626.2 | 511.6 | 522.5 |
| 2 Linear | 0.0159 | 178.6 | 64.2 | 72.4 | 1.3735 | 678.3 | 563.9 | 572.1 | 0.8324 | 622.2 | 507.8 | 516.0 |
| Flat + Linear | 0.0156 | 176.5 | 62.2 | 67.7 | 1.3487 | 676.2 | 561.9 | 567.4 | 0.8181 | 620.2 | 505.9 | 511.4 |
| 2 Flat | 0.0161 | 180.0 | 65.8 | 71.2 | 1.5494 | 691.7 | 577.5 | 582.9 | 0.8810 | 628.5 | 514.2 | 519.7 |
| 3 Linear | 0.0159 | 179.2 | 64.6 | 75.5 | 1.3738 | 678.5 | 563.9 | 574.8 | 0.8397 | 623.3 | 508.8 | 519.6 |
| 90-month outcome | ||||||||||||
| 1 Linear | 0.0149 | 171.5 | 57.3 | 62.7 | 1.6063 | 695.7 | 581.5 | 587.0 | 0.9101 | 632.1 | 517.9 | 523.3 |
| 1 Quadratic | 0.0144 | 167.5 | 53.1 | 61.3 | 1.5215 | 689.8 | 575.4 | 583.6 | 0.8081 | 618.9 | 504.5 | 512.7 |
| 1 Cubic | 0.0145 | 168.6 | 54.1 | 65.0 | 1.5383 | 691.1 | 576.6 | 587.4 | 0.8226 | 621.0 | 506.4 | 517.3 |
| 2 Linear | 0.0142 | 166.2 | 51.8 | 60.0 | 1.5138 | 689.2 | 574.8 | 583.0 | 0.8104 | 619.2 | 504.8 | 513.0 |
| Flat + Linear | 0.0140 | 164.8 | 50.6 | 56.0 | 1.4892 | 687.3 | 573.0 | 578.5 | 0.7958 | 617.1 | 502.9 | 508.3 |
| 2 Flat | 0.0144 | 167.6 | 53.4 | 58.8 | 1.5494 | 691.7 | 577.5 | 582.9 | 0.8416 | 623.3 | 509.1 | 514.6 |
| 3 Linear | 0.0140 | 165.1 | 50.6 | 61.4 | 1.5260 | 690.2 | 575.7 | 586.5 | 0.8096 | 619.2 | 504.7 | 515.5 |
| 120-month outcome | ||||||||||||
| 1 Linear | 0.0140 | 140.4 | 36.2 | 41.4 | 1.1998 | 594.5 | 490.3 | 495.5 | 0.8269 | 556.6 | 452.3 | 457.6 |
| 1 Quadratic | 0.0129 | 132.7 | 28.3 | 36.2 | 1.0955 | 585.4 | 481.0 | 488.8 | 0.7801 | 550.7 | 446.3 | 454.2 |
| 1 Cubic | 0.0131 | 134.3 | 29.7 | 40.2 | 1.1166 | 587.5 | 482.8 | 493.3 | 0.7951 | 552.8 | 448.2 | 458.7 |
| 2 Linear | 0.0128 | 131.7 | 27.3 | 35.2 | 1.0771 | 583.6 | 479.2 | 487.1 | 0.7777 | 550.4 | 446.0 | 453.9 |
| Flat + Linear | 0.0127 | 130.6 | 26.3 | 31.6 | 1.0610 | 582.0 | 477.7 | 483.0 | 0.7644 | 548.5 | 444.3 | 449.6 |
| 2 Flat | 0.0129 | 132.1 | 27.9 | 33.1 | 1.0680 | 582.7 | 478.4 | 483.7 | 0.8203 | 555.7 | 451.5 | 456.8 |
| 3 Linear | 0.0129 | 132.4 | 27.8 | 38.3 | 1.0704 | 583.1 | 478.5 | 489.0 | 0.7899 | 552.2 | 447.5 | 458.0 |
Note: Seven spline regression models were fit for each outcome (social functioning, Global Assessment of Functioning [GAF], and Hamilton Rating Scale for Depression [HAM-D]) at each follow-up (30-month, 60-month, 90-month, and 120-month). The analyzed outcome is given in the header row, and the follow-up wave is given in the first column. Models differed with regard to the number of segments (one, two, or three), and shape of the association (flat, linear, quadratic, or cubic) between the predictor—initial course during the first 30 months—and outcome. When a multi-segment model fits best, this suggests presence of qualitatively distinct subgroups within data. Bold indicates best fit among the seven models for a given outcome and follow-up. GCV = Generalized Cross Validation criterion, AICC1 = Akaike Information Criterion Corrected 1, AIC = Akaike Information Criterion, BIC = Bayesian Information Criterion.
The study was naturalistic. The proportion of the sample receiving treatment at each follow-up ranged from 40.7% – 54.5%. As described elsewhere, treatment was generally not associated with outcomes (Klein et al., 2006). The study was approved by the Stony Brook University Institutional Review Board and written informed consent was obtained from all participants.
Baseline Measures
The baseline evaluation, conducted shortly after admission, included the Structured Clinical Interview for DSM-III-R (SCID; Spitzer, Williams, Gibbon, & First, 1990), 24-item Hamilton Depression Rating Scale (HAM-D; Miller, Bishop, Norman, & Maddever, 1985), and Personality Disorder Examination (Loranger, 1988). A second rater administered a semi-structured interview assessing the home environment before age 15, including quality of parenting and history of sexual abuse (Lizardi, et al., 1995).
As described more fully in earlier publications (e.g., Klein et al., 1995; Lizardi et al., 1995), interrater reliabilities, expressed as Kappa (K), for diagnoses of current MDD, DD, anxiety disorder and personality disorder were .78, .90, 1.00, and .80, respectively. Interrater reliabilities for quality of maternal and paternal parenting, expressed as intraclass correlations (ICC), were .79, and .76, respectively. Interrater reliability for physical and sexual abuse were both K = .68.
All available first-degree relatives were interviewed with the SCID and patients provided information about the remaining family members using the Family History Research Diagnostic Criteria interview guide (FH-RDC; Andreasen, Endicott, Spitzer, & Winokur, 1977). We were able to obtain direct interviews with 40% of the relatives. Of the remaining relatives who were not available for direct interview (e.g., due to death or lack of proband or relative consent), we attempted to obtain additional information on the FH-RDC from a second family member. Overall, we were able to obtain at least two sources of information (direct and family history interview or two family history interviews) for 73% of all relatives (see Klein et al., 1995 for details). Interviewers were unaware of patients’ diagnoses. Relatives’ diagnoses were derived using a consensus best-estimate procedure (Klein, Ouimette, Kelly, Ferro, & Riso, 1994). Interrater reliabilities of relatives’ best-estimate diagnoses of MDD and DD were K = .90, and .75, respectively.
