Abstract
Background/Object:
The ligation and transection of anterior third of superior sagittal sinus (AT-SSS) is an important step to approach anterior skull base lesions. Some clinical studies have shown frontal lobe venous infarct following such surgical procedures questioning the safety of its ligation. We have studied the variations in venous drainage patterns to AT-SSS in the normal population using postcontrast magnetic resonance venogram (MRV). A novel scoring system to recognize the subgroup with dominant venous drainage from frontal lobes has been described.
Materials and Methods:
In this study, 60 three-dimensional contrast-enhanced (CE) MRVs were obtained from those cases being evaluated for a headache not harboring any intracranial mass lesion. The AT-SSS with all its draining veins was studied in detail. Morphology of individual veins such as length, caliber, tributaries, and angulation with AT-SSS was studied, and a numerical value of 0 or 1 was assigned for each of the above parameters. Summing up these scores derived from the individual cortical veins quantified the drainage of AT-SSS.
Results:
There are 3–4 veins on either side draining to AT-SSS. Barely, 3% of the veins had > 3 tributaries. Only 6.6% of veins had a caliber >3 mm, and 16.5% drained at acute angles to AT-SSS. About 26% of the veins did cross at least half of the lateral frontal lobe. We found in 26 individuals the AT-SSS score was 0–2, in 22 it was 3–5 and, in only in 12 (20%) the score was 6 or more (dominant drainage).
Conclusion:
There are anatomical variations in venous drainage of frontal lobes into AT-SSS. Those with dominant drainage are likely to develop venous congestion and complications if sacrificed. It is possible to identify these individuals on the basis of venous drainage pattern as shown in CE-MRV.
Keywords: Anterior third superior sagittal sinus, high risk, ligation, normal population, scoring system, three-dimensional contrast-enhanced magnetic resonance venogram, variations
Introduction
Resection of anterior third of superior sagittal sinus (AT-SSS) has been considered safe since the descriptions of parasagittal meningiomas by Cushing.[1] Apart from parasagittal meningiomas, AT-SSS has been ligated and transected to approach anterior skull base lesions. However, the consequences of it are less discussed. The literature related to complications secondary to ligation of AT-SSS is sparse.[2,3] Usually, they manifest as venous infarct or edema of frontal lobes in a few cases of anterior skull base lesions where the AT-SSS is ligated and transected.
It was thought that the AT-SSS drains a little portion of frontal lobes justifying its resection. In addition, the venous flow may be diverted to sylvian veins after its ligation. However, it may not be true in all individuals. In fact, there is some evidence that in a subset, the AT-SSS receives venous drainage from a major portion of frontal lobes.[3,4] Probably, these are the cases where resection or ligation and division of AT-SSS may produce complications.
Preoperative risk stratification for safe ligation of AT-SSS is, therefore, essential in anterior skull base surgery. The purpose of this study was to evaluate the variation in patterns of venous drainage to AT-SSS using three-dimensional contrast-enhanced magnetic resonance venogram (3D CEMRV) in normal individuals and to identify the individuals with dominant drainage where ligation of AT-SSS may be unsafe.
Materials and Methods
Data
We studied the venous architecture of AT-SSS with 3D CEMRV in 60 adults who had normal findings on MR examination. These patients were evaluated for a headache. Patients with intracranial mass lesions, congenital anomalies, venous thrombosis, cerebrovascular disease, or previous intracranial surgery were excluded from the study.
Imaging technique
All magnetic resonance imaging (MRI) studies were performed on 3.0T MR scanners (Siemens Medical Solutions, Erlangen, Germany) using 32 channel head coil. Initially, routine MRI sequences were acquired including nonenhanced T1-weighted (volumetric magnetization-prepared, rapid acquisition gradient echo), axial T2-weighted, and axial fluid-attenuated inversion recovery. Subsequently, time-resolved 3D CEMRV sequence was performed which allows for the acquisition of fast low angle shot (FLASH) data. A gadolinium-based contrast agent and saline were intravenously injected into the antecubital vein in each patient at the rate of 3 mL/s, using a power injector. For the CE 3D FLASH MRV acquisition, the contrast agent was administered at a dose of 0.1 mmoL/kg of body weight. Each contrast-medium injection was followed by injection of 25 ml of saline. The same injection protocol was followed in all patients. Three set of sequential acquisitions were done at 15 s delay, each yielding precontrast, angiography, and venography 3D data set. MRV 3D data were postprocessed on MR system inbuilt software, and maximum intensity projection and multiplanar reconstruction (MPR) were performed. Thickness of axial MPR image was subsequently increased to optimum threshold to include all the cortical veins and SSS in a single image. Inferior sagittal sinus (ISS) and its tributaries were carefully excluded by varying the axial thickness on correlation with corresponding sagittal and coronal MPR images or by manual exclusion of ISS on sagittal and coronal planes by postprocessing tool. Selective inclusion of SSS and cortical veins was obtained by cropping.
