Abstract
Background:
Migraine is a common disabling primary headache disorder. Globally, migraine was ranked as the seventh highest cause of disability.
Aim:
The aim of the study was to explore the clinical profile and functional disability of patients with migraine.
Settings and Design:
A cross-sectional survey was conducted at the neurology outpatient department of a tertiary care hospital in Karnataka.
Materials and Methods:
Using a consecutive sampling technique, 60 patients were recruited for the study. Descriptive and inferential statistics were used to analyze the data.
Results:
Majority of the participants were in the age group of 18–40 years with a mean age 35.22 years. There was a female preponderance with 70% of study participants being females. The various symptoms experienced by patients include throbbing pain (90%), photophobia (93.3%), phonophobia (85%), nausea (76.7%), and vomiting (41.7%). Most of the subjects (73.3%) under the study belonged to moderate to severe levels of functional disability. About 53.3% of patients were in the category of episodic migraine and 46.7% were in the category of chronic migraine.
Conclusion:
Migraine is associated with moderate to severe functional disability. Frequency of migraine has a positive correlation with the levels of disability/migraine disability assessment scores of migraineurs.
Keywords: Clinical profile, disability, headache, migraine disability assessment, migraine, migraineur
Introduction
Migraine is a common disabling primary headache disorder. The two major subtypes of migraine are the “migraine without aura” and the “migraine with aura.” Migraine without aura is a clinical syndrome characterized by specific features and associated symptoms whereas migraine with aura is characterized by focal neurological symptoms that precede or sometimes accompany the headache.[1]
Migraine and tension-type headaches are reported as the most prevalent disorders of mankind by the “Atlas of Headache Disorders, WHO.” The prevalence of migraine in South East Asian region is 10.9%.[2] Extrapolated statistics on “Prevalence Rate of Migraine to Countries and Regions” reported that approximately 109 million Indians are suffering from migraine.[3] A study on population-based prevalence estimates of headache disorders in Karnataka reported the crude 1-year prevalence of migraine as 25.6%. The prevalence of migraine among females (32.4%) is higher than that of males (18.6%).[4]
Migraine is documented as a major cause of disability worldwide. The World Health Report 2001 cited migraine as the 19th leading cause of Years of Life lived with Disability.[5] The “Global Burden of Headache a documentation of headache prevalence and disability worldwide” reported migraine as the leading cause of disability among neurological disorders.[6,7,8] Globally, migraine was ranked as the seventh highest cause of disability.[8]
Migraine is associated with considerable functional disabilities and may lead to physical, psychological, and social consequences. Aspects of the lives including occupational, academic, social, leisure, and family responsibilities are affected by migraine. The objective of the study was to explore the clinical profile and functional disability of patients with migraine.
Materials and Methods
Research design and sample
The study approach was a quantitative research approach and the design was a cross-sectional survey design. The study was conducted at the neurology outpatient department of a tertiary care hospital in Karnataka. The study population comprised adults of age group, 18–64 years who were diagnosed to have “migraine without aura.” Those subjects with known psychiatric comorbidities, those who refused consent, and those who were acutely ill during the time of hospital visit were excluded from the study.
Sampling and data collection
Using a consecutive sampling technique, 60 patients were recruited for the study. The sample size for the study was calculated statistically. The study was conducted in the year 2013 with 1 month for data collection. International Classification of Headache Diseases II criteria was used to diagnose the patients. The diagnosis of the patients was made by a registered neurologist.[1]
Ethical considerations
To safeguard the rights of patients and to abide by the principles of bioethics, administrative permissions were obtained from the concerned administrators of the respective institutions. The study was reviewed and approved by the Institutional Review Committee and Institutional Ethics Committee. Written informed consent was obtained from the migraineurs prior to the data collection. Migraineurs were informed of their rights to voluntarily consent or decline to participate and to withdraw participation at any time without penalty.
Data collection instruments
Demographic and clinical data questionnaire
The questionnaire consisted of two parts. Part A comprised 8 items that were used to gather the basic background information of the study participants such as age, gender, education, occupation, place of residence, type of family, duration of illness, and family history of migraine. Part B consisted of 10 items pertaining to the clinical features/symptoms experienced by the migraineurs.