Follow-up Measures
Follow-up evaluations of patients included the 24-item HAM-D and the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al., 1987). The LIFE is a semi-structured interview that assesses the longitudinal course of specific disorders and social functioning. Psychiatric Status Ratings (PSRs) for MDD and DD were made for each month of follow-up. The PSRs for MDD and DD were combined to create an overall depression PSR variable as follows: 1 = minimal/no symptoms of MDD or DD; 2 = subthreshold symptoms of MDD or DD, but does not meet criteria for either; 3 = full symptom criteria for DD (i.e., depressed mood plus at least two other symptoms most of the day, for more days than not, for the entire month) but not MDD; 4 = full criteria for MDD (i.e., depressed mood and/or loss of interest or pleasure and a total of 5 symptoms most of the day nearly every day for a minimum of two consecutive weeks during that month) (see Klein et al., 2006). Thus, each level of the scale involves a progressive increase in symptom severity, as well as a likely increase in persistence (e.g., 3 = “more days than not” for the month; 4 = “nearly every day” for a minimum of two consecutive weeks during that month). Depression PSRs were averaged across the first follow-up interval to create an index of the course of depression over the initial 30 months of the follow-up. This mean depression PSR score can be interpreted as reflecting the severity-weighted persistence of depression across the first follow-up interval.
The LIFE social functioning module assessed impairment in work, school, interpersonal relationships, house work, and parenting in the past month (Leader & Klein, 1996). We used the interviewer-rated global social functioning scale for the last month in each follow-up interval, with scores ranging from 1 = “no impairment/very good adjustment” to 6 = “incapacitation in major role”. Interviewers completed the Global Assessment of Functioning (GAF) scale, rating the worst week of the last month of each follow-up interval on a 1–100 scale, with 1 reflecting the lowest and 100 the highest level of global functioning.
Follow-up interviews were conducted by masters- and doctoral-level clinicians who were unaware of patients’ baseline data. Interrater reliabilities, expressed as ICCs, were .79, .96, .87, and .88 for mean depression PSR, HAM-D, social functioning, and GAF, respectively.
The three outcome measures were correlated as expected. Correlations across follow-ups ranged from .52 to .65 (median = .61) for HAM-D and social adjustment; −.64 to −.83 (median = −.77) for HAM-D and GAF; and −.78 to −.81 (median = −.80) for social adjustment and GAF.
Data Analysis
First, we examined the relationships of initial prospective course, as operationalized by mean depression PSR score over the initial 30-month follow-up period, with HAM-D, LIFE social adjustment, and GAF scores at the end of each follow-up period (12 relationships in total) using spline regression. Spline regression is a piecewise regression procedure that fits polynomial functions onto segments of the regression line between predictor and outcome variables (Marsh & Cormier, 2001; Muggeo, 2003). The number, length, and shape (degree of polynomial) of segments can vary. The transition between segments can be smooth or with a sharp boundary. We selected transition type, number, and shape of segments; the procedure determined starting points, slopes, and endpoints of segments and assessed model fit.
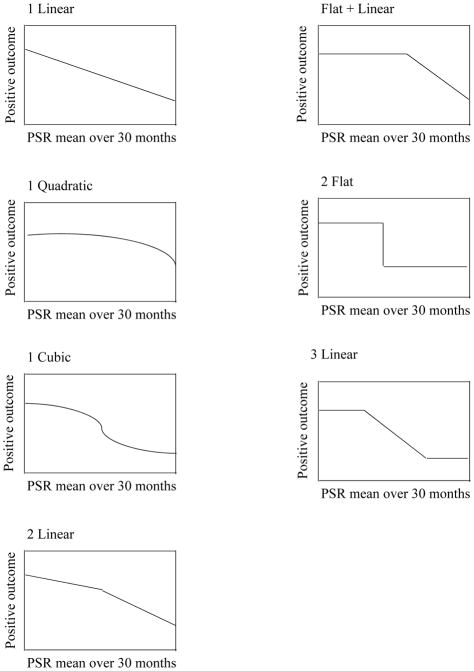
We tested 7 models of the relationship between course during the first follow-up interval and each of the 3 outcome variables at each of the 4 follow-up assessments. The 7 models, graphically depicted in Figure 1, included 3 types of continuous relationships between initial course and outcome: 1 linear segment, 1 quadratic segment, and 1 cubic segment. We also tested 3 types of models with a single boundary: 2 linear segments (reflecting linear associations in both classes); a flat segment and a linear segment (reflecting a linear association in one of the two classes); and 2 flat segments (a “step-function” with no linear within-class relationships between initial course and outcome). Finally, we tested 1 model with 3 linear segments, reflecting 2 discrete boundaries and linear associations between initial course and outcome in each of the 3 classes. Thus, each of these 7 models were fit to the 12 scatterplots between mean depression PSR and the 12 outcomes (three measures at four occasions).
Figure 1.
Illustrative depictions of the seven spline models fit to describe relations between predictor and outcomes. Y-axis is the outcome measure keyed in positive direction; the same direction as Global Assessment of Functioning (GAF), but opposite to Hamilton Depression Rating Scale (HAM-D) and social functioning measure.
We used 4 fit indices--ordered from least to most parsimonious--to compare the fit of the spline regression models: the Akaike information criterion (AIC), the generalized cross-validation criterion (GCV), the Akaike information criterion corrected 1 (AICC1), and the Bayesian Information Criterion (BIC) (Akaike, 1998; Burnham & Anderson, 2002; Craven & Wahba, 1978; Hurvich, Simonoff, &, Tsai, 1998). These indices do not have absolute cutoffs, but can be used to compare models; lower values represent better fit.
In order to validate the findings from these analyses, we assigned patients to groups based on the segments identified in the spline regression using their course during the first follow-up interval, as operationalized by mean PSR score, and compared the groups on baseline characteristics, risk factors, and outcomes. Chi-Square and Fisher’s Exact tests were used for categorical variables; t-tests were used for quantitative variables. Based on the literature (Klein & Allmann, 2014; Klein & Black, in press), we expected that the empirically-defined chronic group would be more likely to have had a chronic depression diagnosis at baseline, higher rates of anxiety and personality disorder diagnoses, a greater family history of DD, more childhood sexual abuse and poorer parenting, and poorer functioning on the three outcome variables (HAM-D, social adjustment, and GAF), than the empirically-defined less chronic group. Hence, one-tailed tests were employed in these comparisons.
Results
Spline Regression Analyses
We fit the spline regression models described above to the data on the associations between course during the first follow-up interval and the outcome variables assessed at each follow-up evaluation. Table 1 reports model fit for the 7 functional relationships depicted in Figure 1 of course during the first 30 months of follow-up with the 3 outcome variables (HAM-D, social adjustment, GAF) at the 4 outcome assessments (30, 60, 90, and 120-months) using the 4 fit indices.
