Abstract
The aim of this field study is to describe night shift resting and napping strategies and to examine their beneficial effects on sleepiness and quality of work. The study was carried out with 16 nurses working in an intensive care unit. Data collected during 20 night shifts were related to job demands (systematic observations), to the duration and timing of rests and naps taken by nurses (systematic observations, sleep diaries), to sleepiness (Karolinska Sleepiness Scale), and to quality of work scores (visual analog scale). The results showed that the number of rests and naps depended on the job demands. Resting and napping lowered the levels of sleepiness at the end of the shift. There was no direct relationship between sleepiness and the quality of work score. Discussions about the choice of indicators for the quality of work are necessary. Suggestions for implementing regulations for prescribed napping during night shifts are presented.
Keywords: Ergonomics, Hospital performance, Job outcomes, Night shift countermeasures, Shift work, Work analysis
The beneficial effects of napping during night shifts on various psychological and physiological measures have been demonstrated both in laboratory based studies and field studies. Field studies have shown that naps effectively decrease sleepiness measured subjectively (SSS) or objectively (EEG) and by using self-reported levels1, 2), and also help to maintain performance on a vigilance task in terms of response times3). Napping at work can also improve some mood dimensions4) and the quality and ease of work at night1). A recent review5) concluded that night shift napping led to decreased sleepiness and improved sleep related performance. In particular, the results of workplace napping studies have demonstrated these benefits mainly toward the end of the shift when the risk of errors is higher1, 4). Moreover, Smith-Coggins et al.5) showed that napping could improve performance in a simulated care task (intravenous catheter insertion) for healthcare professionals.
Nevertheless, napping is not always allowed in field situations and only resting is possible. The majority of studies suggesting that regular rests are an effective means of managing and maintaining performance have only assessed driving behavior and flight simulations during day shifts6). Rests must be understood as quiet times, different from eating or talking to co-workers or an experimenter. These studies underline the importance of autonomy and flexibility in the timing of within shift breaks, and also emphasize their effectiveness. Although many researchers recommend breaks to increase reliability (Eilers & Nachreiner, 1990, in Tucker, 20036)), few studies have found that resting during night shifts has a significant positive impact on performance. Given the relative lack of studies in this area, it is necessary to be careful when determining the respective effects of napping and resting. However, according to Åkerstedt & Landström7), rests can have a similar recuperating value to that of naps and can increase alertness at work. In line with Tucker6), we suggest that napping during a night shift will have a greater restorative effect on alertness than resting.
Post-nap and post-rest effects on job outcomes are not easy to assess, first because the number of errors, incidents, or accidents at work is low, and second because workers develop strategies to cope with variations in alertness and to accomplish tasks efficiently8). Thus, when evaluating job performance or work quality, one must find indicators other than the traditional ones to better represent the work actually accomplished. In order to assess hospital workers’ performance and work quality, it is necessary to understand that hospital performance is a multidimensional construct9), defined by the WHO as the achievement of objectives set in terms of services provided and their cost. Performance can be measured in terms of work quality as it is perceived by the different individuals concerned (patients, healthcare personnel, and financial and administrative staff) in relation to their expectations. The quality of night work, as defined above, can be considered from the standpoint of the health workers themselves, by attempting to determine their feelings about having finished their job on time and having done good work10).
In the present study, we tested the following hypotheses. First, the possibility of resting and napping at work, when there are no official scheduled periods for doing so, depends significantly on the job demands. Second, such rests and naps significantly reduce sleepiness at the end of a shift, with napping significantly more effective than resting. Third, rests and naps have some beneficial effects on self-evaluated healthcare work done by nurses, with napping having a significantly greater effect.
The study was carried out in an intensive care unit of a hospital cardiology ward with a total capacity of 20 patients. The staff of 16 nurses was composed of two alternating fixed night work teams consisting of five nurses each. The night shift hours were 8:45 p.m. to 6:45 a.m. The nursing staff had to administer health care and prescribed drugs to patients five times during the shift: 10 p.m., midnight, 2 a.m., 4 a.m., and 6 a.m. All sixteen nurses, who were between the ages of 22 and 52, volunteered to participate in the study. They had 6 months to 30 yr of experience in this care unit and 6 months to 10 yr on the night shift. Informed consent was obtained from each participant in the study.