Modified Kuppuswamy's socioeconomic status scale
Modified Kuppuswamy's socioeconomic status scale (2012) was used to assess the socioeconomic status of the migraineurs. The scale determines the socioeconomic status of family based on education and occupation of head of the family. It consists of 3 items, and each item is subdivided into seven subscales. The maximum score is 27 and the minimum score is 3. Based on the total scores, socioeconomic status is divided into five levels, the upper class (26–29), upper middle class (16–25), lower middle class (11–15), upper lower class (5–10), and lower class (<5).[9]
Migraine disability assessment questionnaire
The migraine disability assessment (MIDAS) is a short, self-administered questionnaire that is a widely used tool in clinical research and as well as in clinical practice to assess migraine-related functional disability.[10,11,12,13] It determines how many days in the past 3 months of the migraineurs life was affected to the point that he/she was unable to function in a way to which he/she is accustomed to. The MIDAS score is derived as a sum of 5 questions pertaining to missed days of nonwork-related activities (family, social, and leisure) as well as the number of days the productivity at work (household and paid work) was reduced by half during the past 3-month period.[11] The total scores are classified into five levels of disability (Grade I - Little or No Disability, Grade II - Mild disability, Grade III - Moderate disability, and Grade IV - High disability). Validity and reliability of MIDAs have been demonstrated by a large number of studies.[10,14,15,16]
Psychometric testing of the instruments
To establish the content validity of the tool, the tools were submitted to a panel of five experts and an experiential validator. The experts were selected on the basis of their clinical expertise, experience and interest in the problem being studied. The experts evaluated each item in terms of their relevance, adequacy, and appropriateness. The Item Content Validity Index (ICVI) and the scale content validity index (S-CVI/Ave) were calculated. The mean ICVI as well as the S-CVI/Ave of the tools was 1.0. Hence, it was found relevant to use these tools in the study.
All the data collection instruments were in English and was translated to Kannada (local language) using a centered translation approach. A professional language translator translated the tool from English to Kannada. To ensure the accuracy of the translation, the tools were then retranslated into English. The translated and retranslated tools were found to be the same. The Kannada versions of instruments were subjected to pretesting among 10 migraineurs. As there was no ambiguity/confusion raised by the migraineurs, no modifications were made.
After validation, translation and pretesting, the Kannada version of the Modified Kuppuswamy's Socio-Economic Status Scale as well as the MIDAS questionnaire was subjected to the test for its reliability. The tools were administered to 20 migraineurs. The internal consistency aspect of the tools was computed using Cronbach's Alpha (α) formula. The reliability coefficient for the Kannada version of the modified Kuppuswamy's socioeconomic status scale was “α” = 0.90 and the MIDAS questionnaire was “α” = 0.71. Hence, the tools were considered reliable.
A pilot study was conducted among 20 migraineurs to assess the feasibility and practicability of the research design. The migraineurs of the pilot study possessed the same characteristics as that of the migraineurs of the main study. The study was found feasible to be conducted in the planned setting.
Statistical analysis
IBM Statistical Package for Social Sciences software (version 15) was used for data analysis. Descriptive and inferential statistics was used to analyze the data. Frequency and percentage were computed for summarizing the categorical variables. Spearman's correlation coefficient was used to find the relationship between the frequency of attacks and functional disability. The results are presented in narratives, tables, and figures.
Results
Sociodemographic characteristics
Majority of the study participants were in the age group of 18–40 years (65%). There was a female preponderance with 70% of the study participants being females. Sixty-eight percent of the participants were residing in rural areas and most of them (83.3%) were from the nuclear type of family. A positive family history of migraine was present only in 28.3% of the study participants. The sociodemographic characteristics are described in Table 1.
Table 1.