The results were remarkably consistent (see Table 1). As indicated by the bolded values in the table, the discontinuous (i.e., multi-segment) models provided a better fit than the continuous (1-segment linear, quadratic, or cubic) models for each of the 3 outcomes at each of the 4 follow-ups on all 4 fit indices. Moreover, after the first follow-up wave, the model with 1 flat and 1 linear segment (“flat + linear”) provided the best fit for all 3 outcomes in each of the 60-, 90-, and 120-month follow-ups on all 4 fit indices.
The analyses were less consistent at the 30-month evaluation; the GVC, AIC, and AICC1 supported the 3 linear or 2 linear segments models, and the BIC supported the 1 flat segment and 1 linear segment model. We selected this last model, owing to BIC’s greater emphasis on parsimony.
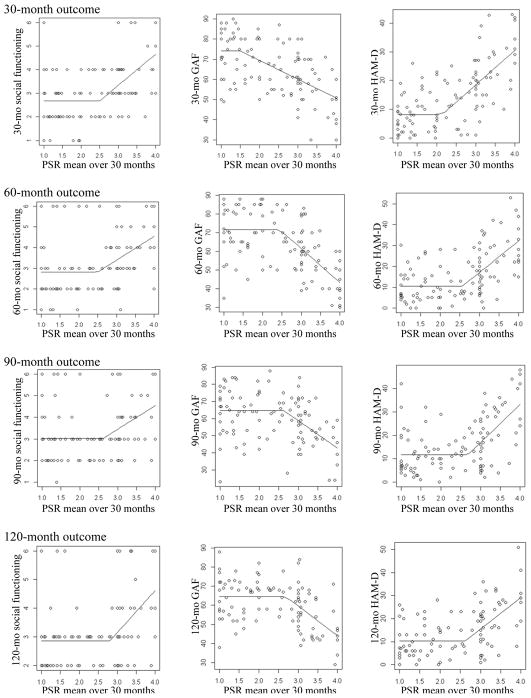
The results for the best-fitting (1 flat segment plus 1 linear segment) spline model for each outcome at each follow-up assessment are illustrated in Figure 2. Each panel depicts how the relationship between mean depression PSR score during the first 30 months of follow-up (plotted on the X-axis) and an outcome at a given follow-up (plotted on the Y-axis) changes across the range of the PSR scores from the initial follow-up period. It is noteworthy that the point demarcating the 2 segments (i.e., the point of discontinuity, or “knot”) was nearly identical across all analyses (PSR=2.4 – 2.8; about mid-way between subthreshold depression and DD), with the exception of the 30-month outcomes, where it was more variable (PSR=1.48 – 2.50).
Figure 2.
Curves for the best-fitting spline models (flat + linear) for each outcome and follow-up. The curves depict the relationship between the mean Psychiatric Status Rating (PSR) during the first 30 months of follow-up (X-axis) and the outcomes (Y-axis), and show how this relationship changes across the range of PSR scores. Social functioning is in the first column, Global Assessment of Functioning (GAF) in the second column, and Hamilton Depression Rating Scale (HAM-D) in the third column; panels are organized in order of follow-up wave from 30-month (top) to 120-month (bottom).
Overall, the data in Table 1 and Figure 2 indicate that for patients with a better course during the first follow-up period (i.e., mean depression PSR scores below the knot), there is no association of initial course with symptom and functional outcomes in subsequent follow-ups. However, for patients with a worse course during the first follow-up period (mean depression PSR scores above the knot), there is a linear relationship, with a poorer initial course predicting higher levels of depression and poorer social adjustment and global functioning at all follow-ups.1
Validating the Distinction
In order further test the validity of the results of the spline regression analyses, we assigned patients to groups based on their course over the first follow-up interval. Knot values were inconsistent for the 30-month outcomes but similar for all subsequent waves. Therefore we used the median value of the knots for the flat-linear segments solution across analyses of 60-, 90-, and 120-month outcomes (PSR=2.62) as the cut-point for assigning patients to the two empirically-derived groups. Sixty-three patients were assigned to the chronic group and 64 patients to the non-chronic group.
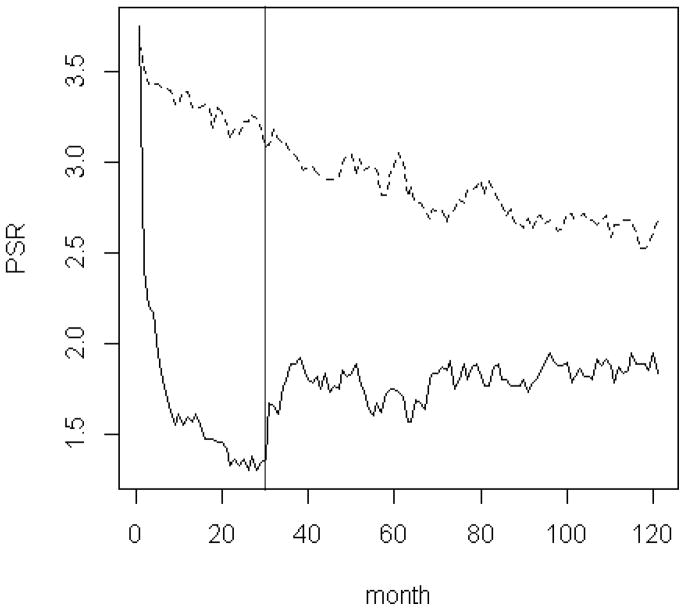
The 2 groups did not differ on duration of follow-up. Their 10-year course of depression (monthly depression PSRs) appears in Figure 3. As can be seen in the figure, the groups were equally depressed when they entered the study. Over the following 30 months—the period used to define the groups—virtually all patients in the empirically-defined non-chronic group remitted, whereas patients in the empirically-defined chronic group experienced only minor improvement. After the definition period, the empirically-defined non-chronic group exhibited a modest rebound of depressive symptoms, but within several months their symptoms stabilized below the subthreshold level, at a depression PSR of less than 2. The empirically-defined chronic group slowly continued to improve until month 70, when they stabilized at a depression PSR of about 2.5, indicating significant persisting depressive symptoms.
Figure 3.
Psychiatric Status Ratings (PSRs) across 120 months since study enrollment for the two empirical groups. Persistent group is dashed line, non-persistent is solid line; X-axis is months since study enrollment; Y-axis is the monthly PSR rating. The initial period of illness course that was used to define the groups is to the left of the vertical line.
