Abstract
Understanding the association between polysubstance use and impulsivity is pertinent to treatment planning and efficacy. Delay discounting, a measure of impulsivity, supplies the rate at which a reinforcer loses value as the temporal delay to its receipt increases. Excessive delay discounting has been widely observed among drug using individuals; though, the impact of using more than one substance has been only minimally studied. Here, after controlling for demographic variables, we systematically compare delay discounting in community controls, heavy smokers, alcohol-dependent, and cocaine-dependent individuals to assess the impact of non-, mono-, dual-, and tri-substance use. All substance-using groups discount significantly more than community controls (p < 0.05). Additionally, groups that smoke cigarettes in addition to another substance dependency discount significantly more than cigarette smoking alone (p < 0.05). Lastly, tri-substance users who were alcohol-dependent, cocaine-dependent and heavy cigarette smokers discount significantly more than heavy smokers (p < 0.01). However, tri-substance users do not discount significantly more than any dual-substance group. Tri-substance use is associated with greater impulsivity than mono-substance smoking, but no greater impulsivity than dual-substance users, suggesting a ceiling effect on discounting when more than two substances are in use. The present study suggests that smokers who engage in additional substance use may experience worse treatment outcomes given that excessive discounting is predictive of poor therapeutic outcomes in several studies.
Keywords: delay discounting, polysubstance use, alcohol, cocaine, cigarette smoking
Introduction
Delay discounting, or the reduced valuation of future rewards, has been suggested to be a marker of addiction (Bickel, Koffarnus, Moody, & Wilson, 2014). If so, multiple substance use may be associated with greater discounting. However, ceiling effects may be encountered as the number of substances used increases. Here, we explore explicitly the relation of multiple substances on the rate of discounting.
Eighty percent of substance users regularly use more than one substance (Batel, Pessione, Maitre, & Rueff, 1995; Kalman, Morissette, & George, 2005). Despite the prevalence of dual- and tri-substance users, most research to date has reported on mono-substance users—whether that is due to studying mono-substance users or reporting only on the primary substance of use. In order to clarify and extend the understanding of polysubstance use profiles we consider all combinations of cigarette smokers, alcohol-dependent, and cocaine-dependent individuals. Here, substance use profiles were compared in terms of delay discounting
Previously, greater discounting of future rewards has been widely documented in individuals with addiction. Steeper discounting, considered an indicator of a facet of impulsivity, has been observed in cocaine users (Coffey, Gudleski, Saladin, & Brady, 2003.; Heil, Johnson, Higgins, & Bickel, 2006), nicotine users (Bickel, Odum, & Madden, 1999), methamphetamine users (Hoffman et al., 2006), alcohol users (Petry, 2001), and opioid users (Kirby, Petry, & Bickel, 1999; Madden, Petry, Badger, & Bickel, 1997). Indeed, the only substance of abuse that research has not shown to have a clear relationship to delay discounting is marijuana use (Johnson et al., 2010).
Here, we set out to examine the effects of mono-, dual-, and tri-substance use on rates of delay discounting so as to evaluate two opposing hypotheses. Polysubstance use may be associated with additive effects where for each additional substance-used increases the rate of discounting. Alternatively, a ceiling effect may prevent further increments in discounting beyond that seen in mono-substance use.
To date, three previous studies have looked at the relationship between polysubstance dependence and delay discounting (Businelle, McVay, Kendzor, & Copeland, 2010; García-Rodríguez, Secades-Villa, Weidberg, & Yoon, 2013; Moallem & Ray, 2012). With regard to discounting, these studies report equivocal results with respect to increased discounting among polysubstance users. Among dual substance users, Moallem and Ray (2012) found increased discounting in heavy drinkers and smokers compared to mono use of either substance. However, others fail to find evidence of an additive effect of dual use on discounting. Specifically, Businelle, McVay et al. (2010) did not find evidence of increased discouting in combined cigarette smokers with and without a comorbid substance use disorder compared to either smoking alone or substane dependence alone. So too, García-Rodríguez et al. (2013) did not find an increase in discounting in combined smoking and cocaine-dependent individuals compared to cocaine dependence alone.
