Abstract
The aim of this study was to determine the risk factors associated with left ventricular (LV) hypertrophy (LVH) among 89 untreated children with primary hypertension. Clinic hypertension was confirmed by 24‐hour ambulatory blood pressure (BP) monitoring. LV mass (LVM) index was calculated as LVM (g)/height (m)2.7 and LVH was defined as LVM index >95th percentile. Children with (n=32) and without (n=57) LVH were compared. Both obesity and systolic BP were independently associated with LVH, with a higher contribution by body mass index. Obesity contributed significantly, with a nearly nine‐fold increased risk of LVH. There was evidence of effect modification by the presence or absence of obesity on the relationship between systolic BP and LVH, whereby the relationship existed mainly in nonobese rather than obese children. Hence, to achieve reversal of LVH, clinicians should take into account both BP control and weight management.
Primary hypertension or essential hypertension (EH) can lead to cardiovascular changes in childhood, including subclinical hypertensive cardiomyopathy,1, 2, 3 aortopathy4 and vasculopathy.5, 6 Left ventricular (LV) hypertrophy (LVH), as demonstrated by an increase in LV mass (LVM) on echocardiography, is the most common surrogate marker of end‐organ damage from EH7, 8, 9 on echocardiography. Blood pressure (BP) levels alone cannot predict LVH and, hence, echocardiography is recommended in all children with hypertension.10 Presence of LVH in adults with EH has been associated with impaired LV systolic11 and diastolic function12 and thus overall worse cardiovascular morbidity and mortality.13, 14, 15, 16, 17, 18, 19, 20 Therefore, early detection and treatment of LVH in childhood is crucial to prevent cardiovascular events in adult life. Moreover, investigating end‐organ damage in childhood can give further information on the origins of subclinical hypertensive cardiomyopathy in humans.
Multiple risk factors, both genetic and environmental, have been associated with the LVH phenotype in adults and children with EH. The LVH phenotype in children has been associated with family history of EH,21 with multiple markers of the child's BP such as diagnosis of hypertension,2 systolic BP,22, 23 diastolic BP,22, 24 ambulatory BP,25, 26, 27 nocturnal systolic BP,28, 29 and daytime systolic variability,29 as well as with metabolic markers such as body mass index,22, 23, 24, 26, 30 obesity,27, 31, 32 body fatness,27 lean tissue mass,27 insulin resistance,31 C‐reactive protein,23 and microalbuminuria.23
BP levels have been shown to explain only about 40% of the variability in LVM among adults with untreated EH.33 Controlling BP has been shown to decrease LVH in both adults and children with hypertension34 but weight loss can also decrease LVH in those who do not have hypertension.35 Among children with EH, it is unknown which has the greater influence on LVH––BP or weight. The aim of this study was to examine the contributory factors associated with LVH phenotype in childhood‐onset EH and determine individual contributions by weight and BP on LVH.
Methods
Institutional Approval
The study was approved by the Institutional Committee for the Protection of Human Subjects at the University of Texas Health Science Center and Children's Memorial Hermann Hospital, Texas Medical Center. All participants and parents gave informed assent and consent, respectively, for this study.
Patient Population
This was a single‐center, case‐control study of children who were diagnosed with elevated BP prior to antihypertensive therapy. We prospectively enrolled children aged 9 to 18 years from our tertiary pediatric hypertension clinic whereby they were referred or recruited as follows: (1) Referral Study Population: These patients were referred to the clinic after detection of elevated BP from either an ambulatory setting by a primary care provider or an inpatient setting. (2) Recruited Study Population: Patients recruited by screening comprised a small proportion of patients in our clinic and were identified by systematic school‐based screening for hypertension in students aged 11 to 18 years in Houston area public schools.36 Patients recruited by these two methods, ie, school screening or referral as described above, have been reported to be similar in a prior publication;36 this was confirmed in our current data set during this analysis. All enrolled children underwent further evaluation including ambulatory BP monitoring (ABPM) as described further below. Demographic and anthropometric data were collected on all participants at study entry. Obesity was defined as body mass index (BMI) at or above 95th percentile for age and sex.