We compared these empirically-defined chronicity groups on key baseline characteristics and subsequent outcomes (Table 2). The 2 groups were similar on demographics, except that the more chronic group had attained less education. The groups differed significantly on baseline depression diagnosis: 88.9% of the empirically-defined chronic group had a DSM-III-R diagnosis of chronic depression at baseline, compared to 48.4% of the empirically-defined non-chronic group. The groups did not differ on baseline HAM-D and social adjustment, but the chronic group had a poorer baseline GAF. As hypothesized, compared to the non-chronic group, patients in the empirically-defined chronic group were significantly more likely to have comorbid anxiety and personality disorders, a family history of DD (but not MDD), a childhood history of sexual abuse and higher levels of maladaptive parenting by both parents.
Table 2.
Comparisons of Groups Based on First 29 Months of Follow-Up
| Variable | Non-Persistent Group (N = 64)
|
Persistent Group (N = 63)
|
Test statistic | ||
|---|---|---|---|---|---|
| M (SD) | N (%) | M (SD) | N (%) | ||
| Demographics | |||||
| Age | 30.88 (8.80) | 31.94 (9.38) | t (125) = −0.66, NS | ||
| Sex, male | 19 (29.7%) | 18 (28.6%) | FET, p = 1.00 | ||
| Marital status | χ2 (3) = 0.13, NS | ||||
| Never married | 30 (46.9%) | 30 (47.6%) | |||
| Married | 20 (31.3%) | 18 (28.6%) | |||
| Divorced/separated | 13 (20.3%) | 14 (22.2%) | |||
| Widowed | 1 (1.6%) | 1 (1.6%) | |||
| Education, years | 14.02 (2.36) | 13.10 (2.10) | t (125) = 2.32, p = 02 | ||
| Risk factors | |||||
| Family history of MDD | 45 (70.0%) | 41 (65.1%) | FET p = .57 | ||
| Family history of dysthymia | 13 (20.3%) | 22 (34.9%) | FET p = .05 | ||
| Quality of maternal parenting | 1.23 (1.48) | 1.91 (1.81) | t (119.6) = −2.30, p = .01 | ||
| Quality of paternal parenting | 1.80 (1.65) | 2.58 (1.82) | t (121) = −2.47, p < .01 | ||
| Childhood sexual abuse | 11 (17.2%) | 20 (31.7%) | FET p = .04 | ||
| Baseline | |||||
| HAM-D | 26.91 (8.50) | 27.19 (10.92) | t (117.0) = −0.16, NS | ||
| Social adjustment | 3.94 (0.94) | 4.11 (1.18) | t (117.9) = −0.92, NS | ||
| GAF | 58.88 (9.00) | 54.83 (10.22) | t (125) = 2.37, p < .02 | ||
| Depression diagnosis | χ2 (2) = 24.34, P < .001 | ||||
| Non-chronic MDD | 33 (51.6%) | 7 (11.1%) | |||
| Dysthymia | 14 (21.6%) | 22 (34.9%) | |||
| Chronic form of MDD | 17 (26.6%) | 34 (54.0%) | |||
| Anxiety disorder | 13 (20.3%) | 27 (42.9%) | FET, p = .005 | ||
| Personality disorder | 19 (29.7%) | 39 (61.9%) | FET p < .001 | ||
| Follow-up | |||||
| Follow-up Duration, months | 114.08 (23.21) | 112.05 (22.66) | t (125) = 0.50, NS | ||
| HAM-D 30 months | 9.07 (7.03) | 21.46 (10.68) | t (80.9) = −7.08, p < .001 | ||
| HAM-D 60 months | 10.45 (7.94) | 21.54 (12.52) | t (95.2) = −5.62, p < .001 | ||
| HAM-D 90 months | 11.75 (8.47) | 21.25 (12.13) | t (94.1) = 4.77, p < .001 | ||
| HAM-D 120 months | 10.23 (7.58) | 19.13 (11.20) | t (78.8) = 4.62, p < .001 | ||
| Social adjustment 30 months | 2.68 (1.12) | 3.72 (1.25) | t (111) = −4.65, p < .001 | ||
| Social adjustment 60 months | 2.84 (1.40) | 3.72 (1.32) | t (110) = −3.44, p < .001 | ||
| Social adjustment 90 months | 3.05 (1.26) | 3.70 (1.31) | t (110) = −2.68, p < .005 | ||
| Social adjustment 120 months | 2.89 (1.03) | 3.51 (1.37) | t (84.6) = −2.55, p < .01 | ||
| GAF 30 months | 71.38 (11.66) | 57.94 (12.59) | t (111) = 5.87, p < .001 | ||
| GAF 60 months | 71.44 (13.08) | 56.09 (13.62) | t (110) = 6.08, p < .001 | ||
| GAF 90 months | 64.62 (13.57) | 54.78 (13.69) | t (110) = 3.82, p < .001 | ||
| GAF 120 months | 64.29 (9.83) | 55.85 (12.58) | t (110) = 3.80, p < .001 | ||
| Depressed at end of follow-upa | 9 (16.7%) | 25 (54.3%) | FET p < .001 | ||
| Suicide attemptb | 0 (0.0%) | 13 (26.5%) | FET p < .001 | ||
| Psychiatric hospitalizationb | 3 (5.9%) | 18 (34.6%) | FET p < .001 | ||
Defined as meeting symptom criteria for dysthymia (Psychiatric Status Rating [PSR] = 3) or MDD (PDSR = 4) on the Longitudinal Follow-up Interval Evaluation in the final month of the 120 month follow-up.
Any suicide attempt or psychiatric hospitalization between month 30 and month 120 during the follow-up.
MDD = Major Depressive Disorder; FET = Fishers Exact Test; HAM-D = Hamilton Rating Scale for Depression; GAF = Global Assessment of Functioning.
At each of the four follow-up evaluations, patients assigned to the empirically-defined chronic group on the basis of their course during the initial follow-up period had significantly higher HAM-D scores and poorer social adjustment and global functioning than the non-chronic group. Patients in the empirically-defined chronic group were also much more likely to meet symptom criteria for a depressive disorder in their final month of follow-up. Finally, after excluding the initial follow-up interval to prevent confounding, patients in the empirically-defined chronic group had strikingly higher rates of attempted suicide and psychiatric hospitalization during the remainder of the study (i.e., months 31 – 120).
Discussion
We observed a sharp and consistent discontinuity in the relationship of depression course over a 2.5-year period with subsequent symptom, social functioning, and global outcomes in a sample of outpatients who sought treatment for non-bipolar depression and were then followed for 10 years. The findings were remarkably consistent across 4 follow-up waves, 3 outcome variables, and 4 fit indices. Moreover, the empirically-determined point of discontinuity was almost identical across analyses, and appeared near the mid-point between subthreshold depressive symptoms and DD, which is consistent with the current conceptualization of persistent depression as being present for at least half the time for two years.