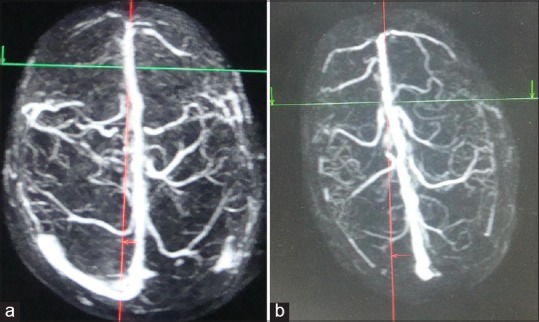
Coronal suture was identified on sagittal MPR images, and the corresponding point was marked on axial MPR images by placing cross references lines [Figure 1]. The AT-SSS, approximately 1 cm anterior to the marked point (corresponding to the coronal suture) and its draining veins were analyzed.
Figure 1.
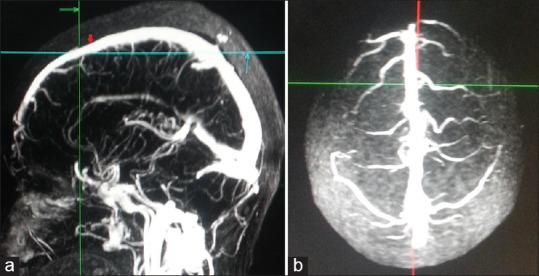
Methodology to mark anterior third superior sagittal sinus. (a) Point at the level of coronal suture on superior sagittal sinus was marked (red arrow) in midsagittal three-dimensional contrast-enhanced magnetic resonance venogram. 1 cm anterior to it marks the posterior limit of anterior third superior sagittal sinus (intersection of green and blue lines). (b) Corresponding superior view showing anterior third of superior sagittal sinus
Image analysis
In each case, the superior view of AT-SSS and all its draining veins were studied in detail. The numbers of veins draining on either side of AT-SSS were counted. Each draining vein was analyzed for its caliber, length, tributaries, and angle of drainage into AT-SSS. The caliber of each vein (millimeters) was measured at the middle of its length [Figure 2]. The length of veins (from its origin to the point where it drain to SSS) was measured. Each frontal lobe seen on the superior view was divided into 2 halves with a vertical paramedian line [Figure 3]. Attention was paid whether the vein extended beyond the paramedian line. Orientation of cortical veins that is angulation (in degrees) with the SSS was also noted. The posterior angle subtended by the line along the draining vein with the line along the SSS was calculated [Figure 4]. Veins were categorized into acute-angled, right-angled, or obtuse angled. A number of tributaries of each draining vein was noted [Figure 5].
Figure 2.
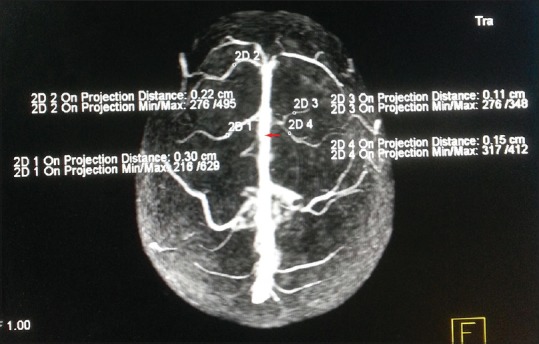
Superior view of three-dimensional contrast-enhanced magnetic resonance venogram showing multiple cortical veins draining to anterior third of superior sagittal sinus. The caliber of draining veins has been measured in a millimeter at its midpoint of the visible length (marked by small circles). The posterior limit of anterior third of superior sagittal sinus has been marked with red arrows
Figure 3.