BP Protocol
Children with untreated newly diagnosed EH without any identifiable etiology for the hypertension were enrolled in the study. BP was reported as the participant's BP factored by their age‐, sex‐, and height‐specific 95th percentile (BP index). Hypertension status was evaluated by both clinic and ambulatory BP monitoring for 24 hours in all children as follows: clinic hypertensive status was diagnosed when three separate measurements of systolic and/or diastolic BP >95th percentile for height, age, and sex per the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (Fourth Report)37 were recorded and elevated BP by Critikon oscillometric monitor (Tampa, FL) was determined at the first visit to the hypertension clinic. The hypertension in clinic was confirmed by manual auscultation with a mercury sphygmomanometer by trained personnel using methods recommended by the Fourth Report.37 Clinic BP measurements considered the average of the last three of four BP measurements performed by oscillometric monitor after 5 minutes of rest. Prehypertension, stage I hypertension, and stage II hypertension were classified per the Fourth Report.37 Children who were older than 5 years underwent ABPM using Spacelabs oscillometric monitors (Spacelabs, Inc, Redmond, WA). The children along with their families were instructed on avoidance of caffeinated beverages or supplements, any medications, herbal or over‐the‐counter products, smoking, and alcohol for 24 hours prior to and during the ABPM. While undergoing ABPM, BP was measured every 20 minutes for 24 hours. Children with casual hypertension but with 24‐hour systolic BP and diastolic BP less than the pediatric 95th percentile and BP load <25% were considered to have white‐coat hypertension. Children with mean 24‐hour systolic BP or diastolic BP greater than the pediatric 95th percentile or BP load (percentage of BP values exceeding the 95th percentile for the 24‐hour period) >25% were considered to have ambulatory hypertension.38
Diagnosis of EH
Once hypertension was confirmed, the diagnosis of primary hypertension or EH was made by extensive evaluation per recommendations by the Fourth Report,37 including a urinary evaluation, blood tests, renal ultrasound, and echocardiography. Children with congenital cardiac disease including bicuspid aortic valve were excluded from this study. Criteria for the diagnosis of EH were: (1) clinic BP elevation above the 95th percentile on three previous occasions, (2) absence of secondary causes of hypertension, and (3) no concurrent medication with the potential to raise BP (eg, steroids, central stimulants).
Echocardiography and Vascular Ultrasound Protocol
All children underwent transthoracic echocardiography and vascular ultrasound and the measurements were made in a manner‐blinded fashion. The reproducibility of measurements for both were determined by repeat assessments for 10 values by the same sonographer and by two sonographers independently, yielding kappa values >0.8. The echocardiographic studies were performed for all participants using an Acuson Sequoia 512 ultrasound machine (Siemens, Malvern, PA) by trained pediatric sonographers using a standard protocol to evaluate congenital cardiac disease39 and LVH.40, 41 Quantification of LVM was made from two‐dimensionally guided M‐mode measurements during diastole of the LV internal dimension, interventricular septal thickness, and posterior wall thickness according to methods established by the American Society of Echocardiography.40, 41 LVM was calculated using the equation reported by Devereux and colleagues42 LVM index (LVMI2.7) was calculated by dividing LVM by height in meters to the 2.7th power to minimize the effect of age, sex, ethnicity, and overweight status.43, 44 For this study, LVH was defined as an LVMI 38.6 g/m2.7, a value reported to represent the pediatric 95th percentile of LVMI2.7 in normotensive healthy children.43, 44, 45 Because the quantiles of LVMI2.7 vary only a little after the age of 9 years, we did not use these in our cohort of children since they were 9 years and older.46 Eccentric and concentric hypertrophy was defined similarly to that previously reported in the literature.9 The measurements of diastolic function (peak E and A velocities, E/A ratio, isovolumic relaxation time, and deceleration times) were made by simultaneous transmitral and transaortic spectral Doppler flow velocities.41 Carotid artery duplex ultrasound was performed by protocol to measure carotid intima‐media thickness (CIMT) by experienced vascular sonographers in a standard manner.47 The thickest IMT complex of the far wall of the distal common carotid artery was measured in the longitudinal B‐mode section using a high‐resolution 8 MHz transducer. The values of right and left CIMT were averaged for the purpose of this study.
Statistical Analysis
Patients with LVH and no LVH were compared. Data from the medical records was abstracted and tabulated. Mean (standard deviations [SDs]) and medians (interquartile ranges) for continuous variables were compared between groups using parametric (t tests, analysis of variance with post hoc Tukey) and nonparametric (Mann‐Whitney, Kruskal‐Wallis) tests, depending on the distribution of the variable. Chi‐square tests were used to compare categorical variables across groups. Multivariable logistic regression analyses were performed to assess odds of LVH relative to differences in demographic, anthropometric, BP, laboratory, and vascular ultrasound parameters. Backward stepwise selection was used to optimize the regression model and calculate the odds ratios (ORs) along with 95% confidence intervals (CIs). All analyses were performed with STATA version 11 (StataCorp, College Station, TX). Statistical significance was assumed at a type I error rate of .05.