Importantly, across these studies the substance use profiles of participants were heterogeneous. Specifically, Moallem and Ray (2012) found additive discounting effects of smoking and alcohol use whereas García-Rodríguez et al. (2013) and Businelle et al. (2010) did not find an increase in discounting effects in combined smoking and cocaine dependence or combined smoking and substance dependence, respectively. Moreover, Businelle's design allowed for all substance dependencies other than nicotine dependence for inclusion in a “substance use disorder’ group. Classifying the different substance dependencies into a single group precludes the ability to statistically compare specific substance use profiles. To the best of our knowledge, no study of delay discounting has examined tri-substance using alcohol, cocaine, and nicotine users. Here, we systematically compare the eight possible substance groups (all combinations of use and non-use among alcohol, smoking, and cocaine). We refer to these eight groups as substance profile groups henceforth, and further distinguish these profiles as non-, mono-, dual-, and tri-substance use to determine their association with delay discounting.
Methods
Participants
Participants (N = 599) were individuals (mean age = 41.07 years, 68% males) who participated in any of 13 separate study protocols conducted by our research group over the course of 5 years (See Table 1). One individual reported 32 years of education and another reported a monthly income of 10,000 dollars. These values were outliers with respect to other data in this study and were excluded.
Table 1.
Subject data from thirteen protocols were included in the present study. Protocols varied in terms of dependencies necessary for inclusion, exclusionary dependencies, and whether or not subjects were treatment seeking and the version of the delay discounting task administered.
| Protocol | Primary substance use | N | Other dependences possible? | Treatment seeking | Discounting version |
|---|---|---|---|---|---|
| 1 | None (Control) | 61 | No | N/A | 1 |
| 2 | Nicotine | 24 | No | No | 2 |
| 3 | Nicotine | 20 | No | No | 1 |
| 4 | Nicotine | 13 | No | No | 1 |
| 5 | Cocaine | 71 | Yes (nicotine and marijuana only) | No | 3 |
| 6 | Nicotine | 27 | N | No | 2 |
| 7 | Nicotine | 9 | N | No | 1 |
| 8 | Alcohol | 56 | Yes (nicotine only) | No | 1 |
| 9 | Nicotine | 15 | No | No | 2 |
| 10 | None (Control) | 15 | No | N/A | 5 |
| 11 | Nicotine | 7 | No | No | 4 |
| 12 | Alcohol and/or cocaine | 272 | Yes (any substances) | Yes | 1 |
| 13 | Nicotine | 9 | No | No | 4 |
Discounting Task 1: Delays of 1 day, 1 week, 1 month, 6 months, 1 year, 5 years, 25 years with blocked delays presented in chronological order
Discounting Task 2: Delays of 1 day, 1 week, 1 month, 6 months, 1 year, and 5 years with blocked delays presented in a random order
Discounting Task 3: Delays of 1 day, 1 week, 1 month, 3 months, 6 months, and 1 year with blocked delays presented in a random order
Discounting Task 4: Delays of 1 day, 1 week, 1 month, 6 months, 1 year, 5 years, and 25 years with blocked delays presented in a random order
Discounting Task 5: Variable delays determined by k value calculated from brief 5-item discounting task; blocked delays are then presented in a random order
The eight substance profile groups included individuals with no substance use (n = 122), mono-substance use, dual-substance use, and tri-substance use. The mono-substance use groups include heavy smokers as defined as smoking more than 10 cigarettes a day over the past 30 days (n = 137), alcohol-dependent only (n = 47), and cocaine-dependent only (n = 28). The dual-substance use profiles include co-occurring heavy smoking and alcohol dependence (n = 79), co-occurring heavy smoking and cocaine dependence (n =47), and co-occurring alcohol and cocaine dependence (n = 49). Finally, the tri-substance use profile consisted of individuals with co-occurring heavy smoking, and alcohol and cocaine dependence (n = 90). Table 1 reports characteristics of the 13 studies from which data records were used.
Participants for these studies were recruited from the greater New River Valley and Roanoke Valley area in Virginia as well as the metropolitan and outlaying areas of Little Rock, Arkansas. All participants provided written consent that was approved by either the IRB at University of Arkansas or Virginia Tech. Participants were recruited using flyers posted around the community and in local substance abuse treatment programs, through radio and newspaper advertisements and by word of mouth. All participants completed a brief telephone or in-person screen to assess initial eligibility criteria. Participants provided information regarding past and recent drug and alcohol use, as well as demographic information, employment status and income, current health and medical history, and cigarette smoking habits. Individuals that reported alcohol or drug use over the past year were assessed for primary and, if applicable, secondary dependencies. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994) criteria for substance and/or alcohol dependence was assessed by trained research associates using the alcohol and substance dependence modules of the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). Individuals reporting multiple substance dependencies, for example both alcohol and cocaine dependence, were classified as polysubstance dependent. Participants that met current diagnostic criteria for substance dependence other than cocaine (either powder or crack), alcohol, and/or nicotine were excluded from the analyses. Participants were excluded from participation if they reported current unstable or significant medical or psychiatric conditions (e.g., seizure disorders, major depressive disorder, post-traumatic stress disorder). Completion of a delay discounting task was a requirement for inclusion in this study.