In order to further validate these findings, we assigned patients to empirically-defined groups based on their course during the first follow-up interval. The empirically-defined chronic group was characterized by significantly higher rates of baseline DSM-III-R chronic depression diagnoses, comorbid anxiety and personality disorders; family history of DD (but not MDD); and histories of poorer parenting and greater sexual abuse than the non-chronic group. The empirically-defined chronic group also exhibited significantly poorer outcomes in subsequent follow-up waves, with greater depressive symptoms and poorer social and global functioning at the 60-, 90-, and 120-month evaluations, as well as dramatically higher rates of attempted suicide, psychiatric hospitalization, and current depressive disorders at the final follow-up assessment. Taken together, these data suggest that a consideration of longitudinal course reveals qualitative distinctions within the depressive disorders.
Our results are consistent with two previous findings suggesting qualitative differences between chronic and non-chronic depressions. First, chronic depression aggregates in families of probands with chronic, but not episodic depression (Klein et al., 1995, 2004; Mondimore et al., 2006). Second, when patients with chronic depression recover and then relapse, it is generally into another period of chronic depression; in contrast, when patients with episodic MDD relapse, it is typically into a non-chronic episode (Klein et al., 2006).
The lack of association between depression during the first follow-up interval and subsequent symptom, social functioning, and global outcomes for the group with the better initial course, but a strong linear relationship for patients with greater chronicity suggests that these two types of depression reflect distinct etiological or maintenance processes. Importantly, the absence of an association for the group with the better initial course is not due to insufficient variation in symptoms after recovery from the index episode, as the means and standard deviations in Table 1 do not suggest floor effects and 73.4% of these patients had at least one further episode of MDD during the follow-up. Rather, it appears that course does not appear to be an important factor in outcomes for the less chronic group.
In contrast, in the more chronic group, mean level of depressive symptoms over the first study interval was linearly related to all outcomes in the three subsequent follow-ups. Thus, the best-fitting model did not take the form of a step-function. Rather, degree of chronicity appears to be an important predictor of outcomes, but only after it reaches a critical threshold. A prominent challenge for future research is to elucidate the process(es) underlying the linear relationship between course during the initial follow-up interval and longer term outcomes among patients with chronic depressions. This finding may reflect pre-existing individual differences in a liability for a more chronic course (e.g., genes, temperament, environmental adversity); the effects of associated poor prognostic factors (e.g., comorbid anxiety and personality disorders) that are difficult to disentangle from chronic depression and may derive from overlapping definitions and/or shared etiological influences; or recursive processes in which depression is maintained over time due to factors such as stress generation or maladaptive cognitions, coping, or interpersonal behavior (Hammen, 2006; Joiner, 2000; Klein & Allmann, 2014; Pettit, Hartley, Lewinsohn, Seeley, & Klein, 2013; Wilson, DiRago, & Iacono, 2014).
The results of the spline regression analyses with the 30-month outcomes were less consistent than with the outcomes at 60-, 90-, and 120-months. This is likely due to criterion contamination; the outcome (month 30) immediately followed the predictor (months 1 – 29), hence recall biases may have distorted true associations.
It is important to note that our measure of course (the depression PSRs) blended the severity and persistence of symptoms, in that patients could receive a rating of 4 with more severe, but not necessarily more persistent, symptoms. This is consistent with the conceptualization of chronic depression in DSM-5, which includes PDD as an overarching category but also includes specifiers to distinguish between DD, double depression, and chronic major depression. However, as described in footnote 1, use of a “purer” measure of persistence also found consistent evidence of discontinuity, although it was difficult to choose between the flat-linear and 2 flat (step-function) models. It may be worthwhile for future studies to use measures that separate the dimensions of symptom severity and persistence more cleanly in order to test their unique contributions to understanding etiological mechanisms, course, and treatment response.
Our findings are consistent with DSM-5’s decision to distinguish between PDD and MDD. However, it is important to note that our empirically-defined groups do not map precisely onto DSM-5 diagnoses. While 89% of patients in the more chronic class received chronic depression diagnoses in the baseline assessment, so did 48% of the less chronic class. In part, this may be due to the fact that the two sets of classes were defined using different time periods (up to study entry for the DSM; following study entry for our prospect course-based classification). In addition, the relatively favorable course of patients with a DSM-III-R diagnosis of chronic depression who were placed in the non-chronic class could be due to effective treatment, errors or biases in their retrospective reporting of course during the baseline assessment, or the failure of the DSM criteria to optimally distinguish chronic from non-chronic depression. Future studies should determine how successfully the DSM-5 criteria for PDD identify a discrete subgroup and evaluate alternative criteria for persistent depression (see Klein, 2008 for a discussion of several approaches to defining chronic depression).
The present findings should be viewed as a step towards developing a more comprehensive life-course perspective on depressive disorders (Klein & Allmann, 2014; Monroe & Harkness, 2011). Most current research on the etiology and treatment of depression combines persistent and non-persistent cases. The results of this study suggest that ignoring differences in course may introduce substantial heterogeneity that can obscure important findings. Thus, if different levels of chronicity are associated with differences on etiological, pathophysiological, or maintaining factors, or response to specific treatments, studies that combine these groups may fail to detect significant effects or falsely attribute effects to subgroups for which they do not apply.
It is worth noting that there appears to be growing interest in using course, alone or in conjunction with other factors, to parse the heterogeneity of depression. For example, Monroe and Harkness (2011) contributed an incisive analysis of the single versus recurrent episode distinction and highlighted a number of key questions for future research. In addition, Wakefield and colleagues (e.g., Wakefield & Schmitz, 2014) have proposed that individuals with relatively brief episodes of MDD (< 6 months) in the context of a precipitant, relatively mild impairment, and no suicidality, psychomotor retardation, or worthlessness should be considered as having a benign subtype of depression that differs from more severe and persistent depressive conditions. The present findings suggest that it may be worthwhile to continue this line of inquiry.
Strengths and Limitations
The present study had several significant strengths. Most studies of the natural structure of depression have focused on cross-sectional symptoms (Andrews et al., 2007; Haslam et al., 2012; Solomon et al., 2001), neglecting other parameters--such as course--that have historically been fundamental to delineating mental disorders (Kendler, 2009; Klein, 2008). This is the first study to directly test for a discontinuity in the chronicity of depression. In addition, we conducted five assessments carefully documenting course of depression over 10 years. This provided multiple internal replications, progressively raising the bar by requiring initial course to predict increasingly distal outcomes. Finally, we used spline regression, a novel, powerful approach to investigating nosological questions that is readily applicable to course data (Kotov et al., 2013).