The nursing staff had the opportunity to take rests and/or naps during two periods: first between the 2 a.m. and the 4 a.m. care periods and then between the 4 a.m. and the 6 a.m. care periods. For easier understanding, we refer to these two break opportunities during the night shift as the “3 a.m. break” and the “5 a.m. break”. Nevertheless, these schedules are flexible because break opportunities run from the end of the previous care episode to the beginning of the next care episode. In reality, the time and duration of break opportunities depend on the unit’s workload and differ each day. The administration of this hospital allows nurses to rest or nap during these breaks, even though they do not have a specific room (or suitable beds). Rests and naps are taken in the storage room, in reclining armchairs with the lights off. However, instruments that monitor the patients and give information to nurses for performing their tasks are located in the room and generate a constant level of noise.
Data were collected during 20 night shifts. Five nursing positions to which sixteen nurses were assigned were studied (all volunteers). The number of night shifts per nurse ranged from 1 to 11. Therefore, 20 night shifts for 5 nursing positions resulted in 100 potential night observations and 200 potential break opportunities. Two observations (including 4 break opportunities) were excluded from the analysis because of one nurse’s departure on one night due to operational and staffing demands. Ultimately, the data collected concerned 196 break opportunities. The presence of a researcher was necessary to collect data during these night shifts. The duration and timing of the breaks taken by the nursing staff were identified by systematic observations recorded by the researcher and by means of sleep diaries. Breaks taken by nurses and recorded by the researcher’s observations were labeled as “rest” or “nap”, according to whether or not the nurse declared having slept (time and duration) in her sleep diary.
Sleepiness ratings were obtained six times during the shift (0:30, 3:00, 4:00, 5:00, 6:00, and 6:45) using the Karolinska Sleepiness Scale or KSS, which ranges from 1 (very alert) to 9 (very sleepy, fighting sleep, an effort to stay awake). An earlier KSS rating (20:45) was used as the reference state. Other KSS times were determined before the “lunch” break (0:30), before and after each break opportunity (3:00 and 4:00 for the 3 a.m. break, and 5:00 and 6:00 for the 5 a.m. break) and at the end of the shift (6:45). Systematic observation of the work performed during the shift made it possible to gather information about job demands (hectic versus calm nights). A night was defined as calm if there were no heart failures, respiratory arrests, cardiac instabilities, or deaths that required attention by more than one team member for several minutes. Otherwise, the night was defined as hectic. Among the 20 night shifts observed, 9 were labeled calm and 11 were labeled hectic. At the end of each night shift, all the members of the nursing staff did a self-evaluation of the quality of their work by answering the question “Do you have the feeling that you did your work well?” on a visual analog scale (VAS) ranging from 1 (no) to 10 (yes). The protocol of this ergonomic study was approved by the hospital administration and by the executive management of the cardiology service’s intensive care unit.
Mixed linear models were used to analyze the sleepiness data11). Mixed models are more powerful than traditional multivariate tests because they minimize the consequences of missing data due to attrition. They enabled us to include participants who did not answer the KSS regularly during the night, and to take into account the repeated aspect of the night shifts (for example, the same nurse could be present on nights 1 and 12). This limited data waste and substantially increased the power of the analyses. The first set of analyses examined the effect of napping on the level of sleepiness throughout the night, after adjusting for sleepiness at the beginning of the shift and job demands. The interaction between the rest factor and the time of night was included in the model to detect a difference in sleepiness levels between the types of resting. The measures that were repeated during the night, and on different nights during the study, were included in the model as two random hierarchical effects, in order to take into account the correlation between these measures. One random effect was added for the night (several measures during the same night) and one random effect for the individual (several nights for the same individual). Data analyses were conducted using Stata statistical software (Version 11.2, StataCorp, College Station, TX, USA).