For all studies, the consent appointment was scheduled to occur within two weeks of the initial screening interview. On the day of enrollment into the study, eligibility criteria were reviewed and all participants provided written informed consent after being informed of study risks and benefits. Participants were compensated for consenting into the study and for task completion.
Materials and procedures
Five computer-based delay discounting tasks were used to assess preference for sooner smaller or later larger outcomes across participants. Participants were presented with hypothetical scenarios in which the extent of discounting of a delayed reward (e.g., delayed money) relative to an immediate reward was determined where magnitudes of future rewards were set at $1000. Measures of indifference points between immediate and delayed (e.g., 1 day, 1 month, 6 months, 1 year, 25 years) rewards were obtained and discount rates were computed according to Equation 1 (See below). As delay discounting data were collected over several years and from participants that would eventually be enrolled in a variety of protocols to get a large and comprehensive sample, there was variation in the delay-discounting task used. Table 1 specifies unique characteristics of the delay discounting task used. Variability in discounting attributable to different versions of the delay discounting task was accommodated by allowing the task completed to be a candidate variable in our model selection exercise (see below) and also by comparing variances in discounting ln(k) across the five tasks using Levene's test (Levene, 1960). Prior to beginning the task, participants were instructed to consider each question independently and to answer carefully and thoughtfully as if the choices were real.
Statistical methods
Demographic information was collected including age, gender, income, education, marital status, employment status, and race.
Common variables in all protocols included delay discounting k (see below for description), heavy cigarette smoking status, alcohol dependence, and cocaine dependence. Additional substance use besides cigarette smoking, alcohol, and cocaine use were measured in the study and included amphetamine, benzodiazepine, hallucinogen, opiate, marijuana, and other (e.g., sleeping pills). Frequencies of additional substance use are summarized in Table A1 in the appendix. Additional substance use was combined into a single category because the sample sizes among other substance groups were low in many cases. This additional substance variable was included as a candidate covariate in the variable selection exercise described below.
All delay discounting tasks consisted of a computerized titration questionnaire were participants were asked to choose between hypothetical smaller immediate rewards and a larger delayed reward of $1,000 for a variety of delays where the immediate reward titrates until an indifference point where the subjective value of the immediate rewards is equal to the value of the delayed reward. Discounting task 5 is similar to tasks 1-4 except that the delay for the larger reward is titrated instead of the immediate amount and only a single indifference point is obtained (See Koffarnus & Bickel, 2014 for procedural details). See Table 1 for descriptions of discounting tasks administered in each study.
The indifference points were then fit to the following equation:
| Equation 1 |
where V is the subjective value of the objective monetary amount A, to be delivered after some delay, D (Mazur, 1987). The k values from fitting Equation 1 to indifference points served as a one number summary of discounting for each participant. The parameter k describes the rate of decay in the hyperbolic function and is used as an index of the extent to which participants discount the value of future rewards. Higher k values indicate a tendency to devalue future rewards at a higher rate and this, in turn, suggests greater impulsivity. The k values were natural log transformed (hence denoted ln(k)) to better approximate the assumption of normality underling parametric statistical analysis. While there are other equations used to approximate the rate of discounting (McKerchar et al., 2009; Yi, Landes, & Bickel, 2009), Equation 1 is the most commonly used equation to model discounting behavior in addicted populations. For example, in a recent meta-analysis comparing control groups to addictive behavior groups, Equation 1 was used in 70% of studies reviewed (MacKillop et al., 2011).
To assess each study variable's association with ln(k) individually, a linear model was used to individually model discounting as a function of each study variable. Significance tests based on F statistics and effect sizes in the form of R2 values were used to summarize each relationship (See Table 2). R2 values of 0.01, 0.06, and 0.40 were small, medium, and large respectively (Cohen, 1992).
Table 2.