However, a number of limitations should also be considered. First, the sample size was only moderate. Second, participants entered the study at different points in their episode and with varying histories of depression. Following the Collaborative Depression Study (Keller, Boland, Leon, Solomon, Endicott, & Li,, 2013), we examined the period assessed prospectively from study entry, rather than estimating past course from the SCID due to the higher quality of data afforded by the LIFE, which was developed explicitly to chart the course of psychopathology. However, it is conceivable that results could differ if another time period (e.g., the 30 months prior to study entry) was examined. It will be particularly important to follow individuals experiencing a first-episode of depression and test for non-linearity in subsequent course, although such data are rare and challenging to collect. Third, we required a relatively early onset of depression (< 21 for DD; < 35 for MDD), hence the results may not apply to late-onset chronic depression, which is less familial and has lower rates of early adversity and comorbidity (Klein & Black, in press). Fourth, although attrition was relatively low, participants and sample sizes differed somewhat across follow-up waves. Fifth, we used a patient sample, which has greater clinical relevance but is not representative of cases in the community and may have a more persistent course and poorer outcomes (Klein et al., 2006; Rhebergen et al., 2009). Finally, the patients were predominantly Caucasian. As there is some evidence that depression may have a poorer course in African-Americans and Caribbean Blacks than Caucasians (Williams et al., 2007), it will be important to determine if these results generalize to more diverse samples.
In conclusion, the consistent evidence of non-linearity in this study suggests that chronicity may be useful in distinguishing between qualitatively different forms of depression, although further work is needed to determine how to best characterize and distinguish them. More broadly, our findings underscore the value of using longitudinal course to parse depression into more homogeneous subgroups which may help elucidate etiological and pathophysiological processes and develop more effective treatments (Klein & Allmann, 2014).
General Scientific Summary.
Depression can assume a variety of course patterns, ranging from a brief episode to a chronic condition that persists for decades. However it is unclear whether variations in course are continuous or reflect qualitatively distinct subgroups. Our findings indicate that there are qualitatively distinct classes of chronic and non-chronic depressions that differ on a range of risk factors and long-term outcomes.
Acknowledgments
This paper was supported by NIMH grants RO1 MH45757 (Klein) and RO1 MH094398 (Kotov). We thank Jinmaio Fu for assistance with data analyses.
Footnotes
In order to derive a “pure” measure of persistence that was not weighted by severity, we collapsed depression PSRs of 3 and 4 so that patients received a score of 3 if they were depressed for at least half the time and met symptom criteria for either DD or MDD in that month. Given the high level of chronicity in the sample, this severely truncated the upper range of scores and the results were less stable both in terms of the best-fitting model and point of discontinuity (i.e., the location of the knot). Nonetheless, in all 12 sets of analyses (3 dependent measures at each of 4 follow-up assessments), the best-fitting model was discontinuous, and in 11 of the 12 analyses it specified a single boundary (the 3 linear segments model, with 2 boundaries, provided the best fit for the HAM-D at 30 months). Of the 11 analyses supporting a single discontinuous boundary, the flat-linear model provided the best fit in 5 analyses; the two flat segment (step-function) model provided the best fit in 4 analyses, the flat-linear and the two flat segment models tied for best fit in 1 analysis, and the two linear segment model was best in 1 analysis (30 month GAF). Thus, not surprisingly, eliminating the variation in severity of chronic depression made it difficult to discriminate between the flat-linear and step-function (two flat segment) models. However, it does not alter the conclusion that there is a single discontinuous boundary between levels of depression chronicity.
Contributor Information
Daniel N. Klein, Departments of Psychology and Psychiatry and Behavioral Science, Stony Brook University
Roman Kotov, Departments of Psychiatry and Behavioral Science and Psychology, Stony Brook University.
References
- Akaike H. A new look at statistical model identification. IEEE Transactions on Automatic Control. 1998;19(6):716–723. [Google Scholar]
- Akiskal HS, King D, Rosenthal TL, Robinson D, Scott-Strauss A. Chronic depressions: part I: clinical and familial characteristics in 137 probands. Journal of Affective Disorders. 1981;3(3):297–315. doi: 10.1016/0165-0327(81)90031-8. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 3. Washington, DC: American Psychiatric Association; 1987. revised. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria: Reliability and validity. Archives of General Psychiatry. 1977;34(10):1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- Andrews G, Brugha T, Thase ME, Duffy FF, Rucci P, Slade T. Dimensionality and the category of major depressive episode. International Journal of Methods in Psychiatric Research. 2007;16(S1):S41–S51. doi: 10.1002/mpr.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angst J, Gamma A, Rössler W, Ajdacic V, Klein DN. Long term depression versus episodic major depression: Results from the prospective Zurich study of a community sample. Journal of Affective Disorders. 2009;115:112–121. doi: 10.1016/j.jad.2008.09.023. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Rössler W, Ajdacic V, Klein DN. Childhood adversity and chronicity of mood disorders. European Archives of Psychiatry and Clinical Neuroscience. 2011;261:21–27. doi: 10.1007/s00406-010-0120-3. [DOI] [PubMed] [Google Scholar]
- Benazzi F. Chronic depression: A case series of 203 outpatients treated at a private practice. Journal of Psychiatry and Neuroscience. 1998;23:51–55. [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP. Taxometrics and developmental psychopathology. Development and psychopathology. 2003;15(3):501–527. doi: 10.1017/s0954579403000270. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multimodel inference: A practical information-theoretic approach. 2. New York, NY: Springer-Verlag; 2002. [Google Scholar]
- Blanco C, Okuda M, Markowitz JC, Liu SM, Grant BF, Hasin DS. The epidemiology of chronic major depressive disorder and dysthymic disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2010;71:1645–1656. doi: 10.4088/JCP.09m05663gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multimodel inference: A practical information-theoretic approach. 2. New York: Springer-Verlag; 2002. [Google Scholar]