Table 1 details the distribution of each kind of break. We recorded 83 no rests, 81 rests and 32 naps in the 196 break opportunities. Napping was less frequent after the 2 a.m. care episode, corresponding to the 3 a.m. break (9.18%) than after the 4 a.m. care episode, corresponding to the 5 a.m. break (23.47%) (p<0.001, McNemar’s test). Naps taken during the 3 a.m. break began on average at 3:03 and lasted 59 min (min=34 min; max=85 min; SD=16.0 min). Naps taken during the 5 a.m. break began on average at 4:34 and lasted 49 min (min=10 min; max=88 min; SD=21.7 min). Rests were taken in one or more episodes during both break opportunities. Most of them were taken in one episode (36.7% at 3 a.m. and 44.9% at 5 a.m.) or two episodes (8.2% at 3 a.m. and 18.4% at 5 a.m.) while they were less frequent in the other conditions (1% at 3 a.m. and 2% at 5 a.m. in 3 episodes, and 0% at 3 a.m. and 4.1% at 5 a.m. in 4 episodes). In the two-, three- or four-episode conditions, all rests were interrupted because of a care demand (care monitor alarms, sustained supervision of a patient causing concern, heart failure, etc.). The mean start time of one-episode rests during the 3 a.m. break was 3:06, with a mean duration of 35.4 min (SD=25.05 min), while the mean start time during the 5 a.m. break was 04:28, with a mean duration of 48.4 min (SD=21.60 min). The mean start time of two-episode rests during the 3 a.m. break was 2:48, with a mean duration of 23.0 min (SD=13.80 min). Rests were interrupted on average at around 03:20 and finished at around 03:50 just before the 4:00 care episode. Two-episode rests took place during the 5 a.m. break at roughly the same period as the one-episode rests (between 04:30 and 05:25) with an interruption occurring sometime between 4:45 and 5:00.
Table 1. Rests and naps taken at 3 a.m. and at 5 a.m.: number (N) and percentage (N) of episodes per break.
| 3 a.m. break | 5 a.m. break | Total | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| No rest | 53 | 54.08 | 30 | 30.61 | 83 | 42.34 |
| Rest | 36 | 36.73 | 45 | 45.92 | 81 | 41.32 |
| Nap | 9 | 9.18 | 23 | 23.47 | 32 | 16.32 |
| Total | 98 | 100 | 98 | 100 | 196 | 100 |
In addition, among the 16 nurses who participated in the field study, half (8) took rests and naps; 6 nurses took only rests and 2 nurses did not take any rests or naps.
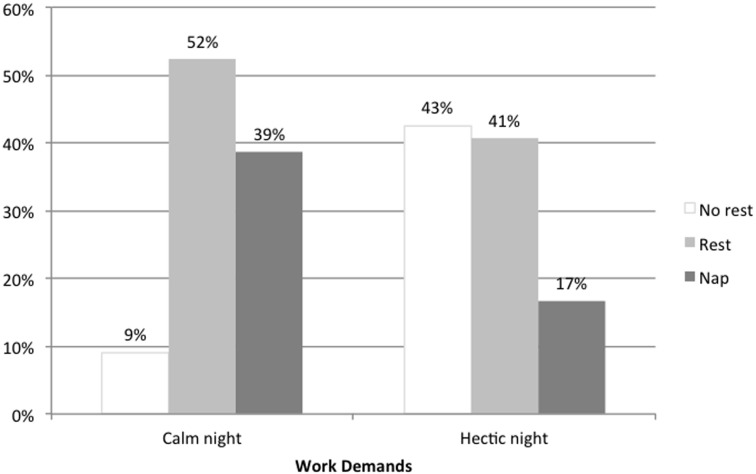
Naps and rests were more likely to be taken during calm night shifts than during hectic ones (p=0.001) (Fig. 1). On calm nights, rests were taken during 52% of the breaks and naps were taken during 39%. In contrast, on hectic nights, rests were taken in only 41% of the breaks while naps were taken in only 17%.