Bivariate relationship between study variables and delay discounting rate, including R2 and significance.
| Variable | N | R2 | F value | df Numerator | df Denominator | p-value |
|---|---|---|---|---|---|---|
| Protocol | 599 | 0.121 | 6.76 | 12 | 586 | <.0001 |
| Discounting version | 599 | 0.041 | 6.35 | 4 | 594 | <.0001 |
| Age | 599 | 0.008 | 4.99 | 1 | 597 | 0.026 |
| Education | 595 | 0.061 | 38.86 | 1 | 593 | <.0001 |
| Employment status | 593 | 0.057 | 11.88 | 3 | 589 | <.0001 |
| Gender | 599 | 0.017 | 10.65 | 1 | 597 | 0.0012 |
| Income | 594 | 0.021 | 13.00 | 1 | 592 | 0.0003 |
| Marital status | 582 | 0.011 | 1.64 | 4 | 577 | 0.1629 |
| Race | 598 | 0.008 | 2.49 | 2 | 595 | 0.0841 |
| Treatment seeking | 599 | 0.007 | 4.51 | 1 | 597 | 0.0341 |
| Alcohol dependence | 599 | 0.005 | 3.02 | 1 | 597 | 0.0827 |
| Cocaine dependence | 599 | 0.048 | 30.02 | 1 | 597 | <.0001 |
| Heavy smoking | 599 | 0.039 | 24.33 | 1 | 597 | <.0001 |
Discounting within each of the substance profiles was assessed in two ways. First, unadjusted group means and standard errors were computed for all eight substance profiles. These values summarize discounting by group without accounting for other participant characteristic and demographic measures. Second, a variable selection routine was used to identify the most relevant covariates and these were used to model discounting alongside the substance profiles. Details of the model selection approach follow.
To address the possibility that other study variables might affect the association between discounting and the primary dependencies, an exhaustive model selection routine was implemented to determine which covariates should be modeled alongside the primary substance use variables. The purpose of this exercise is to determine which subject characteristics are associated with discounting, statistically control for those, and then compare substance profiles in terms of discounting after accounting for other characteristics. Covariates were included in the model selection exercise that might lead to intra-protocol (e.g., additional substance use), inter-protocol (e.g., delay discounting version), or both within and between protocol (e.g., age) variation. The following candidate predictors were considered: age, education, gender, income, marital status, additional substance, protocol, treatment seeking status, employment status, race, and delay discounting task version. Since approximately 96% of participants provided complete data for all measures, model selection was performed on the subset of individuals who had no missing data in any of these dimensions (n = 572). The Bayesian Information criterion (BIC; Schwarz, 1978) was used as a metric to decide which of the available predictors best describe discounting. Briefly, BIC weighs the likelihood of a candidate model for a given set of data and includes a penalty term for complexity, so that a model with fewer parameters would be chosen over a more complex model if the predictive ability of both models was similar. The bestglm package in R (McLeod & Xu, 2010) was used to assess each of the 211-1=2,047 candidate models which arise from the 11 predictors under consideration. The model with the lowest BIC based on covariates was then extended to include the substance use profiles.
Model-adjusted least squares means and standard errors alongside the raw data and unadjusted group means and standard errors, and model-based significance tests and effect sizes were computed. Note that significance tests to compare substance profiles do not account for the uncertainty associated with the model selection exercise used to choose covariates.
Results
The participants (n = 599) had the following characteristics (mean ± sd): age (years): 41.07 ± 11.83, education (years): 12.9 ± 1.94, discounting (lnk): −4.65 ± 2.73. The frequencies (percentages) of employment status are as follows: full-time: 78 (13.15), part-time: 104 (17.54), unemployed: 407 (68.63), retired: 4 (0.67). The frequencies (percentages) of marital status are as follows: single/never married: 267 (45.19), married: 72 (12.37), divorced: 186 (31.96), separated: 51 (8.76), widowed: 10 (1.72). The frequencies of race are as follows: white: 364 (60.87), African-American: 218 (36.45), other: 16 (2.68). The sample included 407 males (67.95). The sample included 272 (45.41) treatment-seeking individuals and 111 (18.53) participants also used other substances (see Table A1 for frequencies of other substances). Income was highly skewed (skew = 6.59) with median monthly income of $400 and interquartile range $115-$1000. Table 1 compares features of the protocols used in this study. Levene's test found no significant evidence that variances in discounting differed among the five discounting task versions (p = 0.351). This suggests that while discounting ln(k) may differ between tasks on average, there is no clear difference in variability among the tasks. This finding justifies the statistical approach to account for differences in discounting ln(k) as proposed. Table 2 describes the bivariate relationship between the natural log of k (ln(k)) and individual variables. The largest effect sizes are associated with protocol (R2 =12.1%), delay discounting version (R2 =4.1%), cocaine dependence (R2=4.8%), heavy smoking (R2=3.9%), employment status (R2=5.7%), and education (R2=6.1%). Education is negatively associated with discounting, and the variability in discounting among protocols is depicted in Table 1.