- Craven P, Wahba G. Smoothing noisy data with spline functions: Estimating the correct degree of smoothing by the method of generalized cross-validation. Numerische Mathematik. 1978;31:377–403. [Google Scholar]
- Evans S, Cloitre M, Kocsis JH, Keitner GI, Holzer CP, Gniwesch L. Social-vocational adjustment in unipolar mood disorders: Results of the DSM-IV field trial. Journal of Affective Disorders. 1996;38:73–80. doi: 10.1016/0165-0327(95)00045-3. [DOI] [PubMed] [Google Scholar]
- Garyfallos G, Adamopoulou A, Karastergiou A, Voikli M, Sotiropoulou A, Donias S, …Paraschos A. Personality disorders in dysthymia and major depression. Acta Psychiatrica Scandinavica. 1999;99:332–340. doi: 10.1111/j.1600-0447.1999.tb07238.x. [DOI] [PubMed] [Google Scholar]
- Gilmer WS, Trivedi MH, Rush AJ, Wisniewski SR, Luther J, Howland RH, … Alpert J. Factors associated with chronic depressive episodes: A preliminary report from the STAR-D project. Acta Psychiatrica Scandinavica. 2005;112:425–433. doi: 10.1111/j.1600-0447.2005.00633.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Schwab-Stone M, Lahey BB, Shaffer D, Jensen PS. Major depression and dysthymia in children and adolescents: Discriminant validity and differential consequences in a community sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:761–770. doi: 10.1097/00004583-200006000-00015. [DOI] [PubMed] [Google Scholar]
- Hammen CL. Stress generation in depressions: Reflections on origins, research, and future directions. Journal of Clinical Psychology. 2006;62(9):1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Haslam N. Kinds of kinds: A conceptual taxonomy of psychiatric categories. Philosophy, Psychiatry, & Psychology. 2002;9(3):203–217. [Google Scholar]
- Haslam N, Holland E, Kuppens P. Categories versus dimensions in personality and psychopathology: A quantitative review of taxometric research. Psychological Medicine. 2012;42:903–920. doi: 10.1017/S0033291711001966. [DOI] [PubMed] [Google Scholar]
- Holm-Denoma JM, Berlim MT, Fleck MPA, Joiner TE. Double depression in adult psychiatric outpatients in Brazil: Distinct from major depression? Psychiatry Research. 2006;144:191–196. doi: 10.1016/j.psychres.2005.06.011. [DOI] [PubMed] [Google Scholar]
- Horwitz AV, Widom CS, McLaughlin J, White HR. The impact of childhood abuse and neglect on adult mental health: A prospective study. Journal of Health and Social Behavior. 2001;42:184–201. [PubMed] [Google Scholar]
- Hurvich CM, Simonoff JS, Tsai CL. Smoothing parameter selection in nonparametric regression using an improved Akaike information criterion. Journal of the Royal Statistical Society, Series B Statistical Methodology. 1998;60(2):271–293. [Google Scholar]
- Joiner TE. Depression’s vicious scree: Self-propagating and erosive processes in depression chronicity. Clinical Psychology: Science and Practice. 2000;7(2):203–218. [Google Scholar]
- Keller MB, Boland R, Leon A, Solomon D, Endicott J, Li C. Clinical course and outcome of unipolar major depression. In: Keller MB, Coryell WH, Endicott J, Maser JD, Schettler PJ, editors. Clinical Guide to Depression and Bipolar Disorder. Washington, DC: American Psychiatric Press; 2013. pp. 155–173. [Google Scholar]
- Keller MB, Klein DN, Hirschfeld RMA, Kocsis JH, McCullough JP, Miller I, … Shea T. Results of the DSM-IV Mood Disorders Field Trial. American Journal of Psychiatry. 1995;152:843–849. doi: 10.1176/ajp.152.6.843. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Neilsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation: A comprehensive method for assessing outcome in longitudinal studies. Archives of General Psychiatry. 1987;44(6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, Shapiro RW. “Double depression”: Superimposition of acute depressive episodes on chronic depressive disorders. American Journal of Psychiatry. 1982;139(4):438–442. doi: 10.1176/ajp.139.4.438. [DOI] [PubMed] [Google Scholar]
- Kendler KS. An historical framework for psychiatric nosology. Psychological Medicine. 2009;39(12):1935–1941. doi: 10.1017/S0033291709005753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN. Classification of depressive disorders in DSM-V: Proposal for a two-dimension system. Journal of Abnormal Psychology. 2008;117(3):552–560. doi: 10.1037/0021-843X.117.3.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Allmann AES. Course of depression: Persistence and recurrence. In: Gotlib IH, Hammen CL, editors. Handbook of depression and its treatment. 3. New York: Guilford Press; 2014. pp. 64–83. [Google Scholar]
- Klein DN, Black SR. Persistent depressive disorder. In: DeRubeis RJ, Strunk DR, editors. Oxford Handbook of Mood Disorders. New York: Oxford University Press; in press. [Google Scholar]
- Klein DN, Kocsis JH, McCullough JP, Holzer CP, III, Hirschfeld RMA, Keller MB. Symptomatology in Dysthymia. Psychiatric Clinics of North America. 1996;19(1):41–55. doi: 10.1016/s0193-953x(05)70272-0. [DOI] [PubMed] [Google Scholar]
- Klein DN, Ouimette PC, Kelly HS, Ferro T, Riso LP. Test-retest reliability of team consensus best-estimate diagnoses of Axis I and II disorders in a family study. American Journal of Psychiatry. 1994;151(7):1043–1047. doi: 10.1176/ajp.151.7.1043. [DOI] [PubMed] [Google Scholar]
- Klein DN, Riso LP. Psychiatric diagnoses: Problems of boundaries and co-occurrences. In: Costello CG, editor. Basic issues in psychopathology. New York: Guilford Press; 1993. pp. 19–66. [Google Scholar]
- Klein DN, Riso LP, Donaldson SK, Schwartz JE, Anderson RL, Ouimette PC, Lizardi H, Aronson TA. Family study of early-onset dysthymia: Mood and personality disorders in relatives of outpatients with dysthymia and episodic major depression and normal controls. Archives of General Psychiatry. 1995;52(6):487–496. [PubMed] [Google Scholar]
- Klein DN, Shankman SA, Lewinsohn PM, Rohde P, Seeley JR. Family study of chronic depression in a community sample of young adults. American Journal of Psychiatry. 2004;161(4):646–653. doi: 10.1176/appi.ajp.161.4.646. [DOI] [PubMed] [Google Scholar]
- Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. American Journal of Psychiatry. 2006;163(5):872–880. doi: 10.1176/ajp.2006.163.5.872. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Frances AJ. A critical discussion of DSM-III dysthymic disorder. American Journal of Psychiatry. 1987;144(12):1534–1542. doi: 10.1176/ajp.144.12.1534. [DOI] [PubMed] [Google Scholar]