Fig. 1.
Percentage of no rests, rests, and naps, by job demands (calm or hectic night) (overall test p=0.001).
Subjective assessments of sleepiness during the night shift evolved in accordance with the rests/naps taken (no rests, rests, or naps) (Table 2). In the multivariate model, the sleepiness level evolved differently throughout the night depending on the type of rest taken, as shown by the interaction between the type of rest and the time (p<0.001). This model also included sleepiness at the beginning of the shift (p=0.007) and the type of night (p=NS) as covariates. Evaluation of sleepiness at 8:45 was thus not possible with this model as it was used as an adjustment variable. Our results showed that first, nurses who took a nap during the night shift had a higher sleepiness level at 4:00, 5:00 and 6:00 compared to nurses who did not nap. At the end of the night shift, this tendency was reversed: the levels of sleepiness at 6:45 were statistically lower in the nap condition than in the no rest condition. Second, nurses who took a rest had a higher sleepiness level at 4:00; 5:00 and 6:00 compared to nurses who did not rest. No significant effect of resting was observed at 6:45. Third, nurses who took naps had a higher sleepiness level at 4:00 and 6:00 than nurses who only rested.
Table 2. Marginal means of sleepiness according to time (0:30, 3:00, 4:00, 5:00, 6:00, 6:45) and type of rest (no rest, rest, nap) obtained from linear mixed model of regression of sleepiness during the night according to type of rest, type of night and sleepiness at the beginning of shift (8:45 p.m.).
| Time | Marginal means [95%CI] |
Comparisons between 2 categories at each time (p values) |
||||
|---|---|---|---|---|---|---|
| No rest (1) |
Rest (2) |
Nap (3) |
(1) vs. (2) | (1) vs. (3) | (2) vs. (3) | |
| 0:30 | 2.18 | 2.51 | 2.61 | 0.33 | 0.27 | 0.77 |
| [1.58 ; 2.79] | [2.01 ; 3.01] | [1.99 ; 3.24] | ||||
| 3:00 | 3.29 | 3.60 | 3.65 | 0.36 | 0.36 | 0.88 |
| [2.69 ; 3.90] | [3.10 ; 4.10] | [3.03 ; 4.27] | ||||
| 4:00 | 3.55 | 4.24 | 5.00 | 0.04* | 0.0003*** | 0.03* |
| [2.93 ; 4.17] | [3.75 ; 4.74] | [4.38 ; 5.62] | ||||
| 5:00 | 3.60 | 4.33 | 4.84 | 0.04* | 0.002** | 0.14 |
| [2.98 ; 4.23] | [3.84 ; 4.83] | [4.22 ; 5.47] | ||||
| 6:00 | 3.38 | 4.40 | 5.23 | 0.004** | <0.001*** | 0.02* |
| [2.74 ; 4.02] | [3.90 ; 4.90] | [4.61 ; 5.85] | ||||
| 6:45 | 4.29 | 3.67 | 3.42 | 0.06 | 0.03* | 0.48 |
| [3.69 ; 4.90] | [3.17 ; 4.16] | [2.80 ; 4.04] | ||||
*p<0.05, **p<0.01, ***p<0.001. No evaluation for sleepiness at 8:45 because this measurement was included as a covariate in the multivariate model.
The feeling of having done good work at the end of the night shift was positive, regardless of whether the nurses rested (no rests, rests, naps). Among the responses, 7% fell between 7 and 9 (on a scale going from 0 to 10) and all were above 4. There was no significant relationship between resting or napping and self-evaluated quality of work (p=0.10).
Conducted in a real work situation, this field study showed that opportunities to rest during night shifts were taken by workers. In France, napping is allowed but not formally scheduled. And in most field study settings, sleeping during work is forbidden. However, night workers are accustomed to getting some “unofficial” sleep whenever the demands of the job permit. In most of these cases, the setting is not suitable for sleeping but resting is possible. Nevertheless, this coping strategy depends on the job demands and the night worker’s level of sleepiness. In our study, nurses took more naps and rests during calm night shifts than during hectic ones. Moreover, there was a relationship between sleepiness during the shift and taking a nap during the night: nurses who took a nap had a higher sleepiness score at 5:00, e.g. before the 5 a.m. break, compared to nurses who did not nap.