Results
Children with EH (n=89, males 65%, mean age 13.5 years, SD 1.8 years) were enrolled in the study. Eight (9%) of the children were diagnosed with prehypertension, 23 (26%) with stage I hypertension, and 58 (65%) with stage II hypertension in the clinic. LVH was detected in 32 (36%) children, with eccentric LVH in 25 (78%) and concentric LVH in seven (22%) of these patients. Their demographic (Table 1), anthropometric (Table 1), BP (Table 2), laboratory (Table 3), vascular ultrasound (Table 3), and echocardiographic (Table 4) parameters are summarized.
Table 1.
Demographic and Laboratory Profiles of Children With Childhood‐Onset Essential Hypertension With and Without Left Ventricular Hypertrophy
| Left Ventricular Hypertrophy | P Value | ||
|---|---|---|---|
| No | Yes | ||
| Number | 57 | 32 | |
| Age, y | 13.5 (1.7) | 13.6 (2.0) | .796 |
| Male, No. (%) | 34 (60) | 24 (75) | .145 |
| Ethnicity, No. (%) | |||
| NHW | 23 (40) | 6 (19) | .175 |
| Black | 19 (33) | 12 (37) | |
| Hispanic | 14 (25) | 13 (41) | |
| Asian | 1 (2) | 1 (3) | |
| Weight, kg | 69.1 (20.2) | 85.1 (18.7) | .0004 |
| Height, m | 1.6 (0.1) | 1.7 (0.1) | .202 |
| BMI, kg/m2 | 25.6 (6.9) | 30.6 (6.5) | .001 |
| BMI z score | 1.2 (0.9) | 1.9 (0.6) | .0002 |
| Weight status, No. (%) | |||
| Normal | 23 (41) | 3 (9) | .002 |
| Overweight | 15 (26) | 7 (22) | |
| Obese | 19 (33) | 22 (69) | |
Abbreviations: BMI, body mass index; NHW, non‐Hispanic white. All values are expressed as mean (standard deviation) unless otherwise indicated.
Table 2.
BP Profile of Children With Childhood‐Onset Essential Hypertension With and Without LVH
| Systolic | Diastolic | |||||
|---|---|---|---|---|---|---|
| No LVH | LVH | P Value | No LVH | LVH | P Value | |
| Clinic BP, mm Hga | 134.3 (9.0) | 138.8 (13.8) | .064 | 75.7 (11.8) | 79.7 (8.6) | .091 |
| Clinic BP Index | 1.1 (0.1) | 1.1 (0.1) | .464 | 0.9 (0.1) | 1.0 (0.1) | .195 |
| Ambulatory BP, mm Hg | ||||||
| Total | 121.8 (7.4) | 124.6 (10.3) | .205 | 68.5 (6.4) | 68.4 (7.3) | .921 |
| Waking | 128 (7.3) | 130.9 (9.8) | .177 | 74.4 (7.3) | 73.5 (9.2) | .686 |
| Sleeping | 111.3 (8.3) | 113.3 (10.7) | .395 | 58.6 (6.1) | 59.2 (7.7) | .719 |
| Ambulatory BP index | ||||||
| Total | 1.0 (0.1) | 1.0 (0.1) | .528 | 0.9 (0.1) | 0.9 (0.1) | .758 |
| Waking | 1.0 (0.1) | 1.0 (0.1) | .426 | 0.9 (0.1) | 0.9 (0.1) | .638 |
| Sleeping | 1.0 (0.1) | 1.0 (0.1) | .804 | 0.9 (0.1) | 0.9 (0.1) | .771 |
| Ambulatory BP load, % | ||||||
| Total | 34.4 (24) | 43 (27.8) | .186 | 19 (17.4) | 20.6 (20.7) | .735 |
| Waking | 36.2 (24.5) | 43.9 (27.9) | .241 | 18.8 (17.3) | 20.8 (22.4) | .676 |
| Sleeping | 30.3 (27) | 32.8 (30.7) | .728 | 18.4 (20) | 20.9 (25.1) | .65 |
| Ambulatory BP dip, % | 10.1 (7) | 10 (7.9) | .986 | 16.3 (10.1) | 14.2 (12.7) | .399 |
| Ambulatory BP nondippers, No. (%) | 10 (23) | 6 (25) | .833 | 1 (2) | 3 (12.5) | .122 |
Abbreviation: LVH, left ventricular hypertrophy. All values are expressed as mean (standard deviation). aClinic blood pressure (BP) is the average of three measurements.