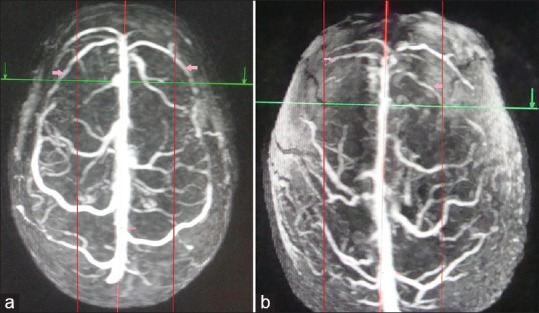
Superior view of three-dimensional contrast-enhanced magnetic resonance venogram of two different individuals showing varying areas of drainage to anterior third of superior sagittal sinus, proportional to the length of cortical veins. The posterior limit of anterior third of superior sagittal sinus has been marked with intersection of green line and red midline. (a) Long draining veins (pink arrows) in the anterior third of superior sagittal sinus crossing half the lateral surface of the frontal lobe (marked by 2 red paramedian lines). (b) Short draining veins (pink arrows) to anterior third of superior sagittal sinus, the length limited to the red parallel lines. The posterior limit of anterior third of superior sagittal sinus has been marked with red arrows
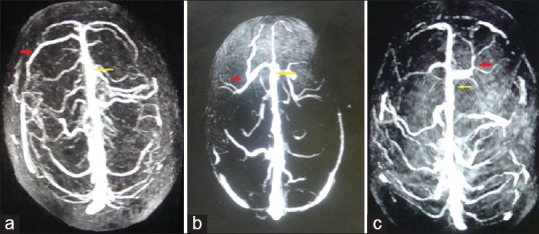
Figure 4.
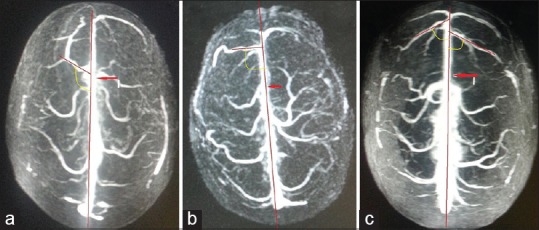
Superior view of three-dimensional contrast-enhanced magnetic resonance venogram of three different individuals showing the angle of drainage of cortical veins into the anterior third of superior sagittal sinus. The posterior angle of the draining vein into anterior third of superior sagittal sinus has been marked with yellow arcs. The angle is measured between the line along the major draining vein and the line along the superior sagittal sinus (Red arrow). (a) Acute angle, (b) right angle, (c) obtuse angle. The posterior limit of anterior third of superior sagittal sinus has been marked with red arrows
Figure 5.
Superior view of three-dimensional contrast-enhanced magnetic resonance venogram of three different individuals showing draining veins to anterior third of superior sagittal sinus and its various branching patterns. The posterior limit of anterior third of superior sagittal sinus has been marked with yellow arrows. (a) No branching of draining veins at anterior third of superior sagittal sinus. (b) Twin branching (red arrow) of draining veins at anterior third of superior sagittal sinus. (c) Multiple branching (red arrow) of draining vein at anterior third of superior sagittal sinus
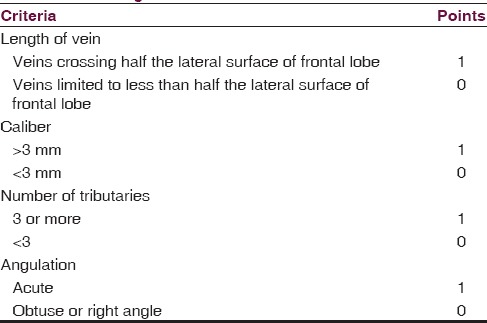
Each of the above-described parameters was assigned a numerical value 0 or 1 [Table 1]. Total points scored by an individual vein were calculated. The maximum score obtained by an individual vein was 4 and the minimum was 0. The draining volume of AT-SSS was derived by summing the points scored by each vein draining into it.
Table 1.