The same result was observed in the rest condition. Napping and resting, like earlier or later scheduling of tasks during night shifts or the informal redistribution of tasks among team members as described in ergonomic studies12), can be seen as a tool for regulating work activity with the goal of enabling workers to be less sleepy and more effective during night work. These individual and collective dispositions are made possible by task flexibility and pace control by the individual worker6). It would be interesting to observe each nurse in the situations of the two job demands: calm night versus hectic night, but it was impossible in the time available for this field study.
Although the mixed linear models used to analyze the sleepiness data take into account individual variability, it was not possible within the current study design to take into account individual differences in the need for rest. For instance, in this field study, (the 2) nurses who did not take any rest or naps both worked during 2 hectic nights. However, it is not known whether these 2 nurses ever took any rest or naps, or if the main reason for not taking rest was the condition (hectic night) during the observed nights.
The originality of the present study lies in our comparison of resting and napping among shift workers, which has rarely been done in earlier studies on this topic4, 6). This study confirms the beneficial effects of napping during night shifts: taking a nap around 5 a.m. reduces sleepiness at the end of the night shift. On the other hand, the study did not demonstrate any positive effects of resting on sleepiness at the end of the night shift. It would be worthwhile to carry out more studies in work situations that give the possibility of using objective measures (for example, EEG and actigraphy) to show the difference between resting and napping. Proving the beneficial effects of naps and resting on work quality is a major argument in favor of introducing napping when organizing night shifts. However, according to the few studies on the subject, evaluating job outcomes in terms of performance and/or quality is a highly complex process5). In our study, the decline in sleepiness during the night shift after the nurses took naps did not systematically correspond to a significant increase in the feeling of having done a good job. We hypothesize that this subjective, qualitative measure of job outcome is not the most appropriate indicator. Future research should attempt to find relevant indicators of the positive impact of napping on work quality measures. The first step would be to find another subjective, qualitative measure that is closer to job performance or work quality, one that better represents the work actually carried out in a hospital. For example, observations from field research have shown that self-evaluation of individual healthcare and relationships with patients can be used to characterize conditions in hospital settings and could help to define indicators of nurses’ job performance. The second step would be to develop objective, quantifiable measures of work, such as the time spent collecting patients’ physiological data at the end of the shift, checking documents, or integrating and memorizing data at the same time, all of which are indicators shown to increase with sleepiness according to other field studies13).
From an operational point of view, planned resting and napping may not necessarily be feasible in all work situations, and therefore require an ergonomic analysis of the work14). Several conditions must be fulfilled. First, the workload has to allow workers to leave their workstation, and the skills of the night team must be shared to enable relaying between workers. Second, each member of the night staff must have shared knowledge of the work of co-workers in order to replace them. Third, a soundproof room that includes a bed for each worker must be reserved for resting and napping. Fourth, planned rests or naps must be prescribed and not just allowed15). Finally, programming and coordinating nap periods could reduce the potential negative side effects of napping, namely sleep inertia (i.e., the temporary degradation of performance in the immediate aftermath of sleep16)), on reliability. This could lead to a better formal organization for night shift teams and would allow workers to rest or sleep while making sure that co-workers stay awake and take over.
Acknowledgments
This work was funded by grants from the following organizations: Direction Générale de la Santé (DGS), Caisse Nationale d’Assurance Maladie des Travailleurs Salariés (CNAMTS), Régime Social des Indépendants (RSI), and Caisse Nationale de Solidarité pour l’Autonomie (CNSA), as part of the call for projects launched by the Institut de Recherche en Santé Publique (IReSP) in 2009. We thank Allison Baubiat, Ludovic Gabet, and Cécile Claveau for their help with data collection. We also thank the hospital ward and all of the nurses and assistant nurses who participated in the study.