Table 3.
Vascular Ultrasound and Laboratory Profiles in Childhood‐Onset Essential Hypertension With and Without Left Ventricular Hypertrophy
| Left Ventricular Hypertrophy | P Value | ||
|---|---|---|---|
| No | Yes | ||
| Carotid intima‐media thickness, mm | 0.56 (0.08) | 0.64 (0.03) | .002 |
| Total cholesterol, mg/dL | 169.1 (32.2) | 173.2 (29.8) | .646 |
| High‐density lipoprotein, mg/dL | 38.2 (8.7) | 35.4 (8.6) | .279 |
| Low‐density lipoprotein, mg/dL | 112.1 (28.6) | 103.6 (32.6) | .348 |
| Triglycerides, mg/dL | 95.1 (59.9) | 148.7 (110.0) | .018 |
| Fasting glucose, mg/dL | 88.2 (9.9) | 89.6 (11.2) | .632 |
| Fasting insulin, IU/L | 13.1 (6.2) | 17.4 (9.8) | .110 |
| Urine albumin/creatinine | 0.07 (0.11) | 0.04 (0.03) | .144 |
All values are expressed as mean (standard deviation).
Table 4.
Echocardiographic Profile in Childhood‐Onset Essential Hypertension With and Without Left Ventricular Hypertrophy
| Left Ventricular Hypertrophy | P Value | ||
|---|---|---|---|
| No | Yes | ||
| Heart rate, beats per min | 74.4 (13.4) | 72.7 (13.6) | .5877 |
| Left ventricular mass, g | 121 (29.5) | 178.7 (30) | <.0001 |
| Left ventricular mass index, g/body surface area | 68.8 (12.3) | 90.8 (12.2) | <.0001 |
| Left ventricular mass index, g/cm2.7 | 31.7 (5.3) | 44.9 (4.6) | <.0001 |
| Relative wall thickness | 0.3 (0.04) | 0.4 (0.05) | <.0001 |
| Shortening fraction, % | 41.2 (9.3) | 50.8 (13.7) | .0002 |
| Ejection fraction, % | 78.2 (10.2) | 85.5 (9.4) | .0016 |
| Mitral valve E wave, cm/s | 98.4 (17.3) | 99.7 (28.2) | .7986 |
| Mitral valve A wave, cm/s | 52.5 (13.2) | 55 (16.1) | .4540 |
| Mitral valve E/A | 2.0 (0.5) | 1.9 (0.4) | .3403 |
| Velocity of circumferential fiber shortening, circ/s | 422.5 (19.1) | 426.1 (27.3) | .5374 |
| Mitral valve deceleration time, ms | 183.0 (35.6) | 180.5 (36.1) | .7557 |
| Mitral valve acceleration time, ms | 90.5 (15.4) | 96.8 (23.7) | .1471 |
| Isovolumic relaxation time, ms | 69.7 (12.8) | 79.6 (21) | .0081 |
| Left ventricular ejection time, ms | 295.6 (22.4) | 296.5 (28.5) | .8683 |
Values are expressed as mean (standard deviation) unless otherwise indicated.
In univariable analysis, LVH was significantly associated with weight/BMI but not with BP (Table 1 and Table 2). CIMT, triglyceride levels, and isovolumic relaxation time were significantly higher among hypertensive children with LVH compared with those without LVH (Table 3 and Table 4). Overall, the BMI z scores were significantly higher in children with LVH (mean, 1.9; SD, 0.6) than in those without LVH (mean, 1.2; SD, 0.9; P=.0002) (Figure 1, Table 1). In addition, univariable analysis of the degree of obesity showed that the odds of LVH was significantly higher in obese compared with normal‐weight children with EH (OR, 8.9; 95% CI, 2.3–34.3; P=.002). A similar trend but of a lower magnitude was observed in overweight children compared with normal‐weight children with EH; however, the trend failed to reach statistical significance (OR, 3.6; 95% CI, 0.8–16.0; P=.096).
Figure 1.

Box plots showing the distribution of body mass index (BMI) z scores in hypertensive children with and without left ventricular hypertrophy (LVH) (P=.0002).