Scoring system for determining the venous drainage to the anterior third superior sagittal sinus based on three-dimensional contrast-enhanced magnetic resonance venogram
Results
We observed two constant veins at the tip of SSS in all cases, and these were not included for the scoring of AT-SSS to make the grading less cumbersome. There were three to four veins draining on either side to AT-SSS. A total of 224 veins draining to AT-SSS were studied in 60 individuals. Sixty-five (29%) of these cortical veins traversed more than half of the breadth of frontal lobe on its superior view. The caliber of 15 (6.6%) veins measured >3 mm and scored 1 point each. Most of the cortical veins are single or have two tributaries and scored a “0” for this parameter. Only 7 (3%) veins in 5 individuals showed three or more branches of cortical veins and scored 1 point each. Usually, the veins drain to the AT-SSS at different angles. Thirty-seven veins (16.5%) drained acute angle (<90°) to the AT-SSS. When these parameters suggesting high flow was studied in individuals the following results were observed. In 15 (25%) individuals, at least one vein had a caliber > 3 mm. Only 5 (8.3%) individuals showed one or more veins on either side of AT-SSS with 3 or more tributaries. In 15 (25%) individuals, the veins drained at an acute angle into the AT-SSS. In 20 (33%), at least one draining vein traversed more than half of the lateral frontal lobe.
On the basis of the four criteria (length of vein, its caliber, number of tributaries, and angulation with the superior sagittal sinus), we divided the cases into three groups. Type I is minimal drainage of frontal lobes into AT-SSS ligation (score 0–2). Type II with moderate drainage into AT-SSS ligation (score 3–5) and Type III is dominant drainage into AT-SSS ligation (score more than 6) [Figures 6 and 7]. In 26 cases, total points scored by cortical veins draining to AT-SSS was <2 (Type I); in 24 cases, it was 3–5 (Type II); and in ten cases, it was 6 or more (Type III).
Figure 6.
Superior view three-dimensional contrast-enhanced magnetic resonance venogram of different individuals categorized into different risk groups based on our risk stratification criteria. The posterior limit of anterior third of superior sagittal sinus has been marked with intersection of red and green lines. (a) Safe for ligation of anterior third of superior sagittal sinus. (b) Relatively safe for anterior third of superior sagittal sinus ligation (commonest variant)
Figure 7.
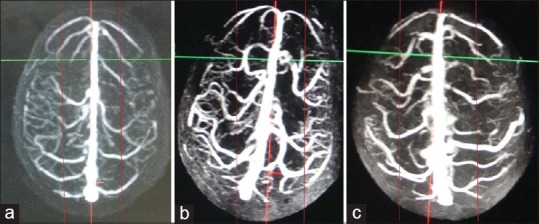
Superior view three-dimensional contrast-enhanced magnetic resonance venogram of 3 different individuals (a-c) categorized into high-risk groups based on our risk stratification criteria. The posterior limit of anterior third of superior sagittal sinus has been marked with red arrows
Discussion
The superior sagittal sinus extends from crista galli to torcular herophili. The SSS can be divided into three parts on the basis of length or in relation to bony landmarks such as bregma and lambda. However, cadaveric study suggests the AT is the length of the SSS located between the crista galli, and a point 16.4 mm (±6.4 mm standard deviation) anterior to the bregma.[4] We have applied these anatomical concepts on radiology and AT-SSS was calculated from the tip until 1 cm anterior to the coronal suture.
Anterior part of SSS mainly receives venous drainage from the frontal lobes. Rhoton described them as anterior, middle, or posterior frontal veins. His anatomical study showed veins entering the anterior part of the superior sagittal sinus are directed slightly posteriorly (obtuse angle).[5] However, we noticed that in 25% of individuals the veins may drain at acute angle into AT-SSS.
The traditional teaching since the time of Cushing is that the AT-SSS can be safely excised.[1] The ligation and division of AT-SSS is a key step to gain access the anterior skull base without retracting the frontal lobe. The result of resection or transection of AT-SSS has not been studied in detail. Nakamura et al. documented mortality in three of their cases due to massive frontal edema following ligation and division of AT-SSS.[2] Salunke et al. have shown that the ligation and transection of this segment can cause severe mental disorders, personality changes, recent memory loss, akinetic mutism, cerebral edema, and frontal venous infarction occasionally leading to death.[3] They postulated that patients harboring anterior skull base lesions with a dominant AT-SSS drainage are more likely to be affected. The anterior skull base lesions possibly compromise the basal venous drainage, making already dominant AT-SSS the only path of frontal venous drainage.[3] Although the tip is ligated, the reflection of the sinus may lead to its kinking at the craniotomy edge leading to stasis and thrombosis.[3] Even when it is not reflected, its mere exposure with small rents covered with gelfoam may lead to progressive thrombosis.