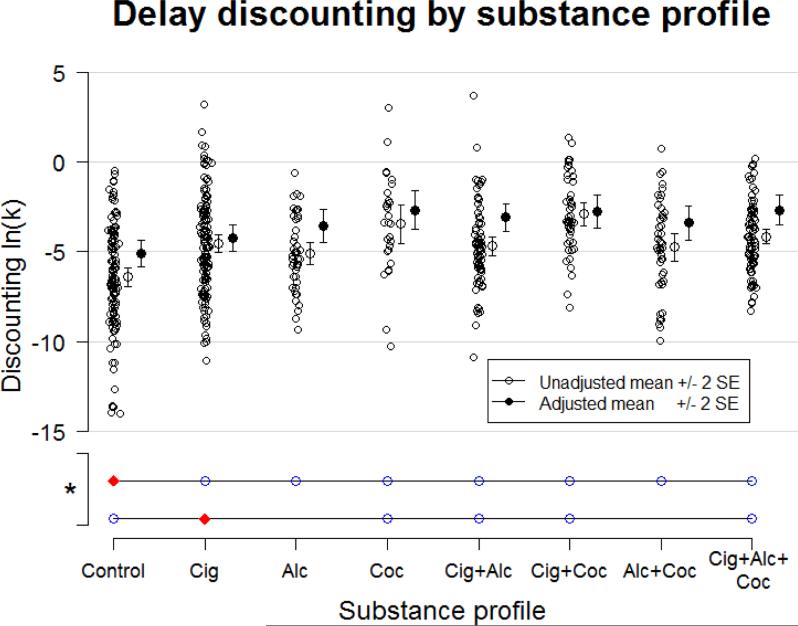
Figure 1 plots the raw data for each of the substance profiles. Group means plus/minus two standard errors are plotted with open circles, and model adjusted means plus/minus two adjusted standard errors are plotted in closed circles. This graphic illustrates an approximate 95% confidence interval for the mean (see the Appendix for details).
Figure 1.
Substance use profiles and delay discounting. Red (filled in) diamond indicates profile from which all open blue circles are significantly different.
The adjusted means and standard errors were generated by modeling substance profile status with years of education, treatment seeking status, and version of delay discounting task as covariates (See Table 3) using the N = 595 records that included full data for this particular model. These covariates were selected because they provided the single lowest BIC among all possible models when predicting discounting ln(k). The top 10 most competitive models according to this selection approach are summarized in the Appendix (See Table A2). In some cases, variables were significantly associated with delay discounting (See Table 2) although they were not selected in the best fit models. This indicates that variance that are associated with discounting ln(k) alone but are excluded from the model (e.g. list a few) do not provide unique, additional predictive value for ln(k) beyond the variables that were included in the model for the observed data (See McLeod & Xu, 2010 for details on model selection criterion and penalties). The extent to which the adjusted and unadjusted intervals differ reflects the impact of the model covariates.
Table 3.
Overall GLM model of delay discounting with selected covariates (i.e., education, income, gender, treatment seeking status, and delay discounting version) and substance use profiles.
| Variable | df | F-value | p-value |
|---|---|---|---|
| Cigarette smoking | 1 | 4.03 | 0.0451 |
| Alcohol dependence | 1 | 2.3 | 0.1297 |
| Cocaine dependence | 1 | 13.04 | 0.0003 |
| Cigarette smoking and alcohol dependence | 1 | 0.18 | 0.6722 |
| Cigarette smoking and cocaine dependence | 1 | 0.56 | 0.4555 |
| Alcohol and cocaine dependence | 1 | 10.3 | 0.0014 |
| Cigarette smoking, alcohol and cocaine dependence | 1 | 1.46 | 0.2278 |
| Years of education | 1 | 27.31 | <.0001 |
| Treatment seeking status | 1 | 0.46 | 0.4974 |
| Delay discounting version | 4 | 6.81 | <.0001 |
For example, in the control group, the model-adjusted results suggest show higher discounting that the unadjusted results. Note that the mean education level in the control group is 13.7 years (compared to 12.9 years study-wide). Also, education is negatively associated with ln(k) overall (r = −0.25, n = 595, p < 0.01). Hence, part of the reason for low discounting in the control group is due to the fact that the control participants are also more highly educated. The adjusted mean and standard error takes education into account, indicating that discounting in the control group is higher than the unadjusted mean suggests, because the unadjusted mean conflates the effects of being a control participant, education, and other unmodeled effects. This model accounted for the impact of both the specific delay discounting procedure and treatment seeking status. Note that delay discounting task versions differed on average in discounting ln(k), but there is no statistical evidence of differing variances in ln(k) among these tasks as shown by the result of Levene's test. Hence, inclusion of discounting task as a candidate predictor does not violate any of the modeling assumptions made in this study. The model R2 = 0.11 is for the group means model (corresponding to the open circle intervals in Figure 1). The model R2 = 0.18 is for the model which included the model selection covariates (corresponding to the closed circle intervals in Figure 1). Table 3 summarizes the effects of the full model. Education, treatment seeking status, and delay discounting version were covariates, cigarette smoking, cocaine dependence, and combined cocaine dependence and heavy smoking interaction are significant at the p = 0.05 level (See Table 3).