Various multivariable models were assessed to identify the factors associated with LVH. Multivariable logistic regression analyses were performed to assess odds of LVH relative to differences in demographic (age, sex, ethnicity), anthropometric (weight, BMI, BMI z score), BP, laboratory, and vascular ultrasound parameters. From all the variables selected, only weight and/or BMI measurements were significantly associated with LVH. Adjusted for mean 24‐hour ambulatory systolic BP, the BMI z scores were significantly associated with LVH (OR, 5.69; 95% CI, 2.10–15.44; P=.001). Thus, for every incremental increase in SD of the BMI z score, the odds of LVH increased by more than five‐fold. The same models also showed that for every 10‐unit increase in mean 24‐hour ambulatory systolic BP, the odds of LVH approximately doubled (OR, 2.16; 95% CI, 1.04–4.49; P=.039).
There was, however, evidence of effect modification by the presence or absence of obesity on this relationship between systolic BP and LVH. Among the nonobese children, mean 24‐hour ambulatory systolic BP was significantly higher in children with LVH compared with those without LVH (mean 132 mm Hg, SD 10 vs mean 123 mm Hg, SD 7, respectively; P=.003) (Figure 2. In comparison, the obese children demonstrated similar levels of mean 24‐hour ambulatory systolic BP between the two LVH groups (mean 122 mm Hg, SD 9 vs mean 120 mm Hg, SD 9, respectively; P=.659) (Figure 2). Based on multivariable analysis, for every 10‐mm Hg increase in mean 24‐hour ambulatory systolic BP, the odds of LVH was much higher in the nonobese population (OR, 5.91; 95% CI, 1.18–29.6; P=.030) than in the obese population (OR, 1.23; 95% CI, 0.44–3.37; P=.693). This differential effect of obesity was also observed in the relationship of systolic BP measurements (in 10‐mm Hg increments) in the clinic and LVH, with a stronger association in obese (OR, 2.43; 95% CI, 1.07–5.52; P=.033) than in nonobese (OR, 1.29; 95% CI, 0.67–2.48; P=.453) children with EH.
Figure 2.
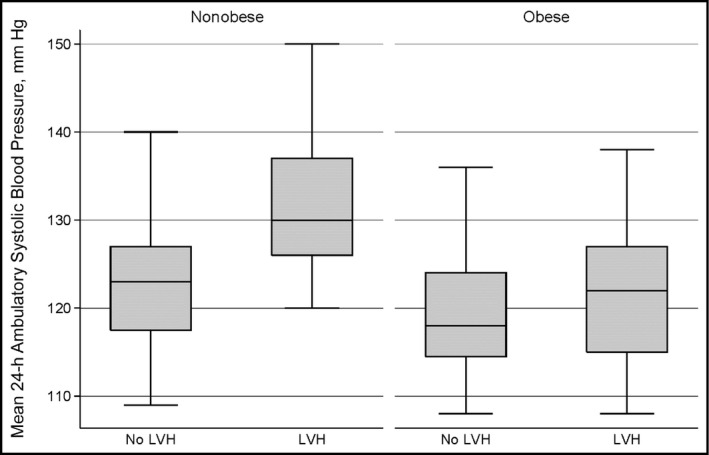
Box plots showing the association of systolic blood pressure with distribution of body mass index (BMI) z scores in obese and nonobese hypertensive children with and without left ventricular hypertrophy (LVH).
Discussion
In this study, we identified that among hypertensive children, BMI had a stronger independent effect on LVH than BP measures, both clinic systolic BP and mean 24‐hour ambulatory systolic BP. In addition, we identified the presence of effect modification by BMI on the association between LVH and BP.
Similar to previous reports,22, 23, 24, 27, 48 and after robust analysis, both BMI and systolic BPs were shown in our study to contribute to the LVH phenotype in children with EH. However, we have demonstrated that BMI has a higher contribution toward the presence of LVH. There was a nearly nine‐fold increased risk in the development of LVH among obese children compared with normal‐weight children with EH. In our study, for every 10‐mm Hg increase in the 24‐hour ambulatory mean systolic BP, the odds of LVH approximately doubled. Comparatively, the odds of LVH increased more than five‐fold for every unit increase in BMI z score.
We further identified that in childhood‐onset EH, both obesity and systolic BP were independently associated with LVH. Interestingly, the relationship between systolic BP and LVH in our study was modified by the presence of obesity, whereby the relationship existed mainly in the nonobese rather than the obese children with EH (Figure 2. Thus, the systolic BP values were significantly different between those with and those without LVH in the nonobese hypertensive children, with higher systolic BP values in those with LVH (Figure 2). However, the systolic BP values were not significantly different between those with and without LVH among the obese hypertensive children (Figure 2. In a study among African American adolescents, both obesity and high BP were found to be independently associated with elevated LVMI.32 Our finding has implications on clinical management of these children and may indicate that even when the systolic BP is controlled, the child may continue to have LVH if he or she is obese, although this needs to be determined by a longitudinal study. It is possible that management of systolic BP alone in obese children would not result in complete resolution of LVH unless weight is also controlled. Comparatively, in nonobese children, BP control may provide a beneficial outcome with respect to resolution of their LVH.