References
- 1.Bonnefond A, Muzet A, Winter-Dill AS, Bailloeuil C, Bitouze F, Bonneau A. (2001) Innovative working schedule: introducing one short nap during the night shift. Ergonomics 44, 937–45. [DOI] [PubMed] [Google Scholar]
- 2.Takahashi M, Fukuda H, Miki K, Haratani T, Kurabayashi L, Hisanaga N, Arito H, Takahashi H, Egoshi M, Sakurai M. (1999) Shift work-related problems in 16-h night shift nurses (2): Effects on subjective symptoms, physical activity, heart rate, and sleep. Ind Health 37, 228–36. [DOI] [PubMed] [Google Scholar]
- 3.Signal TL, Gander PH, Anderson H, Brash S. (2009) Scheduled napping as a countermeasure to sleepiness in air traffic controllers. J Sleep Res 18, 11–9. [DOI] [PubMed] [Google Scholar]
- 4.Smith-Coggins R, Howard SK, Mac DT, Wang C, Kwan S, Rosekind MR, Sowb Y, Balise R, Levis J, Gaba DM. (2006) Improving alertness and performance in emergency department physicians and nurses: the use of planned naps. Ann Emerg Med 48, 596–604, 604.e1–3. [DOI] [PubMed] [Google Scholar]
- 5.Ruggiero JS, Redeker NS. (2014) Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: a systematic review. Biol Res Nurs 16, 134–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tucker P. (2003) The impact of rest breaks upon accident risk, fatigue and performance: a review. Work Stress 17, 123–37. [Google Scholar]
- 7.Åkerstedt T, Landström U. (1998) Work place countermeasures of night shift fatigue. Int J Ind Ergon 21, 167–78. [Google Scholar]
- 8.Barthe B, Quéinnec Y. (2005) Work activity during night shifts in a hospital’s neonatal department: how nurses reorganize health care to adapt to their alertness decrease. Ergonomia IJE HF 27, 119–29. [Google Scholar]
- 9.Sicotte C, Champagne F, Contandriopoulos AP, Barnsley J, Béland F, Leggat SG, Denis JL, Bilodeau H, Langley A, Brémond M, Baker GR. (1998) A conceptual framework for the analysis of health care organizations’ performance. Health Serv Manage Res 11, 24–41, discussion 41–8. [DOI] [PubMed] [Google Scholar]
- 10.Daniellou F. (2009) L’ergonome et les débats sur la performance de l’entreprise. Actes des Journées de Bordeaux sur la Pratique de l’Ergonomie, 9–18. [Google Scholar]
- 11.Rabe-Hesketh S, Skrondal A. (2000) Multilevel and Longitudinal Modeling Using Stata, 2nd Ed. Stata Press, Texas.
- 12.Toupin C, Barthe B, Prunier-Poulmaire S .(2014) From constrained to constructed working time: Toward an enabling organization of work in rotating shifts and night shifts. In: Falzon P (Ed.), Constructive ergonomics 1–94, CRC Press, Boca Raton. [Google Scholar]
- 13.Tirilly G, Cabon P, Beslot P .(2011) Strategies used by train drivers to cope with irregular working hours. 20th International Symposium on Shiftwork and Working Time, 27 June-1 July 2011, Stockholm.
- 14.Guerin F, Laville A, Daniellou F, Duraffourg J, Kerguelen A .(2007) Understanding and Transforming Work. The Practice of Ergonomics. ANACT, Lyon. [Google Scholar]
- 15.Takahashi M. (2003) The role of prescribed napping in sleep medicine. Sleep Med Rev 7, 227–35. [DOI] [PubMed] [Google Scholar]
- 16.Dinges DF .(1992) Adult napping and its effects on ability to function. In: Stampi CA (Ed.), Why We Nap: Evolution Chronobiology and Functions of Polyphasic and Ultrashort Sleep, 118–134, Birkhäuser, Boston. [Google Scholar]