- Kotov R, Leong SH, Mojtabai R, Erlanger ACE, Fochtmann LJ, Constantino E, Carlson GA, Bromet EJ. Boundaries of schizoaffective disorder: Revisiting Kraepelin. JAMA Psychiatry. 2013;70(12):1276–1286. doi: 10.1001/jamapsychiatry.2013.2350. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Akiskal HS, Gatsonis C, Parrone PL. Childhood-onset dysthymic disorder: Clinical features and prospective naturalistic outcome. Archives of General Psychiatry. 1994;51(5):365–374. doi: 10.1001/archpsyc.1994.03950050025003. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Psychiatrie. 6. Leipzig: Barth; 1899. [Google Scholar]
- Leader JB, Klein DN. Social adjustment in dysthymia, double depression, and episodic major depression. Journal of Affective Disorders. 1996;37(2–3):91–101. doi: 10.1016/0165-0327(95)00076-3. [DOI] [PubMed] [Google Scholar]
- Lizardi H, Klein DN, Ouimette PC, Riso LP, Anderson RL, Donaldson SK. Reports of the childhood home environment in early-onset dysthymia and episodic major depression. Journal of Abnormal Psychology. 1995;104(1):132–139. doi: 10.1037//0021-843x.104.1.132. [DOI] [PubMed] [Google Scholar]
- Loranger AW. Personality Disorder Examination manual. New York: DV Communications; 1988. [Google Scholar]
- Markowitz JC, Moran ME, Kocsis JH, Frances AJ. Prevalence and comorbidity of dysthymic disorder among psychiatric outpatients. Journal of Affective Disorders. 1992;24:63–71. doi: 10.1016/0165-0327(92)90020-7. [DOI] [PubMed] [Google Scholar]
- Marsh LC, Cormier DR. Spline regression models. Thousand Oaks, CA: Sage Publications; 2001. Sage University Papers Series on Quantitative Applications in the Social Sciences. [Google Scholar]
- McCullough JP, Klein DN, Keller MB, Holzer CE, Davis SM, Kornstein SG, Howland RH, Thase ME, Harrison WM. Comparison of DSM-III-R chronic major depression and major depression superimposed on dysthymia (double depression): A study of the validity and value of differential diagnosis. Journal of Abnormal Psychology. 2000;109(3):419–427. [PubMed] [Google Scholar]
- McCullough JP, Klein DN, Borian FE, Howland RH, Riso LP, Keller MB, Banks PLC. Group comparisons of DSM-IV subtypes of chronic depression: Validity of the distinctions, Part 2. Journal of Abnormal Psychology. 2003;112(4):614–622. doi: 10.1037/0021-843X.112.4.614. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop S, Norman WH, Maddever H. The Modified Hamilton Rating Scale for Depression: Reliability and validity. Psychiatry Research. 1985;14(2):131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Mondimore FM, Zandi PP, MacKinnon DF, McInnis MG, Miller EB, Crowe RP, Scheftner WA, Marta DH, Weissman MM, Levinson DF, Murphy-Ebenez KP, DePaulo JR, Jr, Potash JB. Familial aggregation of illness chronicity in recurrent, early-onset depression pedigrees. American Journal of Psychiatry. 2006;163(9):1554–1560. doi: 10.1176/ajp.2006.163.9.1554. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Recurrence in major depression: A conceptual analysis. Psychological Review. 2011;118(4):655–674. doi: 10.1037/a0025190. [DOI] [PubMed] [Google Scholar]
- Muggeo VMR. Estimating regression models with unknown break-points. Statistics in Medicine. 2003;22(19):3055–3071. doi: 10.1002/sim.1545. [DOI] [PubMed] [Google Scholar]
- Murphy JA, Byrne GJ. Prevalence and correlates of the proposed DSM-5 diagnosis of Chronic Depressive Disorder. Journal of Affective Disorders. 2012;139(2):172–180. doi: 10.1016/j.jad.2012.01.033. [DOI] [PubMed] [Google Scholar]
- Pepper CM, Klein DN, Anderson RL, Riso LP, Ouimette PC, Lizardi H. Axis II comorbidity in dysthymia and major depression. American Journal of Psychiatry. 1995;152:239–247. doi: 10.1176/ajp.152.2.239. [DOI] [PubMed] [Google Scholar]
- Pettit JW, Hartley C, Lewinsohn PM, Seeley JR, Klein DN. Is liability to recurrent major depressive disorder present before first episode onset in adolescence or acquired after the initial episode? Journal of Abnormal Psychology. 2013;122(2):353–358. doi: 10.1037/a0032655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhebergen D, Beekman ATF, de Graaf R, Nolen WA, Spijker J, Hoogendijk WJ, Pennix BW. The three-year naturalistic course of major depressive disorder, dysthymic disorder and double depression. Journal of Affective Disorders. 2009;115(3):450–459. doi: 10.1016/j.jad.2008.10.018. [DOI] [PubMed] [Google Scholar]
- Riso LP, du Toit PL, Blandino JA, Penna S, Darcy S, Duin JS, … Ulmer CS. Cognitive aspects of chronic depression. Journal of Abnormal Psychology. 2003;112:72–80. doi: 10.1037/0021-843X.112.1.72. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Sholomskas D, Prusoff BA. Chronic mood disorders in depressed outpatients: diagnosis and response to pharmacotherapy. Journal of Affective Disorders. 1980;2(2):73–88. doi: 10.1016/0165-0327(80)90007-5. [DOI] [PubMed] [Google Scholar]
- Ruscio J, Ruscio AM. A structure-based approach to psychological assessment: Matching measurement models to latent structure. Assessment. 2002;9(1):4–16. doi: 10.1177/1073191102091002. [DOI] [PubMed] [Google Scholar]
- Sang W, Li Y, Su L, Yang F, Wu W, Shang X, … Li K. A comparison of the clinical characteristics of Chinese patients with recurrent major depressive disorder with and without dysthymia. Journal of Affective Disorders. 2011;135:106–110. doi: 10.1016/j.jad.2011.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon ARI, Haaga DAF, Arnow BA. Is clinical depression distinct from subthreshold depressive symptoms? A review of the continuity issue in depression research. Journal of Nervous & Mental Disease. 2001;189(8):498–506. doi: 10.1097/00005053-200108000-00002. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R (SCID) Washington, DC: American Psychiatric Press; 1990. [Google Scholar]
- Wakefield JC, Schmitz MF. Predictive validation of single-episode uncomplicated depression as a benign subtype of unipolar major depression. Acta Psychiatrica Scandinavica. 2014;129(6):445–457. doi: 10.1111/acps.12184. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL. The chronic depressive in the community: Unrecognized and poorly treated. Comprehensive Psychiatry. 1977;18(6):523–532. doi: 10.1016/s0010-440x(97)90002-x. [DOI] [PubMed] [Google Scholar]
- Wiersma JE, Hovens JGFM, van Oppen P, Gittay EJ, Van Schaik DJ, Beekman AT, Pennix BW. The importance of childhood trauma and childhood life events for chronicity of depression in adults. Journal of Clinical Psychiatry. 2009;70(7):983–989. doi: 10.4088/jcp.08m04521. [DOI] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Archives of General Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Wilson S, DiRago AC, Iacono WG. Prospective inter-relationships between late adolescent personality and major depressive disorder in early adulthood. Psychological Medicine. 2014;44(03):567–577. doi: 10.1017/S0033291713001104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T, Dunner DL. Differential subtyping of depression. Depression & Anxiety. 2001;13(1):11–17. doi: 10.1002/1520-6394(2001)13:1<11::aid-da2>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]