We found that LVH phenotype was significantly associated with higher body size, triglycerides, and arterial thickening. From previous studies, we know that LVH is prevalent among obese children and is seen in association with both elevated BP49, 50 and without elevated BP.27, 48, 51 Therefore, it is not surprising that even in children with EH in our study, obesity plays a role in the development of LVH. In our previous study, after multivariate analysis, we demonstrated that LV compliance indices correlated significantly with serum insulin levels in nondiabetic children with EH.1 Obesity along with elevated triglycerides was seen in association with LVH in our current study, indicating a potential role of cardiometabolic phenotype51 in the development of LVH among children with EH.
We also found abnormal diastolic distensibility or ventricular relaxation as evidenced by prolongation of the isovolumic relaxation time of the left ventricle in association with LVH in childhood‐onset EH. An alteration in LV filling with myocardial fibrosis and ischemia has been demonstrated in adults with hypertension. This diastolic dysfunction is related to inappropriately high levels of LVM, disproportionate to the hemodynamic load predicted by the individual body size and cardiac load. Delayed LV relaxation has been independently associated with concentric LV geometry in hypertensive adults, including obese patients.
Study Limitations
Our study was limited by the small sample size and lack of longitudinal data. Furthermore, our findings may not be generalizable as a result of its single‐center design. We recommend a larger, multicenter study with longitudinal data to confirm our findings.
Conclusions
In our multiethnic study of hypertensive children, we identified that obesity and systolic BP were both independently associated with LVH. Hence, to achieve reversal of end‐organ damage in children with EH, clinicians should take into account both BP control and weight management.
Acknowledgments and Disclosures
The project described was partially supported by grant number K23HL089301 (PI Monesha Gupta, MD) from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. Karen Redwine was funded by Arkansas Biosciences Institute, the major research component of the Tobacco Settlement Proceeds Act of 2000. Monesha Gupta‐Malhotra, MBBS, was funded by the National Institutes of Health.
J Clin Hypertens (Greenwich). 2016;18:449–455. DOI: 10.1111/jch.12708. © 2015 Wiley Periodicals, Inc.
References
- 1. Agu NC, McNiece Redwine K, Bell C, et al. Detection of early diastolic alterations by tissue Doppler imaging in untreated childhood‐onset essential hypertension. J Am Soc Hypertens. 2014;8:303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McNiece KL, Gupta‐Malhotra M, Samuels J, et al. Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 national high blood pressure education program working group staging criteria. Hypertension. 2007;50:392–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hanevold C, Waller J, Daniels S, et al. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the international pediatric hypertension association. Pediatrics. 2004;113:328–333. [DOI] [PubMed] [Google Scholar]
- 4. Gupta‐Malhotra M, Devereux RB, Dave A, et al. Aortic dilatation in children with systemic hypertension. J Am Soc Hypertens. 2014;8:239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sorof JM, Alexandrov AV, Cardwell G, Portman RJ. Carotid artery intimal‐medial thickness and left ventricular hypertrophy in children with elevated blood pressure. Pediatrics. 2003;111:61–66. [DOI] [PubMed] [Google Scholar]
- 6. Lande MB, Carson NL, Roy J, Meagher CC. Effects of childhood primary hypertension on carotid intima media thickness: a matched controlled study. Hypertension. 2006;48:40–44. [DOI] [PubMed] [Google Scholar]
- 7. Kimball TR, Daniels SR, Loggie JM, et al. Relation of left ventricular mass, preload, afterload and contractility in pediatric patients with essential hypertension. J Am Coll Cardiol. 1993;21:997–1001. [DOI] [PubMed] [Google Scholar]
- 8. Devereux RB, Pickering TG, Alderman MH, et al. Left ventricular hypertrophy in hypertension. Prevalence and relationship to pathophysiologic variables. Hypertension. 1987;9:II53–II60. [DOI] [PubMed] [Google Scholar]