Preoperative evaluation is, therefore, essential in anterior skull base surgery to identify cases with frontal venous drainage predominantly to AT-SSS. CE MRV has now been accepted as a good alternative to traditional angiographic methods in interpreting cortical veins and sinus architecture.[6] The portion of SSS nearly 1 cm anterior to the coronal suture corresponds to the AT-SSS as described in the anatomical studies. The length, caliber, and its tributaries probably determine the area of frontal lobe a vein drains into the AT-SSS. Longer, larger veins are likely to drain more blood. Similarly, those veins with more tributaries would carry more blood. In addition, an acutely angulated vein into the AT-SSS is likely to drain more posterior and eloquent areas of frontal lobes. Hence, we used to these 4 parameters to judge the venous drainage into AT-SSS.
Different patterns of venous drainage to the AT-SSS have been described in a cadaveric study based on various morphological characters such as length of vein, its caliber, number of tributaries, and its angle of drainage into AT-SSS. These are (i) no drainage (7.14%); (ii) drainage of the frontal pole to less than a half of the lobe (64.29%); (iii) half of the anterior frontal lobe until the precentral sulcus (28.57%); and (iv) drainage of the entire surface of the frontal lobe (0%). The architecture of cortical veins determines the area of frontal lobe draining to the AT-SSS.[4]
We used similar parameters to analyze the venous drainage pattern of AT-SSS based on 3D CEMRV. A new scoring system was introduced to quantify individual draining vein. With this, we were able to predict the amount of venous drainage to each AT-SSS on postcontrast MRVs. The anatomical study on SSS has shown more than half of the frontal lobe drainage to AT-SSS in over 20% of cadavers.[4]
Extrapolating these results to our scoring system; 20% of the individuals had scores > 6 and suggested AT-SSS with dominant frontal lobe drainage. Probably, these are the cases having high drainage from frontal lobe to the AT-SSS where its ligation and transaction may not be safe.
The study suffers from some limitations. The study represents only a small subset of population. In addition, patients with anterior skull base tumors were not included thereby its clinical utility remains to be tested.
Nevertheless, the study does show possible variations of venous drainage of AT-SSS, and a method to quantify its venous drainage. A stratification and distribution of cases according to a score is presented. Further studies are needed to validate: (1) The structure-function association presented and (2) the proposed score clinical predictive value in defined context and usability. This would help us in identifying the individuals where ligation and transection of AT-SSS may be deemed risky.
Conclusion
The ligation and resection of AT-SSS may be dangerous in some patients. It is possible to identify individuals with dominant venous drainage into AT-SSS using contrast-enhanced-MRV where its sacrifice may be lead to untoward consequences.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shrivastava RK, Segal S, Camins MB, Sen C, Post KD. Harvey Cushing's meningiomas text and the historical origin of resectability criteria for the anterior one third of the superior sagittal sinus. J Neurosurg. 2003;99:787–91. doi: 10.3171/jns.2003.99.4.0787. [DOI] [PubMed] [Google Scholar]
- 2.Nakamura M, Struck M, Roser F, Vorkapic P, Samii M. Olfactory groove meningiomas: Clinical outcome and recurrence rates after tumor removal through the frontolateral and bifrontal approach. Neurosurgery. 2007;60:844–52. doi: 10.1227/01.NEU.0000255453.20602.80. [DOI] [PubMed] [Google Scholar]
- 3.Salunke P, Sodhi HB, Aggarwal A, Ahuja CK, Dhandapani SS, Chhabra R, et al. Is ligation and division of anterior third of superior sagittal sinus really safe? Clin Neurol Neurosurg. 2013;115:1998–2002. doi: 10.1016/j.clineuro.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Reis CV, Ferreira MA, Zabramski JM, Crusius MU, Deshmukh P, Gusmao SN, et al. The Divisions of the Superior Sagittal Sinus and the Ligation of its Anterior Third: Reviewing Concepts. Poster Presented at Congress of Neurological Surgeons Annual Meeting; Chicago, Illinois. 2006. [Google Scholar]
- 5.Rhoton AL., Jr The cerebral veins. Neurosurgery. 2002;51(4 Suppl):S159–205. [PubMed] [Google Scholar]
- 6.Nael K, Fenchel M, Salamon N, Duckwiler GR, Laub G, Finn JP, et al. Three-dimensional cerebral contrast-enhanced magnetic resonance venography at 3.0 Tesla: Initial results using highly accelerated parallel acquisition. Invest Radiol. 2006;41:763–8. doi: 10.1097/01.rli.0000236992.21065.04. [DOI] [PubMed] [Google Scholar]