The above model allows all substance use group combinations to vary freely with regard to discounting while also including variance attributed to important covariates (i.e., education, income, treatment seeking status, and delay discounting version) as chosen by BIC selection. Simple comparisons of the community controls and substance use groups revealed several significant comparisons. Heavy smokers (p = 0.04), alcohol-dependent (p < 0.01), cocaine-dependent (p < 0.01), heavy smokers and alcohol dependent (p < 0.01), cocaine and alcohol-dependent (p < .01), heavy smokers and cocaine-dependent (p < 0.01), and heavy smokers combined with alcohol and cocaine dependence (p < 0.01) discounted future rewards more than community controls. Furthermore, cocaine-dependent (p = 0.02), heavy smokers with alcohol dependence (p = 0.03), heavy smokers with cocaine dependence (p = 0.01), and heavy smokers with both alcohol and cocaine dependence (p < 0.01) discount future rewards more than individuals that were only heavy smokers.
Discussion
In the current study, the delay discounting for future monetary rewards were examined among heavy smokers, alcohol-dependent and cocaine-dependent individuals. All substance use profiles were found to discount significantly more than community control participants. Additionally, dual-substance users that were either cocaine- or alcohol-dependent in addition to cigarette smoking discount significantly more than cigarette smokers alone (p = 0.01 and p = 0.03, respectively). We found that tri-substance users (i.e., alcohol- and cocaine-dependent in addition to smoking cigarettes) discounted significantly more than mono-substance users that used cigarettes (p < 0.01), however not significantly more than mono-substance using alcohol-dependent users (p = 0.06), cocaine-dependent users (p = 0.97) or any of the dual-substance use profiles including cigarette and alcohol use, cigarette and cocaine use, and alcohol and cocaine use (p = 0.30, 0.88, 0.11, respectively). In the section to follow we would like to discuss six points about these findings.
First, discounting in the control group was significantly less than all of the substance using groups, broadly replicating a vast body of discounting literature reporting that substance using populations discount more than controls (for meta-analysis see MacKillop et al., 2011).
Second, the results associated with dual substance use resulted in two different findings. On one hand, when heavy smoking was present, dual-substance use was associated with greater discounting than cigarette smoking alone. This observation indicates an additive effect of dual-substance use with regard to cigarette smoking populations, consistent with the findings of García-Rodríguez et al. (2013) and Moallem and Ray (2012). On the other hand, dual-substance use of alcohol and cocaine was not associated with significantly different rates of discounting than the mono use of any substance. Whether this observation is a reliable one will await additional replication.
Third, tri-substance use was associated with significantly more delay discounting than mono-substance heavy smokers, however, tri-substance users did not discount significantly more than alcohol alone, cocaine alone, or any of the dual-substance using groups. These data suggest the relevance of both competing hypotheses; that is, the observation of tri- and dual-substance users discounting comparably supports the ceiling hypothesis on discounting, while comparing mono and dual dependencies support the additive hypothesis.
Fourth, in line with previous reports (i.e., Businelle et al., 2010; García-Rodríguez et al., 2013; Moallem & Ray, 2012), years of education explains a relatively large portion of variance in discounting (6.1%) and, not surprisingly, is systematically related to types of substance use profiles. Furthermore, we found that the delay discounting task version contributed to discounting rates by accounting for 4.1% of variance observed. The different delays and task duration may be one possible explanation for the variance across different discounting procedures (for comparison of discounting tasks see Table 1).