- 9. Daniels SR, Loggie JM, Khoury P, Kimball TR. Left ventricular geometry and severe left ventricular hypertrophy in children and adolescents with essential hypertension. Circulation. 1998;97:1907–1911. [DOI] [PubMed] [Google Scholar]
- 10. Brady TM, Fivush B, Flynn JT, Parekh R. Ability of blood pressure to predict left ventricular hypertrophy in children with primary hypertension. J Pediatr. 2008;152:73–78, 78 e71. [DOI] [PubMed] [Google Scholar]
- 11. Schillaci G, Vaudo G, Pasqualini L, et al. Left ventricular mass and systolic dysfunction in essential hypertension. J Hum Hypertens. 2002;16:117–122. [DOI] [PubMed] [Google Scholar]
- 12. Schillaci G, Pasqualini L, Verdecchia P, et al. Prognostic significance of left ventricular diastolic dysfunction in essential hypertension. J Am Coll Cardiol. 2002;39:2005–2011. [DOI] [PubMed] [Google Scholar]
- 13. Muiesan ML, Salvetti M, Monteduro C, et al. Left ventricular concentric geometry during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension. 2004;43:731–738. [DOI] [PubMed] [Google Scholar]
- 14. Devereux RB, Wachtell K, Gerdts E, et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA. 2004;292:2350–2356. [DOI] [PubMed] [Google Scholar]
- 15. Verdecchia P, Porcellati C, Reboldi G, et al. Left ventricular hypertrophy as an independent predictor of acute cerebrovascular events in essential hypertension. Circulation. 2001;104:2039–2044. [DOI] [PubMed] [Google Scholar]
- 16. Verdecchia P, Carini G, Circo A, et al. Left ventricular mass and cardiovascular morbidity in essential hypertension: the mavi study. J Am Coll Cardiol. 2001;38:1829–1835. [DOI] [PubMed] [Google Scholar]
- 17. Koren MJ, Devereux RB, Casale PN, et al. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991;114:345–352. [DOI] [PubMed] [Google Scholar]
- 18. Schillaci G, Verdecchia P, Porcellati C, et al. Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension. 2000;35:580–586. [DOI] [PubMed] [Google Scholar]
- 19. Levy D, Garrison RJ, Savage DD, et al. Prognostic implications of echocardiographically determined left ventricular mass in the framingham heart study. N Engl J Med. 1990;322:1561–1566. [DOI] [PubMed] [Google Scholar]
- 20. Dahlof B, Devereux RB, Julius S, et al. Characteristics of 9194 patients with left ventricular hypertrophy: the life study. Losartan intervention for endpoint reduction in hypertension. Hypertension. 1998;32:989–997. [DOI] [PubMed] [Google Scholar]
- 21. Cook BB, Treiber FA, Mensah G, et al. Family history of hypertension and left ventricular mass in youth: possible mediating parameters. Am J Hypertens. 2001;14:351–356. [DOI] [PubMed] [Google Scholar]
- 22. Richey PA, Disessa TG, Somes GW, et al. Left ventricular geometry in children and adolescents with primary hypertension. Am J Hypertens. 2010;23:24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Assadi F. Relation of left ventricular hypertrophy to microalbuminuria and C‐reactive protein in children and adolescents with essential hypertension. Pediatr Cardiol. 2008;29:580–584. [DOI] [PubMed] [Google Scholar]
- 24. Pruette CS, Fivush BA, Flynn JT, Brady TM. Effects of obesity and race on left ventricular geometry in hypertensive children. Pediatr Nephrol. 2013;28:2015–2022. [DOI] [PubMed] [Google Scholar]
- 25. Sorof JM, Cardwell G, Franco K, Portman RJ. Ambulatory blood pressure and left ventricular mass index in hypertensive children. Hypertension. 2002;39:903–908. [DOI] [PubMed] [Google Scholar]
- 26. Richey PA, Disessa TG, Hastings MC, et al. Ambulatory blood pressure and increased left ventricular mass in children at risk for hypertension. J Pediatr. 2008;152:343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Maggio AB, Aggoun Y, Marchand LM, et al. Associations among obesity, blood pressure, and left ventricular mass. J Pediatr. 2008;152:489–493. [DOI] [PubMed] [Google Scholar]
- 28. Belsha CW, Wells TG, McNiece KL, et al. Influence of diurnal blood pressure variations on target organ abnormalities in adolescents with mild essential hypertension. Am J Hypertens. 1998;11:410–417. [DOI] [PubMed] [Google Scholar]
- 29. Sharma AP, Mohammed J, Thomas B, et al. Nighttime blood pressure, systolic blood pressure variability, and left ventricular mass index in children with hypertension. Pediatr Nephrol. 2013;28:1275–1282. [DOI] [PubMed] [Google Scholar]
- 30. Litwin M, Sladowska J, Antoniewicz J, et al. Metabolic abnormalities, insulin resistance, and metabolic syndrome in children with primary hypertension. Am J Hypertens. 2007;20:875–882. [DOI] [PubMed] [Google Scholar]