Sociodemographic characteristics of participants (n=60)

Clinical profile
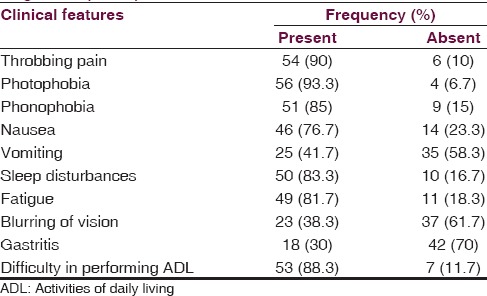
The clinical features/symptoms experienced by patients with migraine were explored. Ninety percent of the participants experienced throbbing kind of headaches. Photophobia was experienced by 93.3% of the participants whereas 85% reported having phonophobia. Nausea and vomiting were experienced by 76.7% and 41.7% of participants, respectively. Sleep disturbance was experienced by 83.3% of the study participants. Majority of the participants (88.3%) reported that they experience difficulty in performing the activities of daily living. The clinical features are discussed in Table 2.
Table 2.
The clinical features of the patients with migraine (n=60)
To have a better understanding on the frequency of attacks, migraineurs were categorized as cases of episodic and chronic migraine (CM). Migraineurs who have 0–14 headache days per month are categorized as episodic migraine (EM) whereas those with 15 or more days per month are categorized as CM.[17] Frequency and percentage analysis showed that 32 (53.3%) of subjects were having EM and 28 (46.7%) were having CM [Figure 1].
Figure 1.
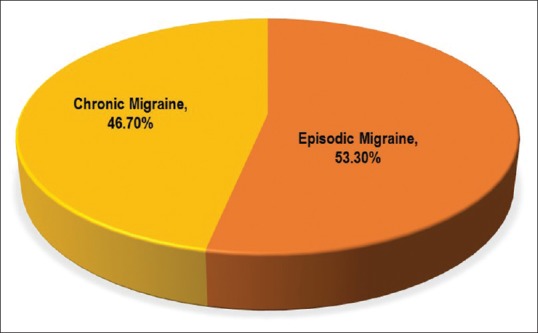
Pie diagram on the type of migraine
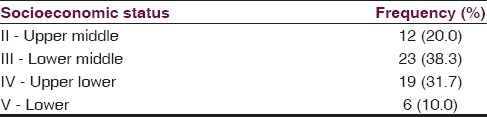
Socioeconomic status
Socioeconomic status of the participants was assessed using the Kuppuswamy's socioeconomic status scale. All the participants belonged to the middle or upper class families. Of the 60 participants, 12 (20%) belonged to the upper middle class, 23 (38.3%) to lower middle class, 19 (31.7%) to the upper lower class, and 6 (10%) in the lower class [Table 3].
Table 3.
Socioeconomic status of the study participants (n=60)
Functional disability of migraineurs
Disability assessment of migraineurs using MIDAS questionnaire revealed that 41.7% of migraineurs had moderate disability and 31.6% had severe disability [Figure 2].
Figure 2.
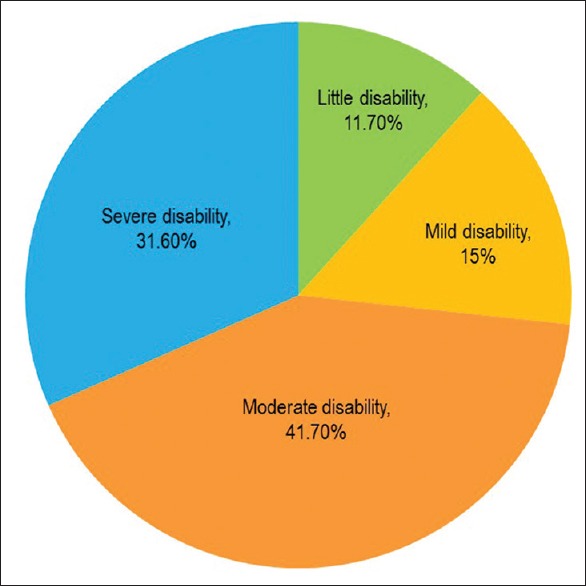
Pie diagram on functional disability of migraineurs (n = 60)
For further understanding, area-specific frequency estimates for levels of disability was computed. The results showed that there is a progressive trend in disability across subjects in the episodic and CM groups. In the EM group (n = 32), 21.9% had little or no disability, 28.1% had mild disability, and 50% had high disability. In the CM group (n = 28), none of them had little or mild levels of disability. The majority in this group (67.90%) demonstrated high levels of functional disability [Figure 3].