Fifth, the findings presented here assimilate and add to the existing understanding of how combined substance use relates to valuation of future rewards. To date, three previous studies have examined the relationship between delay discounting and dual substance use and report varying results. Overall, our results largely replicate the findings of García-Rodríguez et al. (2013) and Moallem and Ray (2012). However, our findings are in contrast to Businelle et al. (2010)'s observations that individuals meeting DSM-IV criteria for any substance use disorder in addition to smoking cigarettes did not discount more than cigarette smokers alone. Businelle et al. (2010) combined all substance use disorders without comparing the impact of unique substances, therefore, the heterogeneity of this group may wash out differences in discounting that would be evident when examining more homogenous groups.
Sixth, possible limitations of our analyses are three fold. One limitation is that we did not obtain a measure of addiction severity. Therefore, we may have included individuals differing in terms of severity of physiological or psychological substance dependence. In future studies utilizing a severity measure may further illuminate the impact of polysubstance use. Another limitation of this study is the variability in the delay-discounting task administered. Participants in this study completed different task versions of a computerized delay discounting task. In future studies, consistency in the task administered may lead to a less variance in the data. Lastly, another source of variance may be heterogeneity in nicotine dependence in our sample. We did not obtain a measure of nicotine dependence, rather cigarette smokers were required to smoke 10 or more cigarettes a day to participate. Thus, we may have included both dependent and non-dependent cigarette smokers.
In conclusion, our findings contribute to the extant literature by providing greater understanding of the association between dual- and tri-substance dependence and delay discounting. Specifically, the significantly higher discount rates of dual-substance and tri-substance cigarette smokers than mono-substance cigarette smokers indicates that treatment seeking alcohol- and cocaine- dependent individuals that also smoke may be quantitatively different than individuals who only smoke cigarettes. Furthermore, a limit on the rate of discounting was observed in tri-substance users whereby a ceiling effect was detected when greater than two substance are being used. In sum, an awareness of the impact of multi-substance use is of research and potential clinical import in the study and treatment of substance use.
Acknowledgments
This research was supported by NIDA grants R01DA024080 and R01DA034755, and supplement R01DA034755-01A1S1.
Dr. Bickel is a principal with HealthSim, LLC, a software development company.
Appendix
Mean plus/minus two standard errors and confidence intervals
Recall that the standard formula for a 95% confidence interval for a mean based on the normal approximation as n → ∞ is
The term under the radical above is the standard error of the sample mean. Hence, by adding and subtracting two standard errors (rather than 1.96), Figure 1 displays an interval, which is visually similar to a 95% confidence interval for the mean given large sample size. The smallest group in this study is the cocaine only group with a sample size of 28. In this small group, 1.96 would be replaced with 2.05 (the 97.5% percentile of a t27 distribution). It seems almost certain that the small differences in these percentiles would not be visually decipherable to the naked eye, so mean plus/minus two standard errors was plotted in all cases for simplicity.
Table A1.
Summary of other substance use reported by participants. Of the sample, 111 participants reported using at least one other substance.
| Other Substances Used | Frequency |
|---|---|
| Opioids | 51 |
| Marijuana | 49 |
| Benzodiazepines | 18 |
| Amphetamines | 25 |
| Hallucinogens | 4 |
| Other (unspecified) | 1 |
Table A2.
Top 10 models for covariates based on BIC. Models with a low BIC exhibit the best statistical tradeoff between predictive ability and model complexity. The optimal model by this criterion includes years of education and protocol.
| Model | Age | Education | Gender | Income | Marital status | Other substances uses | Protocols number | Treatment seeking status | Employments status | Race | Delay discounting version | BIC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | No | Yes | No | No | No | No | No | Yes | No | No | Yes | 1088.32 |
| 2 | No | Yes | Yes | No | No | No | No | Yes | No | No | Yes | 1090.11 |
| 3 | Yes | Yes | No | No | No | No | No | Yes | No | No | Yes | 1090.74 |
| 4 | No | Yes | No | Yes | No | No | No | Yes | No | No | Yes | 1091.51 |
| 5 | No | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes | 1092.93 |
| 6 | No | Yes | No | No | No | No | No | Yes | Yes | No | Yes | 1093.14 |
| 7 | Yes | Yes | No | Yes | No | No | No | Yes | No | No | Yes | 1093.42 |
| 8 | Yes | Yes | Yes | No | No | No | No | Yes | No | No | Yes | 1093.71 |
| 9 | No | Yes | No | No | No | Yes | No | Yes | No | No | Yes | 1094.09 |
| 10 | Yes | Yes | No | Yes | No | No | No | No | No | No | Yes | 1094.55 |
Footnotes
Disclosures
All authors contributed to this manuscript and have read and approved the final manuscript.