- 31. Sladowska‐Kozlowska J, Litwin M, Niemirska A, et al. Change in left ventricular geometry during antihypertensive treatment in children with primary hypertension. Pediatr Nephrol. 2011;26:2201–2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Falkner B, DeLoach S, Keith SW, Gidding SS. High risk blood pressure and obesity increase the risk for left ventricular hypertrophy in african‐american adolescents. J Pediatr. 2013;162:94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Armario P, del Rey RH, Sanchez P, et al. Determinants of left ventricular mass in untreated mildly hypertensive subjects: hospitalet study in mild hypertension. Am J Hypertens. 1999;12:1084–1090. [DOI] [PubMed] [Google Scholar]
- 34. Seeman T, Dostalek L, Gilik J. Control of hypertension in treated children and its association with target organ damage. Am J Hypertens. 2012;25:389–395. [DOI] [PubMed] [Google Scholar]
- 35. Ippisch HM, Inge TH, Daniels SR, et al. Reversibility of cardiac abnormalities in morbidly obese adolescents. J Am Coll Cardiol. 2008;51:1342–1348. [DOI] [PubMed] [Google Scholar]
- 36. Sorof JM, Turner J, Franco K, Portman RJ. Characteristics of hypertensive children identified by primary care referral compared with school‐based screening. J Pediatr. 2004;144:485–489. [DOI] [PubMed] [Google Scholar]
- 37.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 38. Urbina E, Alpert B, Flynn J, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association atherosclerosis, hypertension, and obesity in youth committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433–451. [DOI] [PubMed] [Google Scholar]
- 39. Lai WW, Geva T, Shirali GS, et al. Guidelines and standards for performance of a pediatric echocardiogram: a report from the task force of the pediatric council of the American Society of Echocardiography. J Am Soc Echocardiogr. 2006;19:1413–1430. [DOI] [PubMed] [Google Scholar]
- 40. Gottdiener JS, Bednarz J, Devereux R, et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17:1086–1119. [DOI] [PubMed] [Google Scholar]
- 41. Lopez L, Colan SD, Frommelt PC, et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the pediatric measurements writing group of the American Society of Echocardiography pediatric and congenital heart disease council. J Am Soc Echocardiogr. 2010;23:465–495; quiz 576‐467. [DOI] [PubMed] [Google Scholar]
- 42. Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458. [DOI] [PubMed] [Google Scholar]
- 43. Daniels SR, Kimball TR, Morrison JA, et al. Indexing left ventricular mass to account for differences in body size in children and adolescents without cardiovascular disease. Am J Cardiol. 1995;76:699–701. [DOI] [PubMed] [Google Scholar]
- 44. de Simone G, Daniels SR, Devereux RB, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20:1251–1260. [DOI] [PubMed] [Google Scholar]
- 45. de Simone G, Devereux RB, Daniels SR, et al. Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol. 1995;25:1056–1062. [DOI] [PubMed] [Google Scholar]
- 46. Khoury PR, Mitsnefes M, Daniels SR, Kimball TR. Age‐specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr. 2009;22:709–714. [DOI] [PubMed] [Google Scholar]
- 47. Roman MJ, Naqvi TZ, Gardin JM, et al. Clinical application of noninvasive vascular ultrasound in cardiovascular risk stratification: a report from the American Society of Echocardiography and the Society of Vascular Medicine and Biology. J Am Soc Echocardiogr. 2006;19:943–954. [DOI] [PubMed] [Google Scholar]
- 48. Kharod AM, Ramlogan SR, Kumar S, et al. Childhood obesity increases left‐ventricular mass irrespective of blood pressure status. Pediatr Cardiol. 2014;35:353–360. [DOI] [PubMed] [Google Scholar]
- 49. Chorin E, Hassidim A, Hartal M, et al. Trends in adolescents obesity and the association between BMI and blood pressure: a cross‐sectional study in 714,922 healthy teenagers. Am J Hypertens. 2015;28:1157–1163. [DOI] [PubMed] [Google Scholar]
- 50. Flynn JT, Alderman MH. Characteristics of children with primary hypertension seen at a referral center. Pediatr Nephrol. 2005;20:961–966. [DOI] [PubMed] [Google Scholar]
- 51. Di Bonito P, Moio N, Sibilio G, et al. Cardiometabolic phenotype in children with obesity. J Pediatr. 2014;165:1184–1189. [DOI] [PubMed] [Google Scholar]