Figure 3.
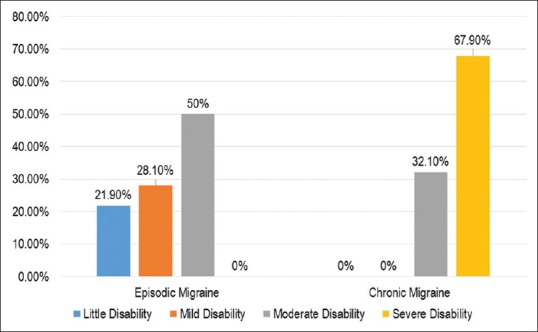
Bar diagram on levels of functional disability (Episodic vs. Chronic Migraine) (n = 60)
Item-wise frequency and percentage of functional disability were computed among episodic (n = 32), chronic (n = 28), and the total number (n = 60) of participants. The item-wise mean scores obtained in questions 1 through 5 and the 2 supplementary questions are shown in Table 3. The group with CM had more missed more days from work/school (1.89 [95% confidence interval (CI), 0.8–2.9] vs. 0.69 [95% CI, 0.2–1.1]), had more days of reduced productivity at work/school (6.71 [95% CI, 3.5–9.9] vs. 1.91 [95% CI, 0.8–2.9]), missed more days of housework (4.57 [95% CI, 3.07–6.08] vs. 2.44 [95% CI,1.35–3.52]), reduced effectiveness in housework (9.43 [95% CI, 6.53–12.33] vs. 4.28 [95% CI, 2.63–5.94]), days missed from family, social, or leisure activities (1.0 [95% CI, 0.28–1.72] vs. 0.19 [95% CI, 0.02–0.36]), total headache days over 3 months (23 [95% CI, 21.5–25.6] vs. 9.5 [95% CI, 8.0–10.9]) [Table 4].
Table 4.
Item-wise frequency and percentage of migraine disability assessment

Pain scores
Pain intensity was assessed using the last item of MIDAS test. The pain scores ranged from 4 to 10 on a 10-point numerical pain scale. The mean (standard deviation [SD]) pain score was 7.75 (1.71) (95% CI, 7.31–8.19), which denotes that migraine often results in high-intensity pain [Table 3]. Figure 4 represents the pain score of migraineurs.
Figure 4.
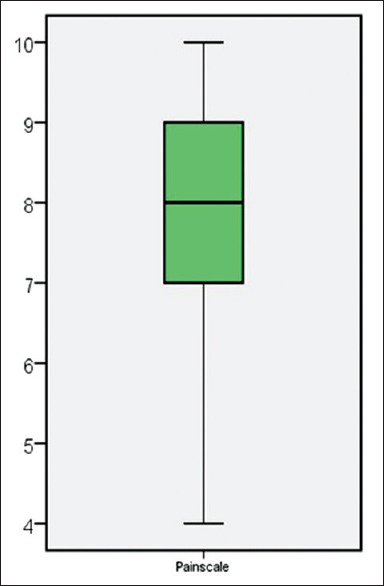
Box and Whiskers plot on pain score of migraineurs (n = 60)
Correlation between frequency of attacks and the levels of disability
Spearman's rho was computed in order to find the relationship between the frequency of attacks (EM, CM) and the levels of disability (little, mild, moderate, severe). The frequency of migraine had a positive correlation with the levels of disability (P = 0.76) of migraineurs. It is interpreted that patients with high frequency of migraine attacks experience higher levels of functional disability.
Discussion
Migraine is represented as a spectrum of disease with migraine characterized by high rates of attacks associated with high levels of pain at one end and mild attacks with fewer pain scores at another end. This wide variability in illness representation has got implications in the treatment for migraine. MIDAS questionnaire can be used as an effective clinical measure to identify the severity of illness and can be an inevitable tool in planning treatment for migraineurs.[11] The findings of the present study support and further illuminate results of similar researches specific to the disability of patients with migraine.[12,13,18,19,20,21,22]
Majority of the participants in the present study were in the age group of 18–40 years with a mean age 35.22 years. There was a female preponderance with 70% of study participants being females. Family history of migraine was present in 28.3% of subjects. The various symptoms experienced by patients include throbbing pain (90%), photophobia (93.3%), phonophobia (85%), nausea (76.7%), and vomiting (41.7). Most of the subjects (73.3%) under the study belonged to moderate to severe levels of functional disability. About 53.3% of patients were in the category of EM, and 46.7% were in the category of CM. Frequency of migraine had a positive correlation with the levels of disability/MIDAS scores of migraineurs.