References
- Association, A. P. Diagnostic and statistical manual of mental disorders (DSM) American psychiatric association; Washington, DC: 1994. pp. 143–147. [Google Scholar]
- Batel P, Pessione F, Maitre C, Rueff B. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;90(7):977–980. doi: 10.1046/j.1360-0443.1995.90797711.x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Koffarnus MN, Moody L, Wilson AG. The behavioral-and neuro-economic process of temporal discounting: a candidate behavioral marker of addiction. Neuropharmacology. 2014;76:518–527. doi: 10.1016/j.neuropharm.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Odum AL, Madden GJ. Impulsivity and cigarette smoking: delay discounting in current, never, and ex-smokers. Psychopharmacology. 1999;146(4):447–454. doi: 10.1007/pl00005490. [DOI] [PubMed] [Google Scholar]
- Businelle MS, McVay MA, Kendzor D, Copeland A. A comparison of delay discounting among smokers, substance abusers, and non-dependent controls. Drug and alcohol dependence. 2010;112(3):247–250. doi: 10.1016/j.drugalcdep.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Gudleski GD, Saladin ME, Brady KT. Impulsivity and rapid discounting of delayed hypothetical rewards in cocaine-dependent individuals. Experimental and clinical psychopharmacology. 2003;11(1):18. doi: 10.1037//1064-1297.11.1.18. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological bulletin. 1992;112(1):155. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- García-Rodríguez O, Secades-Villa R, Weidberg S, Yoon JH. A systematic assessment of delay discounting in relation to cocaine and nicotine dependence. Behavioural processes. 2013 doi: 10.1016/j.beproc.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Olkin I. Statistical method for meta-analysis. Academic press; 2014. [Google Scholar]
- Heil SH, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addictive Behaviors. 2006;31(7):1290–1294. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Hoffman WF, Moore M, Templin R, McFarland B, Hitzemann RJ, Mitchell SH. Neuropsychological function and delay discounting in methamphetamine-dependent individuals. Psychopharmacology. 2006;188(2):162–170. doi: 10.1007/s00213-006-0494-0. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, Baker F, Moore BA, Badger GJ, Budney AJ. Delay discounting in current and former marijuana-dependent individuals. Experimental and clinical psychopharmacology. 2010;18(1):99. doi: 10.1037/a0018333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalman D, Morissette SB, George TP. Co - Morbidity of Smoking in Patients with Psychiatric and Substance Use Disorders. The American Journal on Addictions. 2005;14(2):106–123. doi: 10.1080/10550490590924728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128(1):78. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Koffarnus MN, Bickel WK. A 5-trial adjusting delay discounting task: Accurate discount rates in less than one minute. Experimental and clinical psychopharmacology. 2014;22(3):222. doi: 10.1037/a0035973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levene H. Robust tests for equality of variances1. Contributions to probability and statistics: Essays in honor of Harold Hotelling. 1960;2:278–292. [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafò MR. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology. 2011;216(3):305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Petry NM, Badger GJ, Bickel WK. Impulsive and self- control choices in opioid-dependent patients and non-drug-using control patients: Drug and monetary rewards. Experimental and clinical psychopharmacology. 1997;5(3):256. doi: 10.1037//1064-1297.5.3.256. [DOI] [PubMed] [Google Scholar]
- Mazur JE, editor. An adjusting procedure for studying delayed reinforcement. Vol. 5. Erlbaum; Hillsdale, N.J.: 1987. [Google Scholar]
- McKerchar TL, Green L, Myerson J, Pickford TS, Hill JC, Stout SC. A comparison of four models of delay discounting in humans. Behavioural processes. 2009;81(2):256–259. doi: 10.1016/j.beproc.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod A, Xu C. bestglm: Best subset GLM. 2010 URL http://CRAN. R-project.org/package= bestglm.
- Moallem NR, Ray LA. Dimensions of impulsivity among heavy drinkers, smokers, and heavy drinking smokers: singular and combined effects. Addictive Behaviors. 2012;37(7):871–874. doi: 10.1016/j.addbeh.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology. 2001;154(3):243–250. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. The annals of statistics. 1978;6(2):461–464. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Yi R, Landes RD, Bickel WK. Novel models of intertemporal valuation: past and future outcomes. Journal of neuroscience, psychology, and economics. 2009;2(2):102. doi: 10.1037/a0017571. [DOI] [PMC free article] [PubMed] [Google Scholar]