These study findings are consistent with the study findings of Bigal et al.[12] In their study, the researchers compared the MIDAS scores of patients with episodic (n = 182) and CM (n = 86). The sample consisted of mainly women (72.5%), with a mean age of 38.3 years. The results showed that people with CM have higher grades of disability (MIDAS grade IV) when compared to EM. The average total MIDAS score was 34.9 in CM group whereas it was 19.3 in the EM group.
Our study is in par with the findings of the study by Ruscheweyh et al.[18] and Blumenfeld et al.,[19] which reported a high prevalence of migraine among females. The above studies[18,19] also reported that MIDAS grades were significantly higher among CM than EM.
In our study, the mean (SD) of headache frequency for the past 3 months in EM group was 9.5 (4.13) and the majority of the subjects had mild to moderate levels of functional disability. These findings are supported by the study of Smitherman[20] which reported the 3-month mean (SD) headache frequency among EM as 9.39 (10.47).
Stewart et al.[13] explored the relationship of MIDAS scores with headache frequency, intensity, and other headache symptoms. Regression analysis showed that MIDAS score is associated with headache frequency and average pain score. These findings support the findings of the present study.
The present study contradicts the findings of a US-based study by Frederick et al.,[21] which strongly supports positive family history as a correlate of migraine prevalence, whereas in our study, only a small population (28.3%) of the participants presented with a positive family history of migraine.
FRAMIG 3,[22] a population-based study conducted in France, examined the MIDAS scores of 1843 subjects: Of these, majority were in the category of Grade I (65.0%) and only 6.1% where in the grade IV category, whereas in our study only 11.7% of the participants were in the Grade I and 31.6% were in the grade IV category.
Limitations
The results of our study must be seen within its limitations. The study was conducted for a small representative group of the whole population. Hence, generalization is limited. Since it was a cross-sectional study, the effect of drugs on the level of disability was not measured. A prospective longitudinal study would give more insight on this area. Even though we did a separate analysis for EM and CM, we could not match or stratify the subjects during the sampling process.
Conclusion
In this study, we found that migraine is associated with moderate to severe functional disability. The results of the study can be used as an evidence base to develop a holistic management plan for patients with migraine headaches. MIDAS can be used as a valuable instrument to identify the headache-related disability and plan treatment accordingly. Despite its high prevalence and burden it pose on the sufferers, unfortunately, migraine remains as a less researched area of primary care. More studies focusing on the quality of life, well-being, and disability levels of patients with migraine are necessary.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. The World Health Report 2001. Geneva: WHO; 2001. [Google Scholar]
- 3.Extrapolation Statistics on Prevalence Rate of Migraine to Countries and Regions 2012. [Last accessed on 2013 Mar 03]. Available from: http://www.rightdiagnosis.com/m/migraine/stats-country.htm#extrapwarning .
- 4.Kulkarni GB, Rao GN, Gururaj G, Stovner LJ, Steiner TJ. Headache disorders and public ill-health in India: Prevalence estimates in Karnataka State. J Headache Pain. 2015;16:67. doi: 10.1186/s10194-015-0549-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Atlas of Headache Disorders and Resources in the World 2011. Geneva: WHO; 2011. [Google Scholar]
- 6.Leonardi M, Steiner TJ, Scher AT, Lipton RB. The global burden of migraine: Measuring disability in headache disorders with WHO's classification of functioning, disability and health (ICF) J Headache Pain. 2005;6:429–40. doi: 10.1007/s10194-005-0252-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, et al. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210. doi: 10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 8.Steiner TJ, Stovner LJ, Birbeck GL. Migraine: The seventh disabler. J Headache Pain. 2013;14:1. doi: 10.1186/1129-2377-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar N, Gupta N, Kishore J. Kuppuswamy's socioeconomic scale: Updating income ranges for the year 2012. Indian J Public Health. 2012;56:103–4. doi: 10.4103/0019-557X.96988. [DOI] [PubMed] [Google Scholar]
- 10.Stewart WF, Lipton RB, Whyte J, Dowson A, Kolodner K, Liberman JN, et al. An international study to assess reliability of the migraine disability assessment (MIDAS) score. Neurology. 1999;53:988–94. doi: 10.1212/wnl.53.5.988. [DOI] [PubMed] [Google Scholar]
- 11.Lipton RB, Stewart WF, Sawyer J, Edmeads JG. Clinical utility of an instrument assessing migraine disability: The migraine disability assessment (MIDAS) questionnaire. Headache. 2001;41:854–61. [PubMed] [Google Scholar]
- 12.Bigal ME, Rapoport AM, Lipton RB, Tepper SJ, Sheftell FD. Assessment of migraine disability using the migraine disability assessment (MIDAS) questionnaire: A comparison of chronic migraine with episodic migraine. Headache. 2003;43:336–42. doi: 10.1046/j.1526-4610.2003.03068.x. [DOI] [PubMed] [Google Scholar]
- 13.Stewart WF, Lipton RB, Kolodner K. Migraine disability assessment (MIDAS) score: Relation to headache frequency, pain intensity, and headache symptoms. Headache. 2003;43:258–65. doi: 10.1046/j.1526-4610.2003.03050.x. [DOI] [PubMed] [Google Scholar]
- 14.Stewart WF, Lipton RB, Kolodner K, Liberman J, Sawyer J. Reliability of the migraine disability assessment score in a population-based sample of headache sufferers. Cephalalgia. 1999;19:107–14. doi: 10.1046/j.1468-2982.1999.019002107.x. [DOI] [PubMed] [Google Scholar]
- 15.Stewart WF, Lipton RB, Kolodner KB, Sawyer J, Lee C, Liberman JN. Validity of the migraine disability assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain. 2000;88:41–52. doi: 10.1016/S0304-3959(00)00305-5. [DOI] [PubMed] [Google Scholar]
- 16.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20–8. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 17.Katsarava Z, Buse DC, Manack AN, Lipton RB. Defining the differences between episodic migraine and chronic migraine. Curr Pain Headache Rep. 2012;16:86–92. doi: 10.1007/s11916-011-0233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruscheweyh R, Müller M, Blum B, Straube A. Correlation of headache frequency and psychosocial impairment in migraine: A cross-sectional study. Headache. 2014;54:861–71. doi: 10.1111/head.12195. [DOI] [PubMed] [Google Scholar]
- 19.Blumenfeld AM, Bloudek LM, Becker WJ, Buse DC, Varon SF, Maglinte GA, et al. Patterns of use and reasons for discontinuation of prophylactic medications for episodic migraine and chronic migraine: Results from the second international burden of migraine study (IBMS-II) Headache. 2013;53:644–55. doi: 10.1111/head.12055. [DOI] [PubMed] [Google Scholar]
- 20.Smitherman TA, McDermott MJ, Buchanan EM. Negative impact of episodic migraine on a university population: Quality of life, functional impairment, and comorbid psychiatric symptoms. Headache. 2011;51:581–9. doi: 10.1111/j.1526-4610.2011.01857.x. [DOI] [PubMed] [Google Scholar]
- 21.Frederick IO, Qiu C, Enquobahrie DA, Aurora SK, Peterlin BL, Gelaye B, et al. Lifetime prevalence and correlates of migraine among women in a pacific northwest pregnancy cohort study. Headache. 2014;54:675–85. doi: 10.1111/head.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lucas C, Géraud G, Valade D, Chautard MH, Lantéri-Minet M. Recognition and therapeutic management of migraine in 2004, in France: Results of FRAMIG 3, a French nationwide population-based survey. Headache. 2006;46:715–25. doi: 10.1111/j.1526-4610.2006.00430.x. [DOI] [PubMed] [Google Scholar]


